ABSTRACT
BACKGROUND
Ageing and depression are associated with disability and have significant consequences for health systems in many other developing countries. Depression prevalence figures among the elderly are scarce in developing countries.
OBJECTIVE
To estimate the prevalence of depressive symptoms and their cross-sectional association with selected covariates in a community sample of Mexico City older adults affiliated to the main healthcare provider.
DESIGN
Cross-sectional, multistage community survey.
PARTICIPANTS
A total of 7,449 persons aged 60 years and older.
MEASUREMENTS
Depression was assessed using the 30-item Geriatric Depression Scale (GDS); cognitive impairment, using the Mini-Mental State Examination; and health-related quality of life with the SF-36 questionnaire.
MAIN RESULTS
The prevalence of significant depressive symptoms was estimated to be 21.7%, and 25.3% in those aged 80 and older. After correcting for GDS sensitivity and specificity, major depression prevalence was estimated at 13.2%. Comparisons that follow are adjusted for age, sex, education and stressful life events. The prevalence of cognitive impairment was estimated to be 18.9% in depressed elderly and 13.7% in non-depressed. SF-36 overall scores were 48.0 in depressed participants and 68.2 in non-depressed (adjusted mean difference = −20.2, 95% CI = −21.3, −19.1). Compared to non-depressed elderly, the odds of healthcare utilization were higher among those depressed, both for any health problem (aOR 1.4, 95% CI = 1.1, 1.7) and for emotional problems (aOR 2.7, 95% CI = 2.2, 3.2).
CONCLUSIONS
According to GDS estimates, one of every eight Mexican older adults had major depressive symptoms. Detection and management of older patients with depression should be a high priority in developing countries.
KEY WORDS: aged, depression, comorbidity, primary healthcare
INTRODUCTION
The Global Burden of Disease study identified unipolar depression as the main cause of years lost to disability worldwide in 2001, amounting to about 9.5% of all losses1. If depression at all ages is an important public health problem, depression in the elderly represents an even greater challenge because of its implications for families, the society as a whole, and for public health services2. Depression in the elderly can predispose to chronic medical conditions or adversely affect their evolution3–5 and can delay rehabilitation due to the impact on mental and social functional decline6. The toll of depression also includes a decrease in quality of life3,7,8 and a higher risk of premature death from cardiovascular disease5. However, only a fraction of people with depression are recognized, and an even a smaller fraction receives adequate treatment, increasing the demand for healthcare services and associated costs9–14.
In developed countries, depression prevalence in the elderly has been found to range between 7 and 36% in out-patients and to be close to 40% in hospitalized patients15. Prevalence estimates from developing countries are scarcer. In Mexico, for instance, the few depression prevalence studies carried out have not focused on persons 60 years and older, and, consequently, sample sizes have been too small to yield precise estimates16–19.
However, depression in older adults may have significant consequences for health systems in Mexico and many other developing countries. The overarching goal of this study was to analyze the scope of depression among older adults as well as the cross-sectional relationships of depression with cognitive impairment, social and demographic variables, quality of life, and utilization of health services in a representative community sample of Mexico City residents aged 60 years and older, insured by the main healthcare provider in the city, the Mexican Institute of Social Security (IMSS for its initials in Spanish: Instituto Mexicano del Seguro Social).
MATERIALS AND METHODS
Study Population
Data reported here are from the first wave of the “Integrated Study of Depression Among Elderly Insured by IMSS in Mexico City.” The population base consists of all non-institutionalized persons 60 years or older insured by IMSS and residing in Mexico City (N = 384,000), which represents 48% of all Mexico City people 60 years and older. IMSS is a mandatory social security system offering a comprehensive package of benefits, including healthcare at all levels, as well as economic benefits such as a retirement pension. IMSS-insured workers and their close relatives are affiliated to a Family Medicine Unit on the basis of their home address. Elderly insured by the IMSS are more likely to have 6 or less years of education than their non-IMSS affiliated counterparts.
Sampling Strategy and Representativeness
A three-stage cluster sampling procedure was used to obtain a probabilistic sample of IMSS affiliates, regardless of their healthcare utilization. Initially, 8 of the 45 IMSS Family Medicine Units existing in the City were randomly selected (two in each of four regions in which Mexico City is divided by IMSS). Next, within each selected Family Medicine Unit, we randomly selected 12 physician offices. Finally, a list of all insured people (locally named “patient lists”) for each physician office was obtained, and the records of 29,340 Mexico City residents who were 60 years or older at the time of the survey were extracted from these lists regardless of service utilization to avoid selection bias.
However, it is important to note that patient lists are kept locally and are not actively updated in case of death or change of address. They contain only information on date of birth, gender, and the patient’s address. Up to two home visits by research interviewers were scheduled for all the 29,340 identified persons. During the home visits, we were not able to contact 11,373 identified persons for the reasons stated in Figure 1, mainly due to address errors or change of address (73%) or because the chosen respondent had died (24%). Thus, 17,967 enlisted persons were potentially reachable to be interviewed. Of them, 4.1% were either sick at the time of the interview or had a delirium-associated altered mental state, as assessed by the trained personnel who made the home visits, and 7,482 were interviewed (25.5% of those originally identified and 41.9% of those reachable to be interviewed). No contact could be established with 8,846 potential participants. Only a small fraction of potential participants openly refused to participate in the study (4.9%). A sub-study on a 10% random sample of those not contacted was done to test if a more intensive household visiting strategy would yield different results, but very similar rates were obtained (data available upon request). Thus, correcting the sample frame for address errors or changes resulted in a total sampling frame of 12, 172 individuals, and a response rate of 61.5%. The response rates are consistent with similar studies around the world20.
