Abstract
This study examined predictors of readmission for a sample of 522 adolescents enrolled in Medicaid and admitted to three inpatient psychiatric hospitals in Maryland. Comprehensive data on clinical, treatment, and health care system characteristics were collected from archival sources (medical records, Medicaid claims, and Area Resource File). Predictors of readmission were examined with bivariate (Kaplan Meier) and multivariate (Cox Regression) survival techniques. One year readmission rates were 38% with the majority occurring within 3 months after discharge. Adolescent demographic (age and gender), clinical (severity of symptoms, comorbidity, suicidality) and family characteristics (level of family risk) were associated with readmission. However, treatment factors including type of aftercare, post-discharge living environment, medication noncompliance, and hospital provider were among the strongest predictors of readmission. Study findings underscore the importance of careful discharge planning and linkage to appropriate aftercare. The differing rates of readmission across hospitals also suggest that organizational level factors may play a vital role in determining treatment outcomes.
Keywords: inpatient psychiatric hospitalization, adolescents, readmission
It is estimated that 24% to 37% of youths will be readmitted to a psychiatric hospital within one year after discharge, and latest data suggest that rates of readmission are increasing despite cost-containment efforts and emphasis on community-based treatment alternatives (Blader, 2004; Fontanella, Zuravin, & Burry, 2006; Pavkov, Goerge, Lee, & Howard, 1994; Soloman, Evans, & Delaney, 1993). In the United States, inpatient services account for about 33% ($3.9 billion) of the total mental health expenditures for children and adolescents; across age groups adolescents are the highest users of inpatient services (Ringel & Sturm, 2001).
Some researchers speculate that the increased readmission rates can be attributed to premature discharges resulting from shortened lengths of stay (Appley, Desai, Luchins, Gibbons, & Hedeker, 1993; Lien, 2002; Wickizer, Lessler, & Boyd-Wickizer, 1999). In fact, studies on Medicaid populations (Callahan, Shepard, Beinecke, Larson, & Cavanaugh, 1995; Dickey, Normand, Norton, Rupp, & Azeni, 2001; Saunders & Heflinger, 2003) have shown increases in readmission rates resulting from managed care imposed restrictions on length of stay. For example, in Massachusetts, Callahan and colleagues (1995) found that 30-day readmission rates for children and adolescents increased from 7.5% to 10.1% after the implementation of managed care. Similarly, in Tennessee 30-days readmission rates increased from 9.2% in 1995 to 12.2% in 2000 for school aged children enrolled in TennCare (Saunders & Heflinger, 2003). Others contend that higher readmission rates stem from inadequate continuity of care and lack of available alternative community-based services (Lyons et al., 1997, 1998a). Nevertheless, the factors most associated with readmission of children remain poorly understood. As hospitals continue to adapt to a changing health care environment where resources are limited and pressures to reduce lengths of stay are great, more information is needed about effective strategies to reduce readmissions. Understanding factors that contribute to readmission is essential not only for continued quality improvement, but also for the development of targeted prevention programs aimed at those at greatest risk.
The few existing studies (Arnold et al., 2003; Blader, 2004; Romansky, Lyons, Lehner, & West, 2003) that have examined predictors of readmission among children and adolescents vary considerably with regard to design (retrospective versus prospective), data source (hospital records versus administrative data), operational definition of readmission (to the same hospital versus any hospital in the state or managed care network), population (publicly insured versus privately insured), and type of predictor variables examined. Consequently, methodological differences across studies make it difficult to integrate findings or draw definitive conclusions about factors that lead to readmissions. Moreover, most studies have focused on a limited range of variables, primarily clinical and demographics, neither of which is amenable to intervention. Yet, review of the research literature (see Klinkenberg & Calsyn, 1996) suggests that multiple risk factors within several domains are associated with readmission. To advance the literature, comprehensive, multi-level models are needed to assess the contributions of variables from multiple systems.
Using comprehensive data on adolescents who were enrolled in Medicaid and admitted to three psychiatric hospitals, the primary aim of the study was to identify which individual, family, treatment, and health care system characteristics predict readmission. The study focuses specifically on publicly insured youths because research suggests that Medicaid populations and adolescents have higher rates of inpatient utilization compared to privately insured youth and adults (Ringel & Sturm, 2001). In general, Medicaid populations are considered a high-risk group because of their higher level of mental health need and exposure to multiple risk factors (e.g., low socioeconomic status, chronic family stress); therefore, their inpatient utilization patterns may differ from non-Medicaid populations (Dalton, Moseley, & McDermott, 1997; Pottick, McAlpine, & Andelman, 2000).
The study builds upon prior research by making several methodological improvements. First, I assess the simultaneous influence of risk factors across multiple systems (child, family, treatment, and health care). Second, I examine additional variables that previous researchers have largely ignored such as the effect of treatment (discharge planning, linkage to aftercare services), organizational factors (facility ownership), and health care system characteristics (availability of community resources). Third, I merged data from multiple data sources, which enhances the validity of the analyses. Previous researchers have limited the type and quantity of information collected because they used single data sources. Fourth, I used a large sample from three hospitals; most prior treatment outcome studies have employed small samples from one hospital. Finally, few have considered readmissions to facilities other than the index hospital, which may underestimate the rate of readmission and confound study findings.
Predictors of Readmission
Review of the empirical studies show a wide range of predictors and correlates of readmission. These predictor variables can be categorized into four domains involving characteristics of the child/adolescent, family, treatment and health care system.
Child/adolescent characteristics
Child and adolescent characteristics examined include: demographic (age, race/ethnicity, and gender) and clinical factors (diagnoses, severity of symptoms, comorbidity, and risk factors). Findings from research that have examined demographic variables are contradictory. Some investigators (e.g., Arnold et al., 2003; Foster, 1999; Pavkov, Goerge, & Lee, 1997) have found an association between child's age and readmission, while others (e.g., Blader, 2004; Cornsweet-Barber & Evans, 1999; Romansky et al., 2003) have not. Neither race nor gender has been found to consistently predict readmission (Arnold et al., 2003; Blader, 2004; Foster, 1999; Pavkov et al., 1997; Romansky et al., 2003).
The strong association between various clinical factors and readmission, particularly diagnosis and severity of symptoms, is well documented in the research literature; youths diagnosed with affective, behavioral disorders and/or psychoses with more severe symptoms are at greater risk for readmission (Arnold et al., 2003; Blader, 2004; Foster, 1999; Lyons et al., 1997; Pavkov et al., 1997). The influence of other clinical factors such as suicidal and homicidal behavior, history of abuse, and comorbidity is less clear and has not been consistently examined by researchers. For example, some studies (Cornsweet-Barber & Evans, 1999) have found that suicidal behavior (number of prior suicide attempts) were positively associated with readmission, whereas others have reported no associations (Arnold et al., 2003) or negative findings (Foster, 1999; Lyons et al., 1997). No significant associations were found between level of dangerousness (assaultive behavior) and readmission; only one study found that history of physical abuse increased likelihood of multiple inpatient hospitalizations (Cornsweet-Barber, Rosenblatt, Harris, & Attkisson, 1992). Of the studies that examined comorbidity (e.g., psychiatric, substance abuse, developmental delay/mental retardation), only one found an association with readmission (Arnold et al., 2003; Cornsweet-Barber et al., 1992; Lyons et al., 1997; Romansky et al., 2003). Romansky and colleagues (2003) found that children in state custody who had a co-occurring learning disability or serious development delay were more likely to be readmitted than those youths without such problems. However, the investigators failed to control for other factors in the analyses.
Family characteristics
Few investigators (Blader, 2004; Cornsweet-Barber & Evans, 1999; Foster, 1999) have examined the relationship between family factors and readmission, and findings are difficult to compare due to differences in the types of variables examined and operational definitions. Taken together, however, these studies suggest that youths who come from poorly functioning, high risk families characterized by parental history of mental illness, substance abuse, suicide, and/or criminal behavior are at greater risk for readmission. Other family factors associated with readmission include harsh parenting practices, high degree of caregiver burden, and low level of parental involvement in treatment (Blader, 2004; Foster, 1999).
