Abstract
To address concerns that a flavivirus vaccine/wild-type recombinant virus might have a high mosquito infectivity phenotype, the yellow fever virus (YFV) 17D backbone of the ChimeriVax– dengue 4 virus was replaced with the corresponding gene sequences of the virulent YFV Asibi strain. Field-collected and laboratory-colonized Aedes aegypti mosquitoes were fed on blood containing each of the viruses under investigation and held for 14 days after infection. Infection and dissemination rates were based on antigen detection in titrated body or head triturates. Our data indicate that, even in the highly unlikely event of recombination or substantial backbone reversion, virulent sequences do not enhance the transmissibility of ChimeriVax viruses. In light of the low-level viremias that have been observed after vaccination in human volunteers coupled with low mosquito infectivity, it is predicted that the risk of mosquito infection and transmission of ChimeriVax vaccine recombinant/revertant viruses in nature is minimal.
Dengue (DEN; genus, Flavivirus; family, Flaviviridae) is the most significant emerging arboviral disease [1, 2]. Because of increased travel to tropical locals and expansion of vector distribution, the incidence of DEN fever and DEN hemorrhagic fever/DEN shock syndrome have increased dramatically in many regions of the world, with an estimated 2.5 billion people at risk [3]. Classic vector control has been the primary strategy to combat mosquitoborne diseases; however, population expansion of Aedes aegypti, the predominant peridomestic vector of the DEN viruses (DENV), emphasizes the urgent need for a DEN vaccine [3, 4]. DEN hemorrhagic fever is commonly associated with secondary exposure of an individual with preexisting antibody to a heterologous serotype. Therefore, because there are 4 serotypes of DENV (DENV1–4), an efficacious DEN vaccine must confer long-lasting tetravalent humoral and cellular immunity [5].
The yellow fever virus (YFV) 17D live attenuated vaccine (LAV) has been regarded as one of the safest and most efficacious vaccines [6]. The ChimeriVax platform developed by Acambis, Inc., has resulted in the generation of chimeric flavivirus vaccines with the highly attenuated 17D LAV backbone and structural genes of heterologous flaviviruses, including St. Louis encephalitis virus, West Nile virus, Japanese encephalitis virus, and the DENV [7–10]. It has long been known that, although wild-type (WT) YFV Asibi can infect and disseminate in A. aegypti, the predominant peridomestic vector, 17D can only occasionally infect these mosquitoes and cannot be transmitted by them [11]. Additionally, experimental observations of ChimeriVax vaccine candidate virus-vector interactions have demonstrated corresponding attenuation in mosquito transmissibility [12–15].
Although >400 million doses of YFV 17D have been administered worldwide to date—frequently in situations in which vaccinees may be infected with WT YFV—Seligman and Gould have recommended caution in the use of LAV, because of the hypothetical risk of recombination-driven reversion to a virulent phenotype [16]. Although recombination events have been documented for flaviviruses [17], there is neither experimental nor field data to suggest that recombination between vaccine and WT flaviviruses has ever occurred. As such, the incidence of, and potential for, such events may have been overestimated [18–21]. Because of the relatively long and benign interaction between the virus and mosquito vector, it is hypothesized that a recombination event is more likely to occur in the arthropod than in the vertebrate host. For such a recombination to occur and have a significant impact on public health, a mosquito host would have to be infected with both a WT and vaccine virus, either simultaneously or sequentially, and survive long enough to allow for viral replication, dissemination, and subsequent transmission.
We are beginning to understand how sequence differences between YFV 17D and Asibi strains may influence vector infection [22, 23], but it is unknown whether any phenotypic effects would result from a recombination/reversion event occuring while replicating in the vector. If a change in the ChimeriVax-YFV 17D platform did occur, virus would have to replicate in the vertebrate host after transmission to a sufficient titer to infect subsequently feeding mosquitoes. Large sequence changes are less probable than events leading to single mutations. With a total of 33 amino acid differences between the 17D vaccine and Asibi WT strains of YFV, a recombination event or multiple mutational events that change the attenuated phenotype to one of virulence and simultaneously enhance the capacity of the virus to replicate, disseminate, and be transmitted by the mosquito seems highly unlikely. Furthermore, some of these mechanisms are apparently under multigenic control [22, 23], and chimerization typically compromises replication competence [24, 25], underscoring the low probability that a vaccine/WT recombinant would possess a high mosquito infectivity phenotype.
Although recombination in this vaccine strategy is theoretically unlikely, it is important to test the consequences of recombination in a laboratory setting. ChimeriVax-DEN4 was selected for these experiments, because, although it is highly attenuated, it may be marginally more infectious than the other ChimeriVax-DEN vaccine candidates for Aedes mosquitoes [12]. Here, we modeled the worst-case scenario, in which the YFV 17D backbone of the well-characterized attenuated ChimeriVax-DEN4 virus was wholly replaced with sequences of the virulent YFV Asibi strain. To produce this virus, we constructed a parental YFV infectious clone (IC) based on the Asibi WT [26] and used this clone to generate a chimeric virus encoding the nonstructural gene sequences of YFV Asibi and the structural gene sequences of ChimeriVax-DEN4 (Asibi/DEN4 M-E). To evaluate the mosquito infectivity phenotype of this virus, A. aegypti mosquitoes were presented with infected blood meals and analyzed to determine infection and dissemination rates. The vertebrate pathogenicity of this virus was also evaluated in nonhuman primates (see the accompanying report [27]).
