Abstract
This study tested whether the Risk Perception Attitude Framework predicted nutrition-related cancer prevention cognitions and behavioral intentions. Data from the 2003 Health Information National Trends Survey (HINTS) were analyzed to assess respondents’ reported likelihood of developing cancer (risk) and perceptions of whether they could lower their chances of getting cancer (efficacy). Respondents with higher efficacy were more likely to report that good nutrition can prevent cancer and reported more preventive dietary changes compared to respondents with lower efficacy. Respondents with higher efficacy were more likely to report intentions to change their diets to prevent cancer and reported more preventive dietary changes to their own diets, but only at higher levels of risk. Results suggest that to improve cognitions about the role of nutrition in cancer prevention, interventions should target cancer prevention efficacy; however, to increase intentions to change nutrition behaviors, interventions should target efficacy and risk perceptions.
Keywords: Risk Perception Attitude Framework, Health Information National Trends Survey, cancer prevention
It has been estimated that approximately 35% of cancer deaths could be prevented through appropriate diet (Danaei et al., 2005). Accordingly, several public health programs emphasize the benefits of good nutrition to motivate people to improve their diets (e.g., 5-A-Day for Better Health; Stables et al., 2002). Past studies have shown that about 70% of people agree—when explicitly asked—that there is a link between nutrition and cancer (e.g., Harnack, Block, Subar, Lanes, & Brand, 1997). However, this approach likely overestimates the percentage of people who would spontaneously report that good nutrition can prevent cancer (Barnard & Nicholson, 1997). Data suggest that people who agree that nutrition is related to cancer have healthier diets (e.g., Harnack et al. 1997), while few people who do not meet recommended guidelines for fruit and vegetable intake report that good nutrition can prevent cancer (Cerully, Klein, & McCaul, 2006). Thus, strategies to change people’s nutrition-related cancer prevention cognitions could impact dietary behavior and ultimately decrease cancer rates. Psychological constructs associated with nutrition-related outcomes provide potential targets to inform health communication messages and interventions. A framework that allows researchers to identify people with varying nutrition-related cancer prevention cognitions and behavioral intentions is needed.
Two psychological constructs with good potential to determine how people think about nutrition-related cancer prevention are perceived risk, or the extent to which people believe they are vulnerable to a particular outcome (e.g., cancer), and perceived efficacy, or the extent to which people believe they are able to take action to avoid the outcome. These constructs have been used to explain cognitions and behaviors in a number of health behavior and health communication theories (e.g., protection motivation theory [Maddux & Rogers, 1983], extended parallel process model [EPPM; Witte & Allen, 2000]).
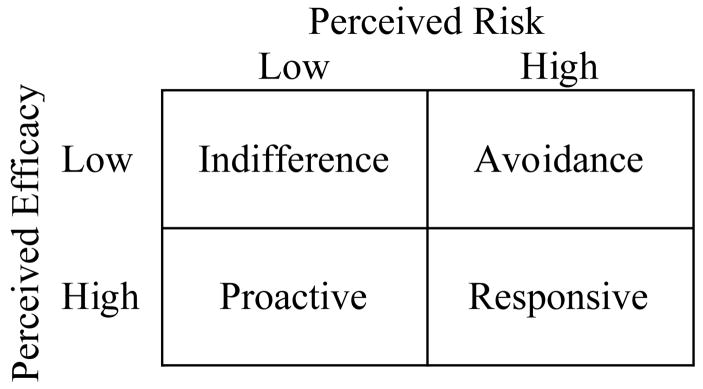
The Risk Perception Attitude (RPA) framework, based on the EPPM, was developed to explain how these constructs might be used to identify groups of people who could be targeted for health campaigns (Rimal, 2001; Rimal & Real, 2003). Whereas the EPPM addresses the effects of threat and efficacy contained in a message, the RPA framework focuses on the effects of the individual’s perceived risk and efficacy. The RPA framework identifies four separate groups based on differences in perceived risk and efficacy (Figure 1). People who do not see themselves as at risk for a negative health event and who do not believe the adverse outcome could be avoided are classified as indifference. Those who do not see themselves as at risk but do believe the outcome could be avoided are classified as proactive. Those who see themselves as at risk but do not believe the outcome could be avoided are classified as avoidance. Finally, those who see themselves as at risk and believe the outcome could be avoided are classified as responsive.
Figure 1.
Risk Perception Attitude Framework Categories.
The central hypotheses of the RPA framework are based on the expectation that perceived efficacy moderates the effect of risk perceptions on cognitions and behaviors. When people do not believe they are at risk, they are not motivated to act; therefore, whether they believe they can take action does not have any impact on their cognitions or behavior. When people believe they are at risk they are motivated to act, but they can only do so if they believe they can act (Rimal & Real, 2003). Thus, the RPA framework predicts that responsive individuals will be the most likely to adopt risk-reducing, health promoting cognitions and behaviors, followed by proactive, avoidance, and indifference individuals. Among individuals with low perceived risk, perceived efficacy is predicted not to have an impact (i.e., indifference and proactive individuals are hypothesized to exhibit similar cognitions and behaviors), whereas perceived efficacy is predicted to have an impact among individuals with high perceived risk. Specifically, responsive individuals are predicted to be more likely to adopt risk-reducing, health promoting cognitions and behaviors than are avoidance individuals.
