Abstract
Previous research has suggested that, when compared to European Americans (EAs), African Americans (AAs) are at higher risk of metastatic disease at time of cancer diagnosis, and a higher risk of shorter survival. Although AA patients have reported worse physical health than EA patients, studies have rarely addressed whether racial/ethnic disparities exist on the social, emotional, and functional aspects of health-related quality of life (HRQL). Five hundred and two AA and 396 EA patients with AIDS-related malignancies or breast, colon, head/neck, and lung cancers seeking treatment within the contiguous United States and Puerto Rico participated in the present study. Responses on the Functional Assessment of Cancer Therapy- General (FACT-G) were analyzed for possible racial/ethnic disparities using multivariable regression models and item response theory (IRT) modeling to detect differential item functioning (DIF). DIF was found in six items of the FACT-G, indicating that AA and EA participants had different probabilities of responding to these items. Compared to EAs at the same level of HRQL, AAs reported more severe symptomatology on items that reflected malaise and ability to work, and less severe symptomatology on items that reflected fatigue, treatment side effects, and outlook on life. At the subscale level, AAs reported poorer physical and social well-being, but better emotional well-being, than EAs. Similar to previous studies, AA patients reported poorer physical functioning than a comparable group of EA patients. Some items appear to be responded to differently by AAs and EAs, suggesting it is important to consider race/ethnicity when evaluating responses to questions about HRQL.
Keywords: Quality of Life, Cancer, Measurement, Race, African Americans
Introduction
In the United States, numerous disparities in health care delivery and outcomes have been identified when one compares groups of people across socio-economic status, ethnicity, and race. Studies of racial/ethnic disparities in cancer have tended to focus on outcome disparities between African-American (AA) and European-American (EA), non-Hispanic1–5 people. These studies have investigated general racial/ethnic differences in physical health outcomes, such as mortality rate, stage of disease, and treatment.
Results have shown that AA women with breast cancer are more likely to be younger, be in an advanced stage of disease by the time they are diagnosed, and have higher mortality rates than EA women with breast cancer.1, 6 Additionally, AA women were more likely than EA women with breast cancer to receive mastectomies and less likely to receive adjuvant treatments to keep their cancer from returning, such as chemotherapy, immunotherapy, hormone therapy, or radiation therapy.2, 7
Similar disparities have been noted with colorectal and lung cancers. Colorectal cancer rates have stabilized for AA men and women, but AAs have lower 5-year survival rates than EAs.4 In addition, although lung cancer rates have decreased for men and stabilized for women over the years, incidence rates for lung cancer are 50% higher for AA men than EA men.4 Furthermore, Thompson and colleagues3 found that AA men with prostate cancer showed higher mortality rates, more extensive disease at time of diagnosis, poorer performance status, younger age, and worse prognosis than EA men with the same diagnosis. Likewise, a number of studies have shown racial/ethnic disparities in cancer stage.5 Hoffman and colleagues8 also found that underemployment, having no insurance or public insurance, and lower socioeconomic status were significantly related to advanced-stage prostate cancer in men across racial/ethnic groups, and socioeconomic factors alone could not sufficiently account for the higher percentages of advanced stage cancer found in the AA population.
Unlike the studies of differences in mortality and treatment described above, studies of health-related quality of life (HRQL) measure the subjective outcomes of physical, emotional, social, and functional well-being.9, 10 Furthermore, much of the research on racial/ethnic differences in HRQL for cancer patients has focused on the general concept of HRQL or the physical well-being dimensions of HRQL. Penedo et al. 11 examined overall HRQL scores, and found that AA and Hispanic men living with prostate cancer reported lower HRQL than EA men living with prostate cancer. Similarly, several studies have found that AA men with prostate cancer reported decreased physical well-being than EA men.12–14 Lubeck and colleagues15 found that AA men with prostate cancer reported poorer physical well-being than EA men with prostate cancer, and they also had slower rates of improvement in HRQL scores over time.
Given the scant amount of research investigating racial/ethnic differences in reporting of non-physical dimensions of HRQL, we set out to identify racial/ethnic differences in the reporting of physical, functional, emotional, and social well-being. We identified racial/ethnic differences in symptoms reported on the FACT-General (FACT-G) from a large and diverse sample of participants with breast, colon, head and neck, and lung cancers, as well as HIV/AIDS-related malignancies. We first evaluated item-by-item differences in responses from people of EA and AA backgrounds. In addition to item level differences, we examined overall racial/ethnic differences on each of the four dimensions of HRQL.
Methods
Patient-reported HRQL data were collected as part of the Bilingual Intercultural Oncology Quality of Life (BIOQOL) project, a cross-sectional validation study of the Functional Assessment of Cancer Therapy (FACT) and Functional Assessment of Human Immunodeficiency Virus Infection (FAHI) scales.9 The aims of the project were to validate the scales across language (English, Spanish), self-identified race/ethnicity (AA non-Hispanic, EA non-Hispanic, Hispanic), literacy (high, low), and mode of administration (interview, self-administration).
