Abstract
BACKGROUND
The implications of measuring and rewarding performance for patients with multiple chronic conditions have not been explored empirically.
OBJECTIVE
To examine whether the number of chronic conditions was associated with patient’s receipt of recommended preventive care.
METHODS
We evaluated the association between the likelihood of receiving recommended preventive care and the number of chronic conditions in the diabetic population by analyzing the 2003 Medical Expenditure Panel Survey using logistic regression. Demographic characteristics and the number of chronic conditions were compared using χ2 tests.
OUTCOME MEASURES
Hemoglobin A1C test and diabetic eye exam.
RESULTS
In 2003, approximately 14.2 million non-institutionalized Americans had diabetes and 23% of them had five or more chronic conditions besides diabetes. Those patients were 67% ( < 0.05) and 50% ( < 0.001) more likely to receive hemoglobin A1C test and eye exams compared with diabetic patients with no additional chronic conditions. After adjusting for the number of office-based physician visits, a larger number of chronic conditions did not significantly affect the likelihood of receiving recommended care. Diabetic patients with more chronic conditions had more frequent office-based physician visits ( < 0.0001), and patients with 11 or more annual office-based physician visits were 43% ( < 0.05) and 40% ( < 0.01) more likely to receive hemoglobin A1C test and eye exam, respectively, compared with diabetic patients who had less than two office-based physician visits.
CONCLUSIONS
Diabetic patients with more chronic conditions may receive better quality of preventive care, partly due to their higher number of office-based physician visits.
KEY WORDS: quality of care, chronic conditions, performance measures
INTRODUCTION
During the past several decades, substantial resources have been invested in the development of clinical practice guidelines (CPGs), adherence to which should decrease improper variation and improve quality of care1. In recent years, an increasing number of health plans have begun profiling physician adherence to specific guideline components (known as “process” measures of quality) and also rewarding providers financially, based on these same quality measures2. Such process measures in pay for performance are generally derived from single CPG recommendations1.
While most CPGs address single diseases3, about 61 million Americans have multiple chronic diseases4, and they utilized 67% of pharmacy services4 and 49% of total health care expenditures4. Physicians could be overwhelmed by the number of recommendations for patients with multiple chronic conditions5, and forced to prioritize procedures due to time and financial constraints6,7. Previous research found that patients with multiple chronic conditions frequently receive uncoordinated care8, and physicians reported difficulty in organizing care for people with multiple chronic conditions9. From a patient’s perspective, receiving multiple pharmacological and lifestyle interventions may increase reluctance to adhere, tolerate and pay for already overwhelming recommendations10.
The widespread implementation of pay for performance, which rewards physicians’ CPG adherence based on single elements of care, has brought to the fore the limitations of single disease guidelines3,5 and raised concerns about patients with multiple diseases for whom physicians’ strict adherence to sets of CPGs may be infeasible or inappropriate . In addition, if physicians’ CPG adherence is appropriately lower for patients with comorbidities for either patient-or physician-driven reasons, then physicians who treat more complicated patients will be unfairly penalized with the implementation of pay-for-performance, creating an incentive to avoid such patients.
Some studies found that patients with higher comorbidity are less likely to receive preventive services11,12, while others suggested to the contrary13,14. The generalizability of these studies, however, has been questioned because data were limited to specific locations11,13,14, senior or minority group11,13, or the sample size was too small12.
In this paper, we evaluated the quality of care among diabetic patients as measured by patients’ receipt of recommended preventive care. We sought to examine whether greater numbers of chronic conditions were associated with patients’ receipt of recommended preventive care. We further sought to investigate what drives the quality differences between patients with greater vs. lower numbers of chronic conditions, and draw out the implications of implementing pay for performance among patients with multiple chronic conditions.
We focused on patients with diabetes based on the following grounds. First, diabetes measures are commonly used to profile the quality of health plans and providers6. Second, CPGs for diabetes and the associated clinical process measures of quality are well-established15. Third, diabetes causes significant health problems and financial burden; approximately 16 million Americans have diabetes16,17, costing $91 billion in 200218.