Treatment characteristics
Treatment characteristics that have been examined as potential predictors of readmission include: hospital-related factors (e.g., length of stay, organizational and provider characteristics); service history (e.g., prior hospitalizations, placement history, and noncompliance with treatment); post-discharge environment and aftercare. The most consistent findings involve service history factors. Studies indicate that prior hospitalizations (Heflinger, Simpkins, & Foster, 2002; Pottick, Hansell, Gutterman, & Raskin-White, 1995) and/or noncompliance (Perkins, 2002) with treatment are strong predictors of subsequent hospitalization. There is also some limited evidence (Rosenau & Linder, 2003) that organizational characteristics (e.g., hospital ownership, bed capacity, staffing ratios) are associated with readmission.
Findings on length of stay are less consistent. Some studies have found shorter (Wickizer, Lessler, & Boyd-Wickizer, 1999) or longer lengths of stays (Pavkov et al., 1997) were associated with readmission; others (Blader, 2004; Lyons et al., 1997) have found no such association. Research on the influence of aftercare and post-discharge environment on readmission is limited, and findings from the few existing studies are inconsistent (Blader, 2004; Foster, 1999). However, prior outcome studies on inpatient care (cf. for review Blotcky et al., 1984; Daniel, Goldston, Harris, Kelly, & Palmes, 2004; Pfeiffer, & Strzelecki, 1990) have emphasized the importance of these variables in predicting positive outcomes following hospitalization and reducing recidivism.
Health care system characteristics
Past research (cf. for review Phillips, Morrison, Andersen, & Aday, 1998) and theory on mental health service use (Aday & Anderson, 1974; Andersen, 1995) suggest that access to mental health care and services utilization is influenced by a number of health care system characteristics including the availability of services, health care policies, and other community-level factors (e.g., urban-rural location). However, only two sets of investigators have examined the relationship between readmission and community-level variables. In a study of children and adolescents readmitted to state psychiatric hospitals in Illinois, Pavkov and colleagues (1997), found that youths from more affluent urban communities were less likely to be readmitted than those from lower SES communities. Romansky and colleagues (2003) found similar results.
Study Hypotheses
Based on prior research, it was hypothesized that the risk of readmission would increase with severity of illness and level of need. That is, it was expected that youths with more severe clinical profiles (e.g., symptoms, comorbidities, risk behaviors), higher levels of family risk, prior psychiatric hospitalizations, and histories of noncompliance would be more likely to be readmitted than those youths with less severe clinical profiles. In addition, it was hypothesized that rates of readmission would vary across hospital providers and that greater risk for readmission would associated with shorter lengths of stay and discharge to lower levels of aftercare. Although findings on length of stay are mixed, it was expected that readmission risk would be greater for youths with shorter length of stay, as the more recent studies (e.g., Appley et al., 1993; Wickizer et al., 1999) have found that reductions in lengths of stay has lead to increased readmission rates. The prediction about aftercare is based on evidence (Heflinger et al., 2002) which suggests that youths placed in more restrictive environments (e.g., residential treatment) are less likely to be hospitalized than those placed in less restrictive environments (e.g., foster care, group home). Finally, based on prior studies it was expected that availability of community providers would be significantly associated with readmission, even after controlling for demographic and clinical factors.
Methods
Overview of Design
This study uses a retrospective cohort design. Research participants included all Medicaid eligible adolescents consecutively admitted to three major free-standing private psychiatric hospitals. Adolescents were followed for a fixed one year period after their index admission to track readmission. Readmission was defined as an inpatient hospitalization (excluding same day transfers) to any Maryland psychiatric facility (including all state, general, and private hospitals) occurring within one year of the adolescent's index admission. Data were collected from multiple archival sources.
Participants and Sampling Plan
Selection of the sample involved a two-stage process. First, eligible adolescents were identified from the total population of adolescents (N=1,595) admitted to the hospitals during the study period. These hospitals (two non-profit and one for-profit) were selected because they are the major psychiatric facilities serving adolescents in Maryland, accounting for almost half of the total adolescent beds (N = 96 of 202) and 72% of the total adolescent private psychiatric beds in the state. Eligibility for inclusion in the sample was based on four selection criteria: (1) admitted to the three private psychiatric hospitals between July 1, 1997 and June 30, 1998; (2) covered by Medicaid at the time of admission; (3) aged 11 to 17.99; and 4) a resident of Maryland. A total of 545 adolescents met these criteria. Second, hospital records were reviewed and adolescents were excluded if they were (a) discharged against medical advice (n = 17), (b) eloped from the hospital (n = 5), or (c) case records were missing (n = 1). Using these criteria, 23 cases were excluded, leaving a final sample of 522. Sample characteristics are described in Table 1.
Table 1.
Characteristics associated with readmission of adolescents to inpatient care at 1, 3, and 12 months
| Total (%)
(N = 522) |
Readmitted (%)
(N =198) |
||||
|---|---|---|---|---|---|
| 1 month | 3 months | 12 months | p-value | ||
| Adolescent characteristics | |||||
| Age at admission (years) | .013 | ||||
| 11-13 | 44.6 | 9.9 | 22.3 | 44.6 | |
| 14-17 | 55.4 | 13.8 | 21.1 | 32.5 | |
| Race/ethnicity | .126 | ||||
| White | 46.4 | 13.2 | 24.0 | 41.3 | |
| Non-white a | 53.6 | 11.1 | 19.6 | 35.0 | |
| Gender | .640 | ||||
| Females | 53.8 | 13.2 | 19.6 | 39.0 | |
| Males | 46.2 | 10.8 | 24.1 | 37.0 | |
| Neuropsychiatric disturbance | <.001 | ||||
| No disturbance | 69.3 | 8.6 | 17.7 | 31.8 | |
| Any disturbance | 30.7 | 20.0 | 30.6 | 51.9 | |
| Emotional disturbance | .055 | ||||
| Mild disturbance | 8.6 | 6.7 | 15.6 | 28.9 | |
| Moderate disturbance | 68.4 | 10.6 | 19.6 | 36.4 | |
| Severe disturbance | 23.0 | 18.3 | 30.0 | 45.8 | |
| Behavioral disturbance | <.001 | ||||
| Mild disturbance | 21.3 | 7.2 | 11.7 | 22.5 | |
| Moderate disturbance | 36.2 | 7.9 | 16.4 | 36.0 | |
| Severe disturbance | 42.5 | 18.0 | 31.1 | 47.3 | |
| Substance abuse problem | .004 | ||||
| Mild problem | 82.4 | 12.6 | 23.5 | 40.9 | |
| Severe problem | 17.6 | 9.8 | 13.0 | 23.9 | |
| Mental retardation | <.001 | ||||
| No | 89.7 | 10.9 | 19.2 | 35.7 | |
| Yes | 10.3 | 22.2 | 42.6 | 57.4 | |
| Suicidality | .217 | ||||
| No history of suicidal behavior | 15.1 | 5.1 | 15.2 | 38.0 | |
| History of suicidal behavior | 17.1 | 15.7 | 25.8 | 46.1 | |
| Recent suicidal behavior | 67.8 | 12.7 | 22.0 | 35.9 | |
| Dangerousness | .024 | ||||
| No history of violent behavior | 10.7 | 5.4 | 12.5 | 26.8 | |
| History of violent behavior | 20.3 | 8.5 | 14.2 | 31.1 | |
| Recent violent behavior | 69.0 | 14.2 | 25.3 | 41.7 | |
| Family characteristics | |||||
| Family risk index | .001 | ||||
| Low risk | 18.8 | 7.1 | 14.3 | 24.5 | |
| Medium risk | 71.1 | 13.5 | 22.9 | 39.1 | |
| High risk | 10.2 | 11.3 | 26.4 | 54.7 | |
| Treatment characteristics | |||||
| Prior hospitalizations | <.001 | ||||
| No | 62.1 | 8.3 | 16.4 | 31.2 | |
| Yes | 37.9 | 18.2 | 30.3 | 49.0 | |
| Med Noncompliance | .039 | ||||
| No | 81.6 | 10.8 | 20.0 | 35.9 | |
| Yes | 18.4 | 17.7 | 29.2 | 46.9 | |
| Hospital provider | .002 | ||||
| Hospital A | 47.5 | 11.7 | 23.4 | 41.1 | |
| Hospital B | 33.1 | 11.0 | 16.2 | 27.8 | |
| Hospital C | 19.3 | 14.9 | 26.7 | 47.5 | |
| Length of stay | .361 | ||||
| 1-5 days | 20.7 | 10.2 | 17.6 | 32.4 | |
| 6-8 days | 29.7 | 11.0 | 23.9 | 40.0 | |
| 9-17 days | 25.1 | 16.0 | 22.1 | 42.8 | |
| >18 days | 24.5 | 10.9 | 21.9 | 35.2 | |
| Aftercare received 30 days post-discharge | <.001 | ||||
| No services | 14.0 | 1.4 | 5.5 | 20.6 | |
| Outpatient treatment | 20.7 | 9.3 | 22.2 | 38.0 | |
| Day treatment b | 22.2 | 14.7 | 28.5 | 50.0 | |
| Therapeutic foster care | 5.6 | 17.2 | 27.6 | 51.7 | |
| Therapeutic group home c | 25.3 | 18.2 | 27.3 | 40.9 | |
| Residential treatment center | 12.3 | 9.4 | 12.5 | 23.4 | |
| Change in residence at discharge | <.001 | ||||
| No | 73.0 | 14.4 | 24.9 | 42.8 | |
| Yes | 27.0 | 5.7 | 12.8 | 24.8 | |
| Service system involvement | .884 | ||||
| 1-2 systems | 60.9 | 10.4 | 21.1 | 38.4 | |
| 3-4 systems | 39.1 | 14.7 | 22.6 | 37.3 | |
| Health care system characteristics | |||||
| Community mental health provider index d | .065 | ||||
| 100-300 providers | 34.5 | 13.9 | 23.9 | 43.3 | |
| > 300 providers | 65.5 | 11.1 | 20.5 | 35.1 | |
Note. p-values are based Log-rank two-tailed tests.