MATERIALS AND METHODS
Construction of YFV Ics
Construction and characterization of the YFV Asibi IC and structural YFV Asibi/17D chimeric variant clones (Asibi/17D M-E and 17D/Asibi M-E [backbone/structural insertion]) were done as described elsewhere [22, 23, 26]. All plasmid constructs were generated using standard polymerase chain reaction (PCR)–based mutagenesis and cloning methods [28]. Briefly, cDNA was generated using random hexanucleotide primers (Promega) and SuperScript II (Invitrogen), followed by PCR amplification of target sequences using Pfu DNA polymerase (Stratagene) under standard conditions.
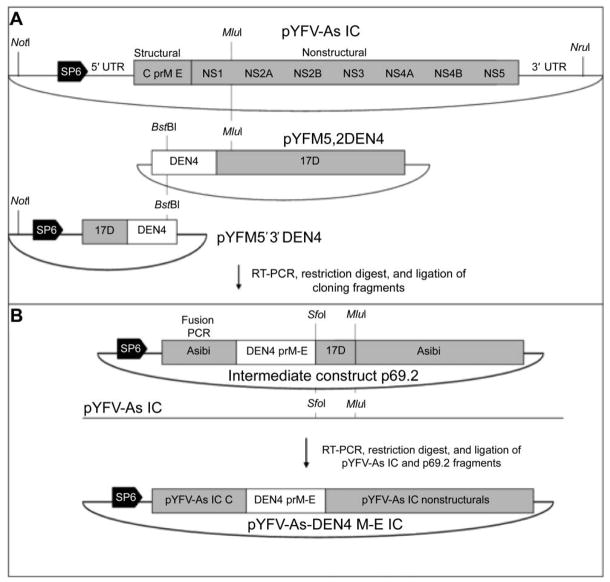
The construction of a YFV variant IC expressing the DEN4 structural proteins membrane (M) and envelope (E) in the virulent YFV Asibi backbone was facilitated via the generation of an intermediate construct, designated plasmid 69.2 (p69.2); p69.2 was made by simultaneous ligation and cloning of 3 DNA fragments via PCR amplification of YFV and DEN4 sequences of interest from plasmids pAsibi 5 IC (Higgs laboratory), pYFM5,2DEN4 (Acambis), and pYFM5′3′DEN4 (Acambis), using unique restriction sites as indicated in figure 1A. The IC pYF-As-DEN4 M-E (figure 1B) was then produced via sequential replacement of heterologous p69.2 sequences with PCR amplicons of pYF-As IC. Fragments for all cloning constructs were ligated using the T4 DNA ligase (Invitrogen) and amplified in Escherichia coli MC1061 cells, and intermediate and final constructs were sequenced to verify that no mutations had resulted during cloning. Plasmid and primer sequences are available on request.
Figure 1.
Cloning strategy for construction of yellow fever virus (YFV) Asibi dengue 4 (DEN4) chimeric virus. A, Construction of intermediate cloning vector plasmid 69.2 (p69.2) from pYFV-As infectious clone (IC), pYFM5,2DEN4 (Acambis), and pYFM5′3′DEN4 (Acambis) sequences. C, capsid; E, envelope; M, membrane; NS, nonstructural; RT-PCR, reverse-transcriptase polymerase chain reaction; prM, premembrane; UTR, untranslated region. B, Construction of pYFV-As-DEN4 M-E IC. Nucleotide positions and unique restriction sites used for cloning are indicated.
Cells and viruses
African green monkey kidney (Vero), baby hamster kidney (BHK-21), and Aedes albopictus (C6/36) cells were grown in Leibovitz L-15 medium supplemented with 10% fetal bovine serum (FBS), 1% penicillin-streptomycin, and 1% glutamine (cellgro; Mediatech), with vertebrate and invertebrate cell lines maintained at 37°C and 28°C, respectively. ChimeriVax-DEN4 virus was obtained as frozen stocks from Acambis, thawed once to prepare aliquots, and then stored at −80°C. The WT parent virus used for construction of ChimeriVax-DEN4 virus was DENV4 (strain 1288). Infectious Asibi, Asibi/17D M-E, 17D/Asibi M-E, and Asibi DEN4 M-E (figure 2) virus stocks were generated from respective ICs, as described elsewhere [26]. Briefly, plasmids were linearized, purified using phenol/chloroform, and transcribed in vitro using the mMESSAGE mMACHINE Kit (Ambion), in accordance with the manufacturer’s protocols. RNA was electroporated into BHK-21 cells as described elsewhere [26, 29], and cell culture supernatant aliquots containing virus were harvested 3–5 days after electroporation on the basis of visualization of cytopathic effect and stored at −80°C. Stock titers were determined by virus titration [29].