Participants in the BIOQOL project were recruited from seven public and private urban cancer care centers in Atlanta, Chicago, and San Juan (Puerto Rico). Patients were eligible to participate if they had a diagnosis of breast, colon, head/neck or lung cancer, or AIDS-related malignancies, were at least 18 years of age, spoke English or Spanish, and provided written informed consent in accordance with institutional review board requirements. This report describes the analysis of data from the AA and EA participants only, and these data came from participants in Chicago and Atlanta.
Functional Assessment of Cancer Therapy-General (FACT-G)
The FACT-G is a 27-item questionnaire with five Likert-type response categories ranging from 0 to 4 (“not at all” to “very much”). The FACT-G demonstrated strong psychometric properties in terms of reliability and validity.16, 17 Four subscales were derived from factor analysis from the original validation sample: physical, emotional, social and functional well-being.16 Certain items were reversed scored such that on all items and aggregated subscale scores, a higher score indicated better HRQL. The physical well-being and functional well-being subscales contain seven items, and scores on these subscales can range from 0 to 28. The social well-being and emotional well-being subscales contain six items, and scores on these subscales can range from 0 to 24. High literacy participants (based on Woodcock Language Proficiency Battery) were randomly assigned to interview- or self-administration of the questionnaire, and all low literacy patients were assigned to interview-administration.
Statistical Analysis
In order to investigate item-level racial/ethnic differences on the FACT-G, we used item response theory (IRT) models. IRT is a family of statistical models used to examine characteristics of items and respondents’ trait levels.18 IRT can help to identify racial/ethnic group differences through an examination of differential item functioning (DIF). DIF examines the differences in probabilities of item endorsement across groups of people.19 Item endorsement refers to the patterning of a participant’s response, or how a participant answered on each item given the five response categories. DIF, sometimes referred to as item bias, enables one to identify questionnaire items that perform differently in one group compared to another.
Confirmatory factor analyses of the FACT-G showed that each subscale has a single factor solution, indicating that each of the four subscales are unidimensional in nature.20 Therefore, IRT modeling was conducted on each subscale separately. One-parameter logistic (1-PL/Rasch) models were used, and DIF analysis was performed for each FACT-G subscale.21 For this, the WINSTEPS calibration program was used.22 WINSTEPS employs one-parameter (Rasch) logistic models as well as “rating scale” models developed for ordered response categories. WINSTEPS uses maximum likelihood procedures to estimate respondents’ levels on a trait and each item’s difficulty (or in the case of health questionnaires, severity of symptomatology). WINSTEPS conducts t-tests to compare the groups’ calibrations on each item. Conducting multiple comparisons simultaneously on the same data increases the likelihood of observing a statistically significant difference by pure chance. Thus, a Bonferroni technique was implemented to adjust for spurious positive findings due to multiple comparisons.23
Separate multivariable linear regression models were constructed with each FACT-G subscale as the dependent variable and race (AA non-Hispanic vs. EA non-Hispanic) as the primary independent variable. Sociodemographic and clinical covariates included gender, marital status (not married vs. married), education (less than high school, high school/GED, bachelors/graduate degree), literacy (high literacy vs. low literacy, based on Woodcock Language Proficiency Battery performance higher or lower than the 6th grade level24), diagnosis (breast cancer, colon cancer, head-neck cancer, lung cancer, AIDS-related malignancies), insurance status (any insurance vs. no insurance), and patient-reported Eastern Cooperative Oncology Group (ECOG) performance status rating (normal activity, some symptoms, bed rest for < 50% of day, bed rest for > 50% of day.25 All covariates that met a screening criterion (P<0.25 in bivariable regressions) were selected for a multivariable model and then removed individually using backward elimination (retention criterion, P<0.05).26,27 The primary goal of these analyses was to estimate the adjusted effects of race on HRQL outcomes, and to determine whether these effects were meaningful.
Results
Participants
Data from 898 participants were analyzed. In Atlanta, the refusal rates were 10.6%, and in Chicago, the refusal rates were 9.0%. More than half of the participants self-identified as AA, non-Hispanic (n=502). The participants’ sociodemographic and clinical characteristics are provided in Table 1.
Table 1.
