INTRODUCTION
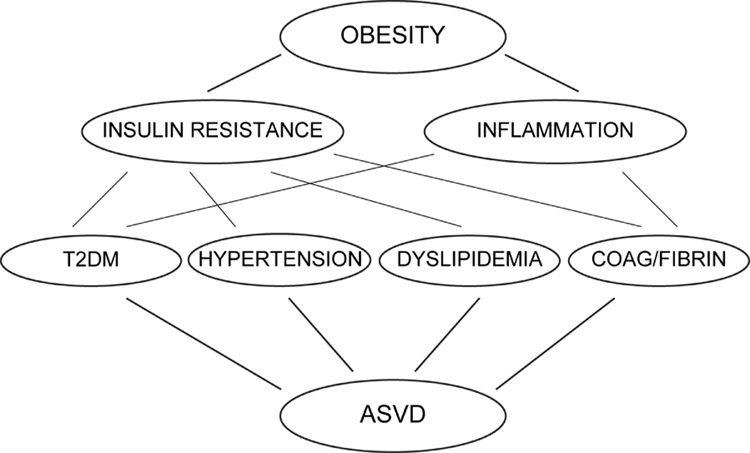
Obesity is closely associated with (peripheral as well as hepatic) insulin resistance (1) and with a low grade state of inflammation characterized by elevation of proinflammatory cytokines in blood and tissues (2). Both, insulin and inflammation, contribute to the development of type 2 diabetes (T2DM), hypertension, atherogenic dyslipidemias and disorders of blood coagulation and fibrinolysis. All these disorders are independent risk factors for atherosclerotic vascular disease (ASVD) such as heart attacks, strokes and peripheral arterial disease (3).
The reason why obesity is associated with insulin resistance is not well understood. In this chapter, I will review evidence demonstrating that free fatty acids (FFA) cause both insulin resistance and inflammation in the major insulin target tissues (skeletal muscle, liver and endothelial cells) and thus are an important link between obesity, insulin resistance, inflammation and the development of T2DM, hypertension, dyslipidemia, disorders of coagulation and ASVD (Figure 1).
Figure 1. Relationship between obesity, insulin resistance, inflammation and atherosclerotic vascular disease.
Obesity causes insulin resistance and a state of low grade inflammation. Both contribute to the development of several disorders, including T2DM, hypertension, dyslipidemia and disorders of coagulation and fibrinolysis which are independent risk factors for the development of atherosclerotic vascular disease. T2DM: Type 2 diabetes mellitus, ASVD: atherosclerotic vascular disease.
The central nervous system effects of FFA, including the demonstration that infusion of oleic acid into the third ventricle of rats reduced food intake and hepatic glucose production, are reviewed separately (see Chapter 4).
FFA AND INSULIN RESISTANCE
The recognition that adipose tissue not only stores and releases fatty acids but also synthesizes and releases a large number of other active compounds (4) has provided a conceptional framework which helps to understand how obesity can result in the development of insulin resistance. According to this concept, an expanding fat mass releases increasing amounts of compounds such as FFA, angiotensin 2, resistin, TNF-α, interleukin 6, interleukin 1-β and others. Some of these compounds, when infused in large amounts, can produce insulin resistance. However, any substance, in order to qualify as a physiological link between obesity and insulin resistance, should meet at least the following 3 criteria: 1) the substance should be elevated in the blood of obese people; 2) raising it’s blood level (within physiologic limits) should increase insulin resistance and 3) lowering it’s blood level should decrease insulin resistance. So far, only FFA can meet these 3 criteria in human subjects. Plasma FFA levels are elevated in most obese individuals (5); raising plasma FFA levels increases insulin resistance (6) and lowering of FFA improves insulin resistance (7).
FFA levels are elevated in obesity
Plasma FFA levels are usually elevated in obesity because 1) the enlarged adipose tissue mass releases more FFA and 2) FFA clearance may be reduced (8). Moreover, once plasma FFA levels are elevated, they will inhibit insulin’s anti-lipolytic action, which will further increase the rate of FFA release into the circulation (9).
Raising FFA increases insulin resistance
In skeletal muscle, acutely raising plasma FFA, for instance by infusing heparinized lipid emulsions, reduces insulin stimulated glucose uptake (more than 80% of which occurs in skeletal muscle) dose-dependently in all individuals irrespective of gender and age (6,10). Under these conditions, the insulin resistance develops within 2–4 h after plasma FFA levels increase and disappears within 4 h after normalization of FFA levels (11).
In the liver, FFA induced hepatic insulin resistance is more difficult to demonstrate because the liver is more insulin sensitive than skeletal muscle (12). Nevertheless, there is convincing evidence that physiological elevations of FFA, such as seen after a fat rich meal, inhibit insulin suppression of hepatic glucose production (HGP) resulting in an increase in HGP (1). Acutely (1–4 h), this rise in HGP is due to FFA mediated inhibition of insulin suppression of glycogenolysis (13). Longer lasting elevations of FFA, however, are likely to also increase gluconeogenesis.