Figure 1.
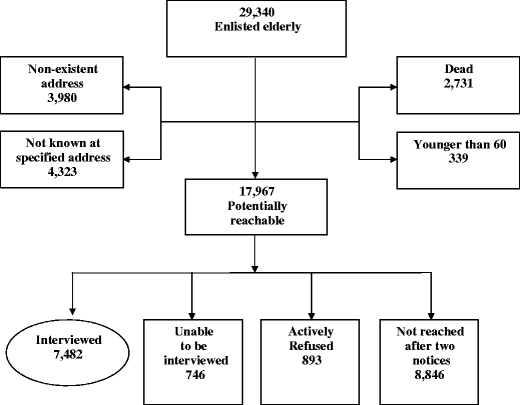
Results of home interview visits to the selected individuals.
In order to improve sample representativeness, we used post-stratification and calculated selection probabilities using census data21. Counts of interviewed persons were obtained for a simultaneous cross-tabulation of 5-year age groups, gender, and five education groups. The same table was assembled for the counts of Mexico City residents, estimated using Census data and official population projections. This allowed us to calculate selection probabilities specific by age, gender, and education, which were used as sampling weights in all statistical analyses. The post stratification allowed to correct for the fact that respondents under-represented those 85 and older as well as those highly educated (28% and 39%, respectively) and over-represented those less educated older adults (60%).
Measurements
Depression was assessed using the 30-item Geriatric Depression Scale (GDS)22. The GDS was developed specifically for interviewing older persons, was not based on somatic symptoms, and has been widely used in different settings23–25, including community studies26. The GDS is easy to administer and possesses adequate sensitivity (∼92%) and specificity (∼89%)27–31. Participants with a score of 11 points or higher in the GDS were considered to have significant depressive symptoms. For this study “depression” was operationally defined as the presence of significant depressive symptoms according to the GDS.
Questions were also included to determine the presence, during the previous year, of nine stressful events that have been found to be associated to depression32. Four events (serious illness or injury, increased trouble with daily activities, and loss of vision or hearing) were considered to indicate the presence of recent severe morbidity. The other five dealt with participant retirement, financial problems, trouble with neighbors, marital separation/divorce, and serious illness of someone close to the participant.
Cognitive impairment was assessed with a previously validated Mexican version of the Mini Mental State Examination (MMSE)33. A threshold of 23 points or less was used to indicate cognitive impairment. Health-related quality of life (HRQOL) was measured with a previously validated Mexican version of the 36-item Short Form Health Survey (SF-36)34–35. Scoring was performed using the RAND algorithm36, which produces an overall SF–36 score as well as scores for eight subscales (physical functioning, role limitations due to physical health or to emotional problems, vitality, emotional well being, social functioning, bodily pain, and general health). Scores range from 0 to 100, with higher scores indicating better health-related quality of life.
Health care utilization was assessed through two questions about health care use during the previous 6 months, “for any reason” or “because of emotional problems,” and by individual questions about the type of healthcare facilities attended in each case, both at any healthcare institution or at specific IMSS healthcare facilities.
Data were collected from July to December of 2004 through a standardized questionnaire, administered through face-to-face interviews at the participant’s home by previously trained personnel, and supervised by qualified research assistants.
Data Analysis
Logistic regression was used to model the prevalence of significant depressive symptoms and cognitive impairment as a function of age, gender, education, marital status, and stressful life events. The association between depression and health-related quality of life and healthcare use was examined by classifying the sample into four groups, based on the cross-tabulation between depression and recent severe morbidity (no depression and no recent severe morbidity, no depression but recent severe morbidity, depression and no recent severe morbidity, and depression and recent severe morbidity). This stratification variable allowed us to identify if lower health-related quality of life or higher healthcare use was due to depression and not to recent severe morbidity and if the effect of depression alone was similar to the effect of recent morbidity alone. This variable was used as the predictor of interest in multivariate models that simultaneously adjusted for age, sex, education, serious illness of someone close, retirement, trouble with neighbors, financial problems, and marital separation. Adjusted means or proportions are presented based on these models and setting the rest of predictors to their mean values in the sample.
Due to the complex sample design and post-stratification of the sample, conventional methods for obtaining standard errors were not appropriate. Rather, standard errors were obtained, in all analyses, through bootstrap re-sampling techniques with 2,500 sample replications37. Replicates were obtained considering the strata and sample clusters employed in our survey. STATA software, version 9.2, was used in all analyses38.