Sample Characteristics (Total n = 898)
| Variable | Mean (Standard Deviation)/Frequency (%) | |
|---|---|---|
| European-American 396 (44.1%) | African-American 502 (55.9%) | |
| Age | M = 56.2 (SD= 13.0) | M =53.3 (SD= 13.4) |
| Female | 267 (67.4%) | 321 (63.9%) |
| Married | 233 (58.8%) | 203 (40.4%) |
| Region | ||
| Chicago | 243 (67.5%) | 253 (52.5%) |
| Atlanta | 117 (32.5%) | 229 (47.5%) |
| Education | ||
| < High School | 59 (14.9%) | 198 (39.4%) |
| High School/GED | 220 (55.6%) | 258 (51.4%) |
| Bachelors degree | 70 (17.7%) | 29 (5.8%) |
| Graduate degree | 47 (12.9%) | 17 (3.4%) |
| High Literacy | 346 (94.0%) | 339 (77.8%) |
| Diagnosis | ||
| Breast cancer | 195 (49.2%) | 195 (38.8%) |
| Colon cancer | 27 (6.8%) | 86 (17.1%) |
| Head/Neck Cancer | 28 (7.1%) | 45 (9.0%) |
| Lung Cancer | 103 (26.0%) | 107 (21.3%) |
| AIDS-related malignancies | 43 (10.9%) | 69 (13.7%) |
| No Current Insurance | 44 (11.8%) | 123 (27.8%) |
| Performance Status | ||
| Normal activity | 168 (42.5%) | 190 (37.9%) |
| Some symptoms | 125 (31.6%) | 156 (31.1%) |
| Bed rest < 50% of day | 82 (20.8%) | 107 (21.4%) |
| Bed rest > 50% of day | 20 (5.1%) | 48 (9.6%) |
| Extent of Disease | ||
| No evidence of disease | 150 (40.7%) | 124 (28.0%) |
| Local Disease | 60 (16.3%) | 105 (23.7%) |
| Regional Spread | 58 (15.7%) | 110 (24.8%) |
| Distant metastases | 101 (27.4%) | 104 (23.5%) |
| Currently on active treatmenta | ||
| Yes | 33 (8.3%) | 54 (10.8%) |
| FACT-G Subscale Scores | ||
| Physical Well-Being | M= 21.7 (SD= 5.6) | M= 20.2 (SD= 6.0) |
| Social Well-Being | M= 23.0 (SD= 4.8) | M= 20.9 (SD= 5.7) |