METHODS
Overview
We conducted a cross-sectional analysis using the 2003 Medical Expenditure Panel Survey19,20. Our study assessed the association between the number of chronic conditions and the likelihood of patients receiving recommended care by using logistic regressions.
Medical Expenditure Panel Survey
In order to address the study question, we analyzed the Medical Expenditure Panel Survey (MEPS)19,20, which is a nationally representative survey of health care use, including sources of payment, medications, expenditures, and insurance coverage for the non-institutionalized civilian U.S. population, conducted by the Agency of Health care Research and Quality (AHRQ). The households selected for the MEPS are a subsample of those drawn for the National Health Interview Survey (NHIS) conducted by the Center for Disease Control and Prevention and National Center for Health Statistics. NHIS uses a stratified, multistage probability cluster sampling design to obtain a representative sample of the U.S. population and oversamples African-American and Hispanic ethnicity. The overall response rate of 2003 MEPS was 64.5%19. The MEPS data include sampling weights that reflect the sampling frame and adjustment for non-response. The overall sample in the 2003 MEPS included approximately 34,000 community dwelling individuals, representing 290 million non-institutionalized people in the United States. Information on disease incidence came from the MEPS Medical Condition File20, which were derived based on patients recall, and recorded by interviewers as verbatim, and then coded by professional coders to ICD-9-CM codes for each medical event reported by respondents. The error rate of the coders did not exceed 2.5%. Our analysis did not include patients younger than 18, because the definition of chronic conditions for children under 18 is different from that of the general population21.
Medical Conditions
Definition of Diabetic Condition
To avoid underreporting problems and maximize sample size, we defined diabetics as patients who had any medical event in 2003, such as emergency room visit, outpatient visit, office-based physician visit, hospitalization, prescription drug refill, or home health events associated with International Classification of Disease, Ninth Revision (ICD-9) code 250.xx.
Definition of Chronic Conditions
We defined chronic conditions based on previous studies21,22. Specifically, a condition that lasted or was likely to last one year or longer, causing functional limitation and/or the need for ongoing medical care, was defined as chronic. Five internists determined whether ICD-9 codes as listed in the MEPS dataset satisfy the definition of chronic conditions, and 177 codes were classified as chronic in adults22.
To count the number of distinct chronic conditions per person, we employed the Agency for Healthcare Research and Quality (AHRQ)’s Clinical Classification Code (CCC20), which grouped all ICD-9 codes into 259 mutually exclusive, clinically homogeneous classes. Therefore, patients were regarded as having two chronic conditions if they had two conditions whose ICD-9 codes were classified as chronic, and if those two conditions were in different CCC classes. We applied CCC classes to MEPS Medical Condition File, which contains ICD-9 codes based on patients recall, and we counted the number of individual patients’ chronic conditions.
CCC has been previously used to measure comorbidity for predicting hospital utilization and mortality, and examine out-of-pocket spending for patients with chronic conditions22.
Number of Office-based Physician Visits
We counted the number of office-based physician visits, based on a speculation that patients with more physician interactions in an office setting would be more likely to receive recommended care, simply because of patient availability. We obtained the number of office-based physician visits per person from the MEPS full-year consolidation file. However, the MEPS full-year consolidate file does not identify whether patients received care by visiting same providers or multiple different providers. We also estimated the number of non-diabetic office-based physician visits, which excluded any office visits that were related with diabetes as indicated by ICD-9 code 250.xx. Non-diabetic office-based physician visits were used in sensitivity analysis to examine the robustness of our results.
Quality Measures
We compared the likelihood of receiving diabetes care, measured by hemoglobin A1C (HbA1C) test twice a year (yes/no) and a dilated eye exam once a year (yes/no), based on the American Diabetic Association (ADA) recommendations15. All of the quality measures were based on self-report.