RESULTS
Prevalence of Significant Depressive Symptoms
A total of 7,482 older adults was interviewed, and 7,449 had non-missing values on key variables. Table 1 shows depression prevalence estimates among IMSS-insured elderly residing in Mexico City by age-group and gender. The overall estimated prevalence of depression in this population was 21.7% (95% CI, 20.4–23.0). Women showed a higher proportion of depression (24.7%) than men (16.2%). In both genders, depression prevalence showed similar figures in all age groups with overlapping 95% confidence intervals, yet it seemed the highest in the 75–79 age group and lowest in those 90 years and older. Depression prevalence for those 80 and older was 25.3% (95% CI, 21.8–29.2).
Table 1.
Prevalence of Significant Depressive Symptoms Among Older Adults in Mexico City Based on Responses to the Geriatric Depression Scale Score of 11 or Higher
| Women | Men | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age in years | n | (%)* | 95% CI† | n | (%)* | 95% CI† | n | (%)* | 95% CI† |
| 60–64 | 1,202 | 23.4 | 21.2–25.7 | 660 | 13.3 | 11.0–16.0 | 1,862 | 20.5 | 18.7–22.4 |
| 65–69 | 1,166 | 22.9 | 20.6–25.4 | 717 | 16.3 | 13.6–19.5 | 1,883 | 20.7 | 18.8–22.6 |
| 70–74 | 994 | 24.5 | 21.7–27.5 | 650 | 17.2 | 14.2–20.8 | 1,644 | 21.7 | 19.4–24.2 |
| 75–79 | 654 | 29.9 | 26.2–33.8 | 441 | 18.6 | 14.9–23.0 | 1,095 | 25.6 | 22.7–28.7 |
| 80–84 | 363 | 25.2 | 20.9–30.1 | 284 | 15.4 | 10.8–21.6 | 647 | 20.9 | 17.4–24.8 |
| 85–90 | 135 | 29.4 | 23.6–35.9 | 86 | 12.1 | 6.5–21.4 | 221 | 22.7 | 18.6–27.4 |
| 90+ | 58 | 17.4 | 9.8–28.9 | 39 | 13.5 | 5.5–29.8 | 97 | 15.8 | 10.0–24.2 |
| Totals | 4,572 | 24.7 | 23.2–26.3 | 2,877 | 16.2 | 14.5–18.1 | 7,449 | 21.7 | 20.4–23.0 |
*(%) denotes prevalence of significant depressive symptoms
†95% CI denotes 95% confidence interval
Depression Correlates
The adjusted odds of depression were 58% higher in women compared to men (Table 2). Also, a monotonic inverse relationship was observed between education and depression prevalence. Stressful events indicating the presence of recent severe morbidity were each independently associated with an increased prevalence of depression with adjusted odds ratios (aORs) ranging between 1.5 and 2.3. The other five stressful situations were also independently associated with increased odds of depression with aORs ranging between 1.3 to 2.8.
Table 2.
Association of Personal Characteristics with Significant Depressive Symptoms as Assessed by a Score of 11 or Higher on the Geriatric Depression Scale
| n | Mean GDS score | aOR* | 95% CI† | ||
|---|---|---|---|---|---|
| Age in years | 60–64‡ | 1,862 | 7.12 | 1.00 | |
| 65–69 | 1,883 | 7.32 | 0.99 | 0.84–1.17 | |
| 70–74 | 1,644 | 7.37 | 1.02 | 0.85–1.23 | |
| 75–79 | 1,095 | 8.16 | 1.17 | 0.98–1.40 | |
| 80–84 | 647 | 7.79 | 0.90 | 0.68–1.19 | |
| 85–89 | 221 | 8.05 | 0.92 | 0.67–1.27 | |
| 90+ | 97 | 7.77 | 0.64 | 0.36–1.14 | |
| Gender§ | Men‡ | 2,877 | 6.57 | 1.00 | |
| Women | 4,572 | 8.04 | 1.58 | 1.40–1.80 | |
| Education (years)§ | Without education‡ | 1,353 | 9.15 | 1.00 | |
| Primary (1–6 years) | 4,170 | 7.71 | 0.74 | 0.63–0.88 | |
| Secondary (7–9 years) | 1,265 | 6.16 | 0.45 | 0.37–0.56 | |
| College (9–12) | 197 | 5.86 | 0.37 | 0.23–0.59 | |
| Higher (13+) | 464 | 4.71 | 0.33 | 0.23–0.47 | |
| Marital status§ | Married‡ | 4,419 | 7.08 | 1.00 | |
| Single | 452 | 7.12 | 0.97 | 0.76–1.24 | |
| Divorced/separated | 360 | 8.70 | 1.43 | 1.05–1.93 | |
| Widowed | 2,218 | 8.13 | 1.16 | 0.98–1.37 | |
| During the past year the person had: | |||||
| Serious illness§ | No‡ | 6,460 | 7.01 | 1.00 | |
| Yes | 989 | 10.51 | 2.28 | 1.95–2.67 | |
| Serious injury§ | No‡ | 7,014 | 7.33 | 1.00 | |
| Yes | 435 | 9.78 | 1.66 | 1.31–2.11 | |
| Increased trouble walking or with other daily activities§ | No‡ | 5,809 | 6.66 | 1.00 | |
| Yes | 1,640 | 10.35 | 2.18 | 1.89–2.51 | |
| Loss of vision or hearing§ | No‡ | 6,033 | 6.96 | 1.00 | |
| Yes | 1,416 | 9.68 | 1.48 | 1.24–1.76 | |
| Serious illness of one close | No‡ | 5,919 | 7.21 | 1.00 | |
| Yes | 1,530 | 8.50 | 1.27 | 1.08–1.49 | |
| Retirement§ | No‡ | 7,358 | 7.45 | 1.00 | |
| Yes | 91 | 9.05 | 1.97 | 1.13–3.44 | |
| Trouble with neighbors§ | No‡ | 7,222 | 7.36 | 1.00 | |
| Yes | 227 | 11.17 | 2.40 | 1.83–3.15 | |
| Financial problems§ | No‡ | 6,536 | 7.18 | 1.00 | |
| Yes | 913 | 9.55 | 1.54 | 1.25–1.88 | |
| Marital separation/divorce§ | No‡ | 7,380 | 7.42 | 1.00 | |
| Yes | 69 | 12.67 | 2.79 | 1.42–5.50 | |
*aOR denotes adjusted odds ratio
†95% CI denotes 95% confidence interval
‡Reference value
§Statistically significant values, p < .05
Odds ratios adjusted for all other variables in the table
Older adults with depression had an adjusted mean MMSE score 0.6 units lower (p < .05) than the corresponding adjusted score estimated for persons without depression (Table 3). Additionally, the adjusted cognitive impairment prevalence was also significantly higher in those with depression (18.9%) compared to those without depression (13.7%).
