Abstract
Objectives
We analyzed the prevalence and characteristics of lower urinary tract symptoms (LUTS) in community-dwelling men 80 years and older.
Methods
We administered the American Urological Association Symptom Index (AUA-SI) by mail to 291 surviving community-dwelling male participants in the Rancho Bernardo Study, a prospective, community-based study of aging. We compared the prevalence, severity, and types of LUTS occurring in men who were ≥ 80 years to those < 80 years.
Results
The mean age was 74.6 years (standard deviation [SD] 8.9, range 48.3–97.1). One third of respondents were ≥ 80. The mean total AUA-SI score increased steadily by decade of life (P-trend = 0.002). The prevalence of LUTS was 70% in men ≥ 80 years and 56% in men < 80 years (P = 0.03). Men ≥ 80 had significantly higher mean total AUA-SI (P = 0.05) and were more likely to complain of incomplete emptying (odds ratio [OR] 2.12, 95% confidence interval [CI] 1.06 to 4.18, P = 0.02), frequency (OR 1.83, 95% CI 1.00 to 3.31, P = 0.03), urgency (OR 1.76, 95% CI 0.96 to 3.20, P = 0.05), and weak stream (OR 1.78, 95% CI 1.01 to 3.12, P = 0.03).
Conclusions
In this cohort of community-dwelling men, prevalence and severity of LUTS increased into the 10th decade of life. Compared to younger men, men ≥ 80 were more likely to complain of incomplete emptying, frequency, urgency, and weak stream. Further studies of LUTS in older men are needed to better delineate these associations.
Keywords: aging, benign prostatic hyperplasia, prevalence, lower urinary tract symptoms, American Urological Association Symptom Index
Introduction
Male lower urinary tract symptoms (LUTS) are highly prevalent, occurring in 15% to 60% of males over the age of 40 years in the U.S. and Europe.1–5 In affected men, the LUTS complex significantly diminishes quality of life,6 while diagnosis and treatment of LUTS-associated conditions—most notably benign prostatic hyperplasia (BPH)—consume staggering amounts of health care resources.1,7
LUTS prevalence rises markedly with age. In the Boston Area Community Health (BACH) Survey, LUTS prevalence increased from 8% in men 30 to 39 years to 35% in men 60 to 69 years.3 Similarly, in the European and Korean UrEpik study the prevalence of male LUTS increased 10% per decade from 40 to 79 years.2 Other population-based studies have demonstrated similar trends in both the U.S. and Europe.5
The increasing prevalence of LUTS with age represents a particularly salient public health issue. By 2030, 20% of the U.S. population will be 65 years or older, including more than 20 million men. Significantly, the fastest-growing segment of the older population is the oldest age group: those over 85. Current estimates are that the number of individuals 80 years and older in the U.S. will rise from 9.3 million in 2000 to 19.5 million in 2030, an increase of over 200%.8
Thus, with increased male longevity, the proportion of much older men in the population—those aged 80 years and older—is expanding considerably each year. Older individuals tend to utilize disproportionately greater shares of health care resources. However, data on LUTS in men over the age of 80 years remain limited. Most prior studies, including BACH and UrEPIK, did not include men over the age of 80; the few that did investigate this group did not analyze in detail the type of LUTS in these men, nor compare characteristics of LUTS in men over 80 to those in younger men.4,5
Further study of LUTS in men over the age of 80 years would provide potentially important observations on the nature of LUTS in this increasingly prominent segment of the population. Therefore, we analyzed the prevalence and characteristics of LUTS in a cohort of community-dwelling older men, focusing on those aged 80 years and older.
Materials and Methods
Participants
The Rancho Bernardo Study, established in 1972, is a cohort of mostly white, middle- to upper middle–class, community-dwelling adults in Southern California, U.S.A. Between 1999 and 2002, 1141 surviving participants attended a research clinic where 463 men completed a male health history questionnaire. In 2006, we administered the American Urological Association Symptom Index (AUA-SI)9 by mail to the 353 surviving male participants who did not report a previous diagnosis of prostate cancer at the 1999–2002 visit.
We analyzed total, individual symptom, and bother scores and collected data on history of BPH, BPH medication use, prostate cancer, and prostate surgery.
We categorized overall urinary symptom severity as none or mild (0 to 7 points), moderate (8 to 19 points), or severe (20 to 35 points). Consistent with prior observational studies, we defined LUTS as total American Urological Association Symptom Index (AUA-SI) score ≥ 8.3
Statistical analysis
This was a cross-sectional analysis. The prevalence, severity, and types of LUTS were compared in those ≥ 80 years and those < 80 years using general linear models for continuous variables and chi-square analysis for categorical variables. All data were analyzed using SAS, version 9.1 (SAS Institute, Cary, North Carolina, U.S.A.).