| Emotional Well-Being | M= 18.2 (SD= 4.5) | M= 18.8 (SD= 5.2) |
| Functional Well-Being | M= 19.6 (SD= 6.3) | M= 18.1 (SD= 7.1) |
Active treatment is defined as chemotherapy, radiotherapy, or antiretroviral therapy. Participants not on active treatment may have been on other medications that are not considered “active,” such as hormonal or analgesic medication.
Differential Item Functioning
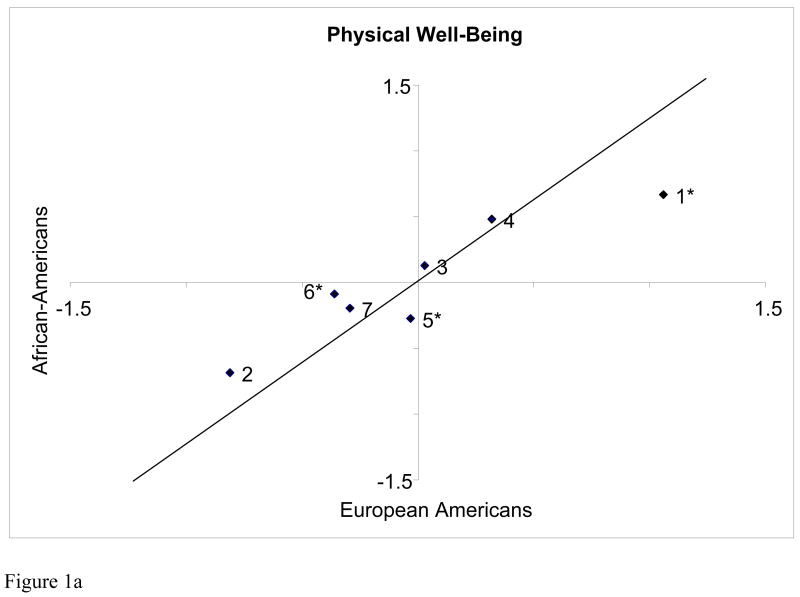
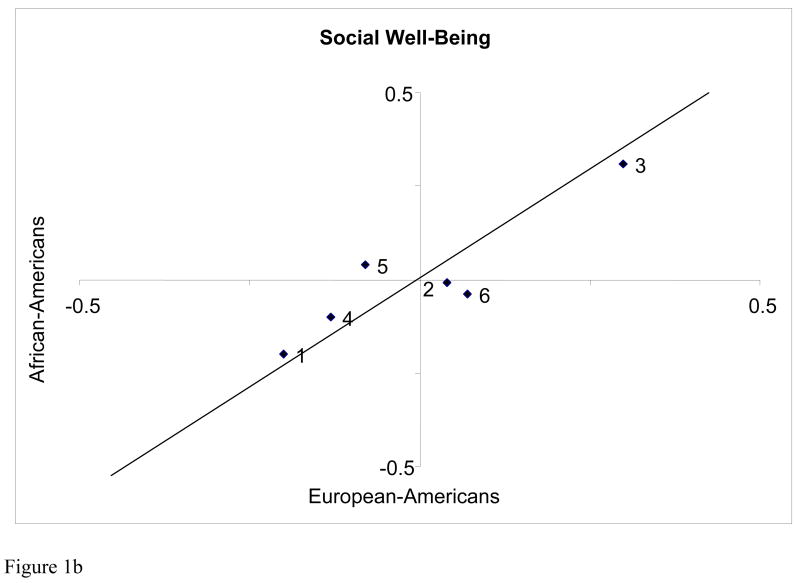
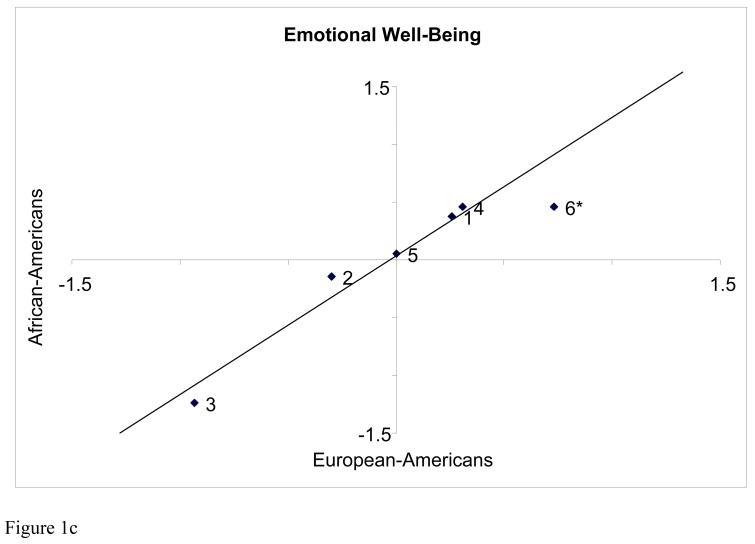
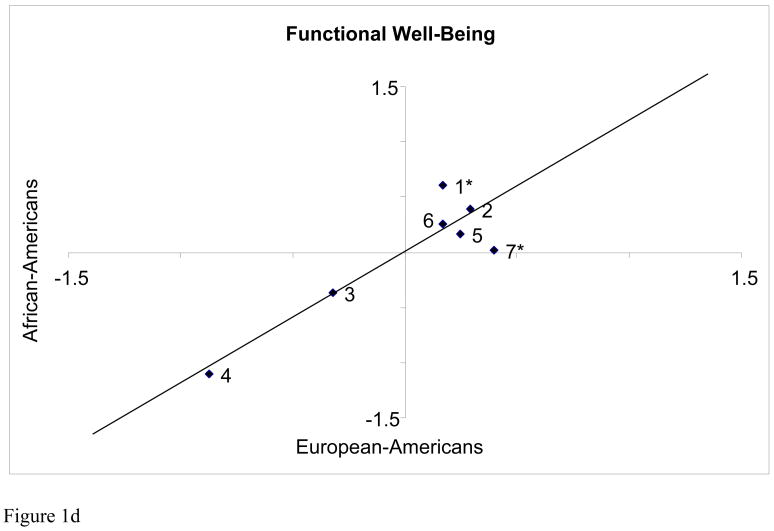
Of the 27 FACT-G items, the question that assessed sexual satisfaction was dropped from the analysis of the social well-being subscale because many participants left this item blank. After the Bonferroni correction was applied, six items of the 26 remaining FACT-G items demonstrated DIF across the two racial/ethnic groups. Item calibrations were estimated separately for AA and EA participants. More positive item calibrations indicated that the item measured less severe symptomatology. More negative item calibrations indicated that the item measured more severe symptomatology. The item calibrations are plotted for each subscale in Figures 1a–1d.
Figures 1a to 1d. Plots of item calibrations for each subscale of the FACT-G.
The X axis represents item calibrations for European-American participants and the Y axis represents item calibrations for African-American participants. The farther the item is located from the reference line, the larger the magnitude of differential item functioning (DIF). Labels for items are abbreviated. Items with asterisks indicate that the items were identified as having DIF.