Table 3.
Cognitive Impairment in Participants with and without Significant Depressive Symptoms as Assessed by a Score of 11 or Higher on the Geriatric Depression Scale
| Without significant depressive symptoms (n = 5,751)* | With significant depressive symptoms (n = 1,439)* | |
|---|---|---|
| MMSE, mean | 26.3 (26.1–26.5) | 25.7 (25.5–25.9) |
| Cognitive impairment†, (%) | 13.7 (12.4–15.1) | 18.9 (16.6–21.4) |
*Two hundred fifty-nine original observations were not included in this analysis because of missing information on key variables
†Cognitive impairment present if MMSE was 23 or less
Estimates adjusted for age, sex, education, and stressful life events are presented in Table 2; 95% confidence intervals in parentheses. MMSE, Mini-Mental State Examination
As seen in Table 4, lower adjusted overall SF-36 scores (p < .05) were observed in those without depression but with recent severe morbidity (63.7), those with depression but no recent severe morbidity (49.6), and those with depression and recent severe morbidity (43.5) than in those with no depression or recent severe morbidity (71.9). Scores in most SF-36 subscales were similar in depressed participants with no recent severe morbidity and in non-depressed persons with recent severe morbidity. However, depressed elderly with no recent severe morbidity showed lower scores in the role limitations due to emotional problems and the emotional wellbeing subscales than those observed in non-depressed elderly with recent severe morbidity.
Table 4.
Overall and Subscale Sf-36 Mean Scores in IMSS-insured Elderly Residing in Mexico City According to the Presence of Significant Depressive Symptoms and Recent Severe Morbidity
| SF36 dimension | Without significant depressive symptoms (n = 5,873)* | With significant depressive symptoms (n = 1,478)* | ||
|---|---|---|---|---|
| …and no recent severe morbidity (n = 3,805) | …and recent severe morbidity (n = 2,068) | …and no recent severe morbidity (n = 533) | …and recent severe morbidity (n = 945) | |
| Physical functioning | 72.6 (71.2–73.9) | 61.7 (59.8–63.6) | 58.9 (55.7–62.2) | 48.9 (46.7–51.1) |
| Role limitations due to physical health | 72.2 (70.4–74.0) | 53.7 (51.0–56.5) | 42.1 (37.6–46.6) | 31.6 (29–34.2) |
| Role limitations due to emotional problems | 85.8 (84.4–87.2) | 76.3 (73.7–78.9) | 45.1 (39.9–50.4) | 41.5 (38.6–44.4) |
| Vitality | 69.9 (68.7–71.2) | 65.1 (64.0–66.2) | 47.1 (44.9–49.3) | 43.2 (41.7–44.8) |
| Emotional well being | 76.9 (75.7–78.1) | 73.8 (72.7–74.8) | 48.1 (46.1–50.1) | 46.0 (44.5–47.5) |
| Social functioning | 85.3 (84.2–86.5) | 79.2 (77.9–80.6) | 65.3 (63.1–67.5) | 58.8 (56.5–61.1) |
| Bodily pain | 77.3 (76.2–78.4) | 66.7 (65.0–68.5) | 58.5 (56–61) | 49.7 (47.5–51.9) |
| General health | 57.4 (56.4–58.4) | 50.0 (49.1–50.9) | 40.1 (38.2–42.1) | 34.7 (33.5–35.9) |
| Overall SF-36 Score | 71.9 (71.1–72.7) | 63.7 (62.5–64.9) | 49.6 (48.2–51.1) | 43.5 (42.3–44.8) |
*Ninety-eight original observations were not included in these analyses due to missing data
Higher scores indicate better functioning. Mean scores adjusted for age, sex, education, serious illness to someone close, retirement, trouble with neighbors, financial problems, and marital separation/divorce; 95% confidence intervals in parentheses
The adjusted percentage of IMSS elderly with neither depression nor recent severe morbidity who visited any healthcare institution during the 6 months previous to the interview for any health problem was 79.3% (Table 5). Compared to this group, persons with depression and no recent severe morbidity had a 64% increase in their adjusted odds of utilization, similar to the increase in utilization seen in persons with recent severe morbidity with or without depression. Similar patterns were found for use of any IMSS facility, of an IMSS family medicine unit, and of an IMSS hospital, for any health problem
Table 5.