We did not include the likelihood of receiving a pap smear test, despite strong evidence of benefit suggested by United States Preventive Services Task Force23, because pap smears are not recommended for patients age 65 and older, the age category for 50% of the patients in our sample (Table 1); thus we will exclude about 75% of our sample (50% male, and then remaining 50% of them are women age 65 and older). Colorectal cancer screening was excluded in our analysis, because MEPS does not allow us to distinguish between sigmoidoscopy and colonoscopy23. An annual foot exam was also excluded from our analysis, because the definition of “foot exam” in MEPS was not clear: since respondents could confuse “visual foot inspection,” which is recommended at every visit for people with neuropathy, with “comprehensive foot exam,” which is recommended by ADA15.
Table 1.
Demographic Characteristics of Non-institutionalized Diabetic Patients in U.S. Population
| Number of chronic conditions other than diabetes | Total | value | ||||
|---|---|---|---|---|---|---|
| 0 | 1∼2 | 3∼4 | 5≥ | |||
| Age | <0.0001 | |||||
| Older than 65 | 16 | 40 | 51 | 54 | 41 | |
| 65 and younger | 85 | 60 | 49 | 46 | 59 | |
| Sex | <0.0001 | |||||
| Male | 56 | 40 | 40 | 31 | 41 | |
| Female | 44 | 60 | 60 | 69 | 59 | |
| Race | 0.002 | |||||
| White | 66 | 74 | 81 | 81 | 77 | |
| Black | 22 | 19 | 13 | 15 | 16 | |
| Others | 11 | 8 | 6 | 4 | 7 | |
| Insurance | <0.0001 | |||||
| Private | 65 | 65 | 65 | 57 | 63 | |
| Public | 30 | 32 | 32 | 40 | 30 | |
| Uninsured | 5 | 3 | 3 | 3 | 7 | |
| Education | 0.95 | |||||
| <High school | 43 | 42 | 42 | 43 | 42 | |
| High school | 35 | 30 | 32 | 35 | 32 | |
| >High school | 23 | 28 | 26 | 23 | 26 | |
| Annual number of office-based physician visits | <0.0001 | |||||
| 0∼2 | 59 | 25 | 15 | 6 | 23 | |
| 3∼5 | 22 | 32 | 27 | 12 | 28 | |
| 6∼10 | 13 | 25 | 29 | 27 | 29 | |
| 11≥ | 5 | 18 | 29 | 54 | 20 | |
| Diabetic population | ||||||
| 17 | 24 | 36 | 23 | 100 | ||
All the numbers are in percent, except the -values
-values were estimated based on χ2 tests
Statistical Analyses
Demographic characteristics and the number of chronic conditions were compared using χ2 tests. We analyzed the likelihood of receiving CPG-concordant care as a function of the number of chronic conditions and other patient characteristics using logistic regression. Age, race (white, black, others), insurance (none, private, or public plans) and education were included in our analysis as independent variables, because previous studies suggested that those variables were associated with quality of care24,25. Insulin use was included in the analysis, because insulin users were more likely to have advanced diabetes, compared with patients who do not use insulin. The number of chronic conditions other than diabetes, and the number of office-based physician visits were categorized into their quartiles to maximize statistical power. The age variable was dichotomized with 65 as a cut-off, because of the skewed nature of its distribution. We specified these variables as continuous and compared the results of logistic regression under continuous vs. categorical specifications, and the results were not different at statistically significant level.
Due to the clustered and correlated nature of the survey data, statistical analysis was performed using survey-specific procedures in SAS version 9.1 (SAS institute Inc, Cary, NC) to account for multistage sampling designs. Appropriate sampling weight, clustering, and stratification information, which are all publicly available, have been applied in the model estimation.
RESULTS
Descriptive Statistics
The sample from the 2003 MEPS data included about 1,700 diabetic patients age 18 and older, representing 14.2 million non-institutionalized civilian diabetic U.S. patients. About 23% of them, or 3.3 million diabetic patients, have 5 or more additional chronic conditions (Table 1). The number of chronic conditions other than diabetes was strongly associated with the number of office-based physician visit, as demonstrated by Table 1 ( < 0.0001). Diabetic patients who have five or more additional chronic conditions are more likely to be older, female, white, publicly insured, and have more office-based physician visits than diabetic patients with no additional chronic conditions ( < 0.01). Differences in the sample size for eye exam (1,396) and HbA1C (1,070) test are due to non-response.
