Abstract
This study evaluated the Penn State Worry Questionnaire, Penn State Worry Questionnaire—Abbreviated, and the Generalized Anxiety Disorder Questionnaire-IV for identifying generalized anxiety disorder in older medical patients. Participants were 191 of 281 patients screened for a clinical trial evaluating cognitive-behavior treatment, n = 110 with generalized anxiety disorder, 81 without. Participants completed the Penn State Worry Questionnaire and Generalized Anxiety Disorder Questionnaire-IV at pretreatment. Kappa coefficients estimated agreement with the Structured Clinical Interview for Diagnosis. Receiver operating characteristic curves compared sensitivity and specificity of self-report measures. The Penn State Worry Questionnaire (cutoff = 50) provided the strongest prediction of generalized anxiety disorder (sensitivity, 76%; specificity, 73%; 75% correctly classified; kappa = .49. Item 2 of the Generalized Anxiety Disorder Questionnaire-IV demonstrated comparable accuracy. The Penn State Worry Questionnaire, Generalized Anxiety Disorder Questionnaire-IV, and briefer versions of these measures may be useful in identifying late-life generalized anxiety disorder in medical settings.
Keywords: late-life anxiety, PSWQ, GAD-Q-IV, PRIME-MD, primary care psychology, sensitivity, specificity
Introduction
Anxiety disorders are prevalent among older adults,1 with serious consequences, including decreased quality of life, increased disability, reduced functional status, and increased health service use.2-5 Late-life anxiety is associated with decreased physical activity, poor self-perceptions of health, decreased life satisfaction, and increased loneliness, even after adjusting for demographic variables and severity of chronic illness.3,6 Anxiety symptoms in older adults have predicted increased frequency of incontinence and falling in longitudinal community studies,7,8 as well as increased functional dependence, one of the most important health outcomes for elderly persons. In a study of bathing disability in community-dwelling older adults, fear of falling was one of the top 3 reasons people were unable to bathe without assistance.9 Late-life anxiety is also a predictor of the progression of worsening disability in functionally limited women older than 65.2
According to community prevalence studies, generalized anxiety disorder (GAD) is one of the most prevalent anxiety disorders in later life, with rates ranging from 3.6%10 to 7.3%.1 Late-life GAD is also frequently found in primary care settings, with prevalence rates of 2.4%11 to 11.2%.12 In both community and primary care settings, prevalence of GAD is higher than prevalence of panic disorder or posttraumatic stress disorder (PTSD).1,10,12,13 Coexistent psychiatric disorders are common among older adults with GAD,14,15 although GAD itself is a pervasive and chronic disorder that creates significantly decreased quality of life.16 Although rates of coexistent depressive disorders are high,17,18 GAD often precedes onset of depression, suggesting it may be a risk factor18-20 and therefore important to identify apart from coexisting syndromes.
Older adults with GAD and other forms of anxiety most often present for assistance to primary care settings, where anxiety symptoms frequently go unrecognized and untreated.21-23 A naturalistic study in ambulatory medical care settings, in fact, suggested that anxiety disorders are rarely diagnosed during office visits made by older adults (1.3%), in spite of the high prevalence and significant impact of late-life anxiety.4 Generalized anxiety disorder can be difficult to diagnose in primary care settings because many associated symptoms (sleep disturbance, fatigue, restlessness, difficulty concentrating) overlap with symptoms of normal aging, medical conditions, and medications common in later life. Diagnosis and assessment of GAD is further complicated in older patients because they tend to minimize psychological symptoms and emphasize somatic symptoms.24-26 A recent large study of GAD and major depression in primary care demonstrated that patients diagnosed with GAD most often presented with complaints of somatic illness and pain, and that physicians were able to diagnose GAD in these patients with only 34% accuracy.11 The disorder also is difficult to detect in older adults with physical disability or chronic medical illness during brief visits with primary care physicians when the focus is on adaptive worry about significant medical issues. Within such time constraints and selective focus, the patient might not demonstrate enough pathological worry or other distinctive GAD symptoms to trigger the physician to probe further or refer the patient for a more in-depth psychological evaluation. Therefore, assessments for late-life GAD need to target worry, anxiety, and physical symptoms to aid in differentiating medical symptoms from anxiety.27
Several measures are reliable and valid for assessing GAD and related anxiety in older adults, including the Beck Anxiety Inventory (BAI),28 the Spielberger State-Trait Anxiety Inventory (STAI),29 the Penn State Worry Questionnaire (PSWQ),30 and The Worry Scale.31 Although several of these are used effectively in academic and mental health settings, assessment of late-life GAD in primary care settings still poses many challenges. Of particular interest is the need to know how to identify late-life GAD effectively and efficiently. Brief and accurate self-report assessment strategies for identifying late-life GAD could facilitate decisions about diagnosis, treatment, consultation, and/or referral in primary care.32 Any effective assessment strategy, however, will have to overcome the challenges of the primary care setting, including limited time, scarce financial resources, and lack of clinic staff familiarity with psychiatric disorders.