Association of Healthcare Use with Presence of Significant Depressive Symptoms with and without Recent Severe Morbidity
| Utilization rates (%) | Adjusted utilization odds ratios (aOR)* | ||||||
|---|---|---|---|---|---|---|---|
| Without depression (n = 5,836)† | With depression (n = 1,460)† | Without depression | With depression | ||||
| And… | |||||||
| No recent severe morbidity (n = 3,788) | Recent severe morbidity (n = 2,048) | No recent severe morbidity (n = 527) | Recent severe morbidity (n = 933) | Recent severe morbidity (n = 2,048) | No recent severe morbidity (n = 527) | Recent severe morbidity (n = 933) | |
| During the past 6 months sought healthcare for any reason at any health care… | |||||||
| Institution | 79.3 (77.7–80.7) | 88.9 (87.1–90.5) | 86.3 (83.1–88.9) | 90.7 (88.4–92.6) | 2.1 (1.8–2.5) | 1.6 (1.3–2.1) | 2.6 (2–3.3) |
| IMSS facility | 66.2 (64.2–68.1) | 73.8 (71.3–76.2) | 72.3 (68.1–76.2) | 78.5 (75.6–81.1) | 1.4 (1.3–1.7) | 1.3 (1.1–1.7) | 1.9 (1.6–2.2) |
| IMSS family medicine clinic‡ | 64.4 (62.5–66.3) | 70.8 (68.0–73.4) | 70.1 (65.8–74.1) | 74.6 (71.8–77.2) | 1.3 (1.2–1.5) | 1.3 (1.1–1.6) | 1.6 (1.4–1.9) |
| IMSS hospital‡ | 17.6 (16.0–19.2) | 29.3 (26.8–32.0) | 21.5 (17.5–26.1) | 36.3 (32.6–40.1) | 1.9 (1.9–2.2) | 1.3 (1.0–1.7) | 2.7 (2.2–3.2) |
| During the past 6 months sought healthcare because felt nervous or worried at any healthcare… | |||||||
| Institution | 5.7 (4.9–6.6) | 7.7 (6.4–9.3) | 15.5 (12.5–19.0) | 17.2 (14.4–20.3) | 1.4 (1.1–1.8) | 3.1 (2.4–3.9) | 3.4 (2.7–4.5) |
| IMSS facility | 3.5 (2.9–4.3) | 4.8 (3.7–6.1) | 10.1 (7.7–13.1) | 10.6 (8.5–13.2) | 1.4 (1.0–1.9) | 3.1 (2.3–4.1) | 3.3 (2.4–4.4) |
| IMSS family medicine clinic‡ | 3.2 (2.6–3.9) | 4.3 (3.2–5.6) | 9.1 (6.8–12.2) | 9.3 (7.5–11.5) | 1.3 (1–1.9) | 3.0 (2.2–4.2) | 3.1 (2.4–4.0) |
| IMSS hospital‡ | 0.3 (.13–.55) | 0.5 (.24–.95) | 0.7 (.26–2.0) | 1.8 (.97–3.3) | 1.8 (.7–4.5) | 2.7 (1.0–7.5) | 6.8 (3–15.9) |
*Reference: Participants without significant depressive symptoms and no recent severe morbidity
†One hundred fifty-three observations were not included in this analysis due to missing information on key variables
‡These events are not mutually exclusive
Estimates adjusted for age, sex, education, serious illness of someone close, retirement, trouble with neighbors, financial problems, and marital separation/divorce; 95% confidence intervals in parentheses
Healthcare utilization associated with feeling nervous or worried represented a small fraction of all healthcare utilization. Persons with depression and no recent severe morbidity showed, in general, similar utilization rates to those found in persons with depression and recent severe morbidity, with aORs generally close to 3, regardless of the type of healthcare facility attended.
DISCUSSION
We present the prevalence of depression and its correlates in a large community sample of elderly insured by the largest healthcare provider in Mexico City. Results, however, must be interpreted in the light of several limitations. First, perhaps the most important limitation of this study is that we were only able to interview a low fraction of those listed in the selected physician offices, in part as a result of a lack of active update in the patient lists used to identify study participants. Census data indicate that we under-sampled city residents with the oldest ages and higher education. We tried to overcome the problem of sample representativeness by calculating selection probabilities specific by age, gender, and education, and we used them as sample weights in all analyses presented here. Additionally we used bootstrapping techniques, considering the sample design, to obtain more valid estimates of standard errors in all statistical analyses. We believe that these procedures allow us to make valid inferences to the non-institutionalized elderly population insured by IMSS residing in Mexico City.