Number of Chronic Conditions, and the Likelihood of Receiving Recommended Services
Figure 1 illustrates that the use of recommended care is positively correlated with the number of chronic conditions other than diabetes ( < 0.001). Tables 2 and 3 summarized the results of regression analyses, analyzing the association between demographic characteristics and the likelihood of receiving HbA1C test and eye exam, respectively. Model 1 (Table 2) and Model 4 (Table 3) are base models which examine the association between the number of chronic conditions and the likelihood of receiving quality of diabetes care, after adjusting for demographic characteristics. Model 1 and Model 4 show that higher number of chronic conditions other than diabetes is strongly associated with the increased use of diabetes management (HbA1C, < 0.05, Model 1, Table 2; eye exam, < 0.01, Model 4, Table 3).
Figure 1.
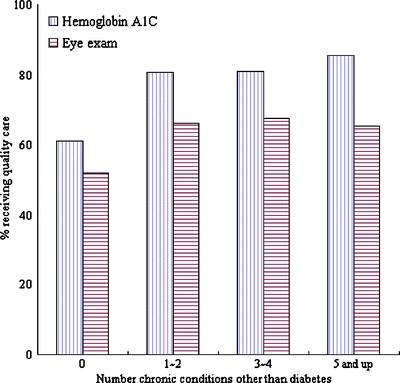
Association between the number of chronic conditions and quality measures. values for hemoglobin A1C test and eye exam vs. number of chronic conditions were less than 0.001, based on χ2 test.
Table 2.
Results of Multivariate Logistic Regression Analysis Adjusted by Number of Additional Chronic Conditions and Other Demographic Characteristics on the Likelihood of Receiving HbA1C Test in the Non-institutionalized, Adult, Diabetic US Population
| HbA1C test | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | |||
| 65 and older vs. younger than 65 | 1.09 (0.89–1.33) | 1.06(0.87–1.30) | 0.89 (0.64–1.22) |
| Sex | |||
| Male vs. female | 0.98 (0.82–1.18) | 0.99 (0.82–1.20) | 1.01 (0.84–1.22) |
| Race | |||
| Other vs. white | 1.24 (0.72–2.13) | 1.22 (0.67–2.22) | 1.01 (0.58–1.77) |
| Black vs. white | 0.96 (0.64–1.42) | 1.01 (0.67–1.54) | 1.04 (0.69–1.57) |
| Education | |||
| <High school(HS) vs. >HS | 0.73 (0.57–0.94)* | 0.76 (0.59–0.97)* | 0.74 (0.57–0.95)* |
| HS vs. >HS | 0.99 (0.80–1.22) | 0.97 (0.78–1.20) | 1.02 (0.82–1.28) |
| Insurance | |||
| Private vs. uninsured | 1.22 (0.95–1.56) | 1.16 (0.91–1.49) | 1.1 (0.83–1.46) |
| Public vs. uninsured | 1.33 (0.95–1.86) | 1.28 (0.91–1.79) | 1.32 (0.62–1.53) |
| Insulin use | |||
| Yes vs. no | 0.93 (0.82–1.18) | 0.9 (0.72–1.11) | 0.86 (0.70–1.07) |
| Number of additional chronic conditions | |||
| 1∼2 vs. none | 1.18 (0.88–1.59) | 1.22 (0.90–1.65) | 1.05 (0.77–1.45) |
| 3∼4 vs. none | 1.1 (0.83–1.44) | 1.03 (0.77–1.36) | 1.11 (0.80–1.54) |
| 5 and up vs. none | 1.67 (1.13–2.46)* | 1.34 (0.89–2.01) | 1.54 (1.01–2.33)* |
| Total number of office-based physician visits | |||
| 3∼5 vs. 0∼2 | − | 0.8 (0.53–1.21) | − |
| 6∼10 vs. 0∼2 | − | 1.62 (1.15–2.28)† | − |
| 11 ≥ vs. 0∼2 | − | 1.43 (1.02–2.01)* | − |
| Total number of non-diabetes related office-based physician visits | |||
| 2–3 vs. 0–1 | − | − | 0.9 (0.63–1.28) |
| 4–7 vs. 0–1 | − | − | 1.2 (0.84–1.70) |
| 8 and up vs. 0–1 | − | − | 1.48 (1.04–2.12)* |
‡Significant at < 0.001; †significant at < 0.01; *significant at < 0.05 .
