Abstract
Generalized anxiety disorder (GAD) is a chronic anxiety disorder, associated with comorbidity and impairment in quality of life, for which improved psychosocial treatments are needed. GAD is also associated with reactivity to and avoidance of internal experiences. The current study examined the efficacy of an acceptance-based behavioral therapy, aimed at increasing acceptance of internal experiences and encouraging action in valued domains, for GAD. Clients were randomly assigned to immediate (n=15) or delayed (n=16) treatment. Acceptance-based behavior therapy led to statistically significant reductions in clinician-rated and self-reported GAD symptoms that were maintained at 3- and 9- month follow-up assessments; significant reductions in depressive symptoms were also observed. Seventy-eight percent of treated participants no longer met criteria for GAD and 77% achieved high end-state functioning at post-treatment assessment; these proportions stayed constant or increased over time. As predicted, treatment was associated with decreases in experiential avoidance and increases in mindfulness.
Keywords: generalized anxiety disorder, mindfulness, experiential avoidance, worry, RCT
Although efficacious individual cognitive behavioral therapies (CBT) have been developed for Generalized Anxiety Disorder (GAD), a large proportion of individuals treated fail to meet criteria for high end state functioning (see Waters & Craske, 2005, for a review), suggesting that further treatment development may be needed. A range of novel approaches are being explored (see Heimberg, Turk, & Mennin, 2004, for reviews). Our efforts have focused on an individual acceptance-based behavior therapy (ABBT) that targets experiential avoidance (attempts to alter the intensity or frequency of unwanted internal experiences, Hayes, Wilson, Gifford, Follette, & Strosahl, 1996), using strategies aimed at increasing awareness and intended action in important life domains.
Research suggests that individuals with GAD negatively evaluate internal experiences such as thoughts, emotions, and physiological sensations, and use worry, along with other strategies, as a means of escaping or avoiding these experiences. Individuals with GAD report distress about a wide range of emotions (e.g., Mennin, Heimberg, Turk, & Fresco, 2005), view their worrisome thoughts as dangerous and uncontrollable (Wells & Carter, 1999), and report a lack of self-compassion toward their own internal experience (Roemer et al., 2007). Engaging in the worry process reduces autonomic reactivity and distracts worriers from more distressing topics (Borkovec, Alcaine, & Behar, 2004). Directly targeting these problematic relationships and responses to internal experiences may improve the efficacy of GAD treatments.
Although behavioral exposure has not been a focus of GAD treatment, individuals with GAD do avoid anxiety-provoking situations (Butler, Gelder, Hibbert, Cullington, & Klimes, 1987). In addition, clients describe making behavioral choices aimed at decreasing anxiety, rather than maximizing satisfaction, and being distracted by worries when they are engaged in important activities. Therefore, an explicit focus on mindful behavioral engagement in valued actions (Wilson & Murrell, 2004) may be beneficial (for an extensive review of the empirical and theoretical rationale for ABBT for GAD, see Roemer & Orsillo, 2005; 2007).
We developed an ABBT for GAD drawing explicitly from cognitive behavioral interventions for GAD (e.g., Borkovec, Newman, Lytle, & Pincus, 2002), as well as Acceptance and Commitment Therapy (ACT; Hayes, Strosahl, & Wilson, 1999), Dialectical Behavior Therapy (DBT; Linehan, 1993) and Mindfulness-Based Cognitive Therapy (MBCT; Segal, Williams, & Teasdale, 2002). A small open trial of ABBT for GAD (Roemer & Orsillo, 2007) revealed promising findings. The current study expands this work by comparing ABBT to a waiting list condition and examining durability of effects over a 9-month follow-up period.
Method1
Participants
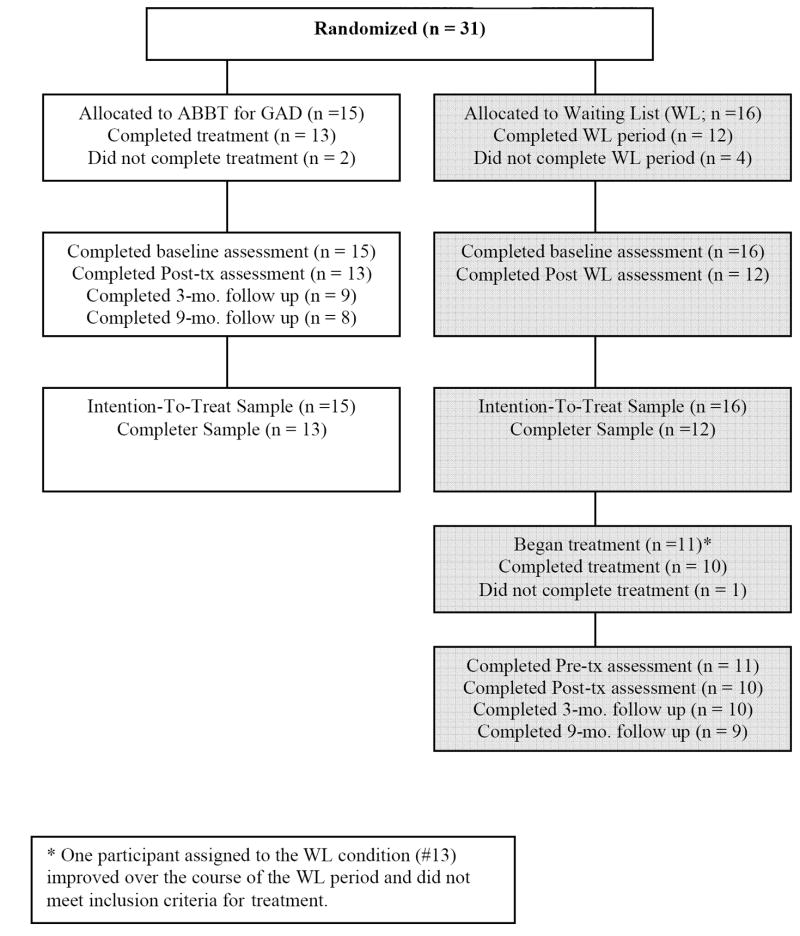
Thirty-one clients consented to participation and were randomized to treatment (n = 15) or waiting list control (n = 16). Two participants withdrew from therapy and four from the waiting list. The remaining waiting list participants received delayed treatment, except one participant who no longer met criteria for GAD post-waiting list. A participant diagnosed with GAD in partial remission following the waiting list period whose remaining symptoms were rated above the clinical cut-off received treatment and was included in subsequent analyses. One waiting list participant withdrew from therapy. Individuals with a principal diagnosis of GAD (excluding the DSM-IV hierarchical rule that GAD could not occur only within the course of a mood disorder2), who did not report current suicidal intent, did not meet criteria for current bipolar, substance dependence, or psychotic disorders, and were at least 18 were eligible for the study regardless of previous treatment history.3 See Table 1 for participant characteristics; conditions did not differ significantly on demographic variables.