Second, depression prevalence was determined using the 30-item GDS, a scale that assesses depressive symptoms without regard of the 4-week timeframe included in the DSM-IV standard and that, consequently, is prone to exhibit a relatively high GDS false-positive rate39. Several validation studies have reported lower GDS specificity than sensitivity values for detecting major depression27–31. We found that one in eight IMSS insured elderly have depression (21.7% overall). Correcting this figure for the average GDS sensitivity and specificity values reported in the reviewed validation studies, we estimate the prevalence of major depression in our target population at 13.2% (6.4% in men and 16.9% in women). The 30-item GDS prevalence figures by gender were similar to those reported in elderly Hispanics in New Mexico using the 15-item GDS40. Alegría et al. recently studied the prevalence of mental illness in several Latino groups, and it is interesting that lifetime prevalence of major depression among Mexican immigrants was lower than other Latino groups (11.8%), unfortunately no specific data for older persons were reported41. Our corrected prevalence figures are similar to those found for persons aged 60 and older in a national community survey in Mexico, using a different screening instrument based on DSM-IV criteria19.
Third, we analyzed the independent association among significant depressive symptoms and socio-demographic factors, stressful events, cognitive impairment, health-related quality of life, and healthcare use. Such cross-sectional associations are subject to temporal ambiguity. Our study will follow up over time all identified participants with depression and a randomly selected sample of surveyed persons without initial depression. This will allow us to confirm or discard the cross-sectional associations found.
Fourth, the association between depression in the elderly with health-related quality of life and healthcare use may be confounded by the presence of co-morbidities such as diabetes, hypertension, cancer, and cardiovascular conditions. We controlled for co-morbidities only through the variable “recent severe morbidity,” a composite of recent severe health problems and increasing disability. Chronic diseases diagnosed by a doctor were only measured in 39% of participants, which will be followed up overtime. In this sub-sample, we did similar analyses to those presented for the entire sample and found that the addition of terms for six chronic conditions reduced only slightly (less than 15%) the associations between depression and health-related quality of life and healthcare use presented here.
Acknowledging the above limitations, our study provides important findings that contribute to what is already known about depression in the elderly worldwide. Depression was more frequent in women, and an inverse relationship between education and depression prevalence was observed42,43. In addition, we found a higher depression prevalence in participants reporting stressful events, as has also been found in other studies32,44,45.
Cognitive impairment was also more common among participants with depression than in persons without depression. As mentioned by others46,47, depression could be a risk factor for cognitive decline and dementia. However, the relationship between depression and dementia could be more complex. Thus, depression could be an early symptom of undiagnosed dementia or share common risk factors with dementia48–49.
Depression has an independent negative impact on health-related quality of life3,7–8. We found lower health-related quality of life in participants with depression, regardless of the presence of recent severe morbidity, than in those without depression or recent severe morbidity. An adjusted SF-36 subscale score indicating impairment among depressed participants without recent severe morbidity was similar to those observed in persons with recent severe morbidity but no depression. The exception was in subscales measuring mental health, where score reductions were higher in the group with depression but no recent severe morbidity.
Both cross-sectional and longitudinal studies have also documented that depression increases healthcare utilization3,12. We found that participants with depression and no recent severe morbidity showed higher increases in utilization rates, both for any reason and for emotional problems, than to those observed in persons who had recent severe morbidity but no depression. Indeed, depression independently increased utilization rates in a similar fashion in those with and without recent severe morbidity. Additionally, consistent with health services research in other countries3,50, persons with depression tended to use IMSS family medicine units more frequently than hospitals.
In conclusion, our study provides useful information on the prevalence of depression among older adults and its correlates for the urban population in a developing country. Even in developing countries, the benefits of elderly depression treatment in primary-care units may more than offset its associated costs. Treatment may lower utilization rates and eventually free up resources that could be applied to improving the functional status of older adults, improved care for medical conditions that accompany depression51, and may even extend life52. In addition, offering treatment for depression may be instrumental in delaying the onset or slowing down the rate of cognitive decline48. Therefore, the design and implementation of systematic training of primary-care physicians on the detection and management of elderly patients with depression should be granted high priority in developing countries. Primary care teams, including a depression care manager, primary care doctor, and psychiatrist, seem to have better results than the usual primary physician-centred care14. Finally, it is also important to continue research in this area and to reinforce primary-level healthcare strategies to confront upcoming challenges.
Acknowledgements
This project was supported by grants from CONACyT (México) 2002-CO1-6868, Mexican Institute of Social Security (IMSS 2002-382), and NIH-FIRCA R03 TW005888.
Dr. Wagner was funded through grant DA 17796 from the National Institute on Drug Abuse and P60-MD002217 from the National Center on Minority Health and Health Disparities.
Conflict of Interest None disclosed.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, eds. In: Global Burden of Disease and Risk Factors. Washington DC: Oxford University Press and The World Bank: 2006:85–6.
- 2.Khandelwai S. Conquering Depression. Geneva: World Health Organization; 2001.