A few studies have tested the predictions of the RPA framework. In one study, the effect of risk perceptions on the extent to which people thought about heart disease was moderated by perceived efficacy as predicted by the RPA framework, such that responsive individuals thought more about heart disease than did avoidance individuals but there was no difference seen between proactive and indifference individuals (Rimal, 2001). However, perceived efficacy did not moderate the effect of risk perceptions in the expected manner when the outcome was use of health information. Instead, responsive and proactive individuals did not differ, whereas avoidance individuals used health information more than did indifference individuals. Responsive and proactive individuals were the most likely to use health information, and indifference individuals were the least likely.
In studies of skin cancer-related information seeking, Rimal and Real (2003, Study 2) and Turner, Rimal, Morrison, and Kim (2006) found that, as predicted, responsive individuals had more skin cancer-related behavioral (e.g., wear sunscreen) and information seeking intentions than did avoidance individuals. In contrast to predictions about the moderating role of efficacy, proactive individuals had more behavioral and information seeking intentions than did indifference individuals. Again, responsive individuals had the most intentions and indifference individuals had the least. Turner and colleagues (2006) obtained similar results in a study on diabetes-related information seeking.
Finally, Rimal and Real (2003; Study 1) in an experimental manipulation of efficacy and risk perceptions regarding skin cancer-related information seeking observed that indifference individuals had the lowest motivation to prevent skin cancer, sought information the least, and had the least behavioral intentions to engage in skin cancer risk-reducing behaviors (e.g., wear sunscreen). However, avoidance individuals tended to have the most motivation, information seeking, and behavioral intentions. Avoidance and responsive individuals did not differ, nor did indifference and proactive individuals. The authors posit that these conflicting results may have been due to the experimental nature of the study; their manipulation may not have successfully induced low efficacy.
Although there is mixed support for the specific hypotheses regarding the moderating effect of efficacy on risk perceptions, this body of research suggests that classifying individuals by their risk perceptions and efficacy beliefs may be a useful tool for determining the likelihood that individuals think about health-related topics, seek information, and change their health behaviors. Previous studies (Rimal, 2001; Rimal & Real, 2003; Turner et al., 2006) have tested the RPA framework in cross-sectional, longitudinal, and experimental designs. This study furthers research on the RPA framework by testing predictions in a nationally representative sample with a focus on nutrition-related outcomes.
Current Study
We examined whether the RPA framework is predictive of two health-related outcomes related to the role of nutrition in cancer prevention: health cognitions and behavioral intentions. This may inform efforts to identify groups of people who will benefit from different messages and interventions concerning nutrition-related cancer prevention.
We first examined whether the characteristics described by the RPA framework were associated with nutrition-related cancer prevention cognitions. Consistent with theory hypotheses, we expected that among individuals with low perceived cancer risk, perceived cancer prevention efficacy would not have an impact, such that indifference and proactive individuals would not differ in their likelihood of reporting that good nutrition can prevent cancer or the number of nutritional changes they reported people should make to prevent cancer. However, among individuals with high perceived cancer risk, perceived cancer prevention efficacy would have an impact, such that responsive individuals would be more likely than avoidance individuals to report that good nutrition can prevent cancer and would list more nutritional changes people should make to prevent cancer than avoidance individuals.
Second, we examined whether the characteristics described by the RPA framework were associated with nutrition-related cancer prevention behavioral intentions. We expected to find the same pattern of results described above when the outcomes were reported intentions to make nutritional changes to prevent cancer and the number of nutritional changes respondents reported they should make to prevent cancer.
Methods
Data Source
The Health Information National Trends Survey (HINTS; Hesse, Moser, Finney Rutten, & Kreps, 2006; Nelson et al., 2004) is a national probability survey of the U.S. adult population conducted by the NCI every two years. The survey assesses the public’s cancer-related knowledge, cognitions, and behaviors. We used data from HINTS 2003, which was administered from October 2002 through April 2003 (http://hints.cancer.gov). Respondents (n = 6,369) were selected using random-digit dialing and completed a one-time telephone interview administered by trained interviewers. A cross-sectional, complex sample survey design was implemented, with oversampling of African Americans and Hispanics. One adult aged 18 or older within each household was selected for the extended interview during a household screener. The final response rate for the household screener was 55%, and the final response rate for extended interview was 62.8%. Further details about the sample and sampling design have been published (Nelson et al., 2004; http://hints.cancer.gov).
Measures
The criteria for inclusion of measures on HINTS were scientific validity criteria, utility criteria, and implementation criteria (see Nelson et al., 2004 for full details). Concurrent protocol analysis techniques were used to evaluate the measures in a cognitive laboratory (Willis, 2005). Scenarios were developed for the instrument as a whole, with prompts and probes built into the scenarios. Cognitive laboratory interviewers took nine participants through one of each of three iterations (27 participants in total). Sessions were audio recorded and problem areas were noted from analysis of the tapes. The cognitive laboratory results aided in the evaluation of such issues as face validity and appropriate wording. If questions could not be altered sufficiently to improve comprehension they were dropped according to the implementation criteria.