One possible instrument for identifying late-life GAD is The Primary Care Evaluation of Mental Disorders (PRIME-MD),33 which includes a 1-page patient questionnaire (PHQ), followed by a 12-page clinician evaluation guide. The PRIME-MD was developed to help primary care physicians accurately and efficiently diagnose mental health problems. Nearly one half (48%) of 287 patients evaluated with this instrument who were fairly well known by their physicians were diagnosed, even though their symptoms had not been recognized before.33 The PRIME-MD showed good agreement with the diagnoses made by independent mental health professionals (kappa = .71, overall accuracy of 88%).
Although the full PRIME-MD took only 8.4 minutes on average, this is a significant amount of time for a primary care setting. Recent studies have supported the validity of the 2-question depression and 3-question anxiety components of the PHQ as a screening tool for adults in primary care.34,35 However, although the PHQ is a highly sensitive screening tool, it may not provide enough specificity for diagnosis and clinical decision-making.34 This measure was used in a recent investigation to screen adult primary care patients for anxiety.36 In this study, however, research staff administered the 14-question follow-up Anxiety Module from the PRIME-MD interview to determine diagnoses of GAD and/or panic. The study did not address the value of the screening questions for identifying patients with anxiety diagnoses. Furthermore, in a primary care setting, the interview component of this kind of assessment may not be feasible because of time constraints. A follow-up self-report questionnaire providing information on all Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnostic criteria for GAD in place of the PRIME-MD interview questions could facilitate diagnosis of late-life GAD, with less physician time to reach diagnosis.
One of the most widely used GAD self-report measures, the PSWQ,30 assesses worry severity but does not assess other DSM-IV criteria for GAD (eg, control of worry, associated physical symptoms, impairment/distress). However, the measure has shown good discriminant validity in distinguishing between individuals with and without GAD.5,32,37 An abbreviated version of the PSWQ (PSWQ-A) was developed for older adults in response to findings that factor solutions of the PSWQ with younger populations do not adequately fit data for older adults meeting criteria for GAD.32 Cutoff scores of 50 (PSWQ) and 22 (PSWQ-A) have been suggested to predict GAD in samples of older medical patients referred for anxiety.5 Therefore, the PSWQ and the PSWQ-A may be good measures for identifying late-life GAD, despite not having items to evaluate all DSM-IV criteria for GAD.
The Generalized Anxiety Disorder Questionnaire-IV (GAD-Q-IV)38 is a potential assessment alternative that may better identify GAD in older primary care patients. This self-report questionnaire was developed and validated in younger clinical samples to directly and efficiently assess DSM-IV criteria for GAD. Although the GAD-Q-IV has shown strong psychometrics with younger populations, previous studies have not examined how it functions with older populations. One strength of the GAD-Q-IV is that, in addition to assessing for worry severity, it provides a thorough evaluation of GAD symptoms with self-report assessment of DSM-IV criteria. Assessment of physical symptoms and complete evaluation of DSM-IV criteria may improve identification of late-life GAD in primary care settings.
The goal of this study was to evaluate the relative utility of the GAD-Q-IV, PSWQ, and the PSWQ-A for identifying late-life GAD in patients who screened positive for anxiety on the PHQ in primary care settings. Based on its attention to the DSM-IV diagnostic criteria for GAD, the GAD-Q-IV was expected to provide better identification of late-life GAD diagnostic status than the PSWQ or PSWQ-A for patients referred for anxiety and depression.
METHODS
Participants
Participants were 191 of 281 patients screened for an ongoing randomized clinical trial evaluating the effectiveness of cognitive-behavior treatment for primary care GAD patients aged 60 and above. Participants were recruited from 2 large clinic sites associated with the Kelsey-Seybold Clinic, a large multispecialty health care provider in the Houston area, from March 2004 to April 2006. Recruitment methods included physician referrals, letters of invitation to patients, and/or educational brochures placed in waiting and examination rooms. For 6 months, recruitment also occurred in the Baylor College of Medicine Family Medicine Clinic. Research clinicians affiliated with the study provided education and outreach to primary care staff to facilitate physician referrals and build collaborative relationships.
Of 733 primary care patients referred to the study (73% self-referred, 21% physician referred, 6% with no data about referral source), 688 (94%) were able to be contacted. Information on demographics and reasons for refusal was not collected from patients who refused to participate. 281 signed consent to participate. These patients were screened for anxiety with 2 questions from the PRIME-MD (“During the past month, have you often been bothered by “nerves” or feeling anxious or on edge?” and “During the past month, have you often been bothered by worrying about a lot of different things?”).
