Abstract
The overarching goal of medical training is to nurture the growth of knowledgeable, caring and insightful clinicians guided by the ideals of medical professionalism. Recent definitions of professional competence identify essential clinical skills, including cognitive expertise, emotional competence, and reflective capacity. This modern framework reflects the increasingly complex nature of the patient-clinician interaction, in which the clinician must exchange diagnostic information while supportively engaging the patient on a deeper, affective level. The affective dimension can be particularly potent when pain is the primary symptom, as it is for the majority of medical visits. Unfortunately, however, current models of professionalism, used as an early guide for medical trainees to develop an understanding of the clinical exchange, largely focus on interactions in the cognitive domain. To emphasize the importance of emotions in professional development, we propose the Cognitive and Emotional Preparedness Model (CEPM), which describes the clinical encounter occurring on two channels, one cognitive and the other emotional, and stresses the importance of multidimensional development in preparing the clinician to 1) communicate clinical information, 2) provide emotional support, and 3) actively reflect on experiences for continued improvement. Together, acquisition of knowledge, emotional development, and reflective skill will improve the clinical interaction.
Perspective
The proficiency of medical trainees in developing clinical skills profoundly shapes patient satisfaction and treatment outcomes. This article reviews the cognitive, emotional and reflective development of medical trainees and presents a model illustrating how clinical development impacts pain care. For improved efficacy, pain education should be calibrated to students' developmental needs.
Keywords: Professionalism, competence, medical education, patient-physician interaction, empathy, compassion, psychosocial
Introduction
Medical training is intended to produce clinicians who meet accepted standards of professional competence. As defined recently, professional competence consists of seven core features, including knowledge acquisition, emotional development, and reflection 18. Despite growing awareness of the complexities of professional competence, most medical schools focus on knowledge-based learning to the exclusion of these broader challenges. Emotional development and reflective preparation are often viewed as supplementary and expected to develop with time 42. Research indicates that although the standard medical curriculum successfully increases declarative knowledge, fostering the development of emotional competence and reflective capacity may be more difficult. Indeed, standard clinical training may actually erode desirable characteristics such as empathy and skillfulness of communication 25,27.
Pain is a common symptom in clinical practice that places special demands on medical trainees because of its inherent negative emotional impact. Studies indicate that the emotional features of pain can impede successful management and that emotionally competent care results in better outcomes for pain and other symptoms 15,16. Consequently, pain assessment, although a common clinical task, deeply tests professional competence, requiring both expert knowledge and emotional development. We highlight pain here to illustrate the challenges that clinicians face in comprehensive symptom-oriented assessment and care.
In an effort to understand how clinicians develop professional competence, we created the Cognitive and Emotional Preparedness Model. This model is derived from 1) new definitions of professional competence, 2) research on cognition and empathy, and 3) observations of novice and expert physician-patient interactions. The literature on professional competence identifies the qualities of knowledge acquisition, emotional development, and reflective capacity, as well as communication, technical skill, clinical reasoning, and values as essential to physician competence18. At the neurobiological level there is additional support for incorporating both cognitive and emotional components into models of clinical interaction; functional MRI research indicates enhanced activity of neural networks hypothesized to support cognition and emotion during periods of pain-reponsive empathy in experimental subjects 28. Finally, medical educators have recognized the importance of emotion for effective patient-physician relationships 41. In teaching encounters with student clinicians, we have observed frustration, suspicion, and dysphoric mood following interactions with patients expressing negative emotions related to pain, while clinical experts completed a pain-care encounter with a period of reflection. In this paper, we review the literature on models of patient-physician interaction, examine how medical trainees develop relevant professional competencies, describe the application of the model, and discuss implications for future research and education. This model was previous presented in abstract form at the 2005 IASP meeting 33.
Background
During the first two years of medical school, tremendous focus is placed on the science of medicine. Students dedicate hundreds of hours to scientific study and advance by completing required examinations. The latter two years of medical school typically focus on acquiring the skills of clinical evaluation, management, and diagnostic reasoning. Thus as training proceeds, emphasis is directed to acquisition of declarative knowledge and physical technical skills. Nonetheless, the ability to provide patients with emotional support and the capacity for self-reflection are similarly essential qualities that should develop and be demonstrated for advancement. Medical schools have typically addressed this issue by presenting pre-clinical students with lectures on medical professionalism, where models of archetypal physician-patient interactions are described. More recently innovative methods promoting professionalism have been implemented including the 'colleges' movement, the development of relationship-centered care and the use of narrative medicine 1,10,21. A conceptual framework for evaluating these approaches is needed.
Traditionally, the leading approach to understanding patient-physician interactions assigned physicians a dominant role, while patients were tasked with compliance 37. However, social restructuring, advances in medical science, and emergence of the allied health professions eroded support for the traditional approach. In response, researchers sought better models of increasingly complex clinical interactions. In this context, a four-fold classification system was developed by Emanuel and Emanuel in which the patient-physician relationship is categorized into four distinct models—Paternalistic, Deliberative, Interpretive, Informative—distinguished by the exchange of medical information and decision-making responsibilities 17. The Paternalistic Model closely reflects the traditional approach, in which the physician decides which actions must be taken to preserve the patient’s interests. In stark contrast is the Informative Model, for which patient autonomy is inviolate: the physician serves as a conduit of diagnostic information and the patient makes decisions with minimal assistance. The Interpretive and Deliberative Models are intermediates between the above extremes. These intermediate approaches are characterized by discussion and collaborative decision-making. The Interpretive Model provides patients with medical information and the physician helps patients to clarify their values. In the Deliberative Model, the physician attempts to educate the patient with respect to accepted health-affirming values related to the condition. Through discussion and deliberative dialogue, the doctor describes selected treatment alternatives and may attempt to persuade the patient toward appropriate healthcare decisions by taking on the role of teacher or guide.