Non-white includes 93% African American youth, 7% Hispanic and Asian;
This category includes partial hospitalization and/or school-based day treatment;
This category includes group home, therapeutic group home, and crisis residential.
Community mental health provider index is the ratio of providers per 10,000 adolescents in county of residence.
Data Sources and Collection Procedures
Data for this study came from hospital case records, Medicaid claims files, and the Area Resource File. The three data files were merged using Medicaid policy numbers and social security numbers to allow for a more comprehensive examination of individual and community-level variables. All procedures were approved by the Institutional Review Boards at the University of Maryland, the state's Department of Health and Mental Health Hygiene, and the three hospitals.
Hospital case records
Detailed information on demographic and family background, clinical (e.g., diagnoses, symptoms, comorbidities, risk behaviors), and treatment characteristics (e.g., prior service history, type of aftercare, discharge living arrangement) was abstracted by two Master's level social work students who were unaware of the purposes of the study. To ensure high inter-rater reliability, a data abstraction instrument was developed and piloted prior to data collection; variables that could not be reliably abstracted from the records were excluded. In addition, a detailed coding manual was developed with descriptions of the data collection protocol, the structure and content of medical records at each hospital site, and operational definitions of each variable and location within the chart. Coders also received comprehensive training and did not begin actual data collection until excellent inter-rater reliability had been achieved (kappa of .81-1.0). One quarter of the charts were independently checked for rater agreement by the project director.
Data on clinical factors were collected from hospital records using the Childhood Severity of Psychiatric Index Scale (CSPI)(Lyons, 1998b), a 25-item, reliable and well-validated standardized instrument that assesses children's mental health needs (Leon, Uziel-Miller, Lyons, & Tracy, 1999; Lyons, Kisiel, Dulcan, Cohen, & Chesler, 1997; Lyons, Rawl, Yeh, Leon, & Tracy, 2002). Each item uses a 4-point anchor scale, requiring the rater to assess severity of symptoms or level of risk (0 = no problem or no risk, 1 = mild problem or low risk, 2 = moderate problem or medium risk, 3 = severe problem or high risk). For the symptoms domain, a rating of 2 or greater corresponds to a Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994) diagnosis within the five broad diagnostic categories: neuropsychiatric disturbance, emotional disturbance, conduct disturbance, oppositional behavior, and impulsivity.
The risk factor domain measures the recency and acuity of risk, with higher ratings indicating more recent and acute risk (e.g., suicide attempt or ideation in the past 7 days). For this study, 9 items were used from the symptom, risk factor, comorbidity, and functioning domains. Average inter-rater reliabilities for the CSPI ratings based on weighted kappa are as follows: Neuropsychiatric, .86; Emotional, .60; Oppositional, .66; Conduct, .63; Impulsivity, .54; Suicide, .79; Danger to Others, .74; Elopement, .81; and Family Functioning, .63.
Medicaid claims data file
Service utilization data on types and dates of mental health services received 30 days before and after the index hospitalization and time to first readmission were abstracted from Medicaid claims data files. Data on state hospital admissions were also obtained from the Hospital Management Information System (HMIS), a data warehouse for clients served by the state mental health authority, to allow for tracking of readmissions to all Maryland hospitals.
Area Resource File
Selected data elements from the Area Resource File (ARF) were used to measure availability of mental health providers. ARF contains over 7,000 county-level variables on health facilities, health professions, utilization, and socioeconomic characteristics of the nation's counties (Bureau of Health Professions, 1998).
Measures
Outcomet Variable
The outcome variable is time to first readmission. Time is measured in days from discharge and could theoretically range from 1 to 365 days (all cases were right censored at 1 year). Readmission is a dichotomous variable coded as “0” for no readmissions and “1” for any readmission during the study period.
Predictor Variables
Adolescent characteristics
Demographic variables included: adolescent's age at admission, race/ethnicity (0 = African American or other minorities, 1 = Caucasian), and gender (0 = male, 1 = female). The CSPI was used to measure severity of symptoms, risk behaviors, and comorbid factors. Variables from the symptom domain of the CSPI included: neuropsychiatric disturbance, emotional disturbance, conduct disturbance, oppositional behavior, and impulsivity. Because of the high correlations (.54 to .60) among the three behavioral symptom scales (conduct, oppositional and impulsivity), these variables were combined to create a behavioral symptom index ranging from 0 (no evidence of disturbance) to 9 (severe disturbance). For analyses, this variable was further recoded into three levels of severity, mild (0-3), moderate (4-6) and severe (7-9) disturbance and coded as 0, 1, 2, respectively. The other symptom variables were also collapsed into two and three level design categories based on frequency distributions: emotional (0 = no or mild disturbance; 1= moderate disturbance; 2 = severe disturbance) and neuropsychiatric (0 = no disturbance; 1= mild, moderate, or severe disturbance). Suicidality and dangerousness from the risk domain of the CSPI were originally coded as a four level ordinal variable (no risk, history of risk, recent risk, and acute risk); however, because the coefficients within the recent and acute risk categories were similar, these variables were recoded into three levels (0 = no known history of suicidal or violent behavior; 1 = history of suicidal or violent behavior; 2 = recent suicidal or violent behavior) to create a more parsimonious model. The substance abuse scale from the comorbidity domain of the CSPI was used to measure severity of substance abuse problems. Because of the small number of cases in the moderate and severe categories, this variable was also dichotomized into 0 = no or mild problems; 1= moderate or severe problems.
Other measures of comorbidity included mental retardation (coded as 0 = no; 1 = yes) if the adolescent received an Axis II diagnosis of mental retardation by the attending psychiatrist or if there was documented evidence (psychological testing) to support the diagnosis based on DSM-IV criteria. Youths were coded as having a history of abuse (0 = no; 1= yes) if there was documented evidence in the medical record of sexual abuse or physical abuse.
Family characteristics
To measure the relationship between number of family risk factors and readmission, the Family Risk Index (FRI), a four-item scale was created. The FRI was constructed from five dichotomous variables: (1) parental history of mental illness; (2) parental history of alcohol or drug abuse; (3) history of family violence; and (4) severe family dysfunction from the CSPI. These particular risk factors were selected because of their well-known associations with childhood mental health problems (Fraser, Richman, & Galinsky, 1999; Rutter, 1987) as well as readmission (Cornsweet-Barber & Evans, 1999). An index was used to measure family risk, rather than using individual items, as research on risk and resilience suggests that the number of family risk factors exerts a stronger influence on outcomes than single risk factors and has a cumulative effect (Forehand, Biggar, & Kotchick, 1998; Rutter, 1987; Sameroff, Bartko, Baldwin, Baldwin, & Seifer, 1999). The total Family Risk Index score was computed by adding responses from each of the four variables. Scores ranged from 0-4 with higher values signifying a greater level of risk. For analysis, this variable was further recoded into three levels based on the number of risk factors (0 = 0 to 1 [low risk], 1 = 2 to 3 [medium risk], 2 = 4 [high risk]).