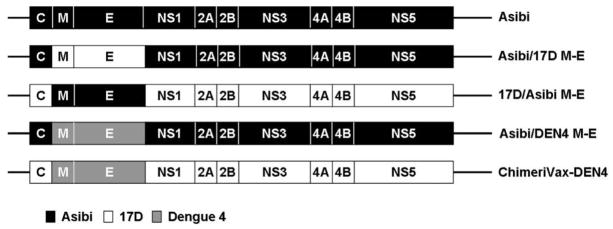
Figure 2.
Graphic depiction of parental and chimeric viruses used in mosquito experiments. Shading indicates source of viral coding sequences. C, capsid; DEN, dengue; E, envelope; M, membrane; NS1–5, nonstructural genes.
Mosquitoes
Two strains of A. aegypti mosquitoes were used for infectious feeds to allow for investigation and comparison of the infection and dissemination of YFV variants in colonized and wild-caught potential vectors. The A. aegypti Rex-D white-eye (WE) Higgs strain was derived from a spontaneous mutation in the Rex-D strain, originally isolated from Rexville, Puerto Rico [30], with mosquitoes used for infectious feeds being >30 filial generations (F). Wild-caught A. aegypti eggs were collected in the spring of 2004 from Mae Sot Province, Thailand (16°45′ N, 98°33′ E) and reared for several generations, and F5 eggs were collected and stored for use in these experiments [12].
Mosquito infection
To elucidate the appropriate conditions to obtain maximum blood meal titers for infectious feeds, 10-day growth curves for all viruses were generated in duplicate using Vero and C6/36 cells infected at an MOI of 0.001 (data not shown). Fresh virus for artificial blood meals was generated by propagation of virus stocks in cell culture or direct harvesting from electroporation. Virus inocula prepared in Vero cell culture included 17D/Asibi M-E and ChimeriVax-DEN4, those propagated in C6/36 cells included Asibi/17D M-E and Asibi/DEN4 M-E, and YFV Asibi was harvested directly from electroporated BHK-21 cells. Virus, cells, and supernatant were harvested in accordance with predicted maximal titer after infection and combined 1:1 with defibrinated sheep blood (Colorado Serum). Adenosine triphosphate was added as a phagostimulant, to a final concentration of 2–3 mmol/L. Oral infection of A. aegypti mosquitoes was performed as described elsewhere [22, 23]. After the feeding period, mosquitoes were chilled, and engorged females (⩾stage 4+ [31]) were transferred to new cartons and maintained as described elsewhere [23]. A 1-mL aliquot of infectious meal was stored at −80°C for virus titration. Positive control mosquitoes for all viruses were generated via intrathoracic inoculation of virus stocks diluted 1:3 in Leibovitz L-15 medium.
Determination of virus titer
Mosquitoes were harvested at 0 and 14 days after infection and assayed for virus by titration, as described elsewhere [12, 29]. Whole individual mosquitoes (0 days after infection) were triturated in 1 mL of L-15 medium (10% FBS, 10% tryptose phosphate broth, 100 U/mL penicillin, 100 μg/mL streptomycin, and 1 μg/mL fungizone) and titrated as 10-fold serial dilutions on Vero cell culture. At 14 days after infection, mosquito bodies and heads were assayed for infectious virus separately to determine infection and dissemination rates, respectively. Mosquito bodies were triturated in 1 mL and heads in 300 μL of L-15 medium (supplemented as described above). For each body homogenate, 100 μL was loaded in duplicate and then titrated in serial 10-fold dilutions in the first 8 wells of a 96-well plate, with head homogenates in the last 4 wells of the same rows as corresponding bodies. Titration plates were incubated at 37°C for 10 days, then fixed with 1:1 acetone-methanol and stored at −20°C for at least 30 min, dried, and analyzed by immunohistochemistry.
Immunohistochemical assay
Viruses varied in their capacity to produce cytopathic effect in Vero cells, so we tested all titration plates for virus by immunohistochemical assay to determine the highest dilution at which antigen was present. Selection of the antibody and optimal dilution was based on visual evaluation of signal intensity using Vero cells infected with each of the viruses, grown on glass coverslips [32]. For all YFV variants, it was determined that MA93, a hyperimmune mouse serum raised against YFV Asibi and 17D (produced by S.H. in 1993), at a concentration of 1:500 provided optimal detection.
Plates were dried and incubated for 10 min at room temperature in PBS (cellgro) supplemented with 1% normal horse serum (Sigma-Aldrich) before the application of primary antibody (MA93) for 30 min. Plates were then rinsed twice in PBS followed by application of secondary antibody, an anti–mouse IgG–horseradish peroxidase conjugate raised in goats (Southern Biotech), at 1:500 for 30 min at room temperature. Plates were subsequently rinsed twice in PBS, followed by visualization using the Vector VIP peroxidase substrate kit (Vector Laboratories) for 7.5 min, and reactions were quenched in distilled water. Blood meal and mosquito titers were calculated as log10 TCID50 per milliliter or mosquito, respectively.
Statistical analysis
Differences in infection and dissemination rates among species were tested for significance by Fisher’s exact test, and differences in average mosquito titers at 0 and 14 days after infection were tested by Student’s t test, using SPSS software (version 14.0; SPSS).