Of the 281 patients who consented to participate, 61 subsequently withdrew or were dropped because of lack of interest (n = 21, 7.5%), negative screen for anxiety (n = 11, 3.9%), inability to be contacted/scheduled (n = 10, 3.6%), or unknown reasons (n = 19, 6.8%).
Thus, 220 participants completed a subsequent diagnostic session, which entailed a cognitive screen using the Mini-Mental State Exam (MMSE)39 and the Structured Clinical Interview for Diagnosis (SCID).40 All SCID interviews were administered by trained clinicians and audiotaped to estimate reliability. Kappa coefficients from the ongoing clinical trial indicate adequate agreement for diagnosis of GAD (.64) that is comparable to figures from other studies.41 Interrater agreement for other diagnostic categories is as follows: depression (kappa = .75), all anxiety disorders combined (kappa = .73), social phobia (kappa = .81), and specific phobia (kappa = .62).
Of the 220 patients assessed, 29 were excluded from the final data set: 14 due to MMSE scores less than 24, 2 for being under 60, 11 for missing GAD-Q-IV data (7 of whom did not respond to item 2), and 2 for missing PSWQ data. The sample used for analyses included 191 patients. Of these, 110 were diagnosed with GAD, and 81 were not diagnosed with GAD. Of the 110 diagnosed with GAD, 55 (50%) were also diagnosed with depression (includes major depressive disorder, dysthymia, bipolar depression, and depression disorder NOS). Comorbid anxiety disorders in the GAD sample included 41 (37%) phobia, 15 (14%) panic disorder and/or agoraphobia, and 3 (3%) PTSD. Of the 81 not diagnosed with GAD, 30 (37%) were diagnosed with depression (15 of whom also had a coexistent anxiety disorder). Another 14 (17%) had an anxiety disorder without depression, 6 (7%) had an alternative diagnosis (eg, adjustment disorder, substance abuse), and 31 (38%) had no diagnosis. ANOVA showed significant differences between patients included in the analyses and those excluded on age, F(1,274) = 7.29, P < .007, and education, F(1,274) = 11.00, P < .001. Included patients were slightly younger and better educated. Chi-square analyses indicated no other differences between included and excluded patients on any other demographic variables.
Procedure
Patients completed the GAD-Q-IV, PSWQ, and demographics form at the time of diagnostic evaluation. The GAD-Q-IV was scored using the original sum total response scoring method suggested by its developers to best reflect the DSM-IV diagnostic threshold for GAD diagnosis.38 According to the developers’ scoring procedure, all yes responses were coded as 1, and all no answers were coded as 0. For item 5 that assesses for number of worry topics, participants were given 1 point for each worry topic listed (up to a maximum of 6 points), and this total was divided by 3. Item 7, which assesses for associated physical symptoms, was scored in the same manner as item 5. For items 8 and 9 that assess degree of distress and interference on a scale of 0 to 8, each was divided by 4 and then added together. Skipped items were scored as 0. Total scores range from 0 to 13. The PSWQ was scored using sum total score for both the full version30 and abbreviated version suggested for use with older populations.32
Data Analysis
Chi-square and ANOVA analyses were used to examine demographic differences between the GAD and no GAD groups. SCID diagnoses were used as the gold standard for comparison with diagnostic classification according to the PSWQ and GAD-Q-IV, and kappa coefficients were computed to estimate relative agreement between these 2 methods. Another set of kappa coefficients evaluated the value of separate GAD-Q-IV items (items 1, 2, 4, and 6) for identifying late-life GAD, again in comparison with the SCID. Specificity, sensitivity, positive predictive values (PPV), and negative predictive values (NPV) were calculated for the self-report measures. Receiver operating characteristic (ROC) curves42,43 were plotted for the GAD-Q-IV, PSWQ, and PSWQ-A scores to compare the sensitivity and specificity of each as a diagnostic measure for late-life GAD. The accuracy of a diagnostic test is evaluated by the area under the ROC curve (AUC), with an area of 1 representing a perfect test and an area of .5 representing a useless test. Exploratory analyses addressed the relative utility of self-report measures for diagnosing late-life GAD across different clinical and demographic groups. Separate ROC curves were plotted for subgroups of the sample based on comorbid depression (present, absent), race (white, black), education (less than college and at least some college), and income (less or more than the mean of $44 600).
Results
Demographic data are presented in Table 1, along with means and standard deviations for the PSWQ, PSWQ-A, and GAD-Q-IV. The distribution of racial groups is representative of the Houston area, and the gender differences reflect the higher prevalence in women typically found for anxiety disorders. Chi-square analyses and ANOVAs indicated no differences between the GAD and no GAD groups on any demographic variable. As expected, ANOVA analyses showed significant mean differences between the GAD and no GAD groups on the PSWQ, F(1,189) = 64.20, P < .001, PSWQ-A,F(1, 189) = 72.78, P < .001, and the GAD-Q-IV,F(1, 189) = 69.16, P < .001.
Table 1.