In endothelial cells, IV infusion of insulin has been shown to increase nitric oxide production resulting in increased peripheral vascular blood flow (14,15). Physiological elevations of plasma FFA produce insulin resistance in endothelial cells by inhibiting the insulin induced increase in nitric oxide and blood flow (16).
Lowering FFA reduces insulin resistance
Chronically elevated plasma FFA levels, as commonly seen in obese diabetic and non-diabetic individuals, also cause insulin resistance. This could be demonstrated by normalizing elevated plasma FFA levels for only 12 h which resulted in normalization of insulin stimulated glucose uptake in obese non-diabetic individuals while improving insulin sensitivity from ~ ¼ to ~ ½ of normal in obese patients with T2DM (7). This suggested that high plasma FFA levels may have been the sole cause for insulin resistance in obese non-diabetic subjects but were responsible for only ~ 1/2 of the insulin resistance in obese patients with T2DM (7). Similar results have been reported in non-diabetic subjects genetically predisposed to T2DM (17).
Mechanisms of FFA Mediated Insulin Resistance
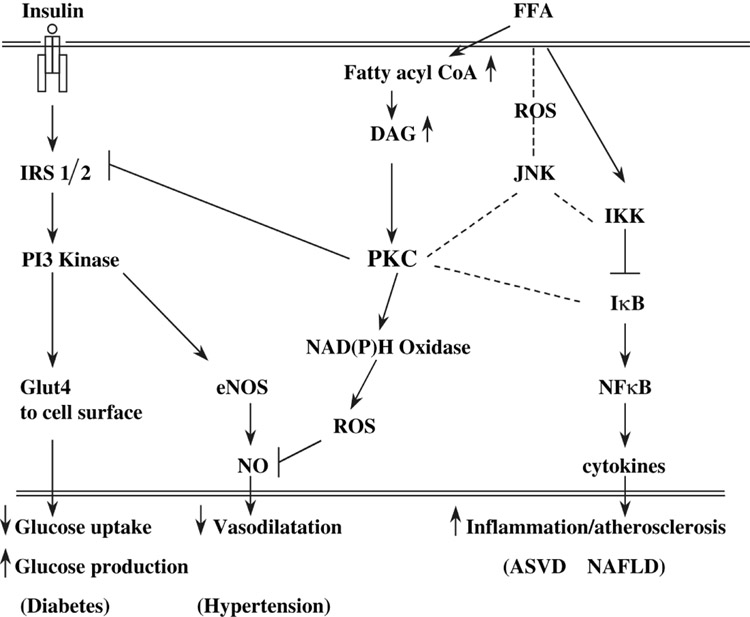
FFA have been shown to produce a defect in insulin stimulated glucose transport and/or phosphorylation which is caused by a defect in insulin signaling (10,18). Plasma FFA can easily enter cells where they are either oxidized to generate energy in the form of ATP or re-esterified for storage as triglycerides (TG). Not surprisingly, therefore, raising blood FFA levels result in intracellular (intramyocellular or intrahepatocellular) accumulation of triglycerides (19). For reasons that are not well understood, raising plasma FFA levels also results in accumulation of several metabolites involved in FFA re-esterification including longchain acyl-CoA and diacylglycerol (DAG) (20). DAG is a potent activator of conventional and novel protein kinase C isoforms (21). In addition to PKC, several other serine/threonine kinases including IKK-β and c-Jun NH2-terminal kinase (JNK) can also be activated by acutely raising plasma FFA levels (22,23). Exactly, how these kinases are activated by FFA is not clear but may include FFA mediated generation of reactive oxygen species (ROS) (24), activation of the Toll like receptor 4 (TLR4) pathway (25) or endoplasmic reticulum stress (23). Once activated, one or several of these serine/threonine kinases can interrupt insulin signaling by decreasing tyrosine phosphorylation of the insulin receptor substrate 1 or 2 (IRS 1/2) (26). This will inhibit the activity of the IRS/PI3 kinase/Akt pathway which controls most of insulin’s metabolic actions including glucose uptake, glycogen synthesis, glycogenolysis and lipolysis (27). The IRS/PI3 kinase/Akt pathway is also important for the activation of endothelial nitric oxide synthase (NOS) and the production of nitric oxide (NO). In addition, FFA can reduce NO production through a second mechanism, namely, by stimulation of NAD(P)H oxidase. This has been shown to occur in a PKC dependent manner, and will lead to increased production of reactive oxygen species (ROS) and a decrease in NO (24) (Figure 2).
Figure 2. Potential mechanisms of FFA-induced insulin resistance and inflammation.