Alternative models of physician-patient interaction have subsequently been developed. Charles et al. emphasized that variables in clinical interactions, e.g., the exchange of information and patient sovereignty, fall on a continuum rather than at discrete points 9: thus three distinct approaches—paternalistic, shared, and informed—serve as descriptive landmarks on a spectrum. Degner and Sloan created a system of three models—patient active, collaborative, and passive—including paired situational comparisons to guide patients in choosing the best approach 14. Other models considered more specific variables, including the role of severity of the patient’s condition 29, family and third party involvement in decision-making 5, and physician interaction and patient coping style 26. Current approaches to teaching the patient-physician interaction emphasize shared decision making.
These models have guided many medical students and physicians in improving clinical skills, and yet are inadequate for most clinical encounters because they do not consider emotional effects. Pain in particular is an internal experience with profound influence on mood and behavior. As physician and patient endeavor to exchange information, emotions can dominate the clinical encounter, frustrating communication. Traditional models do not address this emotional exchange and physicians relying on the traditional models may fail those patients with emotionally distressing symptoms. Studies have shown that almost 30% of patients with pain symptoms are unhappy with the communication and empathy offered by their physician 50. Moreover, patients generally disclose less information about their condition and voice fewer concerns when their doctors fail to communicate effectively or show concern 47. Clearly, a model recognizing the complex nature of patient-physician interactions is necessary. In this report, we propose a model that incorporates cognitive skill acquisition and emotional development as well as the capacity for reflective insight. We proceed by briefly reviewing the development of medical trainees in the domains of cognition, emotion, and reflection.
Development of Cognitive Expertise
Existing models of patient-physician interaction pre-suppose the physician possesses a body of expert knowledge. A developmental model that considers how the presence or absence of cognitive expertise affects the patient-physician interaction may provide valuable insight. Assessing the impact of cognitive expertise becomes essential when pain is the focus because most students are not well versed in pain and pain care 36.
It is well established, as evidenced by the universal use of standardized tests of knowledge for medical licensure, that medical trainees develop cognitive expertise during and after medical school 48. Establishment and maintenance of this knowledge base is widely accepted as absolutely necessary and most medical specialty boards now require periodic retesting for continuation of certification 46. Acquisition of knowledge and cognitive expertise by medical trainees has been studied extensively and important features of the process have been identified and are organized in Table 1. Cognitively-skilled medical trainees manifest important common abilities including: possessing an elaborated structure of knowledge, using semantic skills such as abstraction of details, and early problem representation 8,34. An example of elaborated knowledge structure is the student who can identify the primary features of migraine headache and contrast these with the features of meningitis-related headache. Cognitively-skilled trainees are generally better at reaching correct diagnoses. Important clinical skills are additionally characteristic of skilled medical trainees, including thorough characterization of the chief complaint, clarification of ambiguous information, use of summarizing to confirm understanding, and development of a directed line of questioning 22. Pain-related examples of these skills are provided in Table 1. Thus there is a reasonably solid basis for assessing cognitive preparation for the clinical encounter, both in terms of a well-developed conceptual framework, and the process of assessing skillfulness in cognitively-based communication. Currently, much research focuses on defining effective methods for teaching the cognitively-based skills of medicine.
Table 1.
Components of Cognitive expertise required of Medical Trainees
| Area of expertise | Cognitive expertise components | Examples of specific skills |
|---|---|---|
| Knowledge | Basic and Clinical science content | Most common causes of forefoot pain |
| Elaborated knowledge structure | Chest pain ➔ MI ➔ thrombolysis ➔ risk for bleeding ➔ vigilance for mental status | |
| Relevant information | Sore throat: Antibiotics active for Strept | |
| Semantic skill | Abstraction of details | 40 year old means ‘middle-aged’ |
| Early problem representation | ‘This is a middle-aged male with lower extremity pain following inactivity.’ | |
| Information gathering | Directed line of inquiry | Hand pain: Has the patient had recent trauma? Infection? Insect bites? |
| Attention to appropriate details | ‘How many hours after your recent surgery did this pain begin?’ | |
| Clarification of ambiguous information | ‘Precisely how many pills did you take?’ | |
| Narrative skill | Thorough characterization of chief complaint | ‘Chest pain that is 9/10, crushing, substernal, began this morning and…’ |
| Summarizing to confirm understanding | ‘You are telling me that your arm pain began 1 week ago…’ | |
| Explanation of clinical information to the patient and others involved in care | ‘Peripheral neuropathy is a degeneration of the nerves that do to different parts…’ | |
| Diagnostic Reasoning | Generation of differential diagnosis | MI, aortic rupture, esophageal spasm… |
| Evaluation of data for relevance to putative diagnoses | ‘Does this fever make appendicitis more likely as a cause of abdominal pain?’ | |
| Inclusion of appropriate elements in the physical exam | ‘Should I perform a Phalen's maneuver?’ | |
| Interpretation of exam findings | ‘This is rebound tenderness, it means….’ |
Development of Emotional Competence
Medical students face many challenges to emotional development during their four years of medical school. Some of these challenges are intrinsic to their development as young adults, while others are particular to the medical school experience. Changes in mood during medical school have been analyzed specifically for depression and substance abuse 13,39,45, and it is recognized that medical students as a group show a significant increase in depressive symptoms, particularly in the latter part of their second year of training 11. Additionally, medical students as a group increase intake of alcohol during training and become prone to actual substance abuse 35. Less attention has been paid to defining the events of normal emotional development 20. Medical students, because of their prolonged status as students and the extremely insulating nature of medical training, may not follow the typical developmental patterns of young adulthood 6. Nonetheless, specific ‘milestones’, i.e., emotionally powerful experiences, strongly influence the typical medical student’s emotional growth. Table 2 illustrates when some of these emotionally evocative events might occur during a typical medical school experience. The emotional reactions brought on by milestones will vary from student to student, but for many, the effects are profound. Although often these experiences elicit negative emotions: anxiety, sadness, grief, and frustration, others are profoundly positive. Given these emotional burdens, it seems paradoxical that little is known about the best means of supporting students through these formative events.