RESULTS
Whole-body titers of mosquito triturates were measured at 0 and 14 days after infection for all YFV variants. For each group, mean ± SD titers were calculated for the mosquitoes from which infectious virus was recovered (table 1). Whole-body titers on day 0 confirmed the ingestion of infectious virions during blood feeding for all groups. Infection and dissemination were measured by individual titration of mosquito bodies and heads [12], because previous studies have indicated that DENV detected in mosquito head tissue is representative of a disseminated infection of salivary gland tissue [33]. Infection and dissemination rates were calculated as the percentage of positive mosquitoes from the total number tested. Positive and negative control A. aegypti were included in all virus titration assays.
Table 1.
Comparison of viral titers, analyzed by titration of the bodies of Aedes aegypti mosquitoes, on days 0 and 14 after infection.
| Rex-D white-eye A. aegypti |
Thailand F5 A. aegypti |
|||||
|---|---|---|---|---|---|---|
| Body titer
|
Body titer
|
|||||
| Virus | Blood meal titer | Day 0 | Day 14 | Blood meal titer | Day 0 | Day 14 |
| Asibi | 3.95 | 1.69 ± 0.72 | 3.74 ± 2.13 | 3.95 | 1.29 ± 0.33 | 3.82 ± 1.61 |
| 17D/Asibi M-E | 5.52 | 3.33 ± 0.33a | 2.84 ± 1.00 | 5.52 | 3.28 ± 0.58 | 2.38 ± 1.16 |
| Asibi/17D M-E | 4.95 | 2.33 ± 0.73 | 1.52 | 4.95 | 3.33 ± 0.33 | 1.06 |
| Asibi/DEN4 M-E | 4.52 | 3.00 ± 0.50a | Negative | 4.95 | 2.81 ± 0.25b | 3.52 |
| ChimeriVax-DEN4 | 3.95 | 1.58 ± 0.34a | Negative | 4.52 | 1.06b | Negative |
NOTE. Data are mean ± SD values. Blood meal titers are reported as log10 TCID50/mL, and titers of mosquito bodies are reported as log10 TCID50/mosquito; the limit of detection was 1.06 log10 TCID50/mL for blood meal titers and 1.06 log10 TCID50/mosquito for whole-body titers. DEN, dengue; E, envelope; M, membrane.
P ≤ .02.
P = .003.
Rex-D WE A. aegypti
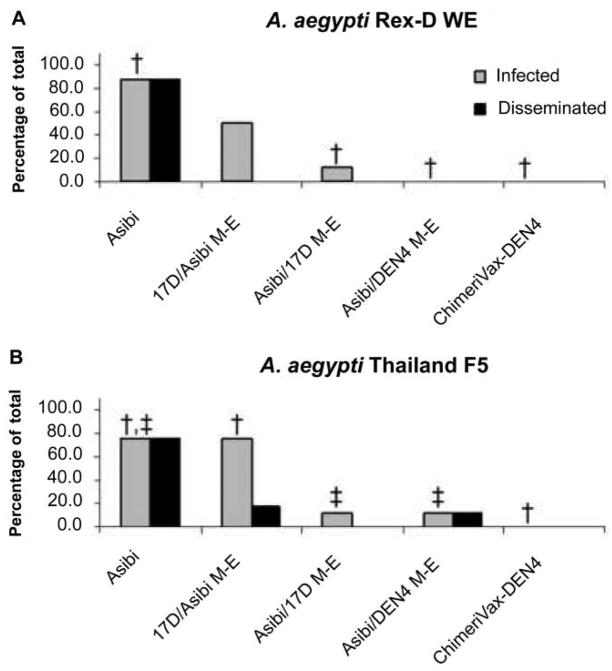
High levels of infection (7/8) and dissemination (7/8) (figure 3) were observed in those mosquitoes infected with virus derived from our Asibi IC (prototypical WT YFV), despite relatively low titers noted in the infectious blood meal and day 0 mosquitoes (3.95 log10 TCID50/mL and 1.69 ± 0.72 log10 TCID50/mosquito, respectively). Substitution of the YFV 17D structural genes in the YFV Asibi backbone resulted in a significant decrease in mosquito infection (1/8; P = .01) and prevented viral dissemination (0/8), whereas the reverse substitution, YFV Asibi M-E in the 17D backbone, was associated with an intermediate infection rate (4/8). Substitution of the DEN4 structural genes into the virulent YFV Asibi backbone (Asibi/DEN4 M-E) (figure 3) also resulted in a significant decrease in mosquito infection (0/8; P ≤ .01) compared with YFV Asibi WT (7/8). Asibi/DEN4 M-E did not have significantly higher mosquito infectivity (0/8) compared with ChimeriVax-DEN4, which was not observed to infect (0/8) or disseminate (0/8) in Rex-D WE A. aegypti.
Figure 3.
Infection and dissemination rates for chimeric yellow fever viruses. A, Aedes aegypti Rex-D white-eye (WE) strain. B, A. aegypti Thailand F5 strain. DEN, dengue; E, envelope; M, membrane. †P ≤ .01; ‡P ≤ .05.