The key event is an increase in plasma FFA concentration. This leads to the accumulation of fatty acid CoA and DAG, and activation of PKC in skeletal muscle, liver and vascular endothelial cells. It is assumed that activation of PKC interrupts insulin signaling by serine phosphorylation of IRS 1/2, resulting in a decrease in tyrosine phosphorylation of IRS 1/2. In endothelial cells, PKC has been shown to activate NAD(P)H oxidase, which produces reactive oxygen species and destroys NO. Elevation of plasma FFA levels also leads to the production of inflammatory and proatherogenic proteins through activation of the IKK/IκB-α/NFκB and JNK pathways. The broken lines indicate that activation of PKC by the IKK/IκB-α/NFκB pathway and by ROS is a possibility that has not yet been demonstrated in human muscle or liver. Increased FFA-induced insulin resistance reduces glucose uptake in muscle and increases glucose production in the liver. Together, this results in hyperglycemia. In endothelial cells, FFA-mediated insulin resistance results in decreased NO and decreased vasodilatation, which may contribute to the development of hypertension. In muscle and liver, FFA activation of the IKK/IκB-α/NFκB and JNK pathways results in low grade inflammation, which may promote ASVD and NAFLD. ASVD: atherosclerotic vascular disease; CoA: Coenzyme A; DAG: diacylglycerol; FFA: free fatty acids; IRS: insulin receptor substrate; NAD(P)H: nicotinamide adenine dinucleotide phosphate, reduced; NAFLD: non-alcoholic fatty liver disease; NFκB: nuclear factor κB; NO: nitric oxide; PI: phosphoinositide; PKC: protein kinase C; ROS: reactive oxygen species.
FFA may also interfere with insulin stimulation of glucose transport by modulating glucose transporter (Glut) gene transcription and mRNA stability (28,29)
FFA AND INFLAMMATION
Obesity is associated with elevated levels of proinflammatory cytokines and chemokines in the circulation and in tissues (2). As mentioned, the adipose tissue produces and releases a large number of cytokines and chemokines (collectively called adipokines) (4), some of which are proinflammatory. Recent studies have shed some light on the reasons for the increased release of proinflammatory cytokines in obesity. In one study, mice fed a high fat diet for 3 months developed low grade hepatic inflammation which was associated with increased production and secretion of several proinflammatory cytokines (30). This suggested that the inflammatory state was caused either by a component of the diet or by a substance released from the enlarged adipose tissue. FFA are good candidates for both possibilities because they are elevated in most obese individuals both during a fat meal (31) and under basal and postprandial conditions (5).
The recent demonstration that acute elevation of plasma FFA, in addition to producing peripheral and hepatic insulin resistance, also activated the proinflammatory NFκB pathway (20) resulting in increased hepatic expression of several proinflammatory cytokines including TNF-α, IL1-β, IL6 and an increase in circulating MCP-1 (22), supported the notion that FFA is a primary link between obesity or high fat feeding and the development of inflammatory changes (Figure 2). In this context, the increase in circulating MCP-1 in response to an acute rise in plasma FFA is particularly interesting because MCP-1 is well established to regulate macrophage recruitment to sites of inflammation (32). The rise in plasma MCP-1 levels, therefore, may explain the recent observation of macrophage infiltration into the adipose tissue of obese animals (33).
The early events leading from a rise in circulating FFA to activation of the NFκB pathway are not clear but include several possibilities. First, as discussed, an increase in plasma FFA results in intramyocellular accumulation of DAG and activation of several PKC isoforms (20,22). Gao et al. have recently shown that the FFA mediated activation of IKK (a kinase involved in the activation of NFκB) in fat cell was PKC dependent (34). Thus, DAG mediated PKC activation may be an upstream effector of NFκB activation. Second, some recent evidence suggests that FFA mediated activation of IKK and NFκB may be, at least partially, mediated by the Toll like receptor-4 (TLR-4) (25). The TLR-4 pathway, which is essential for the development of innate immunity to pathogens, triggers production of inflammatory cytokines (35). Thus, it appears that sensing of excess nutrients such as FFA and sensing of infectious pathogens, may use the same signaling pathway and result in the same downstream effects, i.e., inflammation. Third, obesity and FFA have been shown to induce endoplasmic reticulum stress which can result in activation of IKK, JNK and inflammatory responses (36) and lastly, several G protein coupled receptors, including GRP-40 and GRP-120 have been shown to bind FFA (37,38). There is as yet, however, no evidence that these receptors are involved in any of the FFA activities discussed here.
FFA AND THE METABOLIC SYNDROME
The increase in the metabolic syndrome (also called the insulin resistance syndrome) is mainly driven by the worldwide increase in obesity. Not surprisingly, therefore, obesity associated and fatty acid mediated insulin resistance is intimately connected with all major components of this syndrome, i.e., T2DM, hypertension and atherogenic dyslipidemia as well as other components that have not yet been formally included in the metabolic syndrome complex such as disorders of blood coagulation and fibrinolysis.