Table 2.
Selected emotionally evocative events influencing Medical Student development
| Year 1 | Integration into a new peer group Adaptation to high work expectations Encountering a corpse in the anatomy lab Management of conflicting demands on time |
| Year 2 | First patient encounter Learning about symptoms without developing them Increased risk for depression and academic fatigue Accepting the requirements of professionalism Maintenance of social supports |
| Year 3 | Adjustment to role on clinical team, low status Negotiating response of significant others to new role Identification of appropriate mentors and role models Learning to advocate for patients, respond to needs Choosing an area of medicine that is most rewarding |
| Year 4 | Assumption of responsibility Loss of idealism Management of substance use, avoidance of overuse Interviewing for and selecting internship/residency Responding to medical student abuse in self or others Learning the possibilities and limitations of medical care |
The desirable emotional qualities of medical school graduates include compassion and empathy, emotional intelligence, emotional resilience, and conscientiousness, Table 3. Among these, empathy is advanced as absolutely essential for professional competency. Although it has been proposed that empathy is the cognitive capacity for identifying with another’s experience 24, empathy is more broadly defined as '…vicariously experiencing the feelings, thoughts, and experience of another…' 32. Many simply identify empathy with caring 44. More precisely however, compassion, defined as a 'deep awareness of the suffering of another coupled with' the desire to alleviate it, represents a deeper motivational commitment to clinical excellence 32. Both compassion and empathy are first formed in the early years of life, long before entry into medical school. The goal of medical training then is to cultivate these appropriate emotional responses and the expression of these in the clinical interaction. Because compassion and empathy are perhaps best learned by seeing one’s feelings mirrored by a ‘caring other’, it is unlikely that a medical educational process completely unconcerned for the emotional suffering of medical students could engender empathy or compassion. The task of medical training, however, is broader: Physicians must learn to recognize their own emotional responses to patients and develop strategies for both facilitating and inhibiting these responses, a process often termed ‘emotional intelligence’30. An example in the clinical setting might be a medical student's deep sadness in response to a patient with poorly controlled cancer pain. A prompting comment such as 'How does it feel for you to see this patient?' can provide an opportunity for self-awareness and growth. Emotional resilience is an important characteristic that allows the medical trainee to adapt quickly, responding calmly in emotionally turbulent situations, regulating mood and building emotional reserves, and tolerating ambiguity or uncertainty 49. An example of this can be openly discussing best responses to the angry or frustrated pain patient. Conscientiousness is a fundamental personality characteristic that encompasses diligence and thoughtfulness toward and the ability to prioritize the needs of others and respond to those in need.
Table 3.
Components of emotional qualities needed by Medical Trainees
| Emotional quality | Components of that quality |
|---|---|
| Emotional strength | Empathetic perception of another's emotional state |
| Compassion and Caring | |
| Ability to experience loss and also to celebrate success | |
| Emotional intelligence | Perception of emotions in others and self |
| Anticipation of normal emotional reactions | |
| Recognition of aberrant emotions | |
| Emotional resilience | Maintenance of emotional reserves |
| Tolerance of uncertainty or ambiguity | |
| Capacity to de-escalate emotionally charged situations | |
| Emotional regulation | Prioritizing the needs of others over self when appropriate |
| Conscientiousness and a sense of duty | |
| Willingness to work diligently and postpone rewards |
As a whole, there is no uniform approach to cultivating emotional development based on theories of development. Empirical approaches include ready availability of mental health services, group therapy approaches, mindfulness-based stress reduction, problem-based learning with emphasis on communication and, perhaps most innovatively, the use of guided exposure to opera as an emotive medium. Each of these studies reports varied degrees of efficacy, but none have achieved widespread use. It has been observed that the standard curriculum actually attenuates student empathy and medical trainees experience an additional loss of empathy during their arduous first-year of work experience. Clearly, improved attention to the emotional development of medical trainees is critical to the delivery of effective pain care.