Model 1 shows the association between the number of chronic conditions and the likelihood of receiving HbA1C test, adjusted by demographic characteristics.
Model 2 shows the association between the number of office-based physician visits and the likelihood of receiving HbA1C test, adjusted by demographic characteristics and the number of chronic conditions.
Model 3 shows the association between the number of non-diabetes related office-based physician visits and the likelihood of receiving HbA1C test, adjusted by demographic characteristics and the number of chronic conditions.
Table 3.
Results of Multivariate Logistic Regression Analysis Adjusted by the Number of Additional Chronic Conditions and Other Demographic Characteristics on the Likelihood of Receiving Eye Exam in the Non-institutionalized, Adult, Diabetic US Population
| Eye exam | Model 4 | Model 5 | Model 6 |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | |||
| 65 and older vs. younger than 65 | 1.27 (1.07–1.50)‡ | 1.25 (1.06–1.48)† | 1.28 (1.08–1.52)† |
| Sex | |||
| Male vs. female | 0.83 (0.72–0.96)* | 0.83 (0.72–0.96)* | 0.84 (0.72–0.98)* |
| Race | |||
| Other vs. white | 0.97 (0.72–1.32) | 0.95 (0.69–1.29) | 0.9 (0.65–1.25) |
| Black vs. white | 0.92 (0.71–1.20) | 0.96 (0.74–1.24) | 1.01 (0.77–1.32) |
| Education | |||
| <High School(HS) vs. >HS | 0.71 (0.57–0.88)† | 0.72 (0.58–0.90)† | 0.73 (0.58–0.91)† |
| HS vs. >HS | 1.22 (1.01–1.48)* | 1.21 (0.99–1.48) | 1.27 (1.05–1.54)* |
| Insurance | |||
| Private vs. uninsured | 1.32 (1.04–1.66) | 1.29 (1.01–1.64)* | 1.31 (1.03–1.68)* |
| Public vs. uninsured | 0.99 (0.76–1.28) | 0.95 (0.74–1.24) | 0.89 (0.67–1.18) |
| Insulin use | |||
| yes vs. no | 1.16 (0.99–1.36) | 1.14 (0.97–1.33) | 1.01 (0.93–1.29) |
| Number of additional chronic conditions | |||
| 1∼2 vs. none | 0.88 (0.69–1.13) | 0.92 (0.71–1.17) | 0.85 (0.65–1.11) |
| 3∼4 vs. none | 1.06 (0.85–1.32) | 1.03 (0.83–1.29) | 1.04 (0.83–1.31) |
| 5 and up vs. none | 1.5 (1.15–1.95)† | 1.27 (0.95–1.70) | 1.37 (1.02–1.84)* |
| Total number of office-based physician visits | |||
| 3∼5 vs. 0∼2 | − | 0.81 (0.65–1.01) | − |
| 6∼10 vs. 0∼2 | − | 1.18 (0.93–1.49) | − |
| 11 ≥ vs. 0∼2 | − | 1.4 (1.11–1.76)† | − |
| Total number of non-diabetes related office-based physician visits | |||
| 2–3 vs. 0–1 | − | − | 0.8 (0.63–1.02) |
| 4–7 vs. 0–1 | − | − | 0.98 (0.76–1.27) |
| 8 and up vs. 0–1 | − | − | 1.39 (1.06–1.81)* |
‡Significant at < 0.001; †significant at < 0.01; *significant at < 0.05.