Thailand F5 A. aegypti
Generally, observations of infection and dissemination kinetics in YFV variants were similar in both strains of A. aegypti (Rex-D WE and Thailand F5), with no significant differences in infection observed between the 2 strains for any of the viruses. YFV Asibi infected (6/8) and disseminated (5/8) at a high rate, but substitution of the DEN4 or YFV 17D structural genes M-E significantly decreased (P < .05) mosquito infectivity (Asibi/DEN4 M-E [1/8] and Asibi/17D M-E [1/8]) (figure 3). The 17D/Asibi M-E variant again displayed an intermediate phenotype characterized by significantly increased (P = .007) mosquito infectivity (6/8) compared with ChimeriVax-DEN4 (0/8) but decreased dissemination (1/8) compared with YFV Asibi (5/8) (figure 3). Despite the significantly higher average titer observed in mosquitoes on day 0 (P = .003) (table 1), Asibi/DEN4 M-E did not differ significantly in mosquito infectivity (1/8) compared with ChimeriVax-DEN4, which did not infect (0/8) or disseminate (0/8) in a near-wild Thai strain of A. aegypti.
Although no significant differences were observed between the infection and dissemination rates of our hypothetical recombinant (Asibi/DEN4 M-E) and parental vaccine ChimeriVax-DEN4, Asibi/DEN4 M-E infected (1/8) and disseminated (1/8) in a single mosquito exposed to a relatively high-titer infectious blood meal (4.95 log10 TCID50/mL). The infection rate was significantly lower (5/8; P < .05) than that observed for mosquitoes exposed to a lower-titer infectious blood meal (3.95 log10 TCID50/mL) of YFV Asibi. Because Asibi/DEN4 M-E is a chimera of sequences derived from 2 viruses with high mosquito infectivity phenotypes (YFV Asibi and DEN4 strain 1228; see Materials and Methods), this finding was not entirely unexpected. However, when we consider the low levels of infectious viremia and dramatically attenuated phenotype in nonhuman primates infected with Asibi/DEN4 M-E (see accompanying report [27]), compared with the generation of maximal blood meal titers using cell-culture systems, we must conclude that a mosquito is extremely unlikely to become infected while feeding on an animal infected with this recombinant.
DISCUSSION
Recent experimental observations of YFV IC chimeras have identified some of the molecular determinants of infection and dissemination in mosquito vectors [22, 23]. Investigations of the relative contributions of structural and nonstructural genes to the mosquito infection phenotype of YFV Asibi have identified major determinants of dissemination in the structural genes, specifically E, with nonstructural genes (NS2A and NS4B) also contributing, albeit to a lesser extent [22, 23]. Substitution of the corresponding virulent YFV Asibi sequences into the 17D backbone does not necessarily restore high infectivity for A. aegypti mosquitoes [22, 23]. These observations support the conclusion that multiple attenuating mutations, distributed throughout the 17D backbone, contribute to decreased mosquito infectivity, therefore supporting its use as a safe platform for the development of heterologous flavivirus vaccines.
In vivo vector-competence studies with ChimeriVax-DEN vaccine candidates have consistently demonstrated decreased mosquito infectivity. Analysis of ChimeriVax-DEN2 in A. aegypti and A. albopictus found mosquito infectivity comparable to that of the approved parental 17D vaccine and identified no dissemination at 14 days after infection despite exposure to high blood meal titers of 6.3–7.7 log10 pfu/mL [15]. Additionally, significant decreases in ChimeriVax-DEN2 mosquito infection, associated with a loss in dissemination, were observed in a DENV2-susceptible wild isolate of A. aegypti collected in Puerto Rico. Real-time reverse-transcriptase PCR analysis of ChimeriVax-DEN1–4 in A. aegypti identified attenuated oral infectivity [15]. Significant decreases have been identified in the infection and dissemination rates of ChimeriVax-DEN viruses when fed to near-wild strains of A. aegypti and A. albopictus isolated in Thailand, both individually and as a tetravalent mixture [12].
A. aegypti mosquitoes experimentally infected with YFV Asibi can fatally infect monkeys for up to 168 days after infection [34]. This long-term infectivity, coupled with the opportunity for multiple exposures, indicates that if recombination were to occur, the mosquito would be the most likely organism to facilitate it. Vector-competence studies are therefore a critical component of the evaluation of potential LAV candidates, even though, in regions of extreme and continuous YFV activity, productive recombination in the mosquito vector is highly unlikely for many reasons. Viremias of YFV 17D produced in vaccinees are relatively low and of short duration, and this attenuated strain of virus is poorly infectious to mosquitoes [11, 22, 23, 35]. Because YFV 17D does not disseminate from the midgut [22, 23], recombination would have to occur here after coinfection of cells with both vaccine and WT viruses. Although the mechanism of superinfection resistance—the inability of cells to be sequentially infected by antigenically related viruses [36]—is not fully understood, it has been documented for flaviviruses [37, 38] and may further restrict the potential for recombination. Interestingly, repeated isolations of an E protein stop-codon-mutant DENV have led investigators to conclude that persistence was achieved via superinfection complementation by replication-competent viruses [39]. The tendency for A. aegypti to breed in close proximity to humans, coupled with its high propensity for feeding on humans [40], may also restrict opportunities to feed on multiple different viremic hosts and therefore further reduce the likelihood of dual infection. It seems highly unlikely for these multiple potential hurdles to recombination to be overcome in a vector with a relatively short average life span, perhaps 15 days [41].