Development of Reflective Capacity
Medical education is characterized by an extreme density of study and clinical involvement, with little time for trainees to reflect on the medical experience. Students may encounter patients with disabling pain repeatedly during their medical training but fail to fully recognize the impact of pain on daily life and the extent of suffering engendered by pain. Thus despite multiple time pressures, students need to develop reflective capacity, i.e., the ability to engage in measured self-appraisal of one's internal and external experiences in the clinical encounter, especially one's thoughts, feelings, actions and behaviors; with the goals of improving patient care and strengthening professional competence. An example of reflection-in-practice is the fourth year medical student, who upon assessing a patient with painful small fiber neuropathy concluded that the problem was psychosomatic because a cursory neurological exam did not include testing for pinprick hyperalgesia. This student needs to be assigned both knowledge and skill-focused exercises and as well as receiving instructions to reflect on enhancing compassionate concern and avoiding diagnostic hubris. Reflective capacity is important both for the patient and clinician. Research has shown medical students experience a decrease of idealism over the course of their training 25,51, and a large number of physicians suffer from emotional burnout and compassion fatigue 38,40. Denying medical students the opportunity to develop reflective skills thus minimizes their potential for emotional growth and may have long-term negative effects on career satisfaction.
Fortunately, recent studies have shown that, despite anticipated difficulties in teaching reflective capacity, appropriate skills can indeed be cultivated by encouraging clinicians to actively engage the humanistic dimensions of medicine 31 and gain insight into their own feelings and attitudes 4. To accomplish this, institutions have turned to large- and small-group discussions, implemented student self-assessments, and introduced other exercises to encourage growth in these areas 3,4,31. In one promising approach, interns were relieved of direct patient responsibilities and instructed to observe and reflect on clinical care rendered by others 19. An important, although labor intensive, method for inculcating reflective capacity is role-modeling 12. This approach has been effectively implemented through the creation of an academic core faculty who devote extensive teaching time to the transmission of professional values 21. Intriguingly, it is the process of turning inward through reflection that strengthens the ability of medical trainees to re-focus their medical encounters on the other and develop effective therapeutic relationships. Over the course of a career, reflective insight has the potential to enhance a physician's fulfillment as a health-focused professional with improved capacity to pursue an intellectually rewarding, emotionally satisfying career and increased efficacy through relationship-centered care.
The Cognitive and Emotional Preparedness Model
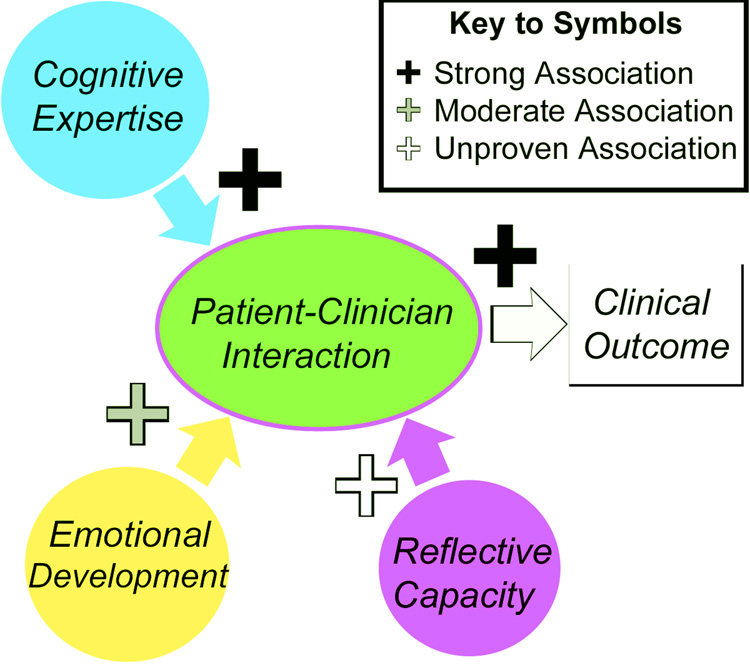
The Cognitive and Emotional Preparedness Model (CEPM) is a conceptual description of the clinical encounter. It incorporates the influence of cognitive expertise, emotional development and reflective capacity, Figure 1. The model envisions information exchange between patient and clinician occurring on two analogous but distinct channels: one cognitive, the other emotional. Ideally the physician operates comfortably in both domains during the encounter and reflects internally on the information gathered and the experience of the encounter. Too often, however, the young clinician is unprepared in the cognitive and/or emotional domains and lacks the reflective skills needed to address deficiencies. Although most medical schools provide knowledge-based training for a variety of medical conditions, formal symptom-focused education in important areas such as pain may be limited. Thus, the description of the model begins with the recognition that in some cases, foundations of expert knowledge about symptom-focused encounters may be absent.
Figure 1. Operational diagram of the model.
Cognitive expertise, Emotional development and Reflective capacity all contribute to the patient-physician interaction. The strength of evidence supporting these associations is indicated by the color of the symbols. Cognitive expertise has a clear impact on patient-physician interactions, there is good evidence to support a role for emotional skills as well. More research is needed to assess the impact of reflective capacity.