Figure 1a. Physical Well-Being
1 = “I have a lack of energy”, 2 = “I have nausea”, 3 = “Because of my physical condition, I have trouble meeting the needs of my family”, 4 = “I have pain”, 5 = “I am bothered by side effects of treatment”, 6= “I feel ill”, 7 = “I am forced to spend time in bed”
Figure 1b. Social Well-Being
1 = “I feel distant from my friends”, 2 = “I get emotional support from my family”, 3 = “I get support from my friends and neighbors”, 4 = “My family has accepted my illness”, 5 = “Family communication about my illness is poor”, 6 = “I feel close to my partner”
Figure 1c. Emotional Well-Being
1 = “I feel sad”, 2 = “I am proud of how I’m coping with my illness”, 3 = “I am losing hope in the fight against my illness”, 4 = “I feel nervous”, 5 = “I worry about dying”, 6 = “I worry that my condition will get worse”
Figure 1d. Functional Well-Being
1 = “I am able to work”, 2 = “My work is fulfilling”, 3 = “I am able to enjoy life”, 4 = “I have accepted my illness”, 5 = “I am sleeping well”, 6 = “I am enjoying the things I usually do for fun”, 7 = “I am content with the quality of my life right now”
Specifically, on the physical well-being subscale, the item “I have a lack of energy” (Figure 1a, Item 1) functioned differently across AAs and EAs. AA participants at comparable physical well-being indicated less severity on this symptom than EA participants. Similarly, on the statement “I am bothered by side effects of treatment” (Figure 1a, Item 5), AA participants indicated less severity on this symptom than comparably-scoring EA participants. In contrast, on the statement “I feel ill” (Figure 1a, Item 6), AA participants indicated more severity on this symptom than comparably scoring EA participants. On the emotional well-being subscale, on the statement “I worry that my condition will get worse” (Figure 1c, Item 6), AA participants indicated less severity on this symptom compared with comparable EA participants. Finally, on the functional well-being subscale, on the statement “I am able to work” (Figure 1d, Item 1), AA participants indicated more severity on this symptom than EA participants. On the statement “I am content with the quality of my life right now” (Figure 1d, Item 7), AA participants indicated less severity on this symptom than comparable EA participants. For these results, when a participant indicated less severity on a symptom, they were reporting a better health status on the symptom being measured.
Multiple Regression Analyses
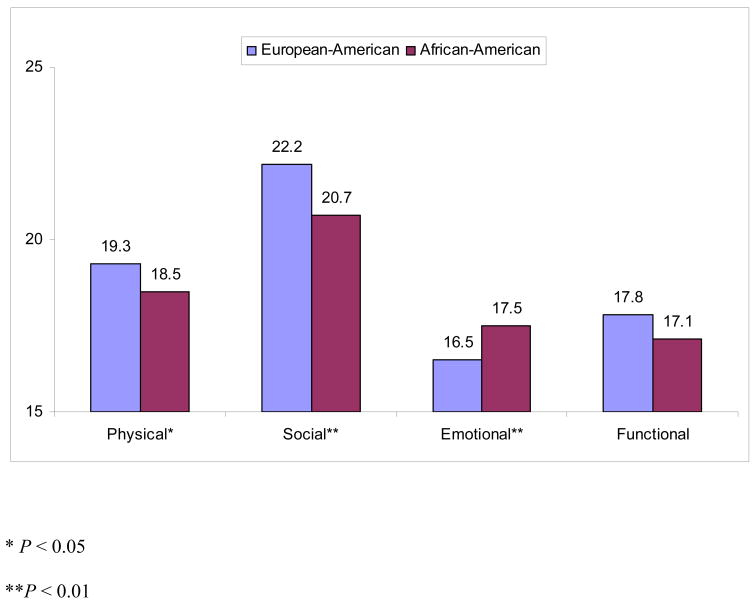
The sociodemographic and clinical covariates described above were entered into univariate analyses with each subscale of the FACT-G. If the variables met screening criteria from these analyses (P < 0.25), they were included in a series of backward elimination multiple regression analyses. Regression statistics for the final models are located in Table 2, and adjusted mean scores for AA and EA participants are illustrated in Figure 2.
Table 2.
Statistics for Regression Analyses of Four FACT-G Subscales
| Subscale | Variable | B | SE B | β | |
|---|---|---|---|---|---|
| Physical Well Being R2 = 0.38b | Race/Ethnicity (Reference: European-American) | −0.92 | 0.34 | −0.08a | |
| Education (Reference: < High school diploma) | |||||
| High school diploma | −0.85 | 0.37 | −0.07c | ||
| Bachelors degree or more | 0.02 | 0.50 | 0.00 | ||
| Patient reported performance status (Reference: Normal activity/without symptoms) | |||||
| Some symptoms | −3.92 | 0.38 | −0.33 | ||
| Bed rest < 50% of day | −3.77 | 0.45 | −0.29 | ||
| Bed rest > 50% of day | −3.02 | 0.67 | −0.14 | ||
| Social Well Being R2 = 0.19b | Race/Ethnicity (Reference: European-American) | −1.45 | 0.48 | −0.13a | |
| Married (Reference: Not married) | 1.47 | 0.52 | 0.13a | ||
| Diagnosis (Reference: Breast Cancer) | |||||
| Colon Cancer | 0.17 | 0.78 | 0.01 | ||
| Head/Neck Cancer | −1.34 | 0.86 | −0.07 | ||
| AIDS Malignancy | −4.22 | 0.78 | −0.27b | ||
| Lung Cancer | −0.57 | 0.61 | −0.04 | ||
| Patient reported performance status (Reference: Normal activity/without symptoms) | |||||
| Some symptoms | −0.42 | 0.56 | −0.04 | ||
| Bed rest < 50% of day | −1.72 | 0.65 | −0.14a | ||
| Bed rest > 50% of day | 0.76 | 1.07 | 0.03 | ||
| Emotional Well Being R2 = 0.12b | Race/Ethnicity (Reference: European-American) | 0.95 | 0.35 | 0.10a | |
| Insurance Status (Reference: No current insurance) | 1.24 | 0.42 | 0.10a | ||
| Diagnosis (Reference: Breast Cancer) | |||||
| Colon Cancer | 0.75 | 0.54 | 0.05 | ||
| Head/Neck Cancer | −0.96 | 0.65 | −0.05 | ||
| AIDS Malignancy | −2.39 | 0.56 | −0.16b | ||
| Lung Cancer | 0.08 | 0.44 | 0.01 | ||
| Patient reported performance status (Reference: Normal activity/without symptoms) | |||||