Table 1.
Participant characteristics of intent-to-treat sample
| All Participants (n = 31) | Treatment (n = 15) | Waiting List (n = 16) | |
|---|---|---|---|
| Number female | 22 | 11 | 11 |
| Self-identified race/ethnicity, n | |||
| White | 27 | 12 | 15 |
| Latino/a | 2 | 2 | 0 |
| Black | 1 | 1 | 0 |
| Asian | 1 | 0 | 1 |
| Age, mean (sd) | 33.59 (11.74) | 32.73(11.05) | 32.88(11.66) |
| Stabilized on medication at start of treatment | 8 | 4 | 4 |
| Most common additional diagnoses | |||
| MDD | 9 | 4 | 5 |
| Social | 6 | 3 | 3 |
Note. MDD = Major Depressive Disorder; Social = Social Anxiety Disorder.
Measures
All assessments included primary measures of anxiety and worry, secondary measures of depression and quality of life, and measures of proposed mechanisms of change (experiential avoidance and mindfulness). The Anxiety Disorders Interview Schedule for DSM-IV – Lifetime Version (ADIS-IV; DiNardo et al., 1994) was used to determine current and lifetime DSM-IV diagnostic status (an abbreviated version focusing on current diagnoses was given for post- and follow-up assessments). The ADIS-IV includes a clinical severity rating (CSR) for each diagnosis received ranging from 0 to 8, with 4 being the diagnostic cut-off. All assessments were administered by doctoral students at the Center for Anxiety and Related Disorders (CARD) who had undergone extensive training and demonstrated reliability in diagnoses4. Diagnoses were confirmed in consensus meetings with a doctoral level psychologist (Dr. T.A. Brown) and by therapists in their initial meetings. The ADIS-IV has a reliability for principal GAD diagnoses of k = .67, and for CSR ratings of GAD of k = .72, in a study conducted at CARD (Brown, DiNardo, Lehmann, & Campbell, 2001). During the time period of this study at CARD, reliability for GAD diagnoses were k = .56, and for CSR ratings of GAD, k=.77. Participants also completed the Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990), a 16-item measure of trait levels of excessive worry (α = .795 in the current sample), and the Depression Anxiety Stress Scales – 21 item version (DASS-21; Lovibond & Lovibond, 1995), a measure that yields separate scores of depression, anxiety and stress. In the current study, the anxiety and stress sub-scales were used as indicators of anxiety, αs = .79 and .87 respectively. The Beck Depression Inventory (BDI-I-A; Beck, Rush, Shaw, & Emery, 1979), α =.87 in the current sample, and an abbreviated version of the Quality of Life Inventory (QOLI; Frisch, Cornwell, Villanueva, & Retzlaff, 1992), a measure of life satisfaction with an α of .836 in the current sample, were considered measures of secondary outcomes. Two measures were included to assess the impact of treatment on proposed mechanisms of action. The 16-item version of the Action and Acceptance Questionnaire (AAQ; Hayes et al., 2004) yields a total score representing severity of experiential avoidance. This version is highly correlated with the reliable and valid 9-item version of the scale, but has better internal consistency and is thought to be more sensitive to change (Hayes et al., 2004). The α in this sample was .84. The Mindful Attention Awareness Scale (MAAS; Brown & Ryan, 2000) is a 15-item self-report measure of present moment attention and awareness added during the study (18 participants completed it). Higher scores indicate higher levels of mindfulness. The scale has good internal consistency, temporal consistency, and validity (Brown & Ryan, 2000); α in this sample was .88.
Procedures
Clients seeking treatment at CARD at several periods between 2003-2005 (when study therapists had openings) who met inclusion/exclusion criteria were referred for this study. Of the 36 clients who were contacted, three declined, a fourth missed the informed consent meeting and did not return phone calls, and a fifth realized during the informed consent meeting that he would be away during the study period. The remaining 31 clients were randomly assigned to the treatment or waiting list condition in a randomized blocked fashion by the PI. Condition assignment was done using a coin flip; subsequent clients who matched an enrolled client in gender, racial minority status, and GAD severity (moderate versus severe) were assigned to the opposite condition to ensure balance across conditions in this small sample. Both the staff member and potential participant were blind to condition until the informed consent process was complete.
Clients assigned to the waiting list completed a post- assessment at least 14 weeks after their informed consent meeting and were offered the full treatment, after which they were assessed. Following treatment or waiting list, clients were assessed by a CARD assessor uninformed of condition and all were assessed again at three and nine months post-treatment.