Type 2 diabetes (T2DM)
FFA mediated insulin resistance will result in the development of T2DM unless the insulin resistance is compensated by oversecretion of insulin. There is increasing evidence that FFA stimulate insulin secretion, acutely and chronically, and that FFA induced insulin resistance is compensated by FFA mediated oversecretion of insulin in obese but otherwise healthy individuals (39). However, in pre-diabetic individuals (subjects with inherited predisposition to develop T2DM including first degree relatives of patients with T2DM) this compensation fails and the consequence of FFA induced insulin resistance will be T2DM (17,39). This explains why only ~ 50% of all obese, insulin resistant individuals, namely those who are unable to compensate, will d1evelop T2DM during their lifetime (40).
Hypertension
FFA induced insulin resistance also reduces endothelial production of nitric oxide through PKC dependent activation of NAD(P)H oxidase, resulting in increased production of ROS (see page 5 and ref. 24). Nitric oxide deficiency decreases vasodilatation and promotes the development of hypertension.
Atherogenic Dyslipidemia
Obesity and insulin resistance are associated with increased production of VLDL-TG. A major factor for this is believed to be the increased flux of FFA to the liver in combination with insulin resistance associated hyperinsulinemia. The precise mechanism of this insulin resistance driven hepatic VLDL overproduction remains, however, uncertain (41).
Disorders of coagulation and fibrinolysis
Hyperinsulinemia, the hallmark of insulin resistance, is now recognized to create a procoagulant state in diabetic and non-diabetic individuals by increasing circulatory levels of tissue factor procoagulant activity, increased generation of thrombin, elevated plasma levels of coagulation factors VII and VIII and activation of platelets (42,43).
Obesity, insulin resistance and T2DM are also associated with impaired fibrinolysis (44). Plasma concentrations of plasminogen activator inhibitor 1 (PAI-1), which is the primary inhibitor of fibrinolysis, are increased in obese insulin resistant individuals and in patients with T2DM (45,46). PAI-1 downregulates fibrinolysis by inhibiting the production of plasmin and thus promotes thrombosis. PAI-1 is synthesized in endothelial cells and hepatocytes and is present in platelets and in plasma (Reviewed in ref. 47). In vitro, PAI-1 secretion is stimulated by insulin in human adipocytes and by FFAs in hepatocytes. Hence, elevated plasma FFA levels, via producing insulin resistance and hyperinsulinemia (with or without hyperglycemia), promote a state of increased tendency for thrombosis (see above) and decreased ability to lyse blood clots. Together, this increases the risk for acute vascular events.
FFA and matrix metalloproteinases
Smoking, together with the established, insulin resistance related risk factors for ASVD such as T2DM, hypertension, atherogenic dyslipidemia and disorders of blood coagulation and fibrinolysis probably cannot completely explain the obesity/insulin resistance related ASVD risk (48). This suggests that there may be other ways by which insulin resistance can increase this risk. Indeed, one such risk factor may be increased activity of several matrix metalloproteinases (MMPs). MMPs are enzymes with proteolytic activities against connective tissue proteins such as collagen, proteoglycans and elastin. They control degradation and remodeling of extracellular matrix. There is accumulating evidence that MMP-2, MMP-9 and MT-MMP play important roles in the development and progression of heart attacks, strokes, peripheral arterial disease and aortic aneurysms (49–52). We have recently found that acutely increasing plasma levels of FFA, particularly when combined with hyperinsulinemia, strongly increased the activities of MMP-2, MMP-9 and MT-MMP in rat aorta (53). As mentioned, FFA also promote the release of proinflammatory cytokines which are known to be potent stimulators of MMP synthesis and release (49). Thus, the combination of increased MMP activity and inflammatory cytokines may lead to progression of atherosclerotic lesions and contribute to the increased risk for cardiovascular disease in obese insulin resistant individuals.
FFA AS TARGET FOR THERAPY
Because insulin resistance is at the core of several serious health problems associated with obesity, insulin resistance should be a major focus of therapy. Whereas weight loss through diet and exercise is clearly the most desirable way to reduce insulin resistance in obese people, neither diet and exercise programs nor presently available pharmacological approaches have been very successful. As pointed out above, elevated plasma FFA levels are responsible for much of the insulin resistance in obese individuals. Therefore, normalizing plasma FFA levels can be expected to improve insulin sensitivity. In support, we have shown that normalization of plasma FFA levels overnight with Acipimox, a nicotinic analog, normalized insulin resistance in obese, non-diabetic subjects and improved insulin resistance in obese patients with T2DM (7). Nicotinic acid or longacting nicotinic acid analogs effectively lower plasma FFA levels. Unfortunately, their use is associated with a rebound of plasma FFA to very high levels (54), which makes this class of drugs unsuitable for the longterm control of plasma FFA. Thiazolidinediones (TZD) lower plasma FFA levels longterm and without rebound. They do this primarily by stimulating fat oxidation through a coordinated induction of genes in adipose tissue related to FFA uptake, binding, β-oxidation and oxidative phosphorylation (55). However, TZD mediated lowering of plasma FFA levels is modest, ranging from < 10% to approximately 20% in most studies (56,57). Moreover, this class of drug has several unwanted effects which limits their use (58). Fibrates, another class of lipid lowering drugs also lower plasma FFA levels modestly and without rebound primarily by stimulating fat oxidation in the liver (59). As both classes of drugs work in different organs (TZDs in fat and fibrates in the liver) and through different mechanisms (TZDs through activation of PPAR-γ and fibrates through activation of PPAR-α), their use in combination produces greater decreases in plasma FFA levels as well as greater improvements in insulin sensitivity than the use of either drug alone (60).