Model 4 shows the association between the number of chronic conditions and the likelihood of receiving eye exam, adjusted by demographic characteristics
Model 5 shows the association between the number of office-based physician visits and the likelihood of receiving eye exam, adjusted by demographic characteristics and the number of chronic conditions
Model 6 shows the association between the number of non-diabetes related office-based physician visits and the likelihood of receiving eye exam, adjusted by demographic characteristics and the number of chronic conditions
Number of Office-based Physician Visits, and the Likelihood of Receiving Recommended Services
After controlling for the number of office-based physician visits, the number of chronic condition other than diabetes became less significant predictor of using recommended services (Model 2, Table 2; Model 5, Table 3). Patients with higher number of office-based physician visits were more likely to receive diabetes management services (HbA1C, < 0.05, Model 2, Table 2; eye exam, < 0.01, Model 5, Table 3) demonstrate that the number of office-based physician visits attenuated the association between the number of chronic conditions and the utilization of diabetes management services, which suggests that the positive correlation between the number of chronic conditions and the increased use of recommended services are driven by the fact that diabetic patients with higher number of conditions have more frequent office-based physician visits, as demonstrated by Table 1.
Sensitivity Analysis
Since the number of office-based physician visits aggregated any office-based physician visits regardless of the nature of the visits, we estimated the number of non-diabetes associated office-based physician visits by excluding any office-based physician visits with ICD-9 code 250.xx, based on a speculation that the number of diabetes-related visits and diabetes management services are not independent. Models 3 and 6 suggest that patients with higher number of non-diabetes related visits were still strong predictors in receiving recommended diabetes cares, increasing the odds of receiving HbA1C by 48% ( < 0.05, Model 3, Table 2) and eye exam by 39% ( < 0.05, Model 6, Table 3).
DISCUSSION
Our results suggest that in the diabetic population, patients with more number of chronic conditions are more likely to receive better quality of care: they received more diabetes management services. Our result is consistent with previous studies, which suggested that patients with multiple diseases are more likely to receive preventive care13,14, and Rosen and colleagues’ study25, which found that diabetic patients with multiple diseases are more likely receive recommended chronic care. We found that the higher quality of care for these diabetic patients was associated with their frequent office-based physician visits, and the finding was robust when we excluded diabetes-related office-based physician visits.
The result of our study is opposite to that of previous studies11,12, which concluded that cancer screening rate decreased as comorbidity increased. The difference may be driven by the fact that they defined the comorbidity based on Charlson comorbidity index, which gives more weight to patients with serious conditions, whereas we added the number of chronic conditions to estimate the competing demand for recommended care. Their studies were focused more on how patients’ health status (i.e., good, mild, severe) affect cancer screening, whereas we explores how competing demand and prioritization affect diabetes quality of care. Our finding is opposite to Frayne and colleagues’ study26, which focus on the impact of mental illness on diabetes care. Since mental illnesses tend to impair diabetic patients’ self-care and communication27, findings from these patients are less likely to be generalizable to our target population, i.e., diabetic patients with any chronic conditions. Our findings are somewhat at odds with Schectman et al.’s study28, which showed that the number of visits are not correlated with quality of care. Yet, it might be possible that our patients are seeing different providers and this led to better quality of care.
Because of time constraints and competing demand6,7, one might assume that patients with multiple chronic conditions are less likely to receive recommended care, which could influence the amount of financial reward for physicians under the pay-for-performance system. We found that those patients actually receive more preventive care services, because those patients are making more office-based visits, and being more available to physicians. If patients in our analysis were seeing same providers, instead of seeing multiple different providers, then our study suggests that implementing pay-for-performance may not necessarily punish physicians who care for patients with multiple chronic conditions. We could not examine whether those patients were seeing single or multiple providers, due to data limitation.
Still, it remains unclear whether receipt of several recommended service is in the best interest of patients, given the burden of complying with several sets of protocols. Moreover, the consequences of applying multiple sets of CPGs may manifest patient behaviors that we were not able to examine in our data, including reduced patient adherence to medication recommendations or behavioral changes indicated by the relevant CPGs.