Treatment
Clients were seen individually for four 90-minute and twelve 60-minute sessions, with the last two sessions tapered (from weekly to every other week). The treatment manual7 was an adapted version of the one used in Roemer and Orsillo (2007). Treatment involves increasing clients’ awareness of the habitual nature of anxious responding, the function of emotions, and the role of judgment and experiential avoidance in paradoxically worsening distress and interference using psychoeducation, experiential demonstrations, and between-session self-monitoring. Clients are taught a variety of mindfulness practices and encouraged to engage in both formal and informal mindfulness practice every day. Clients also engage in written exercises aimed at determining valued directions and treatment focuses on bringing mindful awareness to actions and trying previously avoided valued activities. Near the end of treatment, individualized plans are developed for maintaining the skills acquired in therapy.
Therapists and Treatment Integrity
Clients were treated by six doctoral students under the supervision of the first two authors. Two sessions from each client were randomly selected and rated for adherence by graduate students with extensive exposure to ABBT. Twenty-five percent of sessions were rated by two raters with acceptable reliability, k = .70. An adherence checklist listed twelve allowed and five forbidden strategies (e.g., focus on changing cognitions). Sessions averaged 10.64 allowed strategies; two minor nonprotocol events were recorded.
Results
Overall Analytic plan
Multi-level regression analyses were conducted using the Hierarchical Linear and Nonlinear Modeling software program (HLM 6; Raudenbush, Bryk, & Congdon, 2005). Means and standard errors generated by HLM are reported in Tables 2 and 4. Per Dunlop, Cortina, Vaslow, and Burke (1996), Cohen’s d was calculated based on the between-groups t-test value (d = 2t / √(df)). We first conducted analyses of treatment effects in the controlled trial data (pre- to post- treatment and waiting list) on an ITT (i.e., all randomized participants, n = 31), and a completer (25 of 31 participants) sample. In the ITT sample, power = .80 to detect effects of d ≥ 1.04 at alpha = .05. For the completer sample, power = .80 to detect effects of d ≥ 1.17 at alpha = .05. Results of the completer analyses were highly consistent; only the ITT analyses are presented here.8 We next analyzed uncontrolled effects and maintenance of treatment gains on a sample of all participants who began treatment (i.e., treatment and waiting list control conditions combined, n = 26; using post-WL assessments as pre-treatment assessments for WL participants). Of these participants, four missed 3-month and six missed 9-month follow-up assessment. Also, self-report measures only are missing for one client at post, one at 3-month and two at 9-month follow-up.9
Table 2.
Means (and Standard Errors) of all key study variables as a function of condition and time of measurement for the randomized controlled trial: Intention to treat sample (n = 31)
| Treatment (n = 15) | Waiting list control (n = 16) | |||
|---|---|---|---|---|
| Pre | Post | Pre | Post | |
| Primary Outcomes | ||||
| GAD CSR | 5.73(0.18) | 3.18(0.30) | 5.69(0.12) | 5.32(0.34) |
| PSWQ | 65.72(2.11) | 54.18(2.35) | 72.03(0.94) | 68.93(1.47) |
| DASS-Anxiety | 12.53(1.95) | 5.52(1.35) | 12.25(2.16) | 10.50(2.32) |
| DASS-Stress | 22.93(2.41) | 12.85(1.73) | 22.00(2.59) | 24.93(3.02) |
| Secondary Outcomes | ||||
| BDI | 17.53(1.94) | 5.77(1.33) | 19.69(1.83) | 16.52(2.33) |
| QOLI | 0.83(0.62) | 2.00(0.45) | 0.27(0.48) | .16(0.37) |
| # of add. diagnoses | 0.93(0.26) | 0.51(0.21) | 1.06(0.16) | 1.20(0.23) |
| Mechanism of Change | ||||
| AAQ | 72.87(3.51) | 55.07(3.32) | 77.19(2.11) | 76.25(2.58) |
| MAAS | 52.45(4.35) | 60.91(3.75) | 48.97(4.48) | 49.04(3.56) |
Note. GAD= generalized anxiety disorder, CSR = Clinician’s Severity Rating from the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version; PSWQ = Penn State Worry Questionnaire; DASS-Anxiety = Depression and Anxiety Stress Scales- Anxiety subscale; DASS-Stress = Depression and Anxiety Stress Scales- Stress subscale; BDI = Beck Depression Inventory; QOLI = Quality of Life Inventory; AAQ = Acceptance and Action Questionnaire; MAAS = Mindful Attention and Awareness Scale.
Table 4.
Means (and Standard Errors) of all variables at Pre-, Post-, and 3-month and 9-month Follow-up, and effect sizes, for full sample of participants who began treatment (n = 26)
| Pre | Post | 3-Month | 9-Month |
d |
|||
|---|---|---|---|---|---|---|---|
| Post | 3-month | 9-Month | |||||
| Primary Outcomes | |||||||
| GAD CSR | 5.69(0.13) | 3.10(0.21) | 3.22(0.21) | 2.98(0.30) | 2.97 | 2.83 | 2.34 |
| PSWQ | 67.15(1.39) | 53.23(2.07) | 50.68(1.96) | 49.00(2.39) | 1.58 | 1.94 | 1.86 |
| DASS-Anxiety | 12.23(1.57) | 4.32(0.91) | 3.24(0.74) | 4.10(0.81) | 1.23 | 1.47 | 1.30 |
| DASS-Stress | 24.54(1.88) | 10.03(1.35) | 11.92(1.24) | 11.17(1.42) | 1.77 | 1.58 | 1.61 |
| Secondary Outcomes | |||||||
| BDI | 17.81(1.57) | 5.99(1.10) | 6.68(1.24) | 7.69(1.70) | 1.74 | 1.57 | 1.24 |
| QOLI | .48(0.42) | 2.04(0.35) | 1.99(0.43) | 2.05(0.37) | 0.81 | 0.71 | 0.79 |
| # of add. dx. | 1.12(0.18) | 0.47(0.16) | 0.28(0.13) | 0.41(0.23) | 0.76 | 1.07 | 0.69 |
| Mechanism of Change | |||||||
| AAQ | 74.77(2.41) | 53.23(2.58) | 54.03(2.42) | 52.82(2.23) | 1.65 | 1.63 | 1.80 |
| MAAS | 50.04(2.65) | 57.55(2.59) | 60.39(2.30) | 59.75(2.60) | 0.57 | 0.83 | 0.74 |
Note. GAD= generalized anxiety disorder, CSR = Clinician’s Severity Rating from the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version; PSWQ = Penn State Worry Questionnaire; DASS-Anxiety = Depression and Anxiety Stress Scales-Anxiety subscale; DASS-Stress = Depression and Anxiety Stress Scales- Stress subscale; BDI = Beck Depression Inventory; QOLI = Quality of Life Inventory; AAQ = Acceptance and Action Questionnaire; MAAS = Mindful Attention and Awareness Scale.