Lowering of plasma FFA, in addition to improving insulin sensitivity, may also prevent activation of the proinflammatory and proatherogenic NFκB pathway and thus may reduce the incidence of atherosclerotic vascular problems. Thus, the challenges for the future include the prevention or correction of obesity and elevated plasma FFA levels through methods that include decreased caloric intake and increased caloric expenditure, development of easy, fast and reliable methods to measure FFA in small blood samples (comparable to portable blood sugar monitoring devices) and development of efficient pharmacological approaches to normalize increased plasma FFA levels.
SYNOPSIS
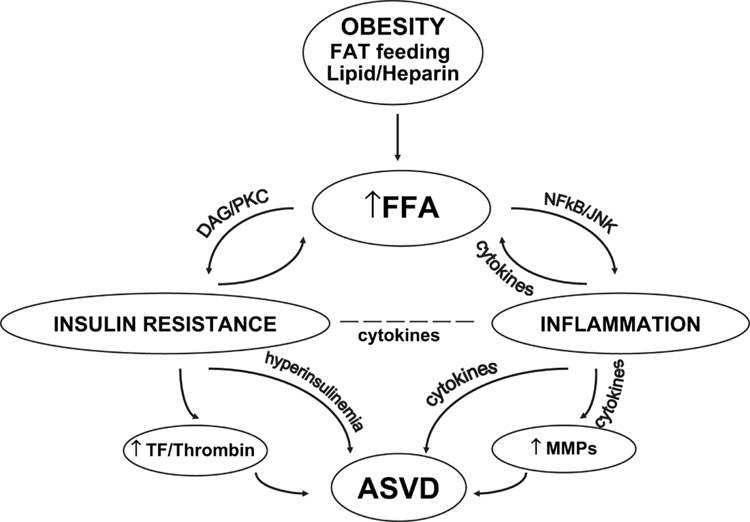
Plasma FFA levels are elevated in obesity. FFA cause insulin resistance in all major insulin target organs (skeletal muscle, liver, endothelial cells) and have emerged as a major link between obesity, the development of the metabolic syndrome and atherosclerotic vascular disease. Mechanisms through which FFA induce insulin resistance involve intramyocellular and intrahepatic accumulation of diacylglycerol and triglycerides, activation of several serine/threonine kinases, reduction of tyrosine phosphorylation of the insulin receptor substrate 1/2 (IRS 1/2) and impairment of the IRS/phosphatidylinositol 3 kinase pathway of insulin signaling. FFA also produce low grade inflammation in skeletal muscle, liver and fat through activation of the nuclear factor-κB and the c-Jun NH2 terminal kinase (JNK) pathways, resulting in release of proinflammatory and proatherogenic cytokines. In addition, FFA contribute to cardiovascular events by promoting a prothrombotic state by reducing fibrinolysis and by activating platelets and arterial matrix metalloproteinases (Figure 3).
Figure 3. Summary of relation between obesity, FFA and ASVD.
Obesity, fat feeding and lipid heparin infusion all raise plasma FFA levels. Elevated plasma FFA produce insulin resistance via DAG/PKC by decreasing insulin signaling at the IRS 1/2 level. Insulin resistance promotes ASVD via chronic hyperinsulinemia, a state of increased tendency to blood coagulation and decreased fibrinolysis and by mechanisms not shown here including hypertension, and atherogenic dyslipidemia. Elevated plasma FFA also cause inflammation via activation of the NFκB and JNK pathways. Inflammation can promote ASVD by increasing the production of inflammatory cytokines and by activation of MMPs. ASVD: atherosclerotic vascular; DAG: diacylglycerol; JNK: c-jun NH2 terminal kinase; MMP: matrix metalloproteinases; PKC: protein kinase C; TF: tissue factor
ACKNOWLEDGEMENTS
We thank Maria Mozzoli, BS and Karen Kresge, BS for technical assistance and Constance Harris Crews for typing the manuscript.