Demographic and Clinical Data for Patients With/Without GAD
| Total Sample, N (%) | With GAD, N (%) | Without GAD, N (%) | |
|---|---|---|---|
| Gender | |||
| Female | 136 (71.2) | 80 (72.7) | 56 (69.1) |
| Race | |||
| White | 139 (72.8) | 86 (78.2) | 53 (65.4) |
| Black | 46 (24.1) | 20 (18.2) | 26 (32.1) |
| Asian | 2 (1.0) | 2 (1.8) | 0 (0.0) |
| Ethnicity | |||
| Hispanic | 17 (8.9) | 13 (11.8) | 4 (4.9) |
| Not hispanic | 168 (88.0) | 95 (86.4) | 73 (90.1) |
| Marital Status | |||
| Married | 112 (58.6) | 71 (64.5) | 41 (50.6) |
| Widowed | 30 (15.7) | 16 (14.5) | 14 (17.3) |
| Separated | 5 (2.6) | 2 (1.8) | 3 (3.7) |
| Divorced | 38 (19.9) | 20 (18.2) | 18 (22.2) |
| Single | 5 (2.6) | 1 (0.9) | 4 (4.9) |
| M (SD) | M (SD) | M (SD) | |
| Age | 67.56 (5.91) | 67.23 (5.93) | 68.01 (5.89) |
| Income | $44 600 (1969) | $46 700 (1927) | $41 700 (2003) |
| Education | 15.72 (3.15) | 15.81 (3.23) | 15.60 (3.05) |
| Anx | |||
| PSWQ | 52.45 (12.85) | 58.14a (11.06) | 44.72a (10.96) |
| PSWQ-A | 24.57 (7.92) | 28.15a (6.80) | 19.72a (6.68) |
| GAD-Q-IV | 4.99 (3.49) | 6.50a (3.05) | 2.95a (3.00) |
Abbreviations: GAD, generalized anxiety disorder; PSWQ, Penn State Worry Questionnaire; PSWQ-A, Penn State Worry Questionnaire-Abbreviated; GAD-Q-IV, Generalized Anxiety Disorder Questionnaire-IV; anx, anxiety.
Signified by differences at P < .001.
Kappa coefficients estimating relative agreement between SCID diagnoses and the different self-report questionnaire cutoff points are presented in Tables 2 and 3. The PSWQ provided the most accurate prediction of GAD diagnosis, according to estimates of sensitivity, specificity, PPV, and NPV. The full-scale PSWQ cutoff also had the strongest diagnostic agreement with the SCID interview. The PSWQ-A and the GAD-Q-IV cutoff methods demonstrated very similar accuracy in predicting GAD diagnostic status, and both were only slightly less accurate than the full PSWQ. Both the PSWQ-A and GAD-Q-IV provided adequate prediction of GAD diagnostic status, although kappa coefficients indicating agreement with SCID diagnoses were not high.
Table 2.
PSWQ and PSWQ-A: Sensitivity, Specificity, Positive Predictive Values, and Negative Predictive Values
| PSWQ Cut point = 50 |
PSWQ-A Cut point = 22 |
Totals | |||
|---|---|---|---|---|---|
| GAD present | GAD absent | GAD present | GAD absent | ||
| SCID Dx (%) | |||||
| GAD present (%) | 86 (45) | 24 (13) | 87 (46) | 23 (12) | N = 110 (58) |
| GAD absent (%) | 24 (13) | 57 (29) | 30 (15) | 51 (27) | N = 81 (42) |
| Totals (%) | 110 (58) | 81 (42) | 117 (61) | 74 (39) | N = 191 (100) |
| Sensitivity (%) | 78 | 79 | |||
| Specificity (%) | 70 | 63 | |||
| Positive predictive value (%) | 78 | 74 | |||
| Negative predictive value (%) | 70 | 69 | |||
| Correctly classified (%) | 143 (75) | 138 (72) | |||
| Kappa reliabilities between questionnaire cutoff method and SCID (%) | Kappa = .48 | Kappa = .43 | |||
Abbreviations: Dx, diagnosis; GAD, generalized anxiety disorder; PSWQ, Penn State Worry Questionnaire; PSWQ-A, Penn State Worry Questionnaire-Abbreviated; SCID, Structured Clinical Interview for Diagnosis.
Table 3.