Preliminary Analyses
Means and standard deviations of all outcome variables at pre- and post- are reported in Table 2. No significant pre-treatment differences between conditions emerged for 8 of 9 outcome/mechanism of change variables (ts < 1.03, ps >.10); waiting list participants reported significantly higher PSWQ scores at pre- (t = 2.70, p <.05).
Controlled Trial
Results of multi-level regression analyses of the controlled trial data are presented in Table 3. The controlled effect sizes for condition by time interactions for primary and secondary outcomes were medium to large with significant condition by time interactions for clinician rated GAD severity, PSWQ, and DASS-Stress, and the BDI. The condition by time interaction for DASS-Anxiety, the QOLI, and number of additional diagnoses approached, but did not reach, significance. Significant condition by time interactions of large effect also emerged for the AAQ and the MAAS, measures of potential mechanisms of change.10
Table 3.
Multi-level regression effects of Time (Pre- to Post-treatment) and Condition by Timea for primary and secondary outcomes and mechanism of change variables
| B | t | pr | p | d | |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| GAD CSR | |||||
| Time | -.37 | -1.07 | 0.35 | .292 | .30 |
| Condition X Time | -2.19 | -4.78 | 0.21 | <.001 | 1.32 |
| PSWQ | |||||
| Time | -3.09 | -2.98 | 0.75 | .005 | .83 |
| Condition X Time | -8.45 | -3.66 | 1.78 | .001 | 1.02 |
| DASS-Anxiety | |||||
| Time | -1.75 | -.88 | 1.13 | .385 | .25 |
| Condition X Time | -5.26 | -1.91 | 1.16 | .062 | .53 |
| DASS-Stress | |||||
| Time | 2.93 | .89 | 0.96 | .378 | .25 |
| Condition X Time | -13.01 | -3.29 | 1.13 | .002 | .92 |
| Secondary Outcomes | |||||
| BDI | |||||
| Time | -3.17 | -2.58 | 1.19 | .013 | .72 |
| Condition X Time | -8.56 | -3.80 | 1.96 | .001 | 1.06 |
| QOLI | |||||
| Time | -.11 | -.30 | 1.55 | .801 | .07 |
| Condition X Time | 1.27 | 2.00 | 0.41 | .051 | .56 |
| # of add. diagnoses | |||||
| Time | .14 | .62 | 0.28 | .537 | .17 |
| Condition X Time | -.56 | -1.94 | 0.21 | .058 | .54 |
| Mechanism of Change | |||||
| AAQ | |||||
| Time | -.93 | -.55 | 1.11 | .586 | .15 |
| Condition X Time | -16.86 | -4.21 | 1.16 | <.001 | 1.18 |
| MAAS | |||||
| Time | .08 | .05 | 0.99 | .965 | .02 |
| Condition X Time | 8.38 | 2.94 | 0.86 | .007 | 1.04 |
Note. GAD= generalized anxiety disorder, CSR = Clinician’s Severity Rating from the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version; PSWQ = Penn State Worry Questionnaire; DASS-Anxiety = Depression and Anxiety Stress Scales- Anxiety subscale; DASS-Stress = Depression and Anxiety Stress Scales- Stress subscale; BDI = Beck Depression Inventory; QOLI = Quality of Life Inventory; AAQ = Acceptance and Action Questionnaire; MAAS = Mindful Attention and Awareness Scale.
Waiting list control is the reference condition.
At post-treatment/waiting list, 76.92% of those treated compared with 16.67 % of those on the wait-list no longer met criteria for GAD (χ2 = 9.08, p <.01). We adapted procedures used by Borkovec and colleagues (2002) and others to determine the clinical significance of change among those treated. Responder status was defined as a reduction of 20% or more on at least three of the four anxiety measures (GAD Severity, PSWQ, DASS-Anxiety, and DASS-Stress). Individuals were considered to demonstrate high end-state functioning if they fell into the normative range (within one standard deviation of published norms or a 3 or lower on GAD-CSR; Ladouceur et al., 2000) on at least three of these four measures. At post-treatment/waiting list, 75% of participants in the treatment condition and 8.3 % of the wait-list condition met criteria for responder status, (χ2 = 10.97, p <.01) and 75% of treated participants vs. 8.3 % of those in the wait-list condition met criteria for high end-state functioning, (χ2 = 10.97, p <.01).
Maintenance of Treatment Response
Means and standard errors of all variables at pre-, post-, and 3-month and 9-month follow-up and uncontrolled effect sizes for all participants who began treatment are presented in Table 4. Multi-level regression analyses of change revealed significant decreases in GAD severity, PWSQ, DASS-Stress, DASS-Anxiety, BDI, number of additional diagnosis, and AAQ scores, and significant increases in MAAS and QOLI scores, from pre- to post-treatment (all ps <.001). Growth curve analyses (reported in Table 5) indicated that treatment gains were maintained for all outcomes (i.e., nonsignificant coefficients of time), while worry scores continued to decrease modestly during follow up. However, the effect size of time on DASS-stress was medium, suggesting a modest increase in these symptoms over time.11
Table 5.