Treatment characteristics
Treatment factors included: (1) hospital provider; (2) length of stay; (3) multiple prior hospitalizations; (4) type of aftercare services received within 30 days post discharge; (5) involvement with multiple service systems; (6) change in residence at discharge; and (7) history of medication non-compliance. Three of the seven variables (medication non-compliance, multiple prior hospitalizations, and change in residence at discharge) were dichotomous, coded as “1” if the characteristic was present and “0” if absent. Hospital provider was a three level variable. Type of aftercare services was a six category variables coded as 0 = no services, 1 = outpatient, 2 = day treatment, 3 = therapeutic foster care, 4 = group home, 5 = residential treatment center. Multiple system involvement was measured by a four item index that included history of involvement with: (1) the mental health system, (2) social services, (3) education system; and (4) juvenile justice. Total scores were calculated by summing responses to each item. Scores ranged from 0-4 with higher scores indicating greater involvement. For analysis, this variable was dichotomized into 0 = 1 to 2 services systems, 1 = 3 to 4 service systems. Length of stay was originally coded as a continuous variable; however, because of the skewed distribution, this variable was recoded into four discrete categories based on quartiles: 0 = 1 to 5 days, 1= 6-8 days, 2 = 9-17 days, 3 = > 18 days.
Health care system characteristics
To measure availability of mental health services, the Community Mental Health Provider Index (CMHPI) was created using county level data from the ARF. This ratio-level measure was defined as the sum of the number of mental health providers–child psychiatrists (ARF, 1999), pediatricians (ARF, 1998), family practitioners (ARF, 1998), psychologists (ARF, 1990) and social workers (ARF, 1990) per 10,000 adolescent population in the county of residence. Because data on mental health providers were not always available for the study period of observation (fiscal year 1998), data from the closest year was used. For analysis, this variable was dichotomized into 0 = ≤ 300 providers and 1 = >300 providers.
Data Analysis Strategy
Survival analysis techniques were used to determine rates of readmission and model predictors of time to readmission. Cumulative readmission rates were estimated using Kaplan Meier product–limit methods. The regression modeling process involved two phases. First, bivariate associations between each of the predictor variables and readmission were assessed using the Log-rank test for categorical variables. Second, Cox regression was used for the multivariate analysis to examine the association between predictor variables and the risk (hazard rate) for first readmission. Event-history models such as this one are preferable to logit models when data contain censored observations (e.g., event under study is not observed) and/or the models include time-varying covariates (Allison, 1995). In this case, adolescents who were event-free (not readmitted) by the end of the study 1 year follow-up period were right censored.
Variables were entered into the Cox regression model sequentially in four blocks based on ecological theory: adolescent demographic and clinical characteristics were entered first, followed by family, treatment, and health care system characteristics. The assumption of proportional hazards was checked by plotting the negative log (estimated survival function) against the log (failure time), and the Schoenfeld residuals. In instances where variables showed evidence of nonproportionality, an interaction term between time and the variable of interest was created and entered into the multivariate model. Interaction terms that were not significant were dropped from the final model. All analyses were conducted using STATA version 9.0 (Stata Corporation, 2005).
Results
Rates of Readmission
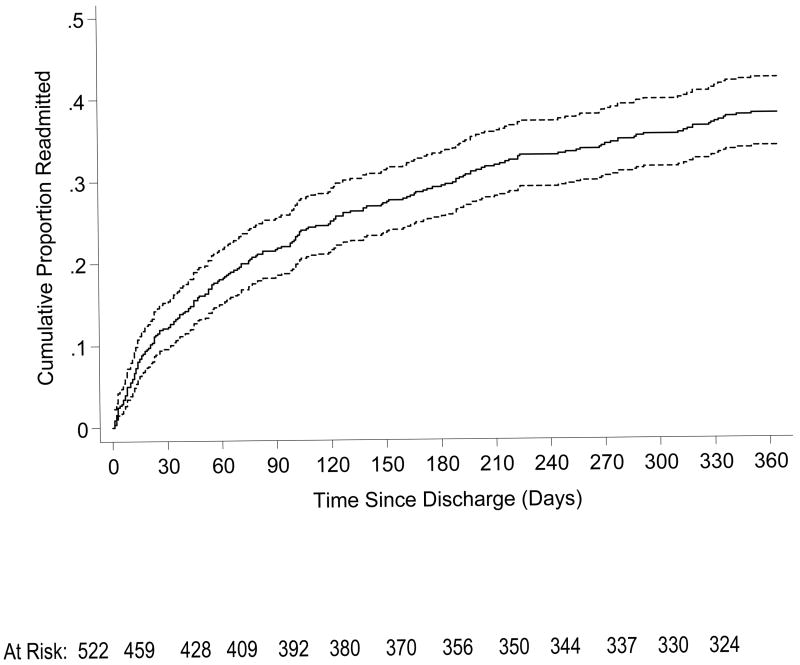
Of the 522 adolescents in the study sample, 198 (37.9%) experienced at least one readmission during the follow-up period. Figure 1 presents a plot of the one-year cumulative readmission rates and 95% confidence interval bands (upper and lower limits) derived from the Kaplan Meier product-limit estimates. The number of adolescents at risk at each 30-day time interval is also depicted. As shown, the estimated proportion of adolescents readmitted at 30, 60, and 90 days post-discharge were 12.1%, 18.0%, and 21.6% respectively. More than half of the adolescents (57%) experienced their first readmission by 90 days.
Figure 1.
Estimated Cumulative Proportion of Adolescents Readmitted Over One Year Period and 95% Confidence Intervals (N=522).
Predictors of Readmission
Bivariate analyses
Table 1 shows the characteristics associated with readmission of adolescents at 1, 3, and 12 months. Variables within each of the four domains—adolescent, family, treatment, and health care system characteristics–were examined. Percentages represent the proportion of youth within each variable category that were readmitted. The result indicated that youths who were younger, had more severe psychiatric disturbances (psychotic and behavioral symptoms), comorbid mental retardation, histories of or recent violent behavior, victims of abuse, and greater level of family risk were more likely to be readmitted. Higher readmission rates were also found for youths with more severe emotional disturbances; however, these differences were not statistically significant (p = .06). Substance abuse was inversely related to readmission; youths with severe substance abuse problems were less likely to be readmitted than those with mild substance abuse problems.
Among the treatment characteristics, service history factors such as prior hospitalizations and medication non-compliance were significantly associated with readmission. Rates of readmission also varied across hospital providers, ranging from 27.8% to 47.5%. Additionally, post-discharge environment and type of aftercare were strongly associated with readmission. At the time of discharge, almost half (49.7%) of youths were living with a parent or relative; the remainder were living in foster care or residential placements. Over one-quarter of the sample (27%) had a change in living situation as a result of hospitalization; these youths were significantly less likely to be readmitted. Readmission rates also varied considerably across types of aftercare, ranging from as high as 50% for youths who went to day treatment or therapeutic foster care (50.0% and 51.7%, respectively) to as low as 23.4% for youths who went to residential treatment. Youths who lived in areas with fewer health care providers also had higher rates of readmission compared to those who lived in areas with more providers; however, these differences only approached statistical significance (p = .07).
Multivariate analyses
Cox regression models were constructed to assess the influence of adolescent, family, treatment, and health care system characteristics on readmission. The results of these analyses including the estimated hazard ratios and significance levels for each predictor variable are shown in Table 2. Hazard ratios greater than 1 indicate increased risk of readmission (shorter time to readmission), while those less than 1 indicate decreased risk of readmission (longer time to readmission).
Table 2.