There are several limitations as to this explanatory analysis. First, we could not observe physicians’ pattern of prioritizing treatment based on the severity of underlying conditions, because ICD-9 codes do not report the severity of the diseases. Also, we did not consider the intensity of office visits because of data limitations; mean length of office visits to physicians ranges from 13.9 to 21.4 minutes per visit29, which might reflect the variation in intensity of visit.
Second, we counted the number of chronic conditions to quantify competing demands for physicians. However, we recognize that counting the number of chronic conditions without accounting for severity of illness over-simplifies the reality.30,31
Third, our analysis does not include other “process” measures of diabetes quality of care, such as microalbuminuria test and serum cholesterol level (LDL-C) screening, because MEPS does not provide such information. We also could not include “outcome” measures for diabetes, like HbA1C<7.0%, due to data limitations. It is not clear whether patients who receive better quality of care measured by our analysis also receive better quality of care in these other quality measures.
Finally, all of our outcome measures were based on self-report, thus patients with better recall are more likely to report more diagnoses, which could lead to a positive correlation between the number of chronic conditions and the quality of care received. Our statistical analysis shows that correlations between quality of care received (eye exam, HbA1C test, PSA, and pap smear; result not shown) and the number of chronic conditions were inconsistent, which implies that our results are less likely to be driven by recall bias. Also, due to data limitation, our study fails to identify whether patients were seeing single provider or multiple providers, which could influence patients’ quality of care. Future research, using patients billing data, is needed to reinforce our findings.
CONCLUSION
In summary, we found that diabetic patients with multiple chronic conditions may receive better quality of preventive care, partly due to their higher number of office-based physician visits. To the extent that our findings reflect a general pattern in receiving recommended preventive care for chronically ill populations, they suggest that current incentive programs would not necessarily disadvantage those who care for patients with multiple chronic conditions, if patients in our analysis were seeing single provider. Given that we found nearly a quarter of patients to have reported 5 or more comorbidities, however, further work is needed to examine appropriate clinical prioritization in these instances.
Acknowledgement
This study was financially supported by Harvard School of Public Health institutional funding. Authors are grateful to Dr. Wenke Hwang for sharing the classification system. Helpful comments from Dr. David Kashikara of Agency of Health Care Research and Quality, and Dr. Chapin White of Congressional Budget Office are also greatly appreciated.
Conflicts of interest None disclosed.
Footnotes
Financial support: Harvard School of Public Health Institutional Funding
Contributor Information
SeungJin Bae, Phone: +82-2-21822537, FAX: +82-2-5856918, Email: genice@hiramail.net, Email: sj.susan.bae@gmail.com
Meredith B. Rosenthal, Phone: +1-617-4323418, FAX: +1-617-4324494, Email: mrosenth@hsph.harvard.edu
References
- 1.Garber AM. Evidence-based guidelines as a foundation for performance incentives. Health Aff (Millwood). 2005;24(1):174–9. [DOI] [PubMed]
- 2.Rosenthal MB, Fernandopulle R, Song HR, Landon B. Paying for quality: providers’ incentives for quality improvement. Health Aff (Millwood). 2004;23(2):127–41. [DOI] [PubMed]
- 3.Tinetti ME, Bogardus ST Jr, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351(27):2870−4. [DOI] [PubMed]
- 4.Anderson G, Horvath J. The growing burden of chronic disease in America. Public Health Rep. 2004;119(3):263−70. [DOI] [PMC free article] [PubMed]