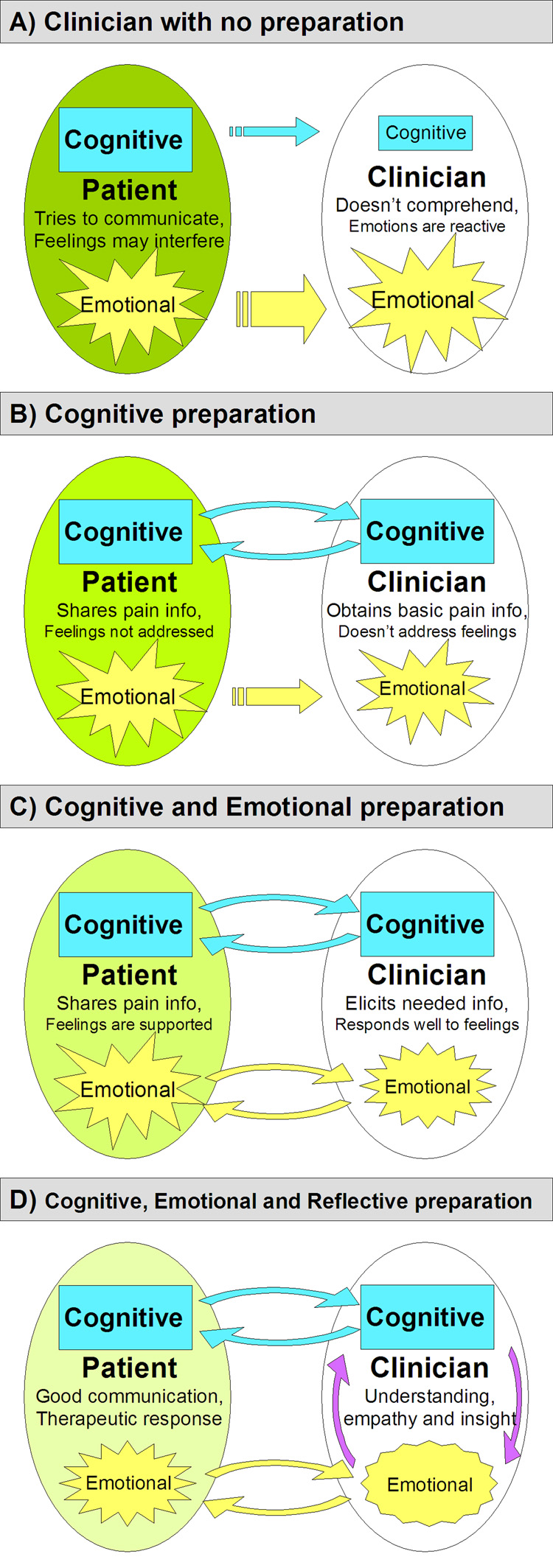
At the beginning of clinical training, medical trainees lack both cognitive preparation and essential knowledge (Figure 2A). At this stage, the clinician does not recognize important information intrinsic to the details of sensory symptoms. In the model diagram, cognitive under-development is represented by a small blue rectangle. The blue ‘cognitive’ communication arrow is small, indicating a general failure of communication, and unidirectional indicating lack of clinician feedback. The clinician is unable to frame the clinical encounter as an opportunity to gather diagnostic clues, misses the opportunity for probing questions that facilitate exchange, and fails to recognize key symptom features. Simultaneously, symptom-associated emotions are expressed by the patient. Complications arise if the patient perceives an absence of cognitive feedback, negative feelings may be amplified, potentially overwhelming other communication and estranging the clinician. This emotional outpouring is represented by a large yellow arrow that leads toward a reactive emotional domain within the clinician. Because the clinician is unable to provide empathy, fails to effectively engage the patient, and may react negatively to the patient’s display of symptom-associated feelings, it is likely that the interaction ends quickly, contributing to inadequate treatment and dissatisfaction.
Figure 2. The Cognitive and Emotional Preparedness Model.
A) Clinician with no preparation. Communication is unidirectional. Clinician’s cognitive domain is underdeveloped as shown by small blue rectangle and the clinician’s emotional experience is reactive, large yellow burst-shape. Details in text. B) Clinician with Cognitive Preparation. Information exchange is bi-directional and productive but affective support for the patient is not provided. C) Clinician with Cognitive and Emotional Preparation. Information exchange is bi-directional and patient experiences emotional support regarding their medical condition. D) Clinician with Cognitive, Emotional and Reflective Preparation. Communication is highly effective in terms of information exchange and emotional support, the reflective clinician is able to continue personal growth and professional development. Note: Because the model represents features of developing clinical expertise not necessarily limited to physicians, the term ‘clinician’ is used in the figure and throughout the text description of the model.
For the clinician exposed to a standard, fact-focused curriculum, the cognitive domain will be more developed. In this scenario (Figure 2B), the clinician is cognitively prepared and carefully characterizes the patient’s symptoms; descriptive detail and scientific fact are shared between patient and clinician. Characteristically, the clinician with cognitive preparation asks carefully formulated questions, engages in discovering features of the condition as clues to diagnosis, and uses the information to form a differential diagnosis. The clinician can utilize this exchange of objective information to establish improved, if limited, communication, and the patient may derive important benefit from the clinician’s perceived interest. The clinician may experience some satisfaction from developing a successful line of diagnostic inquiry. Nonetheless, this clinician is unprepared to address the emotional aspects of the encounter. The potent affective burden of pain and other medical conditions, including distress, frustration, and isolation, continue to perturb the clinical encounter. Standard models of physician-patient interaction do not prepare the young clinician to understand the complexities of an emotionally-charged exchange. When not addressed, the affective nature of pain and other symptoms will increase the risk of alienation and limit potential for the patient and clinician to work together in evaluation and treatment.