Results of growth curve analyses of maintenance of treatment gains for full sample of participants who began treatment (n = 26)
| B | t | pr | p | d | |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| GAD CSR | -.05 | -.31 | .28 | .756 | .08 |
| PSWQ | -1.85 | -1.72 | 1.43 | .091 | .47 |
| DASS-Anxiety | .01 | .03 | .90 | .974 | .01 |
| DASS-Stress | 1.13 | 1.55 | .51 | .127 | .43 |
| Secondary Outcomes | |||||
| BDI | .72 | 1.12 | .52 | .286 | .31 |
| QOLI | -.06 | -.38 | .27 | .706 | .11 |
| # of add. diagnoses | -.03 | -.23 | .24 | .818 | .06 |
| Mechanism of Change | |||||
| AAQ | -.36 | -.33 | 1.16 | .746 | .09 |
| MAAS | .99 | .88 | .77 | .384 | .25 |
Note. GAD= generalized anxiety disorder, CSR = Clinician’s Severity Rating from the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version; PSWQ = Penn State Worry Questionnaire; DASS-Anxiety = Depression and Anxiety Stress Scales- Anxiety subscale; DASS-Stress = Depression and Anxiety Stress Scales- Stress subscale; BDI = Beck Depression Inventory; QOLI = Quality of Life Inventory; AAQ = Acceptance and Action Questionnaire; MAAS = Mindful Attention and Awareness Scale.
The proportions of participants meeting criteria for diagnostic change, responder status, and high end-state functioning across the sample of participants who received treatment are reported in Table 6. To examine the impact of attrition on clinical significance, we also calculated these indicators carrying forward the last available value from post through follow up.
Table 6.
Percentage of treated participants (n = 23) meeting criteria for diagnostic change, responder status, and high endstate functioning at Post-, and 3-month and 9-month Follow-up (with percentages including last available values carried forward in italics)
| Post | 3 Month | 9 Month | |
|---|---|---|---|
| Diagnostic Change | 78.26(18 of 23) | 84.21(16 of 19) | 76.47(13 of 17) |
| 78.26(18 of 23) | 73.91 (17 of 23) | ||
| Responder Status | 77.27(17 of 22) | 83.33(15 of 18) | 80.00(12 of 15) |
| 78.26 (18 of 23) | 78.26 (18 of 23) | ||
| High Endstate | 77.27(17 of 22) | 94.44(17 of 18) | 86.67(13 of 15) |
| 82.61 (19 of 23) | 78.26 (18 of 23) |
Discussion
This initial study revealed promising findings for ABBT for GAD. Using conservative ITT analyses in this small sample, treatment had a significant (large) effect on GAD-specific outcomes as well as depressive symptoms. Marginally significant effects (of medium size) were revealed on self-reported anxious arousal symptoms, quality of life, and clinician-rated additional diagnoses. Initial support was found for the proposed mechanisms of change in ABBT as the treatment had a significant effect on both experiential avoidance and mindfulness. The changes associated with treatment appear to be clinically significant and durable. No significant deterioration was observed from post through nine month follow-up. Seventy-seven percent of the treated sample met criteria for high end-state functioning and responder status at post-assessment and these proportions were stable through 3- and 9-month follow-up.
Given the preliminary nature of this study, several limitations should be noted. The use of a waiting list control comparison does not rule out the possible influence of nonspecific factors. Three participants began taking medication over the course of the study, although evidence for significant, durable effects of treatment diminished only slightly when those participants were dropped from analyses. Longer follow-up periods are needed to assure durability of treatment gains. Also, given that the sample largely self-identified as White, we need to determine the efficacy and acceptability of ABBT across clients from diverse racial and ethnic backgrounds.
Although reliability of clinician severity ratings (a primary outcome measure) at pre-assessment was good, the reliability of GAD diagnoses during the time period of this study was less than desirable. Also, we did not assess reliability of post and follow-up assessments and reliability of GAD diagnosis. Further, although assessors were not informed of treatment condition, we did not confirm that they were blind to condition. Most of the CARD assessors were uninvolved with the study, but three therapists were also CARD assessors (not for their own clients) and could have been biased by a loyalty to the study. Similarly, adherence ratings done by graduate students could have been biased by allegiance.
Efforts were made to study an externally valid sample, including using limited exclusionary criteria and altering DSM-IV hierarchy rules to include individuals who met criteria for GAD solely within the course of MDD. Using a diagnostically heterogeneous sample could minimize between group effects. Further, the absence of competency ratings raises the possibility that treatment effects are underestimated due to poor competency in delivery of the intervention.
Considerable future research is needed to determine the specificity, generalizability, and mechanisms of change underlying the effects observed here; first and foremost, comparison to an active treatment is needed. Such a trial is currently underway. In the meantime, these findings provide initial support for the potential efficacy of an ABBT approach to treating GAD.
Figure 1.
CONSORT flow chart of client enrollment and disposition.
Table 7.