Multiple analyses have indicated that ChimeriVax-DEN viruses are highly attenuated with respect to mosquito infectivity. However, the consequences of a recombination-driven virulent reversion of a chimeric flavivirus vaccine have been much speculated on but were hitherto unknown. Here, we have addressed directly the concerns of Seligman and Gould [16] and report the effects of substituting the 17D nonstructural backbone sequences with the corresponding sequences of virulent YFV Asibi on mosquito infectivity phenotype.
As observed for 17D (data not shown), when an artificial intrathoracic inoculation method was used, A. aegypti became infected with all chimeric viruses. No significant differences were observed in the infection and dissemination profiles of the 2 strains of A. aegypti, although the near-wild Thailand mosquitoes appeared to be slightly more susceptible to infection. Substitution of the WT virulent YFV Asibi sequences into ChimeriVax-DEN4 virus did not produce a virus with an Asibi-like phenotype with respect to mosquito infectivity. Additionally, the mosquito infectivity of Asibi/DEN4 M-E was similar to that of ChimeriVax-DEN4 virus for Aedes mosquitoes collected from Thailand, as reported elsewhere [12]. Although Asibi/DEN4 M-E did disseminate in A. aegypti Thailand F5, dissemination occurred at a low rate despite exposure to relatively high viral titer in the blood meals (4.95 log10 TCID50/mL), especially considering the significantly higher infection rates observed for those mosquitoes exposed to a lower-titer infectious blood meal of YFV Asibi. In light of (1) the short duration of viremia (1.2 ± 1.42 to 1.9 ± 1.23 days) and low circulating titers of vaccine virus expected in vaccinees (33–68 pfu/mL) [42], (2) the relative refractoriness of Aedes mosquitoes to oral infection with ChimeriVax-DEN virus, (3) the low mosquito infectivity of Asibi/DEN4 M-E, and (4) the dramatically attenuated phenotype of Asibi/DEN4 M-E in nonhuman primates (see the accompanying report [27]), we therefore conclude that, even in the incredibly unlikely event of a complete “virulent” backbone reversion, the risk of mosquito transmission is minimal.
Acknowledgments
Sanofi-Pasteur; Centers for Disease Control and Prevention Fellowship Training Program in Vector-Borne Infectious Diseases (grant T01/CCT622892 to C.E.M.); National Institutes of Health (grant T32 A107536 to D.L.V.).
We thank Jing Huang for rearing and maintaining the mosquitoes used for these experiments.
Footnotes
Potential conflicts of interest: Sanofi-Pasteur, manufacturer of the ChimeriVax vaccine, sponsored this study financially. J.L., B.G., and T.D. are all current employees of Sanofi-Pasteur and have a financial interest in this company, which may include stock ownership. C.E.M., K.T, D.L.V., K.L.M., and S.H. do not have any financial interest in Sanofi-Pasteur.
References
- 1.Gratz NG. Emerging and resurging vector-borne diseases. Annu Rev Entomol. 1999;44:51–75. doi: 10.1146/annurev.ento.44.1.51. [DOI] [PubMed] [Google Scholar]
- 2.Gubler DJ. Resurgent vector-borne diseases as a global health problem. Emerg Infect Dis. 1998;4:442–50. doi: 10.3201/eid0403.980326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gubler DJ. Dengue/dengue haemorrhagic fever: history and current status. Novartis Found Symp. 2006;277:3–16. doi: 10.1002/0470058005.ch2. discussion 16–22, 71–3, 251–3. [DOI] [PubMed] [Google Scholar]
- 4.Gubler DJ. The changing epidemiology of yellow fever and dengue, 1900 to 2003: full circle? Comp Immunol Microbiol Infect Dis. 2004;27:319–30. doi: 10.1016/j.cimid.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Chaturvedi UC, Shrivastava R, Nagar R. Dengue vaccines: problems and prospects. Indian J Med Res. 2005;121:639–52. [PubMed] [Google Scholar]
- 6.Marianneau P, Georges-Courbot M, Deubel V. Rarity of adverse effects after 17D yellow-fever vaccination. Lancet. 2001;358:84–5. doi: 10.1016/s0140-6736(01)05374-0. [DOI] [PubMed] [Google Scholar]