The cognitively- and emotionally-prepared clinician (Figure 2C) is comfortable with the cognitive content of the interaction and readily acknowledges the patient's emotional experiences. In the cognitive domain, the clinician asks appropriate questions, extracts relevant information, and formulates a differential diagnosis. Additionally, this clinician anticipates the emotional experiences of the patient and has acquired an understanding of the negative emotional responses associated with medical illness. The physician may still feel sad in response to the situation but is much less likely to end the encounter prematurely. The emotionally prepared clinician establishes therapeutic communication with the patient on the affective level, and can provide the empathy and compassionate support that patients need. As a result, the potential for full patient engagement and establishment of an effective clinical relationship is greatly expanded. The clinician maximizes communication, and builds strong foundations of trust with the patient.
In the final scenario, the clinician is cognitively and emotionally prepared to care for the patient and has also developed the capacity for reflection (Figure 2D). Such clinicians actively assess their internal responses to cognitive interactions as well as to emotional exchanges. This leads to a more comprehensive understanding of situations and enables a sustained clinical effort in this challenging clinical area. In the setting where expert knowledge is reflectively synthesized with preparation in the emotional domain, the clinician can address comprehensively the complex needs of the patient. This clinician will ask appropriate questions, listen attentively, provide explanations, and attend to the differential diagnosis. This clinician interprets, supports, and guides the patient’s emotional response to their condition, is skilled at communicating in the emotional domain, and empathizes appropriately with the patient. This clinician plans for reflective assessment, allows for appropriate self-care, and cultivates opportunities for professional and personal development. Thus, the cognitively-, emotionally- and reflectively-prepared clinician can communicate fluidly on cognitive as well as emotional levels, and grow through reflection. We hypothesize that this clinician is more likely to provide the patient with an ideal clinical experience and attain sustainable high levels of professional competence.
Discussion
The Cognitive and Emotional Preparedness Model highlights cognitive expertise, emotional preparation, and reflective capacity as critical components of the clinical experience. While other models of medical professionalism have been proposed, most explore and acknowledge only a single dimension of the physician-patient interaction. Successful clinical practice, however, is achieved through mastery of many dimensions.
Developing cognitive proficiency has traditionally been the dominant focus of medical education, reflecting the reasonable belief that extensive familiarity with medical fact is central to a physician’s ability to treat patients. As cited, research has reinforced this theory, with cognitively prepared physicians performing better than those less well prepared. Therefore, an indispensable first step is improving pain-focused knowledge acquisition in medical schools and in the ongoing education of medical trainees and physicians in practice.
The medical community is now acknowledging the necessity of emotional competence in the clinical sphere. As all clinicians are placed in situations that challenge their emotional strength, training to prepare for these situations is invaluable. This is evident through research. Di Blasi and colleagues found that when emotional and cognitive care were provided simultaneously, significant improvements in speed of recovery and decreased levels of symptoms resulted 15. In contrast, cognitive interventions alone showed weak, if any correlation to health status. Hojat et al. showed empathy correlated with clinical competence and clerkship performance, whereas cognitive measures, such as grade point average or standardized test performance, did not 23. In the pain-focused clinical encounter, emotional development allows clinicians to consistently exhibit compassion and empathy while shaping emotional responses to foster constructive communication. An important challenge is identifying those medical school applicants that exhibit appropriate emotional capacities. The phenomenon of the emotionally-underdeveloped medical student is an open secret of academic medicine and current approaches such as requiring letters of recommendation and personal interviews, seem equipped only to cull out those candidates with the most glaring interpersonal deficiencies. Our model suggests that a structured approach to emotional assessment may be more successful in this respect.
Reflective skill development allows clinicians to deeply appreciate their role and counteract the emotional demands of a career in medicine. Research has shown the continual emotion al weight shouldered by doctors often takes a significant and disturbing toll 2. One study found that some 30% of physicians identified to some extent with burnout, defined as emotional exhaustion, depersonalization, and low personal accomplishment 7. Similarly, in a study by Shanafelt et al., 87% of the respondents met burnout criteria, and compared to those who did not, reported higher levels of providing sub-optimal care 43. Pain is by its nature exhausting and has the potential to overwhelm poorly prepared clinicians. Encouraging reflection during medical school and beyond allows physicians to revisit their patient encounters, mistakes and successes, and evaluate how these situations could have been handled better for the patient, and for themselves. Although some institutions have established programs to strengthen these skills, more progress is needed in understanding the development of reflective capacity, especially regarding the optimal delivery of pain care.
Future directions include testing the model and it's components in clinical trainees at various stages of development. Because the model is derived from accepted definitions of professional competence, we believe it can be used immediately to educate medical trainees about the complexities of clinical interactions as well as being applied to assessing applicants for medical school readiness. Educational methods that address the emotional and reflective development of medical students, clinical trainees and practicing clinicians are an area that will require extensive additional research. Resources for the systematic development of innovative educational approaches are a critical need. We conclude that balanced development of each competence will lead to more effective relationship-centered care for patients and clinicians seeking to alleviate pain.