RPA Categories
Perceived cancer risk was measured by asking respondents “How likely do you think it is that you will develop cancer in the future?” Respondents rated their chance of getting cancer on a scale ranging from 1 (Very Low) to 4 (Very High). Twenty percent reported very low cancer risk, 26% reported somewhat low cancer risk, 37% reported somewhat moderate cancer risk, 12% reported somewhat high cancer risk, and 5% reported very high cancer risk. Respondents who reported moderate, high, or very high cancer risk were above the median. Perceived cancer prevention efficacy was measured by providing respondents with the statement “There’s not much people can do to lower their chances of getting cancer.” Respondents rated their agreement on a scale ranging from 1 (Strongly Agree) to 4 (Strongly Disagree). Seven percent strongly agreed, 23% somewhat agreed, 35% somewhat disagreed, and 36% strongly disagreed. Respondents who strongly disagreed were above the median. Responses to these items were used to create the four RPA groups: respondents with scores below the median on both the perceived cancer prevention efficacy and perceived cancer risk items were classified as indifference, respondents with scores below the median on perceived cancer prevention efficacy and above the median on perceived cancer risk were classified as avoidance, respondents with scores above the median on perceived cancer prevention efficacy and below the median on perceived cancer risk were classified as proactive, and respondents with scores above the median on both items were classified as responsive (Figure 1).
Nutrition-Related Cancer Prevention Cognitions
Respondents were asked the following question “Can you think of anything people can do to reduce their chances of getting cancer?” Nearly 16% answered “no/nothing” to this question and 46% did not give a nutrition-related response. Respondents were classified according to whether they gave at least one nutrition-related response (e.g., “eat better;” n = 3443) or not (n = 2922) to create a dichotomous measure of nutrition-related cancer prevention cognition. All respondents who gave a nutrition-related response were then asked “What specific changes should people make in their eating habits to reduce their chances of getting cancer?” (e.g., “eat more fruits”). Following Cerully et al. (2006), the number of responses to this item was summed to create an index, ranging from 0 (those who did not give a nutrition related response and those who did not report any specific changes) to 8 (the most responses reported), with higher scores indicating more attitudinal agreement with the role of nutrition in cancer.
Nutrition-Related Behavioral Intentions
Respondents were asked the following question “Is there anything about your behavior or lifestyle that you would like to change to reduce your chances of getting cancer?” Fifty-four percent answered “no/nothing” to this question and 80% did not give a nutrition-related response. Respondents were classified according to whether they gave at least one nutrition-related response (n = 1296) or not (n = 5063) to create a dichotomous measure. All respondents who gave a nutrition-related response were then asked “What specific changes should you make in your eating habits to reduce your chances of getting cancer?” The number of responses to this item was summed to create an index, ranging from 0 (those who did not give a nutrition related response and those who did not report any specific changes) to 7 (the most responses reported), with higher scores indicating more behavioral intentions.
Demographic and Health Characteristics
Respondents reported their age, gender, race/ethnicity, income, and education. Respondents also reported participation in physical activity or exercise during the past month. They reported separately how often they ate fruit, fruit juice, vegetables, and potatoes during the past month. Responses to these four questions were summed and reported as servings per day. Respondents reported their height and weight, which was used to calculate body mass index (BMI=(703×[Weight in Pounds/(Height in inches × Height in inches)]). We categorized BMI as underweight (less than 18.5 kg/m2), normal (18.5 and 24.9 kg/m2), overweight (25–29.9 kg/m2), and obese (over 30 kg/m2).
Analyses
To account for the complex sample survey design, all statistical analyses were conducted using SUDAAN (Research Triangle Institute, 2004) and utilized weighting and jackknife variance estimation. The final weights used in these analyses included calibrations against comparable population data for age, gender, race, and education publicly available from the Current Population Survey. Bivariate analyses and multiple logistic and linear regression analyses were conducted to determine whether demographic and health characteristics differed across RPA groups and whether they were related to study outcomes (nutrition-related cognitions and behavioral intentions).
Logistic and linear regressions with planned contrasts were conducted to determine whether the dichotomous or continuous indicators of nutrition-related cognitions and behavioral intentions differed as predicted between the RPA groups after adjustment for respondents’ demographic and health characteristics. Satterthwaite χ2 values are presented to indicate the statistical significance of RPA group differences on dichotomous and continuous study outcomes. Bonferroni correction adjusted for multiple comparisons; significance was defined as p <.008. Demographic characteristics (i.e., age, gender, race/ethnicity, and education) and health characteristics related to nutrition and energy balance (i.e., exercise, fruit and vegetable intake, and BMI) were included in these models as covariates. Because of multicollinearity with education, income was not included.