Estimated hazard ratios predicting readmission of adolescents to psychiatric hospitals (N = 522)
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Adolescent characteristics | ||||
| Age at admission | 1.30* | 1.31* | 1.32* | 1.32* |
| Race: white | 1.23 | 1.18 | 1.06 | 1.06 |
| Gender: females | 1.21 | 1.21 | 1.40* | 1.39* |
| Neuropsychiatric disturbance: any symptoms | 1.73*** | 1.70*** | 1.55** | 1.56** |
| Emotional disturbance | ||||
| Moderate disturbance | 1.53 | 1.45 | 1.61 | 1.61 |
| Severe disturbance | 2.02* | 1.98* | 2.08* | 2.08* |
| Behavioral Disturbance | ||||
| Moderate disturbance | 1.99** | 1.81* | 1.62 | 1.62 |
| Severe disturbance | 2.99*** | 2.69*** | 2.84*** | 2.84*** |
| Substance abuse problems: severe | 0.53** | 0.54* | 0.64 | 0.64 |
| Mental retardation: yes | 1.99*** | 2.18*** | 2.23*** | 2.23*** |
| Suicidality | ||||
| History of suicidal behavior | 4.86 | 4.59 | 3.88 | 3.87 |
| Recent suicidal behavior | 6.47* | 6.33* | 6.35* | 6.34* |
| Dangerousness | ||||
| History of violent behavior | 0.73 | 0.72 | 0.81 | 0.81 |
| Recent violent behavior | 0.75 | 0.77 | 0.95 | 0.95 |
| Abuse history: yes | 1.45* | 1.40* | 1.41* | 1.41 |
| Age × log(time) | 0.91*** | 0.91*** | 0.91*** | 0.91*** |
| History of suicidal behavior × log(time) | 0.72 | 0.73 | 0.72 | 0.72 |
| Recent suicidal behavior × log(time) | 0.63* | 0.63* | 0.63* | 0.63* |
| Family characteristics | ||||
| Family risk index | ||||
| Medium risk | 1.62* | 1.55 | 1.55 | |
| High risk | 2.14** | 1.78* | 1.78* | |
| Treatment characteristics | ||||
| Prior hospitalizations: yes | 1.38 | 1.38 | ||
| Medication noncompliance: yes | 1.63* | 1.63* | ||
| Hospital provider a | ||||
| Hospital B | NA | NA** | ||
| Hospital C | NA | NA** | ||
| Length of stay | ||||
| 6-8 days | 1.46 | 1.46 | ||
| 9-17 days | 1.42 | 1.42 | ||
| > 18 days | 2.27** | 2.27** | ||
| Aftercare received 30 days post-discharge | ||||
| No services | 1.01 | 1.02 | ||
| Outpatient treatment | 2.13* | 2.13* | ||
| Day treatment | 2.05* | 2.05* | ||
| Therapeutic foster care | 3.10** | 3.10** | ||
| Therapeutic group home | 2.51** | 2.51** | ||
| Change in residence at discharge: yes | 0.42*** | 0.42*** | ||
|
| ||||
| Service system involvement: 3-4 systems | 0.75 | 0.75 | ||
| Health care system characteristics | ||||
| Community mental health | ||||
| Provider index: > 300 providers | 1.01 | |||
| Model chi-square | 103.63*** | 111.10*** | 174.06*** | 174.06*** |
| Degrees of freedom | (18) | (20) | (34) | (35) |
| Chi-square improvement | 103.63*** | 7.47* | 62.96*** | 0.00 |
Note. Analyses are based on Cox regression models. NA = Not applicable. Reference categories are: race: non-white; gender: males; neuropsychiatric disturbance: no disturbance; emotional disturbance: no or mild; behavioral disturbance: no or mild; substance abuse: no or mild; mental retardation: no; suicidality: no history; dangerousness: no history; abuse history: no; prior hospitalizations: no; medication noncompliance: no; hospital provider: Hospital A; length of stay: 1-5 days; type of aftercare: residential treatment center; change in residence: no; service system involvement: 1-2 systems; community mental health provider index: 100-300 providers.
This variable was coded using deviation from the means coding. True hazard ratios are not possible using deviation from means coding.
p < .05.
p < .01.
p < .001.
Model 1 examined the influence of adolescent demographic and clinical characteristics on readmission. The interaction between age and time indicated that at 5 days after discharge, each additional year of age increased the risk of readmission by 13%; however, this effect decreases over time up until about 17 days post-discharge at which point age has a negative effect on readmission. Of the clinical factors, higher risk of readmission was associated with more severe emotional, behavioral and neuropsychiatric symptoms, comorbid mental retardation, and history of abuse. For example, compared to youths with mild behavioral problems, the risk of readmission was 2.0 and 3.0 times higher for youths with moderate and severe behavioral problems, respectively. Lower risk of readmission was associated with substance abuse; youths with severe substance abuse problems were 47% less likely to be readmitted compared to those with mild substance abuse problems. The effect of suicidality varied with time; youth with recent suicidal behavior were at higher risk for readmission soon after discharge compared to those with no known history of suicidal behavior. This effect diminishes over time, such that by 53 days this difference disappears, and subsequently the variable has a negative effect on readmission. For example, at 7 days the hazard ratio or risk of readmission was 2.6, at 15 days it was 1.8, and at 30 days it was 1.3.
Model 2 examined the influence of family characteristics on readmission. The inclusion of the family risk index significantly improved the ability of the model to predict readmission over the model with only demographic and clinical factors (χ2 = 7.5, df = 2, p < .05). The results indicated that youths who came from medium and high risk families (two or more risk factors) were 1.6 and 2.1 times more likely to be readmitted than those who came from low risk families.
Model 3 examined the influence of treatment characteristics on readmission. The inclusion of treatment characteristics significantly improved the ability of the model to predict readmission over the model with only demographic, clinical, and family factors (χ2 = 62.96, df = 14, p < .001). Of the seven variables examined, six were significantly associated with readmission. However, type of aftercare received one month after discharge had the strongest effect. Using residential treatment as the reference category, the risk of readmission was significantly higher for adolescents discharged to outpatient, day treatment, therapeutic foster care, and group homes (HRs of 2.13, 2.05, 3.10, 2.51, respectively). Higher risk of readmission was also associated with medication noncompliance (HR = 1.63, p < .05). Contrary to expectations, however, history of prior hospitalizations was not associated with readmission when other variables were controlled for in the model.
Lower risk of readmission was associated with change in living arrangement at discharge. For example, if the adolescent's placement was changed as a result of discharge planning, the risk of readmission was reduced by 58%. Hospital provider and length of stay were also significantly associated with readmission. Using deviation from the means coding, Hospital B and Hospital C were significantly different from the mean (p < .003 and p < .008, respectively). Youths with longer lengths of stay (greater than 18 days) were 2.3 times more likely to be readmitted compared to those with shorter lengths of stay (1-5 days). When this set of variables was entered into the model, substance abuse problems were no longer significant; however, gender became significant. As shown in Table 2, females were 40% more likely to be readmitted than males.
Model 4 tested the influence of health care system characteristics. The inclusion of the community mental health provider index did not improve the overall fit of the model. When this variable was entered into the model, history of abuse became nonsignificant.
Discussion
The primary purpose of this investigation was to identify factors associated with readmission of adolescents. The study expands upon prior research by examining multiple risk factors and multiple levels of influence using comprehensive data from three merged data sources. Additionally, the study provides an extensive analysis of the important, yet largely ignored treatment factors; in particular, aftercare, post-discharge environment, and hospital setting.
Summary and Interpretation of Findings
In this sample of youths enrolled in Medicaid and admitted to inpatient care, almost 38% of youths were readmitted within one year of discharge; the majority of these readmissions occurred within three months following the initial hospitalization with the highest risk period in the first 30 days. These rates of readmission are consistent with those reported in prior studies on both Medicaid and non-Medicaid populations (Arnold et al., 2003; Blader, 2004; Dougherty Management Associates, 2002; Pavkov et al., 1994).
Multivariate results suggest that multiple factors predict readmission, including demographic, clinical, family, and treatment characteristics. Our estimates showed that type of aftercare, particularly treatment foster care, was a strong predictor of readmission. Consistent with study hypotheses, youths discharged to lower levels of care (e.g., day treatment, therapeutic foster care, group homes) were significantly more likely to be readmitted than those discharged to the highest level of care (residential treatment). Adolescents placed in therapeutic foster care were at greatest risk for readmission; the estimated hazard ratio was more than 3 times greater than for youths discharged to residential treatment. These findings are consistent with the Heflinger et al. (2002) study that found that placement in more restrictive environments (residential treatment vs. group or foster care) reduced the likelihood of hospitalization.