Multi-level regression effects of Time (Pre- to Post-treatment) and Condition by Timea for primary and secondary outcomes and mechanism of change variables in the completer sample (N = 25)
| B | t | pr | p | d | |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| GAD CSR | |||||
| Time | -.42 | -1.22 | 0.33 | .231 | 0.36 |
| Condition X Time | -2.04 | -4.49 | 0.22 | <.001 | 1.32 |
| PSWQ | |||||
| Time | -2.70 | -2.74 | 0.74 | .009 | 0.81 |
| Condition X Time | -8.42 | -3.68 | 1.83 | .001 | 1.83 |
| DASS-Anxiety | |||||
| Time | -2.00 | -0.95 | 1.13 | .348 | 0.25 |
| Condition X Time | -5.26 | -1.91 | 1.16 | .113 | 0.48 |
| DASS-Stress | |||||
| Time | 2.83 | .82 | 0.97 | .417 | 0.24 |
| Condition X Time | -12.73 | -3.09 | 1.11 | .004 | 0.92 |
| Secondary Outcomes | |||||
| BDI | |||||
| Time | -3.42 | -2.89 | 0.97 | .006 | 0.86 |
| Condition X Time | -8.68 | -3.82 | 1.97 | .001 | 1.14 |
| QOLI | |||||
| Time | -0.07 | -0.15 | 1.80 | .883 | 0.06 |
| Condition X Time | 1.37 | 2.03 | 0.43 | .048 | 0.61 |
| # of add. diagnoses | |||||
| Time | 0.17 | 0.72 | 0.26 | .474 | 0.21 |
| Condition X Time | -0.55 | -1.91 | 0.21 | .062 | 0.56 |
| Mechanism of Change | |||||
| AAQ | |||||
| Time | -1.58 | -1.02 | 1.31 | .315 | 0.30 |
| Condition X Time | -15.97 | -3.99 | 1.15 | <.001 | 1.18 |
| MAAS | |||||
| Time | .36 | 0.19 | 0.97 | .849 | 0.07 |
| Condition X Time | 7.81 | 2.71 | 0.87 | .011 | 0.99 |
Note. GAD= generalized anxiety disorder, CSR = Clinician’s Severity Rating from the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version; PSWQ = Penn State Worry Questionnaire; DASS-Anxiety = Depression and Anxiety Stress Scales- Anxiety subscale; DASS-Stress = Depression and Anxiety Stress Scales- Stress subscale; BDI = Beck Depression Inventory; QOLI = Quality of Life Inventory; AAQ = Acceptance and Action Questionnaire; MAAS = Mindful Attention and Awareness Scale.
Waiting list control is the reference condition.
Table 8.
Multi-level regression effects of Time (Pre to Post-treatment) and Condition by Timea for primary and secondary outcomes and mechanism of change variables in sample with post-treatment data from the two participants who changed medications during treatment dropped (N = 31)
| B | t | pr | p | d | |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| GAD CSR | |||||
| Time | -0.51 | -1.48 | 0.30 | .144 | 0.79 |
| Condition X Time | -2.03 | -4.27 | 0.24 | <.001 | 1.21 |
| PSWQ | |||||
| Time | -3.10 | -2.75 | 0.93 | .009 | 0.79 |
| Condition X Time | -7.50 | -3.26 | 1.61 | .002 | 0.93 |
| DASS-Anxiety | |||||
| Time | -1.08 | -0.53 | 1.07 | .600 | 0.15 |
| Condition X Time | -5.90 | -2.05 | 1.15 | .046 | 0.59 |
| DASS-Stress | |||||
| Time | 4.30 | 1.25 | 0.95 | .216 | 0.36 |
| Condition X Time | -14.63 | -3.54 | 1.12 | .001 | 1.18 |
| Secondary Outcomes | |||||
| BDI | |||||
| Time | -3.02 | -2.24 | 2.07 | .030 | 0.64 |
| Condition X Time | -8.20 | -3.47 | 1.63 | .001 | 0.99 |
| QOLI | |||||
| Time | -0.15 | -0.34 | 1.20 | .734 | 0.10 |
| Condition X Time | 1.27 | 1.89 | 0.44 | .064 | 0.54 |
| # of add. diagnoses | |||||
| Time | 0.07 | 0.29 | 0.40 | .777 | 0.08 |
| Condition X Time | -0.43 | -1.48 | 0.25 | .145 | 0.42 |
| Mechanism of Change | |||||
| AAQ | |||||
| Time | 0.28 | 0.18 | 0.97 | .861 | 0.05 |
| Condition X Time | -17.43 | -4.19 | 1.15 | <.001 | 1.20 |
| MAAS | |||||
| Time | 0.19 | 0.10 | 0.99 | .929 | 0.03 |
| Condition X Time | 7.01 | 2.37 | 0.89 | 0.02 | 0.87 |
Note. GAD= generalized anxiety disorder, CSR = Clinician’s Severity Rating from the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version; PSWQ = Penn State Worry Questionnaire; DASS-Anxiety = Depression and Anxiety Stress Scales- Anxiety subscale; DASS-Stress = Depression and Anxiety Stress Scales- Stress subscale; BDI = Beck Depression Inventory; QOLI = Quality of Life Inventory; AAQ = Acceptance and Action Questionnaire; MAAS = Mindful Attention and Awareness Scale.
Waiting list control is the reference condition.
Table 9.
Results of growth curve analyses of treatment maintenance for full sample of participants who began treatment, with data from individuals who changed medications during treatment or follow up dropped for time points subsequent to the change (N = 26)
| B | t | pr | p | d | |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| GAD CSR | 0.12 | 0.88 | 0.14 | .382 | 0.25 |
| PSWQ | -1.27 | -1.17 | 7.39 | .249 | 0.35 |
| DASS-Anxiety | 0.03 | 0.06 | 0.88 | .953 | 0.02 |
| DASS-Stress | 1.91 | 2.60 | 0.41 | .013 | 0.89 |
| Secondary Outcomes | |||||
| BDI | 1.22 | 1.65 | 0.50 | .106 | 0.49 |
| QOLI | -0.12 | -0.65 | 0.24 | .520 | 0.11 |
| # of add. diagnoses | 0.01 | 0.10 | 0.37 | .920 | 0.03 |
| Mechanism of Change | |||||
| AAQ | 0.45 | 0.28 | 0.89 | .709 | 0.11 |
| MAAS | 1.13 | 0.81 | 0.84 | .424 | 0.25 |
Note. GAD= generalized anxiety disorder, CSR = Clinician’s Severity Rating from the Anxiety Disorders Interview Schedule for DSM-IV, Lifetime Version; PSWQ = Penn State Worry Questionnaire; DASS-Anxiety = Depression and Anxiety Stress Scales- Anxiety subscale; DASS-Stress = Depression and Anxiety Stress Scales- Stress subscale; BDI = Beck Depression Inventory; QOLI = Quality of Life Inventory; AAQ = Acceptance and Action Questionnaire; MAAS = Mindful Attention and Awareness Scale.