This work was supported by National Institutes of Health grants RO1-DK-68895, RO1-HL-733267 and RO1-DK-066003.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Boden G. Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes. 1997;46:3–10. [PubMed] [Google Scholar]
- 2.Tataranni PA, Ortega E. A Burning Question. Does an adipokines-induced activation of the immune system mediate the effect of overnutrition on type 2 diabetes? Diabetes. 2005;54:917–927. doi: 10.2337/diabetes.54.4.917. [DOI] [PubMed] [Google Scholar]
- 3.Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89:2583–2589. doi: 10.1210/jc.2004-0535. [DOI] [PubMed] [Google Scholar]
- 4.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548–2556. doi: 10.1210/jc.2004-0395. [DOI] [PubMed] [Google Scholar]
- 5.Reaven GM, Hollenbeck C, Jeng C-Y, et al. Measurement of plasma glucose, free fatty acid, lactate and insulin for 24 h in patients with NIDDM. Diabetes. 1988;37:1020–1024. doi: 10.2337/diab.37.8.1020. [DOI] [PubMed] [Google Scholar]
- 6.Boden G, Chen X, Ruiz J, et al. Mechanisms of fatty acid-induced inhibition of glucose uptake. J Clin Invest. 1994;93:2438–2446. doi: 10.1172/JCI117252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Santomauro ATMG, Boden G, Silva M, et al. Overnight lowering of free fatty acids with acipimox improves insulin resistance and glucose tolerance in obese diabetic and nondiabetic subjects. Diabetes. 1999;48:1836–1841. doi: 10.2337/diabetes.48.9.1836. [DOI] [PubMed] [Google Scholar]
- 8.Bjorntorp P, Bergman H, Varnauskas E. Plasma free fatty acid turnover in obesity. Acta Med Scand. 1969;185:351–356. doi: 10.1111/j.0954-6820.1969.tb07347.x. [DOI] [PubMed] [Google Scholar]
- 9.Jensen MD, Haymond MW, Rizza RA, et al. Influence of body fat distribution on free fatty acid metabolism in obesity. J Clin Invest. 1989;83:1168–1173. doi: 10.1172/JCI113997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boden G, Chen X. Effects of fat on glucose uptake and utilization in patients with non-insulin-dependent diabetes. J Clin Invest. 1995;96:1261–1268. doi: 10.1172/JCI118160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boden G, Jadali F, White J, et al. Effects of fat on insulin stimulated carbohydrate metabolism in normal men. J Clin Invest. 1991;88:960–966. doi: 10.1172/JCI115399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rizza RA, Mandarino LJ, Gerich JE. Dose-response characteristics for effects of insulin on production and utilization of glucose in man. Am J Physiol. 1981;240:E630–E639. doi: 10.1152/ajpendo.1981.240.6.E630. [DOI] [PubMed] [Google Scholar]
- 13.Boden G, Cheung P, Stein TP, et al. FFA cause hepatic insulin resistance by inhibiting insulin suppression of glycogenolysis. Am J Physiol. 2002;283:E12–E19. doi: 10.1152/ajpendo.00429.2001. [DOI] [PubMed] [Google Scholar]
- 14.Baron AD. Insulin resistance and vascular function. J Diabetes Complications. 2002;16:92–102. doi: 10.1016/s1056-8727(01)00209-4. [DOI] [PubMed] [Google Scholar]
- 15.Zeng G, Nystrom FH, Ravichandran LV, et al. Roles for insulin receptor, PI3-kinase and Akt in insulin-signaling pathways related to production of nitric oxide in human vascular endothelial cells. Circulation. 2000;101:L1539–L1545. doi: 10.1161/01.cir.101.13.1539. [DOI] [PubMed] [Google Scholar]
- 16.Steinberg HO, Tarshoby M, Monestel R, et al. Elevated circulating free fatty acid levels impair endothelium-dependent vasodilation. J Clin Invest. 1997;100:1230–1239. doi: 10.1172/JCI119636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cusi K, Kashyap S, Gastaldelli A, et al. Effect on insulin secretion and insulin action of a 48-h reduction of plasma free fatty acids with acipimox in nondiabetic subjects genetically predisposed to type 2 diabetes. Am J Physiol Endocrinol Metab. 2007;292:E1775–E1781. doi: 10.1152/ajpendo.00624.2006. [DOI] [PubMed] [Google Scholar]
- 18.Dresner A, Laurent D, Marcucci M, et al. Effects of free fatty acids on glucose transport and IRS-1 associated phosphatidylinositol 3-kinase activity. J Clin Invest. 1999;103:253–259. doi: 10.1172/JCI5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boden G, Lebed B, Schatz M, et al. Effects of acute changes of plasma free fatty acids on intramyocellular fat content and insulin resistance in healthy subjects. Diabetes. 2001;50:1612–1617. doi: 10.2337/diabetes.50.7.1612. [DOI] [PubMed] [Google Scholar]