GAD-Q-IV With Cut Points of 4.5 and Item 2: Sensitivity, Specificity, Positive Predictive Value, Negative Predictive Value, Kappa Table
| GAD-Q-IV Cut point = 4.5 |
GAD-Q-IV Item 2 |
Totals | |||
|---|---|---|---|---|---|
| GAD present | GAD absent | GAD present | GAD absent | ||
| SCID Dx | |||||
| GAD present (%) | 75 (39) | 35 (18) | 86 (45) | 24 (13) | N = 110 (58) |
| GAD absent (%) | 23 (12) | 58 (31) | 25 (15) | 56 (27) | N = 81 (42) |
| Totals (%) | 98 (51) | 93 (49) | 111 (61) | 80 (39) | N = 191 (100) |
| Sensitivity (%) | 68 | 78 | |||
| Specificity (%) | 72 | 69 | |||
| Positive predictive value (%) | 77 | 77 | |||
| Negative predictive value (%) | 62 | 70 | |||
| Correctly classified (%) | 133 (70) | 142 (74) | |||
| Kappa reliabilities between questionnaire cutoff method and SCID | Kappa = .39 | Kappa = .47 |
Abbreviations: GAD, generalized anxiety disorder; GAD-Q-IV, Generalized Anxiety Disorder Questionnaire-IV; SCID, Structured Clinical Interview for Diagnosis.
Kappa coefficients for individual GAD-Q-IV items ranged from .25 to .47, with item 2 demonstrating strongest agreement with SCID diagnoses. Interestingly, item 2 of the GAD-Q-IV demonstrated comparable accuracy to the best of the full-scale cutoff methods (PSWQ) tested in the current study. Item 2 of the GAD-Q-IV asks, “Is your worry excessive in intensity, frequency, or the amount of distress it causes?”
Receiver operating characteristic curves for the PSWQ, the PSWQ-A, and the GAD-Q-IV are presented in Figure 1. The AUC for the PSWQ was .81 (SE = .032), P < .001. The 95% confidence interval (CI) of the AUC ranged from .75 to .87. Therefore, there is an 81% probability that a patient with GAD will have a higher score on the GAD-Q-IV than a patient without GAD. The ROC curve accuracy indices for the PSWQ-A were identical to the PSWQ, with an AUC of .81 (SE = .032), P < .001. The 95% CI of the AUC ranged from .75 to .87. The GAD-Q-IV demonstrated nearly identical accuracy with an AUC of .80 (SE = .033), P < .001. The 95% CI of the AUC ranged from .74 to .87.
Figure 1.
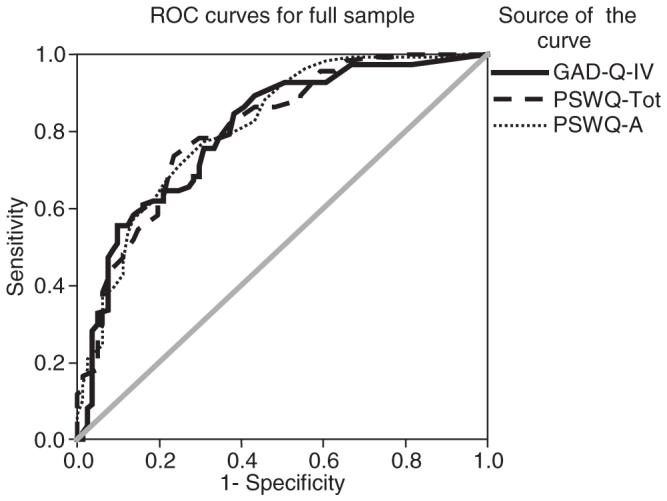
Receiver operating curves for the full sample. GAD-Q-IV = Generalized Anxiety Disorder Questionnaire-IV; ROC = Receiver operating characteristic; PSWQ-Tot = Penn State Worry Questionnaire—Total; PSWQ-A = Penn State Worry Questionnaire—Abbreviated.
Receiver operating characteristic curves were plotted for patients with and without mood disorder diagnoses. All 3 instruments demonstrated similar accuracy for identifying GAD in the absence of mood disorders, with slightly improved accuracy (10% improvement) for patients without mood disorder diagnoses (AUC = .84, PSWQ; .85, PSWQ-A; .84, GAD-Q-IV) than for patients with mood disorder diagnoses (AUC = .74, PSWQ; .74, PSWQ-A; .74, GAD-Q-IV). All 3 measures also provided slightly better accuracy (average, 11%) among the black subgroup (AUC = .89, PSWQ; .91, PSWQ-A; .89, GAD-Q-IV) relative to the white subgroup (AUC = .78, PSWQ; .78, PSWQ-A; .80, GAD-Q-IV). The GAD-Q-IV demonstrated greater accuracy for patients with more education (AUC = .83, some college; .68, high school or less), and all measures identified GAD more accurately for patients with higher income (income above $44 600: AUC = .85, PSWQ; .89, PSWQ-A; .83, GAD-Q-IV; income below $44 600: AUC = .78, PSWQ; .76, PSWQ-A; .78, GAD-Q-IV).
Discussion
The current study provides preliminary support for the GAD-Q-IV, PSWQ, and PSWQ-A in identifying late-life GAD in primary care settings among patients who screen positive for anxiety according to the PHQ. All 3 measures demonstrated strong and similar sensitivity, specificity, and accuracy; but they involve different costs and benefits for assessment of late-life GAD in primary care settings. The practical limitations within primary care related to time, cost, prioritization of physical symptoms, and absence of mental health expertise strongly influence the potential utility of different assessment strategies. Although all 3 measures provide strong self-report identification of GAD, the GAD-Q-IV provides additional information on physical symptoms and DSM-IV criteria particularly relevant in primary care and other medical settings.