- 5.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716−24. [DOI] [PubMed]
- 6.Hofer TP, Zemencuk JK, Hayward RA. When there is too much to do: how practicing physicians prioritize among recommended interventions. J Gen Intern Med. 2004;19(6):646−53. [DOI] [PMC free article] [PubMed]
- 7.Yarnall KSH, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention. Am J Public Health. 2003;93(4):635−41. [DOI] [PMC free article] [PubMed]
- 8.Gurwitz JH, Field TS, Judge J, et al. The incidence of adverse drug events in two large academic long-term care facilities. Am J Med. 2005;118(3):251–8. [DOI] [PubMed]
- 9.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162(20):2269–76. [DOI] [PubMed]
- 10.O’Connor PJ. Adding value to evidence-based clinical guidelines. JAMA. 2005;294(6):741–3. [DOI] [PubMed]
- 11.Kiefe CI, Funkhouser E, Fouad MN, May DS. Chronic disease as a barrier to breast and cervical cancer screening. J Gen Intern Med. 1998;13(6):357–65. [DOI] [PMC free article] [PubMed]
- 12.Schoen RE, Marcus M, Braham RL. Factors associated with the use of screening mammography in a primary care setting. J Community Health. 1994;19(4):239–52. [DOI] [PubMed]
- 13.Heflin MT, Oddone EZ, Pieper CF, Burchett BM, Cohen HJ. The effect of comorbid illness on receipt of cancer screening by older people. J Am Geriatr Soc. 2002;50(10):1651–8. [DOI] [PubMed]
- 14.Bostick RM, Sprafka JM, Virnig BA, Potter JD. Predictors of cancer prevention attitudes and participation in cancer screening examinations. Prev Med. 1994;23(6):816–26. [DOI] [PubMed]
- 15.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2005;28(1):S4–36. [DOI] [PubMed]
- 16.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414–31. [DOI] [PubMed]
- 17.Nathan DM. Long-term complications of diabetes mellitus. N Engl J Med. 1993;328(23):1676–85. [DOI] [PubMed]
- 18.American Diabetes Association. Economic costs of diabetes in the U.S. in 2002. Diabetes Care. 2003;26(3):917–32. [DOI] [PubMed]
- 19.Agency for Healthcare Research and Quality. MEPS HC-079: 2003 Full Year Consolidated Data File. Rockville, MD; 2005 November.
- 20.Agency for Healthcare Research and Quality. MEPS HC-078: 2003 Medical Conditions. Rockville, MD; 2005 November.
- 21.Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. JAMA. 1996;276(18):1473–9. [DOI] [PubMed]
- 22.Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Aff (Millwood). 2001;20(6):267–78. [DOI] [PubMed]
- 23.United States Preventive Services Task Force. 2008. Available at http://www.ahrq.gov/clinic/USpstfix.htm Accessed August 20, 2008.
- 24.Ferris TG, Blumenthal D, Woodruff PG, Clark S, Camargo CA. Insurance and quality of care for adults with acute asthma. J Gen Intern Med. 2002;17(12):905–13. [DOI] [PMC free article] [PubMed]
- 25.Rosen AB, Karter AJ, Liu JY, Selby JV, Schneider EC. Use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in high-risk clinical and ethnic groups with diabetes. J Gen Intern Med. 2004;19(6):669–75. [DOI] [PMC free article] [PubMed]
- 26.Frayne SM, Halanych JH, Miller DR, et al. Disparities in diabetes care: impact of mental illness. Arch Intern Med. 2005;165(22):2631–8. [DOI] [PubMed]
- 27.Desai MM, Rosenheck RA, Druss BG, Perlin JB. Mental disorders and quality of diabetes care in the veterans health administration. Am J Psychiatry. 2002;159(9):1584–90. [DOI] [PubMed]
- 28.Schectman G, Barnas G, Laud P, Cantwell L, Horton M, Zarling EJ. Prolonging the return visit interval in primary care. Am J Med. 2005;118(4):393–9. [DOI] [PubMed]
- 29.Mechanic D, McAlpine DD, Rosenthal M. Are patients’ office visits with physicians getting shorter. N Engl J Med. 2001;344(3):198–204. [DOI] [PubMed]
- 30.Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–31. [DOI] [PubMed]
- 31.Meduru P, Helmer D, Rajan M, Tseng C-L, Pogach L, Sambamoorthi U. Chronic illness with complexity: implications for performance measurement of optimal glycemic control. J Gen Inter Med. 2007;22(Suppl 3):408–18. [DOI] [PMC free article] [PubMed]