- 7.Monath TP, Soike K, Levenbook I, et al. Recombinant, chimaeric live, attenuated vaccine (ChimeriVax) incorporating the envelope genes of Japanese encephalitis (SA14-14-2) virus and the capsid and nonstructural genes of yellow fever (17D) virus is safe, immunogenic and protective in non-human primates. Vaccine. 1999;17:1869–82. doi: 10.1016/s0264-410x(98)00487-3. [DOI] [PubMed] [Google Scholar]
- 8.Pugachev KV, Guirakhoo F, Mitchell F, et al. Construction of yellow fever/St. Louis encephalitis chimeric virus and the use of chimeras as a diagnostic tool. Am J Trop Med Hyg. 2004;71:639–45. [PubMed] [Google Scholar]
- 9.Arroyo J, Miller C, Catalan J, et al. ChimeriVax-West Nile virus live-attenuated vaccine: preclinical evaluation of safety, immunogenicity, and efficacy. J Virol. 2004;78:12497–507. doi: 10.1128/JVI.78.22.12497-12507.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jones T. Technology evaluation: ChimeriVax-DEN, Acambis/Aventis. Curr Opin Mol Ther. 2004;6:443–50. [PubMed] [Google Scholar]
- 11.Whitman L. Failure of Aedes aegypti to transmit yellow fever cultured virus (17D) Am J Trop Med Hyg. 1939;19:16–19. [Google Scholar]
- 12.Higgs S, Vanlandingham DL, Klingler KA, et al. Growth characteristics of ChimeriVax-DEN vaccine viruses in Aedes aegypti and Aedes albopictus from Thailand. Am J Trop Med Hyg. 2006;75:986–93. [PubMed] [Google Scholar]
- 13.Bhatt TR, Crabtree MB, Guirakhoo F, Monath TP, Miller BR. Growth characteristics of the chimeric Japanese encephalitis virus vaccine candidate, ChimeriVax-JE (YF/JE SA14--14--2), in Culex tritaeniorhynchus, Aedes albopictus, and Aedes aegypti mosquitoes. Am J Trop Med Hyg. 2000;62:480–4. doi: 10.4269/ajtmh.2000.62.480. [DOI] [PubMed] [Google Scholar]
- 14.Johnson BW, Chambers TV, Crabtree MB, et al. Growth characteristics of ChimeriVax-DEN2 vaccine virus in Aedes aegypti and Aedes albopictus mosquitoes. Am J Trop Med Hyg. 2002;67:260–5. doi: 10.4269/ajtmh.2002.67.260. [DOI] [PubMed] [Google Scholar]
- 15.Johnson BW, Chambers TV, Crabtree MB, Guirakhoo F, Monath TP, Miller BR. Analysis of the replication kinetics of the ChimeriVax-DEN 1, 2, 3, 4 tetravalent virus mixture in Aedes aegypti by real-time reverse transcriptase-polymerase chain reaction. Am J Trop Med Hyg. 2004;70:89–97. [PubMed] [Google Scholar]
- 16.Seligman SJ, Gould EA. Live flavivirus vaccines: reasons for caution. Lancet. 2004;363:2073–5. doi: 10.1016/S0140-6736(04)16459-3. [DOI] [PubMed] [Google Scholar]
- 17.Twiddy SS, Holmes EC. The extent of homologous recombination in members of the genus Flavivirus. J Gen Virol. 2003;84:429–40. doi: 10.1099/vir.0.18660-0. [DOI] [PubMed] [Google Scholar]
- 18.Monath T. Yellow fever vaccine. In: Plotkin S, Orenstein WA, editors. Vaccines. 4. Philadelphia: WB Saunders; 2004. pp. 1095–176. [Google Scholar]
- 19.Hornbach J, Kurane I, Wood D. Arguments for live flavivirus vaccines. Lancet. 2004;364:499–500. doi: 10.1016/S0140-6736(04)16800-1. [DOI] [PubMed] [Google Scholar]
- 20.de Silva A, Messer W. Arguments for live flavivirus vaccines. Lancet. 2004;364:500. doi: 10.1016/S0140-6736(04)16802-5. [DOI] [PubMed] [Google Scholar]
- 21.Murphy BR, Blaney JE, Jr, Whitehead SS. Arguments for live flavivirus vaccines. Lancet. 2004;364:499–500. doi: 10.1016/S0140-6736(04)16801-3. [DOI] [PubMed] [Google Scholar]
- 22.McElroy KL, Tsetsarkin KA, Vanlandingham DL, Higgs S. Manipulation of the yellow fever virus non-structural genes 2A and 4B and the 3′ non-coding region to evaluate genetic determinants of viral dissemination from the Aedes aegypti midgut. Am J Trop Med Hyg. 2006;75:1158–64. [PubMed] [Google Scholar]
- 23.McElroy KL, Tsetsarkin KA, Vanlandingham DL, Higgs S. Role of the yellow fever virus structural protein genes in viral dissemination from the Aedes aegypti mosquito midgut. J Gen Virol. 2006;87:2993–3001. doi: 10.1099/vir.0.82023-0. [DOI] [PubMed] [Google Scholar]
- 24.Blaney JE, Jr, Hanson CT, Firestone CY, Hanley KA, Murphy BR, White-head SS. Genetically modified, live attenuated dengue virus type 3 vaccine candidates. Am J Trop Med Hyg. 2004;71:811–21. [PubMed] [Google Scholar]