There are two possible explanations for these findings. First, services may not be adequate or intense enough to meet the level of need of these youths, particularly those in therapeutic foster care who have complex problems and exposure to multiple stressors (e.g., poverty, abuse and neglect, separation from family etc.)(Burns et al. 2004). Second, the type of treatment may also have an effect on readmission. If youths are referred to aftercare services that are either inappropriate (e.g., mismatched to targeted problems or programs) or are not evidenced-based, a negative outcome may result. Unfortunately, evidence on the efficacy of commonly used treatments for children and adolescents in clinical practice settings is limited (Hoagwood, Burns, Kiser, Ringeisen, & Schoenwald, 2001). Moreover, even when evidence is available, youths continue to be referred to services that are inappropriate or ineffective either because of lack of provider knowledge or the sheer paucity of evidence-based services (Hoagwood et al., 2001).
Currently three types of interventions—multisystemic therapy, functional family therapy, and multidimensional treatment foster care—have been shown to be effective treatments for children and adolescents with severe emotional and behavioral disturbances. However, in most states these evidenced-based programs are available on a limited basis or minimally funded (DHHS, 2005). For youths on Medicaid, a major obstacle is that many communities lack intensive community-based treatment alternatives or systemic barriers such as inadequate reimbursement, lack of providers, or eligibility requirements prevent children from accessing these needed services; consequently, options for aftercare are often limited (Collins & Collins, 1994).
Post-discharge living environment also significantly influenced readmission. Youths who had a change in living arrangement at discharge were less likely to be readmitted than youths without a change. More than a quarter of the sample experienced a change in placement, most to more restrictive settings. It is striking that more than half of youths who were in foster care at admission were moved to another placement at discharge. These findings are consistent with other research (Newton, Litrownik, & Landsverk, 2000; Rubin et al. 2004) that has found higher rates of mental health problems associated with unstable foster care placements.
Another important finding was the effect of hospital provider on readmission. Rates of readmission varied significantly across hospital providers, ranging from 28% to 48%. These findings are consistent with prior research which has found hospital to be a major predictor of length of stay (Leon, Snowden, Bryant, & Lyon, 2006) and medication use (Warner, Pottick, & Bilder, 2006). Because the study did not examine specific hospital characteristics (e.g., bed capacity, staffing patterns, ownership status), the reason for the variability in readmission rates across hospitals remains unknown. One possibility for the differing rates of readmission across hospital providers may be attributed to the availability of step-down services (e.g., partial hospitalization) and geographic location of the hospital. For example, prior studies (e.g., Garritson, 1999) have shown that utilization of inpatient services is greatly affected by the supply of providers, availability of resources, and location of the hospital. That the hospital with the highest readmission rates was located in a semirural area with few available community resources provides support for this explanation. Hospitals are more likely to admit when community-based alternative services are not available, even if the child does not meet medical necessity criteria. Differences in admission policies and treatment orientation may also be a contributing factor.
Contrary to expectations, adolescents with longer rather than shorter lengths of stay were more likely to be readmitted. Findings from prior studies that have examined the relationship between length of stay and readmission are contradictory; some have found shorter lengths of stays were associated with readmission whereas others have not. These inconsistencies are most likely attributable to differences in study populations and hospital settings. Studies that have focused on Medicaid populations have generally found that longer lengths of stay are associated with readmission. A likely explanation for these findings is that longer lengths of stay may be an indicator of severity of illness and/or placement difficulty.
With regard to health care system characteristics, it was expected that availability of community resources would be associated with readmission even after controlling for demographic and clinical factors. Study findings failed to support this hypothesis. At the bivariate level, there was an association between the supply of providers and readmission; youths who lived in areas with less health providers had higher readmission rates. However, in the final multivariate model when demographic and clinical factors were controlled, availability of providers was not associated with readmission. These results are inconsistent with the Heflinger et al. (2002) study that found that greater availability of community-based services reduced the likelihood of hospitalization. The discrepancy in findings may in part be attributed to differences in how study measures were operationalized.
Increased severity of illness, as expected, was associated with higher risk of readmission. Youths with more severe psychotic, emotional, and behavioral disorders, co-occurring mental retardation, multiple family risk factors, and medication non-compliance were at increased risk for readmission. Suicidality was also associated with readmission; however, this relationship was time dependent. For adolescents with recent suicidal ideation or attempts, the risk of readmission was highest within the first week after discharge, most likely due to suicide reattempts, but gradually decreases over time such that by 53 days the differences are nonexistent. These findings are consistent with prior research (Appleby, Dennehy, Thomas, Faragher, & Lewis, 1999; Huey et al., 2004; Qin & Nordentoft, 2005) which has found that the highest risk period for suicide occurs soon after discharge and highlights the need for intensive aftercare services and family supports to prevent future suicide. While there are no definitive explanations for the high suicide risk immediately after discharge, it appears that the first 60 days is a particularly critical period, as youths may not be fully stabilized nor adequately prepared to transition from inpatient care to a less restrictive setting.
Contrary to expectations, severity of substance abuse was not associated with readmission in the final model. Although studies with adult patients have consistently found strong associations between co-occurring substance abuse disorders and readmission (e.g., Haywood et al., 1995), studies on children and adolescents (e.g., Arnold et al., 2003; Romanksy et al., 2003) have not. One reason for this discrepancy may be that treatment teams are assessing youths for substance abuse problems and appropriately referring them to drug and alcohol programs. The inverse relationship between substance abuse and readmission provides some support for this explanation.
Of the demographic variables examined, adolescent's age and gender were significantly associated with readmission. Consistent with Foster's (1999) study, females were more likely to be readmitted. The effect of age varied with time; older adolescents initially had a higher risk of readmission but after about 17 days the risk of readmission decreases. Pavkov and colleagues (1997) also found increased risk of readmission for younger adolescents which may indicate an earlier onset of disorder and more severe symptomatology. The initial higher rates of readmission for older adolescents may be related to difficulties accessing more intensive services.
Limitations
Several limitations should be considered when interpreting the results. First, because the sample was composed of adolescents who were covered by Medicaid and admitted to three private psychiatric hospitals, results may not be generalizable to general and state hospitals or other non-Medicaid populations. However, because all adolescents have Medicaid as their payment source, the results are relevant to other Medicaid populations in the U.S.
A second set of limitations involves measurement error related to the data source and how some measures were operationalized. This study, like most examining readmission, relies on medical record data which has both advantages and disadvantages. While medical records provide a wealth of information on clinical factors and are generally preferable to administrative data, measures based on medical records may be compromised due to variations in the completeness and accuracy of the recorded information, interpretations of clinical events, and documentation patterns across hospitals (Iezzoni, 1997). In addition, some of the measures, such as the family risk index and provider supply, were not formally tested; therefore, the validity of these measures is uncertain. Although the research literature provides support for constructing indices of family risk based on the sum of the number of risk factors (Forehand et al., 1998), this analytic strategy treats all risk factors equally and it may be that some risk factors are more important than others. Moreover, the measure of supply of providers includes data on some providers, most notably psychologists and social workers, that are nearly a decade old, and may not accurately reflect the number of providers in a given county.
A third limitation relates to unmeasured confounding factors, namely, readmissions to hospitals outside the state of Maryland or intervening factors such as death after discharge (either due to suicide or other causes). Although the likelihood of out-of-state hospitalization and/or death is infrequent, both instances could potentially lead to biased results either by underestimating the numbers of readmissions or artificially inflating the number of youths not at risk for readmission (Aston & Wray, 1996). It should be noted, however, that most readmission studies not only fail to examine mortality but also typically track readmission to the same hospital.
Finally, data were collected in fiscal year 1998 and it is plausible that changes that have occurred since that time may affect readmission patterns. For example, although medical necessity criteria for psychiatric hospitalization has not changed, average length of stays and available beds for state psychiatric facilities have been reduced and policy changes have affected access to and availability of some community-based resources.