- 3.Herrman H, Patrick DL, Diehr P, et al. Longitudinal investigation of depression outcomes in primary care in six countries: the LIDO study. Functional status, health services use and treatment of people with depressive symptoms. Psychol Med. 2002;32:889–902. [DOI] [PubMed]
- 4.Lebowitz B, Pearson J, Scheneider L, et al. Diagnosis and treatment of depression in late life: Consensus Statement update. JAMA. 1997;278(14)1186–90. [DOI] [PubMed]
- 5.Engedal K. Mortality in the elderly-a 3-year follow-up of an elderly community sample. Int J Geriatr Psychiat. 1996;11:467–71. [DOI]
- 6.Shah A, Phongsathom V, Bielawska C, Katona C. Screening for depression among geriatric inpatients with short versions of the geriatric depression scale. Int J Geriatr Psychiat. 1994;11:915–8. [DOI]
- 7.Wells KB, Stewart A, Hays RD. The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA. 1989;262:914–9. [DOI] [PubMed]
- 8.Hays RD, Wells KB, Sherbourne CD. Functioning and well-being outcomes of depressed with depression compared with chronic general medical illnesses. Arch Gen Psychiatry. 1995;52:11–9. [DOI] [PubMed]
- 9.Gallo JJ, Bogner HR, Morales KH, Ford DE. Patient ethnicity and the identification and active management of depression in late life. Arch Int Med. 2005;165(17)1962–8. [DOI] [PMC free article] [PubMed]
- 10.Bogner HR, Ford DE, Gallo JJ. The role of cardiovascular disease in the identification and management of depression by primary care physicians. Am J Geriat Psychiat. 2006;14(1)71–8. [DOI] [PMC free article] [PubMed]
- 11.Beekman AT, Penninx BW, Deeg DJ, de Beurs E, Geerlings SW, van Tilburg W. The impact of depression on the well-being, disability and use services in older adults: a longitudinal perspective. Acta Psychiatr Scand. 2002;105:20–7. [DOI] [PubMed]
- 12.Rowan PJ, Davidson K, Campbell JA, Dobrez DG, MacLean DR. Depressive symptoms predict medical care utilization in a population-based sample. Psychol Med. 2002;32:903–8. [DOI] [PubMed]
- 13.Koopmans GT, Donker MC, Rutten FH. Common mental disorders and use of general health: a review of the literature on population-based studies. Acta Psychiatr Scand. 2005;111:341–50. [DOI] [PubMed]
- 14.Hunkeler E, Katon W, Tang L, et al. Long term outcomes from the IMPACT randomised trail for depressed elderly patients in primary care. BMJ. 2006;332:259–63. [DOI] [PMC free article] [PubMed]
- 15.Gallo JJ, Lebowitz BD. The epidemiology of common late-life mental disorders in the community: Themes for the new century. Psychiat Serv. 1999;50:1158–68. [DOI] [PubMed]
- 16.Wagner FA, Gallo JJ, Delva J. Depression in late life: A hidden public health for Mexico? Salud Pública Mex. 1999;41:189–202. [DOI] [PubMed]
- 17.Medina-Mora ME, Rascón ML, Tapia R, et al. Trastornos emocionales en población urbana mexicana: resultados de un estudio nacional. An Inst Mex Psiquiatr. 1992;3:48–55.
- 18.Caraveo J, Martínez N, Rivera B, Polo A. Prevalencia en la vida de episodios depresivos y utilización de servicios especializados. Salud Mental. 1997;20:15–23.
- 19.Belló M, Puentes-Rosas E, Medina-Mora ME, Lozano R. Salud Publica Mex. 2005;47(Supl 1)4–11. [PubMed]
- 20.Romero LJ, Lindeman RD, Hundley R, et al. Outcome of recruitment and report on participation rate in the New Mexico Elder Health Survey. Ethn Dis. 1998;8(3)350–9. [PubMed]
- 21.Instituto Nacional de Estadística Geografía e Informática de Mexico. XII Censo General de Población y Vivienda 2000. Available at: http://www.inegi.gob.mx/est/contenidos/espanol/proyectos/censos/cpv2000/muestracensal/default.asp?s=est&c=11203. Accessed August 1, 2008.
- 22.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: preliminary report. J Psychiatr Res. 1983;17:37–49. [DOI] [PubMed]
- 23.Sharp L, Lipsky M. Screening for depression across the lifespan: a review of measures foruse in primary care settings. Am Fam Physician. 2002;66:1001–8. [PubMed]
- 24.Rapp S, Parisi S, Walsh D, Wallace C. Detecting depression in elderly medical inpatients. J Consult Clin Psychol. 1988;56:509–13. [DOI] [PubMed]
- 25.Boult C, Boult L, Morishita L, Dowd B, Kane R, Urdangain C. A randomized clinical trial of outpatient geriatric evaluation and management. J Am Geriatr Soc. 2001;49:351–9. [DOI] [PubMed]
- 26.McDowell I, Newell C. Depression. In: McDowell I, Newell C, eds. Measuring Health. A Guide to Rating Scales and Questionnaires. 2nd ed. USA: Oxford University Press: 1996:238–86.