- 20.Itani SI, Ruderman NB, Schmieder , et al. Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IκB-α. Diabetes. 2002;51:2005–2011. doi: 10.2337/diabetes.51.7.2005. [DOI] [PubMed] [Google Scholar]
- 21.Farese R. In: Diabetes Mellitus: a Fundamental and Clinical Text. LeRoith D, Taylor SI, Olefsky JM, editors. Philadelphia: Lippincott; 2000. pp. 239–251. [Google Scholar]
- 22.Boden G, She P, Mozzoli M, et al. Free fatty acids produce insulin resistance and activate the proinflammatory nuclear factor-κB pathway in rat liver. Diabetes. 2005;54:3458–3465. doi: 10.2337/diabetes.54.12.3458. [DOI] [PubMed] [Google Scholar]
- 23.Hotamisligil GS. Role of endoplasmic reticulum stress and c-Jun NH2-terminal kinase pathways in inflammation and origin of obesity and diabetes. Diabetes. 2005;54:S73–S78. doi: 10.2337/diabetes.54.suppl_2.s73. [DOI] [PubMed] [Google Scholar]
- 24.Inoguchi T, Li P, Umeda F, et al. High glucose level and free fatty acid stimulate reactive oxygen species production through protein kinase C-dependent activation of NAD(P)H oxidase in cultured vascular cells. Diabetes. 2000;49:1939–1945. doi: 10.2337/diabetes.49.11.1939. [DOI] [PubMed] [Google Scholar]
- 25.Shi A, Kokoeva V, Inouye K, et al. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest. 2006;116:3015–3025. doi: 10.1172/JCI28898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu C, Chen Y, Cline GW, et al. Mechanism by which fatty acids inhibit activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J Biol Chem. 2002;277:50230–50236. doi: 10.1074/jbc.M200958200. [DOI] [PubMed] [Google Scholar]
- 27.Saltiel AR, Kahn CR. Insulin signaling and the regulation of glucose and lipid metabolism. Nature. 2001;414:799–806. doi: 10.1038/414799a. [DOI] [PubMed] [Google Scholar]
- 28.Long SD, Pekala PH. Regulation of Glut4 gene expression by arachidonic acid. Evidence for multiple pathways, one of which requires oxidation to prostaglandin. E J Biol Chem. 1996;271:1138–1144. doi: 10.1074/jbc.271.2.1138. [DOI] [PubMed] [Google Scholar]
- 29.Armoni M, Harel C, Bar-Yoseph F, et al. Free fatty acids repress the Glut4 gene expression in cardiac muscle via novel response elements. J Biol Chem. 205;280:34786–34795l. doi: 10.1074/jbc.M502740200. [DOI] [PubMed] [Google Scholar]
- 30.Xu H, Barnes GT, Yang Q, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112:1821–1830. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van Oostrom AJ, van Dijk H, Verseyden C, et al. Addition of glucose to an oral fat load reduces postprandial free fatty acids and prevents the postprandial increase in complement component 31–3. Am J Clin Nutr. 2004;79:5–10. doi: 10.1093/ajcn/79.3.510. [DOI] [PubMed] [Google Scholar]
- 32.Rollins BJ, Walz A, Baggiolini M. Recombinant human MCP-1/JE induces chemotaxis, calcium flux, and the respiratory burst in human monocytes. Blood. 1991;78:1112–1116. [PubMed] [Google Scholar]
- 33.Weisberg SP, McCann D, Desai M, et al. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–1808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gao Z, Zhang X, Zuberi A, et al. Inhibition of insulin sensitivity by free fatty acids requires activation of multiple serine kinases in 3T3-L1 adipocytes. Molecular Endocrinology. 2004;18:2024–2034. doi: 10.1210/me.2003-0383. [DOI] [PubMed] [Google Scholar]
- 35.Medzhitov R. Toll-like receptors and innate immunity. Nat Rev Immunol. 2001;1:135–145. doi: 10.1038/35100529. [DOI] [PubMed] [Google Scholar]
- 36.Ozcan U, Cao Q, Yilmaz E, et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science. 2004;306:457–461. doi: 10.1126/science.1103160. [DOI] [PubMed] [Google Scholar]
- 37.Hirasawa A, et al. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR 120. Nat Med. 2005;1:90–94. doi: 10.1038/nm1168. [DOI] [PubMed] [Google Scholar]
- 38.Itoh Y, Kawamata Y, Harada M, et al. Free fatty acids regulate insulin secretion from pancreatic beta cells through GPR40. Nature. 2003;422:173–176. doi: 10.1038/nature01478. [DOI] [PubMed] [Google Scholar]
- 39.Boden G. Free fatty acids and insulin secretion in humans. Current Diabetes Reports. 2005;5:167–270. doi: 10.1007/s11892-005-0004-5. [DOI] [PubMed] [Google Scholar]
- 40.Benjamin SM, Valdez R, Geiss LS, et al. Estimated number of adults with prediabetes in the US in 2000: opportunities for prevention. Diabetes Care. 2003;26:645–649. doi: 10.2337/diacare.26.3.645. [DOI] [PubMed] [Google Scholar]
- 41.Bamba V, Rader DJ. Obesity and atherogenic dyslipidemia. Gastroenterology. 2007;132:2181–2190. doi: 10.1053/j.gastro.2007.03.056. [DOI] [PubMed] [Google Scholar]