Acknowledgments
This study was supported by NIMH Grant MH63208 to the first and second authors. Portions of these data were presented at the 2004 and 2007 annual meetings of the Association for Behavioral and Cognitive Therapies (formerly Association for Advancement of Behavior Therapy). The authors thank Dave Barlow, Tim Brown, and the staff at the Center for Anxiety and Related Disorders for their support of this research, and Tim Brown for assistance with revisions of this manuscript. We also thank Tom Borkovec and Steve Hayes for their helpful consultations. We thank our therapists, Laura Allen, Gabrielle Liverant, Jill Stoddard, Matthew Tull, and Yonit Schorr, as well as our clients, for sharing their experience and their wisdom with us. Finally, we also thank Laura Allen for her exceptional management of the project, Heidi Barrett-Model, Darren Holowka, and Matthew Tull for their therapy integrity ratings, and Shannon Erisman, Cathryn Freid, Michael Treanor, Matthew Tull, and Pete Vernig for their invaluable assistance with data management.
APPENDIX
CONSORT Checklist of items to include when reporting a randomized trial.
| PAPER SECTION And topic | Item | Description | Reported on Page # |
|---|---|---|---|
| TITLE & ABSTRACT | 1 | How participants were allocated to interventions (e.g., “random allocation”, “randomized”, or “randomly assigned”). | 2 |
| INTRODUCTION Background | 2 | Scientific background and explanation of rationale. | 3-4 |
| METHODS Participants | 3 | Eligibility criteria for participants and the settings and locations where the data were collected. | 4-6 |
| Interventions | 4 | Precise details of the interventions intended for each group and how and when they were actually administered. | 7 |
| Objectives | 5 | Specific objectives and hypotheses. | 4 |
| Outcomes | 6 | Clearly defined primary and secondary outcome measures and, when applicable, any methods used to enhance the quality of measurements (e.g., multiple observations, training of assessors). | 7-9 |
| Sample size | 7 | How sample size was determined and, when applicable, explanation of any interim analyses and stopping rules. | 8 |
| Randomization -- Sequence generation | 8 | Method used to generate the random allocation sequence, including details of any restrictions (e.g., blocking, stratification) | 6 |
| Randomization -- Allocation concealment | 9 | Method used to implement the random allocation sequence (e.g., numbered containers or central telephone), clarifying whether the sequence was concealed until interventions were assigned. | 6 |
| Randomization -- Implementation | 10 | Who generated the allocation sequence, who enrolled participants, and who assigned participants to their groups. | 6 |
| Blinding (masking) | 11 | Whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to group assignment. If done, how the success of blinding was evaluated. | 7,10 |
| Statistical methods | 12 | Statistical methods used to compare groups for primary outcome(s); Methods for additional analyses, such as subgroup analyses and adjusted analyses. | 19-20 |
| RESULTS Participant flow | 13 | Flow of participants through each stage (a diagram is strongly recommended). Specifically, for each group report the numbers of participants randomly assigned, receiving intended treatment, completing the study protocol, and analyzed for the primary outcome. Describe protocol deviations from study as planned, together with reasons. | 6, 8, 19 |
| Recruitment | 14 | Dates defining the periods of recruitment and follow-up. | 6 |
| Baseline data | 15 | Baseline demographic and clinical characteristics of each group. | 20-21 |
| Numbers analyzed | 16 | Number of participants (denominator) in each group included in each analysis and whether the analysis was by “intention-to-treat”. State the results in absolute numbers when feasible (e.g., 10/20, not 50%). | 8-9 |
| Outcomes and estimation | 17 | For each primary and secondary outcome, a summary of results for each group, and the estimated effect size and its precision (e.g., 95% confidence interval). | 23-24, 28-29 |
| Ancillary analyses | 18 | Address multiplicity by reporting any other analyses performed, including subgroup analyses and adjusted analyses, indicating those pre-specified and those exploratory. | |
| Adverse events | 19 | All important adverse events or side effects in each intervention group. | 4, 15 |
| DISCUSSION Interpretation | 20 | Interpretation of the results, taking into account study hypotheses, sources of potential bias or imprecision and the dangers associated with multiplicity of analyses and outcomes. | 10-11 |
| Generalizability | 21 | Generalizability (external validity) of the trial findings. | 10-11 |
| Overall evidence | 22 | General interpretation of the results in the context of current evidence. | 11 |
Footnotes
The study was conducted in compliance with the University of Massachusetts Boston, Boston University, Suffolk University, and Boston VA Healthcare System Institutional Review Boards. No adverse events were reported throughout the duration of the study.
Because prior trials have omitted individuals with co-morbid MDD, and the DSM hierarchical rules artificially limit comorbidity (Brown, Campbell, Lehman, Grisham, & Mancill, 2001), we chose to include individuals who met criteria for a current, principal diagnosis of GAD when the rule-out regarding occurring solely during the course of a mood disorder was suspended (i.e., a full six months of GAD symptoms without MDD was not required). These individuals did report that GAD symptoms caused them more severe distress and impairment than did MDD symptoms.
Nineteen clients received prior psychotherapy for anxiety, 3 for depression, and 19 had taken prior psychotropic medications for anxiety or mood problems. Seven participants (4 in the treatment condition) reported receiving a previous trial of CBT at some time before enrolling in the current study (2 for “anxiety”, one for depression, one for panic disorder with agoraphobia, one for GAD and OCD, one for OCD, and one for unspecified reasons). One client maintained intermittent contact (with no focus on CBT or anxiety) with a long-term psychotherapist throughout treatment and follow-up (once every two or three months).