- 25.Blaney JE, Jr, Johnson DH, Manipon GG, et al. Genetic basis of attenuation of dengue virus type 4 small plaque mutants with restricted replication in suckling mice and in SCID mice transplanted with human liver cells. Virology. 2002;300:125–39. doi: 10.1006/viro.2002.1528. [DOI] [PubMed] [Google Scholar]
- 26.McElroy KL, Tsetsarkin KA, Vanlandingham DL, Higgs S. Characterization of an infectious clone of the wild-type yellow fever virus Asibi strain that is able to infect and disseminate in mosquitoes. J Gen Virol. 2005;86:1747–51. doi: 10.1099/vir.0.80746-0. [DOI] [PubMed] [Google Scholar]
- 27.McGee CE, Lewis MG, St Claire M, et al. Recombinant chimeric virus with wild-type dengue 4 virus premembrane and envelope and virulent yellow fever virus Asibi backbone sequences is dramatically attenuated in nonhuman primates. J Infect Dis. 2008;197:693–7. doi: 10.1086/527329. (in this issue) [DOI] [PubMed] [Google Scholar]
- 28.Sambrook JF, Fritsch E, Maniatis T. Molecular cloning: a laboratory manual. 2. Cold Spring Harbor, New York: Cold Spring Laboratory; 1989. [Google Scholar]
- 29.Higgs S, Olson KE, Kamrud KI, Powers AM, Beaty BJ. Viral expression systems and viral infections in insects. In: Crampton JM, Beard CB, Louis C, editors. The molecular biology of disease vectors: a methods manual. London: Chapman and Hall; 1997. pp. 457–83. [Google Scholar]
- 30.Wendell MD, Wilson TG, Higgs S, Black WC. Chemical and gamma-ray mutagenesis of the white gene in Aedes aegypti. Insect Mol Biol. 2000;9:119–25. doi: 10.1046/j.1365-2583.2000.00166.x. [DOI] [PubMed] [Google Scholar]
- 31.Pilitt DR, Jones JC. A qualitative method for estimating the degree of engorgement of Aedes aegypti adults. J Med Entomol. 1972;9:334–7. doi: 10.1093/jmedent/9.4.334. [DOI] [PubMed] [Google Scholar]
- 32.Gould EA, Buckley A, Cammack N. Use of the biotin-streptavidin interaction to improve flavivirus detection by immunofluorescence and ELISA tests. J Virol Methods. 1985;11:41–8. doi: 10.1016/0166-0934(85)90123-5. [DOI] [PubMed] [Google Scholar]
- 33.Olson KE, Higgs S, Gaines PJ, et al. Genetically engineered resistance to dengue-2 virus transmission in mosquitoes. Science. 1996;272:884–6. doi: 10.1126/science.272.5263.884. [DOI] [PubMed] [Google Scholar]
- 34.Philip CB. Transmission of yellow fever virus by aged Aedes aegypti and comments on some other mosquito-virus relationships. Am J Trop Med Hyg. 1962;11:697–701. doi: 10.4269/ajtmh.1962.11.697. [DOI] [PubMed] [Google Scholar]
- 35.Barrett AD, Higgs S. Yellow fever: a disease that has yet to be conquered. Annu Rev Entomol. 2007;52:209–29. doi: 10.1146/annurev.ento.52.110405.091454. [DOI] [PubMed] [Google Scholar]
- 36.Young JAT. Virus entry and uncoating. In: Knipe DM, Howley PM, editors. Fundamental virology. 4. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 87–104. [Google Scholar]
- 37.Venugopal K, Gould EA. Heterologous resistance to superinfection by louping ill virus persistently infected cell cultures. Arch Virol. 1992;125:251–9. doi: 10.1007/BF01309642. [DOI] [PubMed] [Google Scholar]
- 38.Sabin AB. Research on dengue during World War II. Am J Trop Med Hyg. 1952;1:30–50. doi: 10.4269/ajtmh.1952.1.30. [DOI] [PubMed] [Google Scholar]
- 39.Aaskov J, Buzacott K, Thu HM, Lowry K, Holmes EC. Long-term transmission of defective RNA viruses in humans and Aedes mosquitoes. Science. 2006;311:236–8. doi: 10.1126/science.1115030. [DOI] [PubMed] [Google Scholar]
- 40.Scott TW, Chow E, Strickman D, et al. Blood-feeding patterns of Aedes aegypti (Diptera: Culicidae) collected in a rural Thai village. J Med Entomol. 1993;30:922–7. doi: 10.1093/jmedent/30.5.922. [DOI] [PubMed] [Google Scholar]
- 41.Christophers R. The yellow fever mosquito: its life history, bionomics, and structure. Cambridge: Cambridge University Press; 1960. Aedes aegypti; p. 739. [Google Scholar]
- 42.Guirakhoo F, Kitchener S, Morrison D, et al. Live attenuated chimeric yellow fever dengue type 2 (ChimeriVax-DEN2) vaccine: phase I clinical trial for safety and immunogenicity: effect of yellow fever pre-immunity in induction of cross neutralizing antibody responses to all 4 dengue serotypes. Hum Vaccin. 2006;2:60–7. doi: 10.4161/hv.2.2.2555. [DOI] [PubMed] [Google Scholar]