- 42.Boden G, Rao AK. Effects of hyperglycemia and hyperinsulinemia on the tissue factor pathway of blood coagulation. Current Diabetes Reports. 2007;7:223–227. doi: 10.1007/s11892-007-0035-1. [DOI] [PubMed] [Google Scholar]
- 43.Boden G, Vaidyula VR, Homko C, et al. Circulating tissue factor procoagulant activity and thrombin generation in patients with type 2 diabetes: Effects of insulin and glucose. J Clin Endocrinol Metab. 2007;92 doi: 10.1210/jc.2007-0933. 0000-0000, in press. [DOI] [PubMed] [Google Scholar]
- 44.Vague P, Juhan-Vague I, Aillaud MF, et al. Correlation between blood fibrinolytic activity, plasminogen activator inhibitor level, plasma insulin level and relative body weight in normal and obese subjects. Metabolism. 1986;35:250–253. doi: 10.1016/0026-0495(86)90209-x. [DOI] [PubMed] [Google Scholar]
- 45.Pannacciulli N, De Mitrio R, Giorgino R, et al. Effect of glucose tolerance status on PAI-1 plasma levels in overweight and obese subjects. Obes Res. 2002;10:717–725. doi: 10.1038/oby.2002.98. [DOI] [PubMed] [Google Scholar]
- 46.Festa A, D’Agostino R, Jr, Tracy RP, et al. Elevated levels of acute-phase proteins and plasminogen activator inhibitor-1 predict the development of type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetes. 2002;51:1131–1137. doi: 10.2337/diabetes.51.4.1131. [DOI] [PubMed] [Google Scholar]
- 47.Sobel BE, Schneider DJ. Platelet function, coagulopathy, and impaired fibrinolysis in diabetes. Cardiol Clin. 2004;22:511–526. doi: 10.1016/j.ccl.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 48.Hennekens CH. Increasing burden of cardiovascular disease: current knowledge and future directions for research on risk factors. Circulation. 1998;97:1095–1102. doi: 10.1161/01.cir.97.11.1095. [DOI] [PubMed] [Google Scholar]
- 49.Newby AC. Dual role of matrix metalloproteinases (Matrixins) in intimal thickening of atherosclerotic plaque rupture. Physiol Rev. 2005;85:1–31. doi: 10.1152/physrev.00048.2003. [DOI] [PubMed] [Google Scholar]
- 50.Galis ZS, Sukhova GK, Lark MW, et al. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Invest. 1994;94:2493–2503. doi: 10.1172/JCI117619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pasterkamp G, Schoneveld AH, Hijnen DJ, et al. Atherosclerotic arterial remodeling and the localization of macrophages and matrix metalloproteinases 1, 2 and 9 in the human coronary artery. Atherosclerosis. 2000;150:245–253. doi: 10.1016/s0021-9150(99)00371-8. [DOI] [PubMed] [Google Scholar]
- 52.Longo GM, Xiong W, Greiner TC, et al. Matrix metalloproteinases 2 and 9 work in concert to produce aortic aneurysms. J Clin Invest. 2002;110:625–632. doi: 10.1172/JCI15334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boden G, Song W, Pashko L, Kresge K. In vivo effects of insulin and free fatty acids on matrix metalloproteinases in rat aorta. Diabetes. 2007 doi: 10.2337/db07-1261. in press. [DOI] [PubMed] [Google Scholar]
- 54.Chen X, Iqbal N, Boden G. The effects of free fatty acids on gluconeogenesis and glycogenolysis in normal subjects. J Clin Invest. 1999;103:365–372. doi: 10.1172/JCI5479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Boden G, Homko C, Mozzoli M, et al. Thiazolidinediones upregulate fatty acid uptake and oxidation in adipose tissue of diabetic patients. Diabetes. 2005;54:880–885. doi: 10.2337/diabetes.54.3.880. [DOI] [PubMed] [Google Scholar]
- 56.Ghazzi MN, Perez JE, Antonucci TK, et al. Cardiac and glycemic benefits of troglitazone treatment in NIDDM: the Troglitazone Study Group. Diabetes. 1997;46:433–439. doi: 10.2337/diab.46.3.433. [DOI] [PubMed] [Google Scholar]
- 57.Maggs DG, Buchanan TA, Burant CF, et al. Metabolic effects of troglitazone monotherapy in type 2 diabetes mellitus. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1998;128:176–185. doi: 10.7326/0003-4819-128-3-199802010-00002. [DOI] [PubMed] [Google Scholar]
- 58.Boden G, Zhang M. Recent findings concerning thiazolidinediones in the treatment of diabetes. Expert Opin Investig Drugs. 2006;15:243–250. doi: 10.1517/13543784.15.3.243. [DOI] [PubMed] [Google Scholar]
- 59.Staels B, Fruchart J-C. Therapuetic roles of peroxisome proliferator-activated receptor agonists. Diabetes. 2005;54:2460–2470. doi: 10.2337/diabetes.54.8.2460. [DOI] [PubMed] [Google Scholar]
- 60.Boden G, Homko C, Mozzoli M, et al. Combined use of rosiglitazone and fenofibrate in patients with type 2 diabetes. Prevention of fluid retention. Diabetes. 2007;56:248–255. doi: 10.2337/db06-0481. [DOI] [PubMed] [Google Scholar]