- 27.Fernández-San Martín MI, Andrade C, Molina J, et al. Validation of the Spanish version of the Geriatric Depression Scale (GDS) in primary care. Int J Geriatr Psychiat. 2002;17:279–87. [DOI] [PubMed]
- 28.Montorio I, Izal M. The Geriatric Depression Scale: a review of its development and utility. Int Psychogeriatr. 1996;8:103–12. [DOI] [PubMed]
- 29.Lyness J, Noel TK, Cox C, King D, Conwell Y, Caine E. Screening for depression in elderly primary care patients: a comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Arch Int Med. 1997;157:449–54. [DOI] [PubMed]
- 30.Reyes-Frausto S. Population ageing in the Mexican Institute of Social Security: Health Policy and Economic Implications. Instituto Mexicano del Seguro Social. Fundación Mexicana para la Salud. México: FUNSALUD; 2001.
- 31.Salamero M, Marcos T. Factor study of the Geriatric Depression Scale. Acta Psychiatr Scand. 1992;86:283–6. [DOI] [PubMed]
- 32.Kendler KS, Karkowski L, Prescott C. Causal Relationship between stressful events and the onset of major depression. Am J Psychiatry. 1999;156:837–41. [DOI] [PubMed]
- 33.Reyes de Beaman S, Beaman P, García-Peña C, et al. Validation of a modified version of the Mini-Mental State Examination (MMSE) in Spanish. Aging Neuropsychol Cognition. 2004;11:1–11.
- 34.Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [DOI] [PubMed]
- 35.Zuñiga MA, Carrillo-Jimenez GT, Fox PJ, Gandek B, Medina-Moreno MR. Evaluación del estado de salud con la Encuesta SF-36: resultados preliminares. Salud Publica Mex. 1999;41:110–18. [PubMed]
- 36.Hays RD, Sherbourne CD. RAND 36-Item health Survey 1.0 Scoring Manual. Santa Monica, CA: The RAND Corporation; 1992.
- 37.Lehtonen R, Pahkinen E. Practical Methods for Design and Analysis of Complex Surveys (Statistics in Practice). 2nd Ed. West Sussex: John Wiley & Sons LTD; 2004.
- 38.Stata Corporation: Stata statistical Software. Release 9.0. Reference Manual. Stata press, Texas, College Station, 2005.
- 39.Almeida O, Almeida Sh. Short versions of the Geriatric Depression Scale: A study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int J Geriatr Psychiatry. 1999;14:858–65. [DOI] [PubMed]
- 40.Romero L, Ortiz I, Finley R, Wayne S, Linderman R. Prevalence of depressive symptoms in New Mexico Hispanic and non-Hispanic white elderly. Ethnicity Dis. 2005; 15: [PubMed]
- 41.Alegría M, Canino G, Shrout P, et al. Prevalence of mental illness in inmigrant and non-inmigrant US Latino groups. Am J Psychiatry. 2008;165:359–69. [DOI] [PMC free article] [PubMed]
- 42.Urbina Torija JR, Flores Mayor JM, García Salazar MP, Torres Buisán L, Torrubias Fernández RM. [Depressive symptoms in the elderly. Prevalence and associated factors]. Gac Sanit. 2007;21(1)37–42, Jan-Feb. [DOI] [PubMed]
- 43.Lépine JP, Bouchez S. Epidemiology of depression in the elderly. Int Clin Psychopharmacol. 1998;13(Suppl 5)S7–12, Sep. [DOI] [PubMed]
- 44.Zhang AY, Yu LC, Yuan J, Tong Z, Yang C, Foreman SE. Family and cultural correlates of depression among Chinese elderly. Int J Soc Psychiatry. 1997;43(3)199–212, Autumn. [DOI] [PubMed]
- 45.Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand. 2006;113(5)372–87, May. [DOI] [PubMed]
- 46.Ganguli M, Du Y, Dodge H, Ratcliff G, Chang CH. Depressive symptoms and cognitive decline in later life. A Prospective Epidemiological Study. Arch Gen Psychiatry. 2006;63:153–60. [DOI] [PubMed]
- 47.Geerlings MI, Schoevers RA, Beekman AT, et al. Depression and risk of cognitive decline and Alzheimer’s disease. Results of two prospective community-based studies in The Netherlands. Br J Psychiatry. 2000;176:568–75. [DOI] [PubMed]
- 48.Steffens D, Otey E, Alexopoulos G, et al. Perspectives on Depression, Mild Cognitive Impairment and Cognitive Decline. Arch Gen Psychiat. 2006;63:130–8. [DOI] [PubMed]
- 49.Bogner HR, Bruce ML, Reynolds CF 3rd, et al. The effects of memory, attention, and executive dysfunction on outcomes of depression in a primary care intervention trial: the PROSPECT study. Int J Geriatr Psychiatry. 2007;22:922–9. [DOI] [PMC free article] [PubMed]
- 50.Marino S, Gallo JJ, Ford D, Anthony JC. Filters on the pathway to mental health care, I. Incident mental disorders. Psychol Med. 1995;25:1135–48. [DOI] [PubMed]
- 51.Bogner HR, Cary MS, Bruce ML, et al. The role of medical comorbidity in outcome of major depression in primary care: the PROSPECT study. Am J Geriatr Psychiatry. 2005;13:861–8. [DOI] [PMC free article] [PubMed]
- 52.Bogner HR, Morales KH, Post EP, Bruce ML. Diabetes, depression, and death: a randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care. 2007;30:3005–10. [DOI] [PMC free article] [PubMed]