Acknowledgments
The authors thank Drs. James N. Campbell, David Niv (now deceased), Robert Shochet, Christina Spellman, and Scott M. Wright for many helpful discussions of this work. This work was supported in part by grants from the Mayday Fund and the Blaustein Pain Fund (BBM). Dr. Murinson receives support from the Johns Hopkins Clinical Skills Colleges Advisory Program and from the NIH (5K08NS048146).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Beach MC, Inui T. Relationship-centered care. A constructive reframing. J Gen Intern Med. 2006;21 Suppl 1:S3–S8. doi: 10.1111/j.1525-1497.2006.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellini LM, Shea JA. Mood change and empathy decline persist during three years of internal medicine training. Acad Med. 2005;80:164–167. doi: 10.1097/00001888-200502000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Blasco PG, Moreto G, Levites M. Teaching humanities through opera: leading medical students to reflective attitudes. Fam Med. 2005;37:18–20. [PubMed] [Google Scholar]
- 4.Bowman D, Hughes P. Emotional responses of tutors and students in problem-based learning: lessons for staff development. Med Educ. 2005;39:145–153. doi: 10.1111/j.1365-2929.2004.02064.x. [DOI] [PubMed] [Google Scholar]
- 5.Bradley JG, Zia MJ, Hamilton N. Patient preferences for control in medical decision making: a scenario-based approach. Fam Med. 1996;28:496–501. [PubMed] [Google Scholar]
- 6.Branch WT., Jr Supporting the moral development of medical students. J Gen Intern Med. 2000;15:503–508. doi: 10.1046/j.1525-1497.2000.06298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bruce SM, Conaglen HM, Conaglen JV. Burnout in physicians: a case for peer-support. Intern Med J. 2005;35:272–278. doi: 10.1111/j.1445-5994.2005.00782.x. [DOI] [PubMed] [Google Scholar]
- 8.Chang RW, Bordage G, Connell KJ. The importance of early problem representation during case presentations. Acad Med. 1998;73:S109–S111. doi: 10.1097/00001888-199810000-00062. [DOI] [PubMed] [Google Scholar]
- 9.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49:651–661. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 10.Charon R. The patient-physician relationship. Narrative medicine: a model for empathy, reflection, profession, and trust. JAMA. 2001;286:1897–1902. doi: 10.1001/jama.286.15.1897. [DOI] [PubMed] [Google Scholar]
- 11.Clark DC, Zeldow PB. Vicissitudes of depressed mood during four years of medical school. JAMA. 1998;260:2521–2528. [PubMed] [Google Scholar]
- 12.Coulehan J. Viewpoint: today's professionalism: engaging the mind but not the heart. Acad Med. 2005;80:892–898. doi: 10.1097/00001888-200510000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ. 2005;39:594–604. doi: 10.1111/j.1365-2929.2005.02176.x. [DOI] [PubMed] [Google Scholar]
- 14.Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45:941–950. doi: 10.1016/0895-4356(92)90110-9. [DOI] [PubMed] [Google Scholar]
- 15.Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet. 2001;357:757–762. doi: 10.1016/s0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- 16.Edwards RR, Bingham CO, Bathon JM, Haythornthwaite JA. Catastrophizing and pain in arthritis, fibromyalgia and other rheumatic diseases. Arthritis Care and Research 2006. Arthritis Rheum. 2006 Apr 15;55(2):325–332. doi: 10.1002/art.21865. [DOI] [PubMed] [Google Scholar]
- 17.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA. 1992;267:2221–2226. [PubMed] [Google Scholar]
- 18.Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287:226–235. doi: 10.1001/jama.287.2.226. [DOI] [PubMed] [Google Scholar]
- 19.Fins JJ, Gentilesco BJ, Carver A, Lister P, Acres CA, Payne R, Storey-Johnson C. Reflective practice and palliative care education: a clerkship responds to the informal and hidden curricula. Acad Med. 2003;78:307–312. doi: 10.1097/00001888-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Flowers LK. The missing curriculum: experience with emotional competence education and training for premedical and medical students. J Natl Med Assoc. 2005;97:1280–1287. [PMC free article] [PubMed] [Google Scholar]
- 21.Goldstein EA, Maclaren CF, Smith S, Mengert TJ, Maestas RR, Foy HM, Wenrich MD, Ramsey PG. Promoting fundamental clinical skills: a competency-based college approach at the University of Washington. Acad Med. 2005;80:423–433. doi: 10.1097/00001888-200505000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Hasnain M, Bordage G, Connell KJ, Sinacore JM. History-taking behaviors associated with diagnostic competence of clerks: an exploratory study. Acad Med. 2001;76:S14–S17. doi: 10.1097/00001888-200110001-00006. [DOI] [PubMed] [Google Scholar]
- 23.Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, Callahan CA, Magee M. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–527. doi: 10.1046/j.1365-2923.2002.01234.x. [DOI] [PubMed] [Google Scholar]