Training includes instruction, observation of taped and live interviews, and administration of collaborative interviews. For certification, assessors must match with senior assessors on (1) identification of principal diagnosis(es), (2) CSR for principal diagnosis within 1 point, and (3) all additional diagnoses considered clinically significant, for three of five consecutive interviews, and must not commit administration errors. All assessors must attend a weekly consensus meeting to reduce drift and 10% of clients seen in the clinic receive double interviews in order to confirm and maintain reliability.
To establish internal consistency of measures within our sample, αs were calculated from the pre-treatment assessment administration.
Unfortunately, due to a clerical error, 5 domains were omitted from the measure (children, relatives (other than children or partners), home, neighborhood, and community), so the scores reflect responses to the 11 remaining domains (health, self-esteem, goals-and-values, finances, work, recreation, learning, creativity, social/community action, romantic relationship, friends). In a separate sample of 381 individuals recruited on an urban university campus, the full version of the QOLI was given. Scores were calculated for the full and shortened version of the questionnaire and these were correlated at .94, suggesting that scores from the version used in the current study can be seen as reliable estimates of full measure scores for this measure.
Treatment is described in more detail in Roemer and Orsillo (2005). Manual available upon request from the first author.
Results of completer analyses are available in online supplementary material.
Three participants began taking medications over the course of the study; two during therapy and one following post-assessment. The latter also began psychotherapy during the follow-up period. Analyses were conducted both including and excluding these participants.
Analyses repeated without the data from the two individuals who had not maintained a stable medication regimen during treatment were largely consistent, except that the condition by time interaction for number of additional diagnoses was no longer marginally significant (although, remained of medium to large effect). Full results are available in online supplementary material.
Analyses without data from the three individuals who had not maintained a stable medication regimen during follow-up were largely consistent, except that the marginally significant effect of time on the PSWQ was no longer significant and a significant effect of time (Cohen’s d = 0.78) on DASS-stress emerged, suggesting an increase in DASS-stress scores from post to 9-month follow up (although these scores were still significantly lower than scores at pre-treatment). Full results are available in online supplementary material.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at http://www.apa.org/journals/ccp/
Contributor Information
Lizabeth Roemer, Department of Psychology, University of Massachusetts Boston.
Susan M. Orsillo, Department of Psychology, Suffolk University and Department of Psychology, Boston University
Kristalyn Salters-Pedneault, National Center for Posttraumatic Stress Disorder, Boston VA Healthcare System and Department of Psychiatry, Boston University School of Medicine.
References
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford; 1979. [Google Scholar]
- Borkovec TD, Alcaine OM, Behar E. Avoidance theory of worry and generalized anxiety disorder. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorders: Advances in research and practice. New York: Guilford; 2004. pp. 77–108. [Google Scholar]
- Borkovec TD, Newman MG, Lytle R, Pincus A. A component analysis of cognitive behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Butler G, Gelder M, Hibbert G, Cullington A, Klimes I. Anxiety management: Developing effective strategies. Behaviour Research and Therapy. 1987;25:517–522. doi: 10.1016/0005-7967(87)90059-3. [DOI] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. Albany NY: Graywind Publications; 1994. [Google Scholar]
- Dunlop WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Frisch MB, Cornwell J, Villanueva M, Retzlaff PJ. Clinical validation of the Quality of Life Inventory: A measure of life satisfaction of use in treatment planning and outcome assessment. Psychological Assessment. 1992;4:92–101. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford; 1999. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG, Bissett RT, Pistorello J, Toarmino D, et al. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54:553–578. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Turk CL, Mennin DS. Generalized anxiety disorder: Advances in research and practice. New York: Guilford; 2004. [Google Scholar]
- Ladouceur R, Dugas MJ, Freeston MH, Leger E, Gagnon F, Thibodeau N. Efficacy of a new cognitive-behavioral treatment for generalized anxiety disorder: Evaluation in a controlled clinical trial. Journal of Consulting and Clinical Psychology. 2000;68:957–964. [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford; 1993. [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney: The Psychology Foundation of Australia; 1995. [Google Scholar]
- Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behaviour Research and Therapy. 2005;43:1281–1310. doi: 10.1016/j.brat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk A, Congdon R. HLM 6: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: Scientific Software International; 2005. [Google Scholar]
- Roemer L, Lee J, Salters-Pedneault K, Erisman S, Mennin DS, Orsillo SM. Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. 2008 doi: 10.1016/j.beth.2008.04.001. Manuscript submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM. An acceptance based behavior therapy for generalized anxiety disorder. In: Orsillo SM, Roemer L, editors. Acceptance and mindfulness-based approaches to anxiety: Conceptualization and treatment. New York: Springer; 2005. pp. 213–240. [Google Scholar]
- Roemer L, Orsillo SM. An open trial of an acceptance-based behavior therapy for generalized anxiety disorder. Behavior Therapy. 2007;38:72–85. doi: 10.1016/j.beth.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford; 2002. [Google Scholar]
- Waters AM, Craske MG. Generalized anxiety disorder. In: Antony MM, Ledley DR, Heimberg RG, editors. Improving outcomes and preventing relapse in cognitive behavioral therapy. New York: Guilford; 2005. [Google Scholar]
- Wells A, Carter K. Preliminary tests of a cognitive model of generalized anxiety disorder. Behaviour Research and Therapy. 1999;37:585–594. doi: 10.1016/s0005-7967(98)00156-9. [DOI] [PubMed] [Google Scholar]
- Wilson KG, Murrell AR. Values work in acceptance and commitment therapy: setting a course for behavioral treatment. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York: Guilford; 2004. pp. 120–151. [Google Scholar]