The potential value of a single item (2) from the GAD-Q-IV for facilitating diagnosis of GAD is suggested by the remarkably similar sensitivity, specificity, PPV, NPV, and kappa to the PSWQ and the full GAD-Q-IV. If a single question can provide the information needed for facilitating diagnosis, treatment, and referral decisions after an initial screen, this strategy would be more feasible and useful in primary care settings. Of course, future studies will need to test the viability of using the GAD-Q-IV item 2 alone to identify patients with GAD because only the full version was tested here.
Because GAD occurs so frequently with coexistent depression, it was important to evaluate the utility of all instruments to identify GAD when mood disorders were or were not present. All 3 measures demonstrated strong and similar accuracy for patients with and without coexistent mood disorders, with slightly more accuracy among nondepressed patients. These findings support the value of these measures to identify GAD that might be missed if only depression assessment tools were used.
Results also indicate the possibility of slight differences in accuracy of measures based on demographic variables. As might be expected, self-report measures were more accurate with increased education and income, with the largest differences found for the GAD-Q-IV. The higher-level vocabulary of the GAD-Q-IV may explain some of these differences, but given the relatively smaller sample of participants with less than college education (n = 25), these results remain tentative. The GAD-Q-IV may not be appropriate or may need to be modified for use in patient populations with lower education levels.
There are several important limitations to the current study. One serious limitation is that all patients included in this study were either self-referred or physician-referred from primary care clinics for evaluation of anxiety. Furthermore, they all screened positive for anxiety according to questions from the PHQ. This selection bias limits the generalizability of findings to older primary care patients who have already been identified as anxious. The lack of information about referred patients who refused to participate also limits generalizability of findings. Given these limitations to generalizability, different cut points may apply to older primary care patients who have not been prescreened as anxious. Future studies should address the use of these measures for older primary care patients who have not already screened positive for anxiety and who are not seeking treatment.
A second limitation involves the format of the GAD-Q-IV. For example, the discontinue instructions on this measure limit its ability to assess fully for physical symptoms. Eliminating these instructions would allow measurement of physical symptoms regardless of self-reported worry severity and might allow the scale to better represent overall symptom severity. Some language included in the GAD-Q-IV also may be difficult for older adults to understand. For example, the term excessive is difficult to apply to oneself without clinical perspective. In addition, the word excessive is included in 5 of the first 6 items and may be too repetitive.
Another significant limitation of this study involves the ordering of assessments during the diagnostic session. The self-report measures were administered after the SCID interview, which may have primed the participants’ later responses on the questionnaires. To evaluate more fully the accuracy of these self-report methods, future studies will need to counterbalance the assessments.
Even after the recommendations a decade ago of the US Preventive Services Task Force44 for routine screening for psychiatric symptoms with sensitive measurements, late-life anxiety is still underrecognized and undertreated in primary care settings.4,5,21,22,45 With the decreased functioning, health status, and quality of life associated with late-life anxiety, it is very important that older patients suffering with GAD receive accurate diagnosis and treatment in the primary care settings where they often present for help. More research is needed to continue to develop and validate screening and diagnostic measures for use in primary care with diverse populations. Self-report assessment of mental health symptoms improves treatment outcomes for patients seen by outpatient mental health providers.46 Similar self-report assessments such as the PSWQ and the GAD-Q-IV could provide a convenient and cost-effective measure for use in primary care for identifying GAD after a more general screening instrument such as the PHQ. The GAD-Q-IV, in particular, could be a potentially useful self-report screening and diagnostic tool. It could be used in conjunction with the PHQ by asking patients who screen positive for anxiety to complete the GAD-Q-IV in the waiting room. This would provide physicians with all of the information about DSM-IV criteria necessary to make a diagnosis of GAD without requiring any additional interview time. The GAD-Q-IV may also prove, with further study, to be a useful stand-alone screening and diagnostic tool for GAD, as item 2 is highly predictive of a diagnosis. Use of such self-report measures could also improve mental health treatment outcomes by increasing the number of patients accurately recognized with late-life GAD.
Acknowledgments
This research was supported by Grant 53932 from the National Institute of Mental Health to the last author. We thank Anthony Greisinger and the staff of the Kelsey Research Foundation and Kelsey-Seybold Clinic, who provided consultation and assisted with recruitment. Portions of this work were presented at the 2005 convention for the Association for Behavioral and Cognitive Therapies, November, Washington, D.C.