- 24.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–1569. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 25.Hojat M, Mangione S, Nasca TJ, Rattner S, Erdmann JB, Gonnella JS, Magee M. An empirical study of decline in empathy in medical school. Med Educ. 2004;38:934–941. doi: 10.1111/j.1365-2929.2004.01911.x. [DOI] [PubMed] [Google Scholar]
- 26.Humphrey GB, Littlewood JL, Kamps WA. Physician/patient communication: a model considering the interaction of physicians' therapeutic strategy and patients' coping style. J Cancer Educ. 1992;7:147–152. doi: 10.1080/08858199209528157. [DOI] [PubMed] [Google Scholar]
- 27.Humphris GM, Kaney S. Assessing the development of communication skills in undergraduate medical students. Med Educ. 2001;35:225–231. doi: 10.1046/j.1365-2923.2001.00869.x. [DOI] [PubMed] [Google Scholar]
- 28.Jackson PL, Meltzoff AN, Decety J. How do we perceive the pain of others? A window into the neural processes involved in empathy. Neuroimage. 2005;24:771–779. doi: 10.1016/j.neuroimage.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 29.Mansell D, Poses RM, Kazis L, Duefield CA. Clinical factors that influence patients' desire for participation in decisions about illness. Arch Intern Med. 2000;160:2991–2996. doi: 10.1001/archinte.160.19.2991. [DOI] [PubMed] [Google Scholar]
- 30.Mayer JD, DiPaolo M, Salovey P. Perceiving affective content in ambiguous visual stimuli: a component of emotional intelligence. J Pers Assess. 1990;54:772–781. doi: 10.1080/00223891.1990.9674037. [DOI] [PubMed] [Google Scholar]
- 31.McNeilly DP, Wengel SP. The "ER" Seminar: Teaching Psychotherapeutic Techniques to Medical Students. Acad Psychiatry. 2001;25:193–200. doi: 10.1176/appi.ap.25.4.193. [DOI] [PubMed] [Google Scholar]
- 32.The American Heritage Dictionary of the English Language. Fourth Edition. Houghton Mifflin Company; 2004. 20 Jul. 2008. < www.dictionary.com>. [Google Scholar]
- 33.Murinson BB, Jolkovsky LA. The Role of Medical Education in Improved Pain Care: A Conceptual Model of the Clinical Pain Encounter. Seattle, WA: IASP Press; 2005. [Google Scholar]
- 34.Nendaz MR, Bordage G. Promoting diagnostic problem representation. Med Educ. 2002;36:760–766. doi: 10.1046/j.1365-2923.2002.01279.x. [DOI] [PubMed] [Google Scholar]
- 35.Newbury-Birch D, Walshaw D, Kamali F. Drink and drugs: from medical students to doctors. Drug Alcohol Depend. 2001;64:265–270. doi: 10.1016/s0376-8716(01)00128-4. [DOI] [PubMed] [Google Scholar]
- 36.Pilowsky I. An outline curriculum on pain for medical schools. Pain. 1988;33:1–2. doi: 10.1016/0304-3959(88)90196-0. [DOI] [PubMed] [Google Scholar]
- 37.Plato . Jowett Bt. Chapter IV. Laws. New York: Macmillan; 1892. [Google Scholar]
- 38.Pololi LP, Frankel RM, Clay M, Jobe AC. One year's experience with a program to facilitate personal and professional development in medical students using reflection groups. Educ Health (Abingdon) 2001;14:36–49. doi: 10.1080/13576280010015074. [DOI] [PubMed] [Google Scholar]
- 39.Rosenthal JM, Okie S. White coat, mood indigo--depression in medical school. N Engl J Med. 2005;353:1085–1088. doi: 10.1056/NEJMp058183. [DOI] [PubMed] [Google Scholar]
- 40.Rosenzweig S, Reibel DK, Greeson JM, Brainard GC, Hojat M. Mindfulness-based stress reduction lowers psychological distress in medical students. Teach Learn Med. 2003;15:88–92. doi: 10.1207/S15328015TLM1502_03. [DOI] [PubMed] [Google Scholar]
- 41.Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Mechanisms and outcomes. J Gen Intern Med. 2006;21 Suppl 1:S28–S34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Satterfield JM, Hughes E. Emotion skills training for medical students: a systematic review. Med Educ. 2007;41:935–941. doi: 10.1111/j.1365-2923.2007.02835.x. [DOI] [PubMed] [Google Scholar]
- 43.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136:358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 44.Shapiro J. How do physicians teach empathy in the primary care setting? Acad Med. 2002;77:323–328. doi: 10.1097/00001888-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 45.Stecker T. Well-being in an academic environment. Med Educ. 2004;38:465–478. doi: 10.1046/j.1365-2929.2004.01812.x. [DOI] [PubMed] [Google Scholar]
- 46.Steinbrook R. Renewing board certification. N Engl J Med. 2005;353:1994–1997. doi: 10.1056/NEJMp058067. [DOI] [PubMed] [Google Scholar]
- 47.Street RL, Jr, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Med Care. 2005;43:960–969. doi: 10.1097/01.mlr.0000178172.40344.70. [DOI] [PubMed] [Google Scholar]
- 48.USMLE. 2006 USMLE Bulletin. 1,1–39. Federation of State Medical Boards of the United States, Inc. and The National Board of Medical Examiners; 2006. [Google Scholar]
- 49.Viscott DS. Emotional Resilience: Simple Truths for Dealing with the Unfinished Business of Your Past. New York, NY: Three Rivers Press; 1997. [Google Scholar]
- 50.Walling AD, Woolley DC, Molgaard C, Kallail KJ. Patient satisfaction with migraine management by family physicians. J Am Board Fam Pract. 2005;18:563–566. doi: 10.3122/jabfm.18.6.563. [DOI] [PubMed] [Google Scholar]
- 51.Warhaft NJ. The Victorian Doctors Health Program: the first 3 years. Med J Aust. 2004;181:376–379. [PubMed] [Google Scholar]