Results
Demographics
The mean (standard deviation [SD], range) age of the 291 responding participants (response rate 82%) was 74.6 years (8.9, 48.3–97.1). Ninety-five (33%) were ≥ 80 years; of these, 11 (4%) were ≥ 90 years. Mean age for those ≥ 80 years was 85.1 (3.8, 80.0–97.1) and for those < 80 years was 70.4 (6.5, 48.3–79.9) years. Compared to those < 80 years, men ≥ 80 years were more likely to have a history of BPH (59% vs. 36%, P < 0.001) or prostate surgery (23% vs. 7%, P < 0.001) but did not differ significantly for history of prostate cancer diagnosed since the last study visit (4% vs. 2%, P = 0.41) or BPH medication use (18% vs. 13%, P = 0.28).
Total AUA-SI score
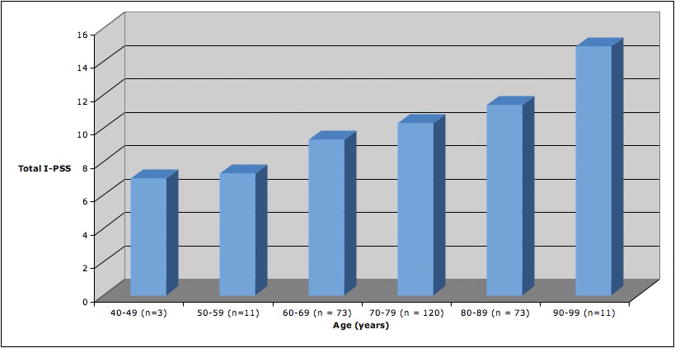
The mean (SD, range) total AUA-SI score for the entire cohort was 10.3 (6.8, 0–31). Mean total AUA-SI increased steadily by decade of life (P-trend = 0.002) (Figure 1). Compared to the younger men, those ≥ 80 years had significantly higher mean total AUA-SI: 11.8 (6.6, 0–6) versus 9.7 (6.8, 0–31) (P = 0.05).
Figure 1.
Mean total American Urological Symptom Index (AUA-SI) score by decade in the Rancho Bernardo Study, 2006 (P-trend = 0.002)
Of the entire cohort, 171 (60%) complained of LUTS. Older men were significantly more likely to report LUTS: 57 (70%) of 82 respondents ≥ 80 years compared to 114 (56%) of 205 respondents < 80 years (odds ratio [OR] 1.82, 95% CI 1.02 to 3.28, P = 0.03). LUTS were present in 9 (90%) of 10 respondents ≥ 90 years.
Repeating these analyses after excluding men with a prior history of prostate surgery (n = 37) strengthened the associations for both total AUA-SI (P = 0.005) and LUTS prevalence for men ≥ 80 years (OR 2.22, 95% CI 1.15 to 4.42, P = 0.01).
AUA-SI symptom domains
Between 288 and 290 men responded to the individual symptom domain questions. Compared to the younger men, those ≥ 80 years were more likely to complain of incomplete emptying, frequency, urgency, and weak stream. There were no significant differences in likelihood of intermittency, straining, or nocturia between groups (Table 1). Repeating these analyses after excluding men with a prior history of prostate surgery produced similar results (data not shown).
Table 1.