Results
Demographic and Health Characteristics
Table 1 summarizes demographic and health characteristics by each RPA group. The RPA groups did not differ by age or gender. Respondents with high perceived cancer prevention efficacy (i.e., proactive and responsive individuals) tended to have higher education, higher income, higher fruit and vegetable consumption, and were more likely to exercise than were respondents with low perceived cancer prevention efficacy (i.e., indifference and avoidance individuals). Responsive individuals were more likely to be White than were all other respondents. Finally, avoidance individuals tended to have higher BMIs and proactive individuals tended to have lower BMIs than all other respondents. In a multivariate analysis, all effects remained the same except that age became significant, such that responsive individuals were younger than all other respondents (p <.03).
Table 1.
Predicted Marginals (95% Confidence Interval) for Demographic and Health Characteristics, by Risk Perception Attitude Framework Categories.
| RPA Categories
|
|||||
|---|---|---|---|---|---|
| Respondent Characteristics | Indifference | Proactive | Avoidance | Responsive | p-value |
| Sample N (Weighted %) | 1355 (28) | 868 (17) | 1737 (36) | 872 (18) | -- |
| Age | 43.15 (42.03–44.27) | 43.12 (41.54–44.70) | 42.78 (42.04–43.52) | 41.55 (40.61–42.49) | .27 |
| Gender (% Female) | 49 (45–53) | 46 (42–50) | 51 (47–55) | 51 (47–55) | .35 |
| Education | <.001 | ||||
| ≤ High School | 48 (44–52) | 35 (31–39) | 50 (48–52) | 38 (34–42) | |
| Some College | 26 (24–28) | 31 (27–35) | 27 (25–29) | 35 (31–39) | |
| ≥ College | 26 (24–28) | 34 (30–38) | 23 (21–25) | 28 (26–30) | |
| Income | <.001 | ||||
| <$25,000 | 28 (26–30) | 20 (16–24) | 27 (25–29) | 20 (16–24) | |
| $25,000–$50,000 | 31 (27–35) | 28 (24–32) | 31 (29–33) | 32 (28–36) | |
| >$50,000 | 41 (37–45) | 52 (48–56) | 42 (38–46) | 47 (43–51) | |
| Race/Ethnicity | .002 | ||||
| White, Non- Hispanic | 69 (65–73) | 72 (68–76) | 75 (73–77) | 80 (76–84) | |
| Black, Non- Hispanic | 11 (9–13) | 11 (9–13) | 9 (7–11) | 7 (5–9) | |
| Hispanic | 14 (12–16) | 11 (9–13) | 10 (8–12) | 7 (5–9) | |
| Other | 7 (5–9) | 6 (4–8) | 6 (4–8) | 6 (4–8) | |
| Body Mass Index | <.001 | ||||
| Underweight (< 18.5) | 2 (0–4) | 2 (0–4) | 2 (0–4) | 2 (0–4) | |
| Normal (18.5–24) | 38 (34–42) | 46 (42–50) | 34 (30–38) | 39 (35–43) | |
| Overweight (25–29) | 40 (36––44) | 34 (30–38) | 35 (33–37) | 35 (31–39) | |
| Obese (30+) | 20 (16–24) | 18 (14–22) | 28 (24–32) | 23 (19–27) | |
| Exercise (% Any) | 74 (70–78) | 82 (78–86) | 68 (66–70) | 78 (74–82) | <.001 |
| Fruit & Vegetable | 2.95 | 3.38 | 2.85 | 3.16 | <.001 |
| Intake (Mean) | (2.81–3.09) | (3.22–3.54) | (2.75–2.95) | (3.00–3.32) | |
Note. P-values are Satterthwaite adjusted.
Table 2 displays the bivariate relations between demographic and health characteristics and nutrition-relation cancer prevention cognitions and behavioral intentions. Overall, 51% of respondents stated that cancer can be prevented through good nutrition, and 19% indicated that they would like to change their eating habits to prevent cancer. Women, compared to men, were more likely to report that good nutrition can prevent cancer and listed more nutritional changes people should make to prevent cancer. Women were also more likely to report intentions to make nutritional changes to prevent cancer, and listed more nutritional changes they should make to prevent cancer. Higher education, higher income, being middle-aged, and being white were positively associated with cognitions (i.e., higher likelihood of reporting that good nutrition can prevent cancer and listing more nutritional changes people should make to prevent cancer) and behavioral intentions (i.e., higher likelihood of reporting intentions to make nutritional changes to prevent cancer and listing more nutritional changes they should make to prevent cancer). Obese respondents were the most likely to report intentions to make nutritional changes to prevent cancer and listed the most nutritional changes they should make to prevent cancer, but they listed fewer nutritional changes people should make to prevent cancer than did normal weight respondents. Respondents who reported exercising, compared to those who did not, were more likely to report that good nutrition can prevent cancer and listed more nutritional changes people should make to prevent cancer; however, they did not differ on either of the behavioral intention measures. Finally, eating more fruits and vegetables was associated with higher likelihood of reporting that good nutrition can prevent cancer and listing more nutritional changes people should make to prevent cancer, but lower likelihood of reporting intentions to make nutritional changes to prevent cancer and listing fewer nutritional changes they should make to prevent cancer.
Table 2.