Implications for Clinical Practice and Research
Study findings have important implications for clinical practice and research. First, the differing rates of readmission across the types of aftercare services suggest that youths may not have received appropriate services that best matches their level of clinical need. One implication of this findings is that we need to develop discharge planning guidelines and standards of care that are preferably linked to outcomes (Bickman, Karver, & Schut, 1997) to ensure that youths are linked to appropriate services. Given that the highest risk period for readmission occurred within three months following discharge, there is also clearly a need for aggressive outreach and follow-up, particularly for high risk youth with prior suicidal behavior. Second, findings underscore the importance of careful discharge planning; when workers intervene to change an unstable placement the likelihood of readmission is reduced. Youths in foster care may be particularly vulnerable to placement instability; therefore this group should receive increased attention. Third, the findings that the hospital provider strongly influenced readmission even after controlling for illness and other demographic factors, highlight the need to better understand how organizational factors affect the care received by youths in inpatient psychiatric facilities.
To further advance the knowledge base, it will be important for future research to examine the specific aspects of treatment itself; that is, the activities and clinical processes involved in the care of youths within acute-care inpatient settings and the effects of organizational climate (e.g., attitudes, job satisfaction, role conflict) and other hospital-level characteristics (e.g., size, teaching status, location, staffing patterns). More fine-grained analyses of aftercare services are also needed. Ideally, the various aspects of aftercare including level of care, treatment approach, and quality of care need to be disentangled and their relationship to clinical and functional outcomes evaluated.
Conclusions
This study suggests that a multitude of factors predict whether an adolescent will be readmitted to a psychiatric hospital. Clinical characteristics strongly influenced readmission. However, it is noteworthy that even after controlling for these demographic and clinical characteristics, it is the treatment factors (e.g., hospital setting, aftercare, post-discharge living environment) that are the best predictors of readmission. Study findings suggest that linkage to appropriate aftercare and discharge planning aimed at increasing the stability of placement reduces the likelihood of readmission. Moreover, hospital providers appear to play a critical role in determining treatment outcomes. As hospitals are faced with the challenge of providing high quality-care within a context of managed care imposed restrictions on length of stay, it will be critical for researchers, hospital administrators, and clinicians to evaluate the effects of treatment characteristics on subsequent outcomes.
Acknowledgments
This study was supported in part by an NIMH postdoctoral training grant (T32) and The Center for Health Care Strategies Inc., under the Annie E. Casey Foundation's Children in Managed Care Initiative (CIMC), the Thomas Wilson Sanitarium for Children of Baltimore City, and the Baltimore Community Foundation. The author thanks the hospital administrators and staff, Tom Merrick and Robin Jacobs from the Maryland Department of Health and Mental Hygiene, and Gary Phillips, M. A. S., senior consulting research statistician from the Ohio State University, Center for Biostatistics.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/ort/
References
- Aday LA, Andersen R. A framework for the study of access to medical care. Health Services Research. 1974;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- Allison P. Survival analysis using SAS: A practical guide. Cary, NC: SAS Institute Inc.; 1995. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Appleby L, Dennehy JA, Thomas CS, Faragher EB, Lewis G. Aftercare and clinical characteristics of people with illness who commit suicide: A case-control study. The Lancet. 1999;353:1397–1400. doi: 10.1016/S0140-6736(98)10014-4. [DOI] [PubMed] [Google Scholar]
- Appleby L, Desai PN, Luchins DJ, Gibbons RD, Hedeker DR. Length of stay and recidivism in schizophrenia: A study of public psychiatric hospital patients. The American Journal of Psychiatry. 1993;150:72–76. doi: 10.1176/ajp.150.1.72. [DOI] [PubMed] [Google Scholar]
- Arnold EM, Goldston DB, Ruggiero A, Reboussin BA, Daniel SS, Hickman EA. Rates and predictors of rehospitalizations among formerly hospitalized adolescents. Psychiatric Services. 2003;54:994–998. doi: 10.1176/appi.ps.54.7.994. [DOI] [PubMed] [Google Scholar]
- Ashton CA, Wray NP. A conceptual framework for the study of early readmission as an indicator of quality of care. Social Science & Medicine. 1996;43:1533–1541. doi: 10.1016/s0277-9536(96)00049-4. [DOI] [PubMed] [Google Scholar]
- Blader JC. Symptom, family, and service predictors of children's psychiatric rehospitalization within one year of discharge. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:440–451. doi: 10.1097/00004583-200404000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickman L, Karver MS, Schut LJ. Clinician reliability and accuracy in judging appropriate level of care. Journal of Consulting and Clinical Psychology. 1997;65:515–520. doi: 10.1037//0022-006x.65.3.515. [DOI] [PubMed] [Google Scholar]
- Blotcky MJ, Dimperio TL, Gossett JT. Follow-up of children treated in psychiatric hospitals: A review of studies. American Journal of Psychiatry. 1984;141:1499–1507. doi: 10.1176/ajp.141.12.1499. [DOI] [PubMed] [Google Scholar]
- Bureau of Health Professions. Area resource file. Fairfax, VA: Quality Resource Systems, Inc.; 1998. Office of Research and Planning. [Google Scholar]
- Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, Landsverk J. Mental health need and access to mental health services by youths involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:960–970. doi: 10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- Callahan JJ, Shepard DS, Beinecke RH, Larson MJ, Cavanaugh D. Mental health/substance abuse treatment in managed care: The Massachusetts Medicaid experience. Health Affairs. 1995;14:173–184. doi: 10.1377/hlthaff.14.3.173. [DOI] [PubMed] [Google Scholar]
- Collins BG, Collins TM. Child and adolescent mental health system: Building a system of care. Journal of Counseling & Development. 1994;72:239–243. [Google Scholar]
- Cornsweet-Barber C, Evans RB. Predicting psychiatric hospital readmission using a tree-based model; Paper presented at 12th Annual Research Conference, A System of Care for Children's Mental Health: Expanding the Research Base; Tampa, Florida. 1999. [Google Scholar]
- Cornsweet-Barber C, Rosenblatt A, Harris L, Attkisson CC. Use of mental health services among severely emotionally disturbed children and adolescents in San Francisco. Journal of Child and Family Studies. 1992;1:183–207. [Google Scholar]
- Dalton R, Moseley T, McDermott B. Psychiatric findings among child psychiatric inpatients groups by public and private payment. Psychiatric Services. 1997;48:689–693. doi: 10.1176/ps.48.5.689. [DOI] [PubMed] [Google Scholar]
- Daniel SS, Goldston DB, Harris AE, Kelley AE, Palmes GK. Review of literature on aftercare services among children and adolescents. Psychiatric Services. 2004;55:901–912. doi: 10.1176/appi.ps.55.8.901. [DOI] [PubMed] [Google Scholar]
- Dickey B, Normand SL, Norton EC, Rupp A, Azeni H. Managed care and children's behavioral health services in Massachusetts. Psychiatric Services. 2001;52:183–188. doi: 10.1176/appi.ps.52.2.183. [DOI] [PubMed] [Google Scholar]
- Dougherty Management Associates, Inc. Children's mental health benchmarking Project: Second year report. Boston, MA: Author; 2002. [Google Scholar]
- Fontanella CA, Zuravin SJ, Burry CL. The effect of a medicaid managed care program on patterns of psychiatric readmission among adolescents: Evidence from Maryland. Journal of Behavioral Health Services Research. 2006;33:39–52. doi: 10.1007/s11414-005-9004-0. [DOI] [PubMed] [Google Scholar]
- Forehand R, Biggar H, Kotchick BA. Cumulative risk across family stressors: Short- and long-term effects for adolescents. Journal of Abnormal Child Psychology. 1998;26:119–128. doi: 10.1023/a:1022669805492. [DOI] [PubMed] [Google Scholar]