American Urological Symptom Index responses comparing men ≥ 80 years to men < 80 years in the Rancho Bernardo Study, 2006. N: number of respondents; prevalence: number of respondents reporting symptom occurring ≥ 1/2 of the time; OR: odds ratio; 95% CI: 95% confidence interval
| Symptom | Age Group | P | |
|---|---|---|---|
| <80 years | ≥ 80 years | ||
| Incomplete emptying | |||
| N | 206 | 84 | |
| Prevalence (%) | 28 (14) | 21(25) | |
| OR | ref | 2.12 | 0.02 |
| 95% CI | 1.06 to 4.18 | ||
|
| |||
| Frequency | |||
| N | 206 | 84 | |
| Prevalence (%) | 46 (22) | 29 (35) | |
| OR | ref | 1.83 | 0.03 |
| 95% CI | 1.00 to 3.31 | ||
|
| |||
| Intermittency | |||
| N | 206 | 84 | |
| Prevalence (%) | 51 (25) | 19(23) | |
| OR | ref | 0.89 | 0.70 |
| 95% CI | .46 to 1.67 | ||
|
| |||
| Urgency | |||
| N | 207 | 82 | |
| Prevalence (%) | 47(23) | 28 (34) | |
| OR | Ref | 1.76 | 0.05 |
| 95% CI | 0.96 to 3.20 | ||
|
| |||
| Weak stream | |||
| N | 206 | 84 | |
| Prevalence (%) | 59 (29) | 35 (42) | |
| OR | ref | 1.78 | 0.03 |
| 95% CI | 1.01 to 3.12 | ||
|
| |||
| Straining | |||
| N | 207 | 84 | |
| Prevalence (%) | 12 (6) | 7 (8) | |
| OR | ref | 1.71 | 0.25 |
| 95% CI | 0.58 to 4.75 | ||
|
| |||
| Nocturia | |||
| N | 206 | 84 | |
| Prevalence (%) | 66 (32) | 25 (30) | |
| OR | ref | 0.90 | 0.70 |
| 95% CI | 0.49 to 1.61 | ||
|
| |||
| Quality of life | |||
| N | 205 | 83 | |
| Increased bother (%)* | 28 (14) | 13 (16) | |
| OR | ref | 1.17 | 0.66 |
| 95% CI | 0.53 to 2.50 | ||
Those responding “mixed,” “mostly dissatisfied,” “unhappy,” or “terrible”
AUA-SI quality of life domain
Compared to the younger men, those ≥ 80 years reported significantly lower quality of life as measured by higher scores in the quality of life domain: 2.89 (2.00 to 2.58) versus 1.87 (1.69 to 2.05) (P = 0.02), respectively. However, there were no significant differences between groups in the proportions of men who reported feeling “mixed,” “mostly dissatisfied,” “unhappy,” or “terrible” regarding their urinary symptoms (Table 1). Repeating these analyses after excluding men with a prior history of prostate surgery produced similar results: 2.31 (2.00 to 2.63) versus 1.84 (1.66 to 2.03) (P = 0.01), respectively.
Discussion
Although previous studies have examined LUTS in older male populations, to our knowledge this is the first community-based study to analyze in detail LUTS among community-dwelling men aged 80 or older and thus provides novel information as to the prevalence and characteristics of LUTS in this rapidly expanding segment of the male population.
The Rancho Bernardo Study has, to our knowledge, the highest mean age (75 years), largest proportion of men over the age of 80 years (1 in 3), and the oldest living study participant (97 years) of any community-based cohort thus far reported in association with male lower urinary tract health. Prior studies of LUTS in older men include a postal survey in England, Scotland, and Wales and an analysis of participants in the U.S. Osteoporotic Fractures in Men (MrOS) cohort. 4,5
In the present cohort, 70% of those ≥ 80 years and 90% of those ≥ 90 years had LUTS. Compared to the younger men, those ≥ 80 years were 82% more likely to have LUTS and 112% more likely to report incomplete emptying, 83% more likely to report frequency, 76% more likely to report urgency, and 78% more likely to report weak stream. There were no significant differences in intermittency, straining, or nocturia. These data suggest that while LUTS prevalence and severity generally increase with age, several symptom domains in older men differ from those in younger men.
The mean quality of life domain scores were slightly higher among the older men, which likely reflects survival bias of healthier elderly, adaptation to age-related health changes, or comparison with one’s age-peer group. In fact, the proportion of older men complaining of substantially reduced quality of life—those evincing “mixed,” “mostly dissatisfied,” “unhappy,” or “terrible” attitudes toward their urinary symptoms—did not differ significantly from the younger men. Perhaps older men perceive their urinary symptoms differently than younger men—an observation with potentially important implications for choice of treatment, as the treating physician may employ the quality of life domain on the AUA-SI to determine the appropriateness of selecting medical or surgical therapy or watchful waiting as primary treatment.
We perceived no discernible pattern to readily explain the differences in symptom domain scores between age brackets. Not surprisingly, the prevalence of BPH was higher among the older men; thus, increased bladder outlet obstruction secondary to age-related prostate growth may have contributed to this observation. However, the 4 symptom domains that were worsened in the older men represented a mix of storage-and voiding-related complaints. Other potential explanations as to why some symptoms were more pronounced in the older men include objective changes in bladder function and differences in the perception of symptoms. Future studies using urodynamics data and/or additional quality of life measures may provide additional insights into these observations.