Predicted Marginals (95% Confidence Interval) for Nutrition-Related Cognitions and Behavioral Intentions, by Demographic and Health Characteristics.
| Cognitions
|
Behavioral Intentions
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Respondent Characteristics | % Reported Nutrition | p- value | N of Nutrition Changes Listed | p- value | % Reported Nutrition | p- value | N of Nutrition Changes Listed | p- value |
| Sample N | 6365 | -- | 6365 | -- | 6359 | -- | 6359 | -- |
| Total | 51 (49–53) | -- | 1.15 (1.11–1.19) | -- | 19 (17–21) | -- | 0.39 (0.37–0.41) | -- |
| Age | <.001 | <.001 | .03 | .10 | ||||
| 18–34 | 39 (34–43) | 2.01 (1.87–2.15) | 16 (14–18) | 2.02 (1.88–2.16) | ||||
| 35–64 | 60 (58–62) | 2.34 (2.28–2.40) | 24 (22–26) | 2.08 (2.00–2.16) | ||||
| 65+ | 45 (41–49) | 2.25 (2.09–2.41) | 10 (8–12) | 2.02 (1.78–2.26) | ||||
| Gender | <.001 | <.001 | <.001 | <.001 | ||||
| Female | 55 (53–57) | 1.33 (1.27–1.39) | 21 (19–23) | 0.45 (0.41–0.49) | ||||
| Male | 48 (46–52) | 0.96 (0.90–1.02) | 16 (14–18) | 0.33 (0.29–0.37) | ||||
| Education | <.001 | <.001 | <.001 | <.001 | ||||
| ≤ High School | 40 (38–42) | 0.83 (0.77–0.89) | 16 (14–18) | 0.31 (0.27–0.35) | ||||
| Some College | 58 (54–62) | 1.30 (1.22–1.38) | 21 (19–23) | 0.45 (0.39–0.51) | ||||
| ≥ College | 69 (67–69) | 1.72 (1.64–1.80) | 25 (23–27) | 0.50 (0.46–0.54) | ||||
| Income | <.001 | <.001 | <.001 | <.001 | ||||
| <$25,000 | 36 (34–38) | 0.76 (0.68–0.84) | 14 (12–16) | 0.27 (0.23–0.31) | ||||
| $25,000–$50,000 | 51 (47–55) | 1.08 (1.00–1.16) | 20 (18–22) | 0.41 (0.35–0.47) | ||||
| >$50,000 | 65 (63–67) | 1.54 (1.461.62) | 23 (21–25) | 0.48 (0.44–0.52) | ||||
| Race/Ethnicity | <.001 | <.001 | .04 | .02 | ||||
| White, Non-Hispanic | 57 (55–59) | 1.30 (1.24–1.36) | 20 (18–22) | 0.42 (0.38–0.46) | ||||
| Black, Non-Hispanic | 45 (41–49) | 0.95 (0.81–1.09) | 19 (15–23) | 0.37 (0.29–0.45) | ||||
| Hispanic | 27 (23–31) | 0.59 (0.51–0.67) | 14 (10–18) | 0.27 (0.21–0.33) | ||||
| Other | 49 (45–53) | 1.06 (0.88–1.24) | 19 (13–25) | 0.42 (0.26–0.58) | ||||
| Body Mass Index | .21 | .003 | <.001 | <.001 | ||||
| Underweight (< 18.5) | 48 (36–60) | 0.97 (0.73–1.21) | 10 (4–16) | 0.21 (0.05–0.37) | ||||
| Normal (18.5–24) | 53 (51–55) | 1.26 (1.18–1.34) | 17 (15–19) | 0.34 (0.30–0.38) | ||||
| Overweight (25–29) | 54 (52–56) | 1.19 (1.11–1.27) | 19 (17–21) | 0.40 (0.36–0.44) | ||||
| Obese (30+) | 49 (45–53) | 1.06 (0.96–1.16) | 24 (22–26) | 0.51 (0.45–0.57) | ||||
| Exercise | <.001 | <.001 | .13 | .22 | ||||
| None | 42 (40–44) | 0.89 (0.83–0.95) | 18 (16–20) | 0.37 (0.31–0.43) | ||||
| Any | 55 (53–57) | 1.27 (1.21–1.33) | 20 (18–22) | 0.41 (0.37–0.45) | ||||
| Fruit & Vegetable Intake | <.001 | <.001 | .003 | .003 | ||||
| < 2 servings | 44 (40–48) | 0.88 (0.80–0.96) | 20 (18–22) | 43 (39–47) | ||||
| 2–4 servings | 54 (52–56) | 1.21 (1.15–1.27) | 20 (18–22) | 40 (36–44) | ||||
| ≥ 5 Servings | 60 (56–64) | 1.61 (1.47–1.75) | 15 (11–19) | 32 (26–38) | ||||
Note. P-values are Satterthwaite adjusted. Age and fruit and vegetable intake were modeled continuously; however, they are presented here as categorical variables for descriptive purposes.
In multivariate analyses, age and race/ethnicity were no longer associated with behavioral intentions, and BMI was no longer associated with listing nutritional changes people should make to prevent cancer (ps >.05). All other effects remained the same.