| Some symptoms | −1.71 | 0.40 | −0.17b | ||
| Bed rest < 50% of day | −0.66 | 0.48 | −0.06 | ||
| Bed rest > 50% of day | −1.36 | 0.72 | −0.07 | ||
| Functional Well Being R2 =0.31b | Race/Ethnicity (Reference: European-American) | −0.90 | 0.43 | −0.07c | |
| Married (Reference: Not married) | 1.29 | 0.41 | 0.09a | ||
| Education (Reference: < High school diploma) | −0.05 | 0.62 | −0.00 | ||
| High school diploma | −0.98 | 0.47 | −0.07c | ||
| Bachelors degree or more | −0.05 | 0.62 | −0.03 | ||
| Diagnosis (Reference: Breast Cancer) | |||||
| Colon Cancer | −0.25 | 0.63 | −0.01 | ||
| Head/Neck Cancer | −3.12 | 0.75 | −0.13b | ||
| AIDS Malignancy | −1.19 | 0.65 | −0.06 | ||
| Lung Cancer | −2.78 | 0.52 | −0.17b | ||
| Patient reported performance status (Reference: Normal activity/without symptoms) | |||||
| Some symptoms | −3.56 | 0.47 | −0.26b | ||
| Bed rest < 50% of day | −3.71 | 0.55 | −0.25b | ||
| Bed rest > 50% of day | −1.05 | 0.83 | −0.04 |
P<0.01.
P<0.001.
P<0.05.
Figure 2. Adjusted mean scores for FACT-G subscales.
Mean Scores adjusted for gender, marital status, education, diagnosis, insurance status, and ECOG performance status.
In the final model with physical well-being subscale, race was a significant predictor after adjusting for education and patient reported performance status. In the final model for social well-being, race was a significant predictor after adjusting for marital status, diagnosis, and patient reported performance status. In the final model with emotional well-being, race was a significant predictor after adjusting for insurance status, diagnosis, and patient-reported performance status. In the final model with functional well-being as the dependent variable, race was a significant predictor after adjusting for marital status, education, diagnosis, and performance status. At the subscale level, AA participants reported poorer overall physical, social, and functional well-being, but better emotional well-being, than EA participants.
Discussion
The present study examined racial/ethnic differences in HRQL at the individual item (e.g., symptom) level as well as on each FACT subscale level (physical, social, emotional and functional HRQL). Relative to EA patients, AAs with cancer reported worse physical and social well-being, and better emotional well-being. At the same overall level of well-being, AAs reported relatively less severe symptomatology than EAs on items reflecting fatigue and treatment side effects, and AAs were more likely to have a better outlook on life than EAs. On the other hand, AAs reported more severe symptomatology on items reflecting malaise (“feel ill”) and ability to work, compared to EA patients at the same level of overall well-being. Previous research with cancer patients demonstrated similar findings, and further found that AAs improve slower and suffer a poorer prognosis.12, 13 This information suggests that AAs with cancer are not as able to manage their illness as EAs with cancer. Difficulty managing illness can be linked with unequal access to care or poor communication with healthcare providers. As a result of these and other factors, AAs do not have their health care needs adequately met.28,29
AAs in the present study reported poorer physical well-being than EAs while at the same time indicating better emotional well-being than EAs. Other studies have found that among AAs, greater access to emotional support was positively associated with poorer perceptions of physical health.30 These results suggest that better emotional well-being may not necessarily reflect better physical well-being. Instead, the results suggest that emotional well-being is related to social support. Social support may help AAs with cancer keep a positive outlook on life, maintain high energy levels, and keep their focus off of treatment side effects. In other words, social support may not help to improve physical symptoms, but it may help people with cancer better cope with their illness.
In terms of specific symptoms of emotional well-being, AA patients in our study reported less worry about a worsening of their condition and were more comfortable with their current health status and quality of life. Utsey et al.31 stated that ethnic identity was the best predictor of AA quality of life. Other recent research has suggested that cultural resources and cultural pride reduce psychological stress.32 Cultural resources of benefit may include close knit friends and family, neighborhood churches, or a personal sense of spirituality. Like social support, attending church and being spiritual may help AAs with cancer cope with their illness. AAs living with cancer can use these cultural resources to deflect the stressors that oftentimes accompany their illness.