- Foster EM. Do aftercare services reduce inpatient psychiatric readmissions? Health Services Research. 1999;34:715–736. [PMC free article] [PubMed] [Google Scholar]
- Fraser MW, Richman JM, Galinsky MJ. Risk, protection, and resilience: Toward a conceptual framework for social work practice. Social Work Research. 1999;23:131–143. [Google Scholar]
- Garritson SH. Availability and performance of psychiatric acute care facilities in California from 1992 to 1996. Psychiatric Services. 1999;50:1453–1460. doi: 10.1176/ps.50.11.1453. [DOI] [PubMed] [Google Scholar]
- Haywood TW, Kravitz HM, Grossman LS, Cavanaugh JL, Davis JM, Lewis DA. Predicting the “revolving door” phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. American Journal of Psychiatry. 1995;152:856–861. doi: 10.1176/ajp.152.6.856. [DOI] [PubMed] [Google Scholar]
- Heflinger CA, Simpkins CG, Foster EM. Modeling child and adolescent psychiatric hospital utilization: A framework for examining predictors of services use. Children's Services: Social Policy, Research, and Practice. 2002;5:151–171. [Google Scholar]
- Hoagwood K, Burns B, Kiser L, Ringeisen H, Schoenwald S. Evidence-based practice in child and adult mental health services. Psychiatric Services. 2001;52:1179–1189. doi: 10.1176/appi.ps.52.9.1179. [DOI] [PubMed] [Google Scholar]
- Huey SJ, Jr, Henggeler SW, Rowland MD, Halliday-Boykins CA, Cunningham PB, Pickrel SG, et al. Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:183–190. doi: 10.1097/00004583-200402000-00014. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI. Risk adjustment for measuring healthcare outcomes. 2nd. Chicago, IL: Health Administration Press; 1997. [Google Scholar]
- Klinkenberg DW, Calsyn RJ. Predictors of receipt of aftercare and recidivism among persons with severe mental illness: A review. Psychiatric Services. 1996;47:487–496. doi: 10.1176/ps.47.5.487. [DOI] [PubMed] [Google Scholar]
- Leon SC, Snowden J, Bryant FB, Lyons JS. The hospital as predictor of children's and adolescents' length of stay. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:322–328. doi: 10.1097/01.chi.0000194565.78536.bb. [DOI] [PubMed] [Google Scholar]
- Leon SC, Uziel-Miller ND, Lyons JS, Tracy P. Psychiatric hospital service utilization of children and adolescents in state custody. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:305–310. doi: 10.1097/00004583-199903000-00018. [DOI] [PubMed] [Google Scholar]
- Lien L. Are readmission rates influenced by how psychiatric services are organized? Nordic Journal of Psychiatry. 2002;56:23–28. doi: 10.1080/08039480252803873. [DOI] [PubMed] [Google Scholar]
- Lyons JS. Readmission as an indicator of quality of care [Letter to the editor] American Journal of Psychiatry. 1998a;155:450. [PubMed] [Google Scholar]
- Lyons JS. Severity of psychiatric illness scale: Child and adolescent version. San Antonio (Texas): Psychological Corp; 1998b. [Google Scholar]
- Lyons JS, Kisiel CL, Dulcan M, Cohen R, Chesler P. Crisis assessment and psychiatric hospitalization of children and adolescents in state custody. Journal of Child and Family Studies. 1997;6:311–320. [Google Scholar]
- Lyons JS, O'Mahoney MT, Miller SI, Neme J, Kabat J, Miller F. Predicting readmission to the psychiatric hospital in a managed care environment: Implications for quality indicators. American Journal of Psychiatry. 1997;154:337–340. doi: 10.1176/ajp.154.3.337. [DOI] [PubMed] [Google Scholar]
- Lyons JS, Rawal P, Yeh I, Leon S, Tracy P. Use of measurement audit in outcomes management. Journal of Behavioral Health Services and Research. 2002;29:75–80. doi: 10.1007/BF02287834. [DOI] [PubMed] [Google Scholar]
- Newton RR, Litrownik AJ, Landsverk JA. Children and youth in foster care: Disentangling the relationship between problem behaviors and number of placements. Child Abuse and Neglect: An International Journal. 2000;24:1363–1374. doi: 10.1016/s0145-2134(00)00189-7. [DOI] [PubMed] [Google Scholar]
- Pavkov T, Goerge R, Lee B, Howard E. Child and adolescent inpatient psychiatric care: An examination of the state hospital population in Illinois; Paper presented at: 7th Annual Research Conference, A System of Care for Children's Mental Health: Expanding the Research Base; Tampa, Florida. 1994. [Google Scholar]
- Pavkov TW, Goerge RM, Lee BJ. State hospital reentry among youth with serious emotional disturbance: a longitudinal analysis. Journal of Child and Family Studies. 1997;6:373–83. [Google Scholar]
- Perkins DO. Predictors of noncompliance in patients with schizophrenia. Journal of Clinical Psychiatry. 2002;63:1121–1128. doi: 10.4088/jcp.v63n1206. [DOI] [PubMed] [Google Scholar]
- Pfieffer SI, Strezelecki SC. Inpatient psychiatric treatment of children and adolescents: a review of outcome studies. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:847–853. doi: 10.1097/00004583-199011000-00001. [DOI] [PubMed] [Google Scholar]
- Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: Assessing environmental and provider-related variables in the behavioral model of utilization. Health Services Research. 1998;33:571–596. [PMC free article] [PubMed] [Google Scholar]
- Pottick K, Hansell S, Gutterman E, Raskin-White H. Factors associated with inpatient and outpatient treatment for children and adolescents with serious mental illness. Journal of the Academy of Child & Adolescent Psychiatry. 1995;34:425–433. [PubMed] [Google Scholar]
- Pottick KJ, McAlpine DD, Andelman RB. Changing patterns of psychiatric inpatient care for children and adolescents in general hospitals, 1988-1995. American Journal of Psychiatry. 2000;157:1267–1273. doi: 10.1176/appi.ajp.157.8.1267. [DOI] [PubMed] [Google Scholar]
- Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: Evidence based on longitudinal registers. Archives of General Psychiatry. 2005;62:427–432. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- Ringel JS, Sturm R. National estimates of mental health utilization and expenditures for children in 1998. Journal of Behavioral Health Services Research. 2001;28:319–333. doi: 10.1007/BF02287247. [DOI] [PubMed] [Google Scholar]
- Romansky JB, Lyons JS, Lehner RK, West CM. Factors related to psychiatric hospital readmission among children and adolescents in state custody. Psychiatric Services. 2003;54:356–62. doi: 10.1176/appi.ps.54.3.356. [DOI] [PubMed] [Google Scholar]
- Rosenau PV, Linder SH. A comparison of the performance of for-profit and nonprofit U.S. psychiatric inpatient care providers since 1980. Psychiatric Services. 2003;54:183–187. doi: 10.1176/appi.ps.54.2.183. [DOI] [PubMed] [Google Scholar]
- Rubin DM, Alessandrini EA, Feudtner C, Mandell DS, Localio AR, Hadley T. Placement stability and mental health costs for children in foster care. Pediatrics. 2004;113:1336–1341. doi: 10.1542/peds.113.5.1336. [DOI] [PubMed] [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Sameroff A, Bartko WT, Baldwin A, Baldwin C, Seifer R. Family and social influences on the development of child competence. In: Lewis M, Feiring C, editors. Families, risk, and competence. Mahwah, NJ: Lawrence Erlbaum; 1999. pp. 161–185. [Google Scholar]
- Saunders RC, Heflinger CA. Access to and patterns of behavioral health services among children and adolescents in TennCare. Psychiatric Services. 2003;54:1364–1371. doi: 10.1176/appi.ps.54.10.1364. [DOI] [PubMed] [Google Scholar]
- Solomon P, Evans D, Delaney MA. Community service utilization by youths hospitalized in a state psychiatric facility. Community Mental Health Journal. 1993;29:333–346. doi: 10.1007/BF00761031. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 9. College Station, TX: StataCorp LP; 2005. [Google Scholar]
- Stiles PG, Culhane DP, Hadley TR. For-profit versus non-profit freestanding psychiatric inpatient facilities: An update. Administration and Policy in Mental Health. 1997;24:191–204. doi: 10.1007/BF02042473. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Subcommittee on evidence-based Practices: Background paper (DHHS Pub No SMA-05-4007) Rockville, MD: Author; 2005. [Google Scholar]
- Warner LA, Pottick K, Bilder SM. Clinical and organizational correlates of medications for youths in U.S. mental health services. Social Service Review. 2005;79:454–481. [Google Scholar]
- Wickizer TM, Lessler D, Boyd-Wickizer J. Effects of health care cost-containment programs on patterns of care and readmissions among children and adolescents. American Journal of Public Health. 1999;89:1353–1358. doi: 10.2105/ajph.89.9.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]