Cognitions
The RPA framework hypotheses were partially supported (Table 3). As predicted, responsive individuals were significantly more likely than avoidance individuals to report that good nutrition can prevent cancer, χ2 (1) = 19.96, p <.0001, and listed significantly more nutritional changes people should make to prevent cancer than did avoidance individuals, χ2 (1) = 28.54, p <.0001. Contrary to predictions, proactive individuals were significantly more likely than indifference individuals to report that good nutrition can prevent cancer, χ2 (1) = 21.90, p <.0001, and listed significantly more nutritional changes people should make to prevent cancer than did indifference individuals, χ2 (1) = 27.93, p <.0001. Further, no significant differences were observed between respondents at the same level of perceived cancer prevention efficacy but varying levels of perceived cancer risk (i.e., indifference vs. avoidance individuals, proactive vs. responsive individuals, ps >.10). This pattern of results suggests that perceived cancer prevention efficacy, but not perceived cancer risk, is important in determining nutrition-related cancer prevention cognitions.
Table 3.
Predicted Marginals (95% Confident Intervals) for Cognitions and Behavioral Intentions, by Risk Perception Attitude Framework Categories.
| Cognition | Behavioral Intentions | |||
|---|---|---|---|---|
| Predictors | % Reported Nutrition | N of Nutrition Changes Listed | % Reported Nutrition | N of Nutrition Changes Listed |
| RPA Categories | ||||
| Indifference | 47 a (43–51) | 1.00 a (0.90–1.10) | 16 a (14–18) | 0.34a (0.28–0.40) |
| Proactive | 64 b (60–68) | 1.59 b (1.45–1.73) | 22 a, b (18–26) | 0.40 a, b (0.32–0.48) |
| Avoidance | 49 a (45–53) | 1.04 a (0.96–1.12) | 20 a (18–22) | 0.41 a (0.37–0.45) |
| Responsive | 65 b (61–69) | 1.59 b (1.45–1.73) | 26 b (22–30) | 0.61 b (0.51–0.71) |
| Total | 54 (52–56) | 1.22 (1.16–1.28) | 21 (20–22) | 0.42 (0.38–0.46) |
Note. Means in the same column sharing the same superscript were not different at Satterthwaite adjusted p <.008.
Behavioral Intentions
The RPA framework hypotheses were supported (Table 3). As predicted, responsive individuals were significantly more likely than avoidance individuals to report intentions to make nutritional changes to prevent cancer, χ2 (1) = 7.40, p =.007, and listed significantly more nutritional changes they should make to prevent cancer than did avoidance individuals, χ2 (1) = 8.47, p =.004. As predicted, proactive and indifference individuals did not differ in behavioral intentions, ps >.01. Further, no significant differences were observed between respondents at the same level of perceived cancer prevention efficacy but varying levels of perceived cancer risk (i.e., indifference vs. avoidance individuals, proactive vs. responsive individuals, ps >.01). These results suggest that, for behavioral intentions, perceived cancer prevention efficacy moderates the effect of cancer risk perceptions, such that at low levels of perceived cancer risk, perceived cancer prevention efficacy does not have an impact, but at high levels of perceived cancer risk, perceived cancer prevention efficacy increases behavioral intentions.
Discussion
This study replicated and extended prior RPA research through testing the RPA framework in the context of cognitions and behavioral intentions related to nutrition and cancer prevention using a nationally representative sample. In our analyses of nutrition-related cancer prevention cognitions, we did not find support for the hypothesis derived from RPA that perceived efficacy moderates the impact of risk perceptions; rather, consistent with previous studies (e.g., Rimal & Real, 2003, Turner et al., 2006), we observed a main effect for perceived cancer prevention efficacy, such that responsive and proactive individuals reported more positive nutrition-related cognitions than avoidance and indifference individuals, respectively. However, RPA hypotheses were fully supported in our analyses of behavioral intentions. For individuals at high levels of perceived cancer risk, those with high perceived cancer prevention efficacy (responsive) reported more nutrition-related behavioral intentions than did those with low perceived cancer prevention efficacy (avoidance), whereas individuals at low levels of perceived cancer risk (proactive and indifference) reported the same levels of behavioral intentions, regardless of perceived cancer prevention efficacy.
Overall, approximately half of respondents endorsed positive nutrition-related cancer prevention cognitions by stating that cancer can be prevented through good nutrition, and approximately 20% endorsed positive nutrition-related cancer prevention behavioral intentions by indicating that they would like to change their eating habits to prevent cancer. Two methodological points are worth noting: first, the percentage of respondents who spontaneously named nutrition as a cancer prevention strategy was lower than in studies with closed-ended measures, suggesting that many people do not automatically think of nutrition as a cancer prevention strategy. Second, as has been noted elsewhere (Cerully et al., 2006), respondents were more likely to report that others should change their eating habits to prevent cancer than they were to report that they should change their own eating habits. Respondents listed more specific changes that other people should make to prevent cancer, compared to the number of specific changes they should make to prevent cancer. These findings highlight the continued need for communication campaigns that convey the importance of nutrition as a cancer prevention strategy, and illustrate the importance of not just promoting positive cognitions about the link between nutrition and cancer prevention but also motivating the public to make appropriate dietary changes.