It is important to consider the role of socioeconomic status (SES) while examining racial/ethnic differences in health outcomes. Although SES does not account for all racial/ethnic differences in health status, the two are related: racial/ethnic minorities are often also categorized as having lower SES.33 SES has typically been estimated using three indicators: income, education, and occupation.34 In the present study, we examined one of these, education, and found that it was significantly related to physical and functional well-being.
Researchers have noted that lower SES is associated with poorer health status across disease categories, and suggest that health behaviors (smoking, physical activity, alcohol consumption) and psychological factors (depression, hostility, stress) are the mechanisms by which these associations occur.34 The Behavioral Model for Vulnerable Populations35, 36 also suggests that predisposing characteristics, such as race/ethnicity and SES, impact patients’ health status. Furthermore, the conceptual models propose that predisposing characteristics, health behaviors, and subsequent health outcomes are linked in a causal chain.35–37 Future research on racial/ethnic disparities in health outcomes can focus on clarifying the role of SES in this causal chain.
There were limitations to this study. First, the study employed a cross-sectional design, and as such, causal conclusions about the relationships between race/ethnicity, HRQL, and the other variables studied cannot be made. In addition, the participants for this study were well enough to participate in research, and thus, these results may not be generalizable to patients with more severe symptomatology. Furthermore, this study examined AAs and EAs, and studies of other racial/ethnic groups may produce different results.
In sum, previous research has primarily examined only the physical well-being dimension of HRQL, and few studies have examined the social, emotional, and functional aspects of HRQL. As a result of this more thorough analysis, the results have helped us to pinpoint specific differences in symptomatology. Future studies can extend these findings and investigate differences in cancer symptomatology with other vulnerable populations, such as people with poorer health literacy, linguistic minorities, and other racial/ethnic groups.
Acknowledgments
This study was supported by grant number R01-CA61679 from the National Cancer Institute (Principal Investigator: David Cella). Deepa Rao is supported by an Advanced Rehabilitation Research Training Grant from the National Institutes on Disability and Rehabilitation Research (H133P030002).
The authors would like to thank Elizabeth Hahn, Gail Shiomoto, Lesbia Hernandez, Maria Corona, and Veronica Valenzuela for their assistance on this project, along with the patients who participated in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shinagawa SM. The excess burden of breast carcinoma in minority and medically underserved communities: application, research, and redressing institutional racism. Cancer. 2000;88(5 Suppl):1217–1223. doi: 10.1002/(sici)1097-0142(20000301)88:5+<1217::aid-cncr7>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 2.Ashing-Giwa K, Padilla G, Tejero J, et al. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina, and Caucasian cancer survivors. Psychooncology. 2004;13:408–428. doi: 10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson I, Tangen C, Tolcher A, et al. Association of African American ethnic background with survival in men with metastatic prostate cancer. J Natl Cancer Inst. 2001;93(3):219–225. doi: 10.1093/jnci/93.3.219. [DOI] [PubMed] [Google Scholar]
- 4.American Cancer Society. Cancer facts & figures for African Americans. Atlanta: American Cancer Society, Inc.; 2003. [Google Scholar]
- 5.Mettlin CJ, Murphy GP, Cunningham MP, Menck HR. The National Cancer Data Base report on race, age, and region variations in prostate cancer treatment. Cancer. 1997;80(7):1261–1266. [PubMed] [Google Scholar]
- 6.Newman L, Carolin K, Simon M, et al. Impact of breast carcinoma on African American women. Cancer. 2001;91(9):1834–1843. doi: 10.1002/1097-0142(20010501)91:9<1834::aid-cncr1204>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 7.Payne R, Medina E, Hampton J. Quality of life concerns in patients with breast cancer. Cancer. 2003;97(1):311–317. doi: 10.1002/cncr.11017. [DOI] [PubMed] [Google Scholar]
- 8.Hoffman RM, Gilliland FD, Eley JW, et al. Racial and ethnic differences in advanced-stage prostate cancer: the Prostate Cancer Outcomes Study. J Natl Cancer Inst. 2001;93(5):388–395. doi: 10.1093/jnci/93.5.388. [DOI] [PubMed] [Google Scholar]
- 9.Cella D, Bonomi A. The Functional Assessment of Cancer Therapy (FACT) and Functional Assessment of HIV Infection (FAHI) quality of life measurement system. In: Spilker B, editor. Quality of life and pharmacoeconomics in clinical trials. Philadelphia: Lippincott-Raven Publishers; 1996. [Google Scholar]
- 10.Wan GJ, Counte MA, Cella DF, et al. An analysis of the impact of demographic, clinical, and social factors on health-related quality of life. Value Health. 1999;2(4):308–318. doi: 10.1046/j.1524-4733.1999.24006.x. [DOI] [PubMed] [Google Scholar]