References
- 1.Beekman ATF, Bremmer MA, Deeg DJH, et al. Anxiety disorders in later life: a report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry. 1998;13:717–726. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 2.Brenes GA, Guralnik JM, Williamson JD, et al. The influence of anxiety on the progression of disability. J Am Geriatr Soc. 2005;53:34–39. doi: 10.1111/j.1532-5415.2005.53007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.deBeurs E, Beekman ATF, van Balkom AJLM, Deeg DJ, van Dyck R, van Tilburg W. Consequences of anxiety in older persons: its effect on disability, well-being and use of health services. Psychol Med. 1999;29:583–593. doi: 10.1017/s0033291799008351. [DOI] [PubMed] [Google Scholar]
- 4.Stanley MA, Roberts RE, Bourland SL, Novy DM. Anxiety disorders among older primary care patients. J Clin Geropsychol. 2001;7:105–116. [Google Scholar]
- 5.Stanley MA, Diefenbach GJ, Hopko DR, et al. The nature of generalized anxiety in older primary care patients: preliminary findings. J Psychopathol Behav Assess. 2003;25:273–280. [Google Scholar]
- 6.Kim HF, Kunik ME, Molinari VA, et al. Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics. 2000;41:465–471. doi: 10.1176/appi.psy.41.6.465. [DOI] [PubMed] [Google Scholar]
- 7.Lenze EJ, Rogers JC, Martire LM, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- 8.Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factor for falls, incontinence, and functional dependence: unifying the approach to geriatric syndromes. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- 9.Naik AD, Concato J, Gill TM. Bathing disability in community-living older persons: common, consequential, and complex. J Am Geriatr Soc. 2004;52:1805–1810. doi: 10.1111/j.1532-5415.2004.52513.x. [DOI] [PubMed] [Google Scholar]
- 10.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorobidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 11.Wittchen HU, Kessler RC, Beesdo K, Krause P, Höfler M, Hoyer J. Generalized anxiety and depression in primary care: prevalence, recognition, and management. J Clin Psychiatry. 2002;63:24–34. [PubMed] [Google Scholar]
- 12.Tolin DF, Robison JT, Gaztambide S, Blank K. Anxiety disorders in older Puerto Rican primary care patients. Am J Geriatr Psychiatry. 2005;13:150–156. doi: 10.1176/appi.ajgp.13.2.150. [DOI] [PubMed] [Google Scholar]
- 13.Rauch SAM, Morales KH, Zubritsky C, Knott K, Oslin D. Posttraumatic stress, depression and health among older adults in primary care. Am J Geriatr Psychiatry. 2006;14:316–324. doi: 10.1097/01.JGP.0000199382.96115.86. [DOI] [PubMed] [Google Scholar]
- 14.Stanley MA, Beck JG, Novy DM, et al. Cognitive-behavioral treatment of late-life generalized anxiety disorder. J Consult Clin Psychol. 2003;71:309–319. doi: 10.1037/0022-006x.71.2.309. [DOI] [PubMed] [Google Scholar]
- 15.Wetherell JL, Gatz M, Craske MG. Treatment of generalized anxiety disorder in older adults. J Consult Clin Psychol. 2003;71:31–40. doi: 10.1037//0022-006x.71.1.31. [DOI] [PubMed] [Google Scholar]
- 16.Bourland SL, Stanley MA, Synder AG, Novy DM, Beck JG, Averill PM. Quality of life in older adults with generalized anxiety disorder. Aging Ment Health. 2000;4:315–323. [Google Scholar]
- 17.Beekman AT, de Beurs E, van Balkom AJ, Deeg DJ, van Dyck R, van Tilburg W. Anxiety and depression in later life: co-occurrence and communality of risk factors. Am J Psychiatry. 2000;157:89–95. doi: 10.1176/ajp.157.1.89. [DOI] [PubMed] [Google Scholar]
- 18.Lenze EJ, Mulsant BH, Shear MK, et al. Comorbid anxiety disorders in depressed elderly patients. Am J Psychiatry. 2000;57:722–728. doi: 10.1176/appi.ajp.157.5.722. [DOI] [PubMed] [Google Scholar]
- 19.Schoevers RA, Deeg DJ, van Tilburg W, Beekman AT. Depression and generalized anxiety disorder: co-occurrence and longitudinal patterns in elderly patients. Am J Geriatr Psychiatry. 2005;13:31–39. doi: 10.1176/appi.ajgp.13.1.31. [DOI] [PubMed] [Google Scholar]
- 20.Wetherell JL, Gatz M, Pedersen NL. A longitudinal analysis of anxiety and depressive symptoms. Psychol Aging. 2001;16:187–195. doi: 10.1037//0882-7974.16.2.187. [DOI] [PubMed] [Google Scholar]
- 21.Blazer D, George LK, Hughes D. The epidemiology of anxiety disorders: an age comparison. In: Salzman C, Lebowtiz BD, editors. Anxiety in the Elderly: Treatment and Research. Springer; New York, NY: 1991. pp. 17–30. [Google Scholar]
- 22.Barlow DH, Lerner JA, Esler JL. Behavioral health care in primary care settings: recognition and treatment of anxiety disorders. In: Reshick RJ, Rozensky RH, editors. Health Psychology Through the Life Span: Practice and Research Opportunities. American Psychological Association; Washington, DC: 1996. [Google Scholar]