Our findings are consistent with other cohort studies in Europe and the U.S. demonstrating an extraordinarily high prevalence of LUTS among community-dwelling older men, underscoring the importance of this issue to the public health.1–5 However, while we found that LUTS prevalence increased steadily with age, prior analyses have produced inconsistent results in this regard. In the UK postal survey, LUTS prevalence increased into the 8th decade of life: from 29% in 50- to 60-year-olds to 41% in 71- to 80-year-olds.5 In both BACH and MrOS, however, LUTS prevalence peaked during the 7th decade, then subsequently declined. In the BACH cohort, LUTS prevalence was 35% for 60- to 69-year-olds and 25% for 70- to 79-year-olds;3 in MrOS, the prevalence in 65- to 69-year-olds was 53%, but in 75- to 79- year-olds it was 49% and in those ≥ 80 years it was 39%.4 Possible explanations for these discrepancies include survival bias; differences in treatment patterns, which may have resulted in differential expression of symptoms across cohorts; demographic differences in the study populations; and temporal differences reflecting the disparate time periods during which the data were collected: the 1990s for the UK postal survey, 2002 to 2005 for the BACH and MrOS surveys, and 2006 for the Rancho Bernardo cohort. Further longitudinal studies are needed to ascertain the natural history of LUTS in much older men.
There are three caveats of our analysis worth addressing. First, the relatively homogenous character of the Rancho Bernardo cohort—mostly white and upper middle class—likely limits the translation of these findings to other socioeconomic and ethnic/racial groups. Although BACH was a more racially and economically diverse sample, that study (like ours) drew from a narrow geographic region. Second, our study population was relatively small, thus limiting the precision of our effect estimates. Nevertheless, our study details LUTS in the largest analysis of men aged 80 or older reported to date. Finally, health status instruments (i.e., the Medical Outcomes Survey SF-12)4 and additional quality of life measures would have provided a more comprehensive outlook on the association of LUTS with health outcomes in these men.
In summary, in this cohort, the prevalence and severity of LUTS continued to increase for men into their 90s. Compared to younger men, men over 80 were more likely to have LUTS and more likely to complain of incomplete emptying, frequency, urgency, and weak stream. These data show that although the prevalence of LUTS in older men is higher, the symptom patterns change with age. Larger studies are needed to better understand these differences.
Acknowledgments
Funding: This study was supported by research grants from the National Institutes of Health on Aging: AG07181 and the National Institute of Diabetes and Digestive and Kidney Diseases: DK31801. Dr. Parsons was supported in part by UCSD Faculty Senate Grant #RF821H.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wei JT, Calhoun E, Jacobsen SJ. Urologic diseases in America project: benign prostatic hyperplasia. J Urol. 2005;173:1256–1261. doi: 10.1097/01.ju.0000155709.37840.fe. [DOI] [PubMed] [Google Scholar]
- 2.Boyle P, Robertson C, Mazzetta C, et al. The prevalence of lower urinary tract symptoms in men and women in four centres: the UrEpik study. BJU Int. 2003;92:409–414. doi: 10.1046/j.1464-410x.2003.04369.x. [DOI] [PubMed] [Google Scholar]
- 3.Kupelian V, Wei JT, O'Leary MP, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) Survey. Arch Intern Med. 2006;166:2381–2387. doi: 10.1001/archinte.166.21.2381. [DOI] [PubMed] [Google Scholar]
- 4.Taylor BC, Wilt TJ, Fink HA, et al. Prevalence, severity, and health correlates of lower urinary tract symptoms among older men: the MrOS study. Urology. 2006;68:804–809. doi: 10.1016/j.urology.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 5.Trueman P, Hood SC, Nayak US, et al. Prevalence of lower urinary tract symptoms and self-reported diagnosed 'benign prostatic hyperplasia', and their effect on quality of life in a community-based survey of men in the UK. BJU Int. 1999;83:410–415. doi: 10.1046/j.1464-410x.1999.00966.x. [DOI] [PubMed] [Google Scholar]
- 6.Welch G, Weinger K, Barry MJ. Quality-of-life impact of lower urinary tract symptom severity: results from the Health Professionals Follow-up Study. Urology. 2002;59:245–250. doi: 10.1016/s0090-4295(01)01506-0. [DOI] [PubMed] [Google Scholar]
- 7.Saigal CS, Joyce G. Economic costs of benign prostatic hyperplasia in the private sector. J Urol. 2005;173:1309–1313. doi: 10.1097/01.ju.0000152318.79184.6f. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control. Public Health and Aging: Trends in Aging—United States and Worldwide. MMWR Morb Mortal Wkly Rep. 2003;52:101–104. [PubMed] [Google Scholar]
- 9.Barry MJ, Fowler FJ, Jr, O'Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–1557. doi: 10.1016/s0022-5347(17)36966-5. [DOI] [PubMed] [Google Scholar]