Results suggest that those who already eat plenty of fruits and vegetables are more likely to report that good nutrition can prevent cancer but are less likely to report intentions to make nutritional changes. Because these individuals are already eating healthily, it does not seem worrisome that they report fewer intentions to change. However, it should be noted that few respondents were currently meeting guidelines for fruit and vegetable consumption (i.e., 85% reported eating less than five servings a day). Thus there is still a substantial proportion of people who need more health education in this area.
Limitations and Future Directions
Though the current study extends previous research by testing RPA in the context of nutrition-related cancer prevention using nationally representative data, there are several limitations to be addressed. For example, in using pre-existing data to test theory, we did not have multiple measures of our key constructs, perceived cancer risk and perceived cancer prevention efficacy. Ideally, we would want to measure not just perceptions of susceptibility to cancer, but also perceived severity of cancer (how serious the harm is expected to be; Witte, 1992). Recent work suggests that the connection between risk perceptions and behavioral outcomes can be increased if feelings about risk, rather than probability judgments, are measured (Weinstein et al., 2007).
Our measure of perceived cancer prevention efficacy was framed in a negative manner, such that respondents were asked to report the extent to which they agreed with the statement, “there’s not much people can do to lower their chances of getting cancer;” this framing may have influenced the way people responded. It is important to note that our “high perceived cancer prevention efficacy” responders were those who strongly disagreed with this statement, as the median was high for this measure. In addition, respondents may have interpreted this measure as either self efficacy (I have the ability to prevent cancer) or response efficacy (methods to prevent cancer can succeed; Witte, 1992). Past tests of the RPA framework have measured either self efficacy alone (Rimal, 2000) or have combined self and response efficacy in one measure (e.g., Rimal & Real, 2003). Future studies should determine whether one—or the combination—of these types of efficacy plays a greater role in the RPA framework. Specifying the type of efficacy needed to increase nutrition-related cancer prevention cognitions and behaviors would aid in the creation of efficacious communication messages and interventions.
There are also limitations to our operationalization of study outcomes. We defined cognitions as reporting that good nutrition can prevent cancer. Because the causal link between nutrition and cancer prevention is an ongoing area of epidemiological research (e.g., Asano & McLeod, 2002), we believe endorsing nutrition as a cancer prevention strategy is best characterized as a cognition, rather than knowledge. HINTS does not directly assess behavioral intentions with questions commonly used in the literature (e.g., degree of agreement with the statement I intend to do [behavior]) and does not assess the strength of intentions; however, by asking respondents whether they had any behaviors they would like to change and specifically which behaviors they should change, we believe that HINTS adequately captures the likelihood of a respondents performing nutrition-related cancer prevention behaviors. A recent meta-analysis of randomized control trials found support for a moderate link between behavioral intentions and behaviors (Webb & Sheeran, 2006); however, there has been criticism of measuring behavioral intentions rather than measuring actual behavior in theory testing (Weinstein, 2007). Although our findings lend support to RPA as a theoretical framework to study nutrition-related behavioral intentions, further research is needed to determine whether the theory is useful in predicting dietary behavior.
In using cross-sectional data, our findings are not causal and therefore cannot tell us whether risk and efficacy perceptions are driving these effects, or whether having strong nutrition-related cancer prevention cognitions and behavioral intentions affect perceived cancer prevention efficacy and perceived cancer risk. Finally, the overall response rate for HINTS 2003, although comparable to other national telephone surveys, reflects a decline in response rates (Nelson, Powell-Griner, Town, & Kovar, 2003).
Implications for Practice
The observed pattern of results in this study; namely, that the RPA moderation hypothesis was supported in analyses of nutrition-related behavioral intentions but not for nutrition-related cognitions, has implications for both the RPA framework and for clinical practice. It may be that perceived efficacy alone can increase the likelihood of adopting positive prevention-related cognitions, whereas both perceived efficacy and perceived risk are necessary to motivate people to actually perform and sustain preventative behaviors. The RPA framework posits that perceived risk is a motivating force; thus, for easier tasks (such as reporting the good nutrition can prevent cancer) the motivation that stems from increased perceived risk may be not be needed. In contrast, for more difficult tasks (such as changing one’s own behavior) people may need to feel that they are at risk before being sufficiently motivated. We found that perceived cancer prevention efficacy plays a more consistent role than perceived cancer risk in the context of nutrition-related prevention cognitions and behaviors, suggesting that a special emphasis be placed on the promotion of perceived cancer prevention efficacy as an intervention strategy. Indeed, printed health information tailored to individual’s levels of perceived efficacy has been shown to be more effective than non-tailored information (Noar, Benac, & Harris, 2007). Thus, practices may consider offering multiple versions of nutrition-related information tailored to patients’ levels of perceived cancer prevention efficacy. Though there is a solid evidence base for the protective role of good nutrition in reducing cancer risk (Danaei et al., 2005), further research should specify the circumstances under which both perceived efficacy and perceived risk effect change as well as whether and how perceived efficacy and perceived risk can be simultaneously affected by interventions to promote health behavior.