- 23.Klap R, Unroe KT, Unutzer J. Caring for mental illness in the United States: a focus on older adults. Am J Geriatr Psychiatry. 2003;11:517–524. [PubMed] [Google Scholar]
- 24.Lenze EJ, Karp JF, Mulsant BH, et al. Somatic symptoms in late-life anxiety: treatment issues. J Geriatr Psychiatry Neurol. 2005;18:89–96. doi: 10.1177/0891988705276251. [DOI] [PubMed] [Google Scholar]
- 25.Salzman C. A primer on geriatric psychopharmacology. Am J Psychiatry. 1982;139:67–74. doi: 10.1176/ajp.139.1.67. [DOI] [PubMed] [Google Scholar]
- 26.Morin CM, Colecchi CA. Psychological assessment of older adults. In: Butcher J, editor. Clinical Personality Assessment: Practical Approaches. Oxford University Press; New York, NY: 1995. [Google Scholar]
- 27.Stanley MA, Beck JG. Anxiety disorders. Clin Psychol Rev. 2000;20:731–754. doi: 10.1016/s0272-7358(99)00064-1. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 29.Spielberger C, Gorsuch R, Lushene R. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto, CA: 1970. [Google Scholar]
- 30.Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 31.Wisocki PA, Handen B, Morse CK. The Worry Scale as a measure of anxiety among homebound and community active elderly. Behav Ther. 1986;5:91–95. [Google Scholar]
- 32.Hopko DR, Stanley MA, Reas DL, et al. Assessing worry in older adults: confirmatory factor analysis of the Penn State Worry Questionnaire and psychometric properties of an abbreviated model. Psychol Assess. 2003;15:173–183. doi: 10.1037/1040-3590.15.2.173. [DOI] [PubMed] [Google Scholar]
- 33.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 34.Kunik ME, Azzam PN, Souchek J, et al. A practical screening tool for anxiety and depression in patients with chronic breathing disorders. Psychosomatics. 2007;48:16–21. doi: 10.1176/appi.psy.48.1.16. [DOI] [PubMed] [Google Scholar]
- 35.Spitzer RL, Kroenke K, Williams JB. Validation and utility of the PRIME-MD Patient Health Questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 1999;183:759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 36.Rollman BL, Belnap BH, Mazumdar S, et al. Symptomatic severity of Prime-MD diagnosed episodes of panic and generalized anxiety disorder in primary care. J Gen Intern Med. 2005;20:623–628. doi: 10.1111/j.1525-1497.2005.0120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stanley MA, Beck JG, Zebb BJ. Psychometric properties of four anxiety measures in older adults. Behav Res Ther. 1996;34:827–838. doi: 10.1016/0005-7967(96)00064-2. [DOI] [PubMed] [Google Scholar]
- 38.Newman MG, Zuellig AR, Kachin KE, et al. Preliminary reliability and validity of the Generalized Anxiety Disorder Questionnaire-IV: a revised self-report diagnostic measure of generalized anxiety disorder. Behav Ther. 2002;33:215–233. [Google Scholar]
- 39.Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 40.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID): I. History, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 41.Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: implications for the classification of emotional disorders. J Abnorm Psychol. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- 42.Fresco DM, Mennin DS, Heimberg RG, Turk CL. Using the Penn State Worry Questionnaire to identify individuals with generalized anxiety disorder: a receiver operating characteristic analysis. J Behav Ther Exper Psychiatry. 2003;34:283–291. doi: 10.1016/j.jbtep.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 43.Weintraub D, Oehlberg KA, Katz IR, Stern MB. Test characteristics of the 15-item Geriatric Depression Scale and Hamilton Depression Rating Scale in Parkinson disease. Am J Geriatr Psychiatry. 2006;14:169–175. doi: 10.1097/01.JGP.0000192488.66049.4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.US Preventive Services Task Force . Guide to Clinical Preventive Services. 2nd ed. Office of Prevention and Health Promotion; Washington, DC: 1996. [Google Scholar]
- 45.Harmen JS, Rollman BL, Hanusa BH, Lenze EJ, Shear MK. Physician office visits of adults for anxiety disorders in the United States, 1985-1998. J Gen Intern Med. 2002;17:165–172. doi: 10.1046/j.1525-1497.2002.10409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brodey BB, Cuffel B, McCulloch J, et al. The acceptability and effectiveness of patient-reported assessments and feedback in a managed behavioral healthcare setting. Am J Manag Care. 2005;11:774–780. [PubMed] [Google Scholar]