- 11.Penedo F, Dahn J, Shen B, Schneiderman N, Antoni M. Ethnicity and determinants of quality of life after prostate cancer treatment. Urology. 2006;67(5):1022–1027. doi: 10.1016/j.urology.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 12.Eton D, Lepore S, Helgeson V. Early quality of life in patients with localized prostate carcinoma. Cancer. 2001;92(6):1451–1459. doi: 10.1002/1097-0142(20010915)92:6<1451::aid-cncr1469>3.0.co;2-r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krupski T, Fink A, Kwan L, et al. Health-related quality of life in low income uninsured men with prostate cancer. J Health Care Poor Underserved. 2005;16:375–390. doi: 10.1353/hpu.2005.0037. [DOI] [PubMed] [Google Scholar]
- 14.Maliski S, Kwan L, Orecklin J, Saigal C, Litwin M. Predictors of fatigue after treatment for prostate cancer. Urology. 2005;65:101–108. doi: 10.1016/j.urology.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 15.Lubeck D, Kim H, Grossfeld G, et al. Health related quality of life differences between black and white men with prostate cancer: data from the cancer of the prostate strategic urologica research endeavor. J Urol. 2001;166:2281–2285. [PubMed] [Google Scholar]
- 16.Cella D, Tulsky D, Gray G, et al. The Functional Assessment of Cancer Therapy (FACT) Scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 17.Cella D, Hernandez L, Bonomi A, et al. Spanish language translation and initial validation of the functional assessment of cancer therapy quality of life instrument. Med Care. 1998;36(9):1407–1418. doi: 10.1097/00005650-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Teresi J, Stewart A, Morales L, Stahl S. Measurement in a multi-ethnic society. Med Care. 2006;44(11 Suppl 3):S3–S4. doi: 10.1097/01.mlr.0000245437.46695.4a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hambleton R, Swaminathan H, Rogers H. Fundamentals of item response theory. Newbury Park, CA: Sage Publications, Inc.; 1991. [Google Scholar]
- 20.Hahn E, Rao D, Choi S, Cella D. Med Care. Comparability of interview- and self-administration of the Functional Assessment of Cancer Therapy-General (FACT-G) in English- and Spanish-speaking cancer patients. in press. AU: PLS UPDATE. [DOI] [PubMed] [Google Scholar]
- 21.Andrich D. A rating scale formulation for ordered response categories. Psychometrika. 1978;43:561–573. [Google Scholar]
- 22.Linacre JM. A user’s guide to WINSTEPS, MINISTEP, Rasch-model computer programs. Chicago: John M. Linacre; 2005. [Google Scholar]
- 23.Green S, Salkind N. Using SPSS for Windows and Macintosh: Analyzing and understanding data. Upper Saddle River, NJ: Prentice Hall; 2003. [Google Scholar]
- 24.Woodcock RW. Examiner’s manual: Woodcock Language Proficiency Battery-Revised. Allen, TX: DLM Publishers; 1991. [Google Scholar]
- 25.Zubrod C, Schneiderman M, Frei E. Appraisal of methods for the study of chemotherapy of cancer in man: comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J Chronic Dis. 1960;11:7–33. [Google Scholar]
- 26.Bendel RB, Afifi AA. Comparison of stopping rules in forward regression. J Am Stat Assoc. 1977;72:46–53. [Google Scholar]
- 27.Pedhazur EJ. Multiple regression in behavioral research. New York: Harcourt Brace College Publishers; 1997. [Google Scholar]
- 28.Green Anderson KO, Baker TA, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4(3):277–294. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 29.Hahn E, Cella D. Health outcomes assessment in vulnerable populations: measurement challenges and recommendations. Arch Phys Med Rehabil. 2003;84(2):35–41. doi: 10.1053/apmr.2003.50245. [DOI] [PubMed] [Google Scholar]
- 30.Bloor LE, Sandler RS, Martin C, Uchino BN, Kinney AY. Associations between emotional support and health-related quality of life among a population-based sample of blacks and whites. J Soc Clin Psychol. 2006;25(1):96–116. [Google Scholar]
- 31.Utsey SO, Chae MH, Brown CF, Kelly D. Effect of ethnic group membership on ethnic identity, race-related stress, and quality of life. Cultur Divers Ethnic Minor Psychol. 2002;8(4):366–377. doi: 10.1037/1099-9809.8.4.367. [DOI] [PubMed] [Google Scholar]
- 32.Bynum MS, Burton E, Best C. Racism experiences and psychological functioning in African American college freshmen: is racial socialization a buffer? Cultur Divers Ethnic Minor Psychol. 2007;13(1):64–71. doi: 10.1037/1099-9809.13.1.64. [DOI] [PubMed] [Google Scholar]
- 33.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26(3):483–505. doi: 10.2190/U9QT-7B7Y-HQ15-JT14. [DOI] [PubMed] [Google Scholar]
- 34.Adler N, Boyce T, Chesney M, et al. Socioeconomic status and health: the challenge of the gradient. In: Mann J, Gruskin S, Grodin M, Annas G, editors. Health and human rights. New York: Routledge; 1999. [Google Scholar]
- 35.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 36.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 37.Wilson IB, Cleary PD. Linking clinical variables with health related quality of life: a conceptual model of patient outcomes. JAMA. 1995;273(1):59–65. [PubMed] [Google Scholar]