Conclusions
This study provides nationally representative data to complement past experimental and smaller-scale studies of the RPA framework (Rimal & Real, 2003; Turner et al., 2006). These results can aid in targeting communication efforts toward people who are less likely to believe that good nutrition can prevent cancer and who have fewer intentions to eat better to prevent cancer. For instance, these findings suggest that to improve cognitions about the role of nutrition in cancer prevention, interventions should target people with low perceived cancer prevention efficacy beliefs; to increase intentions to change nutrition behaviors, interventions should target people with low perceived cancer prevention efficacy and people with low perceived cancer risk. Further, given the variety of behaviors linked to cancer incidence (Danaei et al., 2005), results of this study point to the RPA framework as a useful theoretical framework for the continued study of behavior change related to cancer prevention.
References
- Asano TK, McLeod RS. Dietary fibre for the prevention of colorectal adenomas and carcinomas. Chochrane Database of Systematic Reviews. 2002;(1) doi: 10.1002/14651858.CD003430. [DOI] [PubMed] [Google Scholar]
- Barnard ND, Nicholson AN. Beliefs about dietary factors in breast cancer prevention among American women, 1991 to 1995. Preventive Medicine. 1997;26:109–113. doi: 10.1006/pmed.1996.9987. [DOI] [PubMed] [Google Scholar]
- Cerully JL, Klein WMP, McCaul KD. Lack of acknowledgment of fruit and vegetable recommendations among nonadherent individuals: Associations with information processing and cancer cognitions. Journal of Health Communication. 2006;11:103–115. doi: 10.1080/10810730600637491. [DOI] [PubMed] [Google Scholar]
- Danaei G, Vander Hoorn S, Lopez AD, Murray CJL, Ezzatik M the Comparative Risk Assessment collaborating group (Cancers) Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. The Lancet. 2005;366:1784–1793. doi: 10.1016/S0140-6736(05)67725-2. [DOI] [PubMed] [Google Scholar]
- Harnack L, Block G, Subar A, Lanes S, Brand R. Association of cancer prevention-related nutrition knowledge, beliefs, and attitudes to cancer prevention dietary behavior. J Am Diet Assoc. 1997;97:957–965. doi: 10.1016/S0002-8223(97)00231-9. [DOI] [PubMed] [Google Scholar]
- Hesse BW, Moser RP, Finney Rutten LJ, Kreps GL. The Health Information National Trends Survey: Research From the Baseline. Journal of Health Communication. 2006;11:vii–xvi. doi: 10.1080/10810730600692553. [DOI] [PubMed] [Google Scholar]
- Maddux JE, Rogers RW. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. Journal of Experimental Social Psychology. 1983;19:469–479. [Google Scholar]
- Nelson DE, Kreps GL, Hesse BW, Croyle RT, Willis G, Aurora NK, Rimer BK, Viswanath KV, Weinstein N, Alden S. The Health Information National Trends Survey (HINTS): Development, design, and dissemination. Journal of Health Communication. 2004;9:443–460. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- Nelson DE, Powell-Griner E, Town M, Kovar MG. A comparison of national estimates from the National Health Interview Survey and the Behavioral Risk Factor Surveillance System. Am J Public Health. 2003;93:1335–41. doi: 10.2105/ajph.93.8.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavioral change interventions. Psychological Bulletin. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Rimal RN. Perceived risk and self-efficacy as motivators: Understanding individuals’ long-term use of health information. Journal of Communication. 2001;51:633–651. [Google Scholar]
- Rimal RN, Real K. Perceived risk and efficacy beliefs as motivators of change: Use of the risk perception attitude (RPA) framework to understand health behaviors. Human Communication Research. 2003;29:370–399. [Google Scholar]
- Stables GJ, Subar AF, Patterson BH, et al. Changes in vegetable and fruit consumption and awareness among US adults: results of the 1991 and 1997 5 – A – Day for Better Health surveys. J Am Diet Assoc. 2002;102:809–817. doi: 10.1016/s0002-8223(02)90181-1. [DOI] [PubMed] [Google Scholar]
- Turner MM, Rimal RN, Morrison D, Kim H. The role of anxiety in seeking and retaining risk information: Testing the risk perception attitude framework in two studies. Human Communication Research. 2006;32:130–156. [Google Scholar]
- Weinstein ND. Misleading tests of health behavior theories. Annals of Behavioral Medicine. 2007;33:1–10. doi: 10.1207/s15324796abm3301_1. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, Gibbons FX. Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychology. 2007;26:146–151. doi: 10.1037/0278-6133.26.2.146. [DOI] [PubMed] [Google Scholar]
- Willis GB. Cognitive interviewing: A tool for improving questionnaire design. Thousand Oaks, Calif.: Sage Publications; 2005. [Google Scholar]
- Witte K. Putting the fear back in fear appeals: The extended parallel process model. Communication Monographs. 1992;59:329–349. [Google Scholar]
- Witte K, Allen M. A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education and Behavior. 2000;27:591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]