Abstract
Prior research has questioned the effectiveness of existing methods to identify individuals at high risk for contracting and transmitting the Human Immunodeficiency Virus (HIV) and other sexually transmitted diseases (STDs). Thus, new approaches are needed to provide these individuals with risk-reduction strategies. We review our research on young adults’ sexual decision making, using theories and methods from social and cognitive sciences. Four patterns of condom use and associated levels of risks and beliefs were identified. These patterns suggest value in targeting intervention strategies to individuals at different levels of risk. Findings also imply that the monogamous population may be at higher risk for infection than they realize. Primary-care physicians are the first line of contact for many individuals in the health care system, and may be in the best position to screen for at-risk individuals. Given time demands and other barriers, easy-to-use evidence-based guidelines for such screening are needed. We propose such guidelines for primary-care physicians to use in identifying an individual’s risk, from which custom-tailored intervention strategies can be developed.
Keywords: youth, HIV/AIDS, decision-making, patterns of reasoning, risky sexual behavior, screening, education
Introduction
The spread of the Human Immunodeficiency Virus (HIV) among young people in the United States is of great concern. Between 2001 and 2004, newly reported HIV cases increased for 15–24 year olds,1 and females accounted for 38% of new HIV infections among 13–24 year olds, with the majority of cases being attributed to heterosexual transmission.2 Unprotected sexual intercourse is a predominant method of HIV acquisition among heterosexual individuals. Effective prevention initiatives targeted at individuals engaging in risky sexual behavior are a necessary element in any solution aimed at reducing HIV spread and prevalence.
Decision-making researchers have studied the conditions under which individuals make faulty choices. Most of this work is based on classical decision theory, which focuses on how and why decisions deviate from optimality.3 Classical theories of rationality emphasize the match between actions and beliefs or desires, but do not take into account their nature.4, 5 Thus, if an action follows logically from one’s beliefs and desires, it is considered rational, even though the decision is risky and may lead to a negative outcome. We believe, however, that an individual is also influenced by various situational constraints, which needs to be taken into account for a comprehensive perspective on rationality.6
Questions have been raised regarding effective ways to identify individuals at risk for contracting and transmitting HIV, and providing them with risk-reduction strategies. People do not always do what is best for them, even when they have all of the necessary information to make the best decision.7 Research on risky decision-making by young people can contribute to strategies for decreasing risky behavior, yet the available evidence is rarely incorporated into public-health prevention initiatives. Primary-care physicians are the first line of contact for many individuals in the health care system, and are often in the best position to identify those individuals at risk for HIV. Furthermore, they may be the only health-care professionals to counsel such individuals about potential risk and to recommend HIV testing. Given the time demands on routine doctor visits, easy-to-use evidence-based guidelines for screening are urgently needed.
Background
HIV Risk Assessment and Prevention in Primary Care
The U.S. Public Health Service’s report, Healthy People 2010, has identified “responsible sexual behavior” as one of the leading health indicators as the majority of HIV-infected individuals under 25 are exposed through sexual behavior.8 The U.S. Preventive Services Task Force has outlined recommendations for HIV screening based on available evidence.9 We are unaware of research that relates such HIV screening recommendations to clinical outcomes, except for one study that used a simulation model to assess the performance of increasingly frequent HIV screening of all adults using rapid testing.10 Results indicated the effectiveness of routine, rapid HIV testing for individuals in all areas with a prevalence of undiagnosed HIV infection around 0.2%. These findings are supported by the Center for Disease Control’s (CDC) revised recommendations advocating routine voluntary HIV screening in health-care settings.11
Can clinical or demographic characteristics identify a subgroup of asymptomatic adolescents and adults at increased risk for HIV? Studies in high-risk settings have found that targeted screening based on more inclusive criteria could increase the number of HIV-positive individuals diagnosed, but it would still miss 7–13% of them and requires testing a much greater proportion of people.12 Additionally, Peterman13 found that 20–26% of HIV-infected people identified at federally-funded testing sites reported no known risk factors. Others have recommended lowering the threshold for a physician to recommend HIV testing to low-risk individuals.14 Gerbert et al15 developed and tested a self-administered HIV-risk survey to patients in the waiting room before the physician’s visit. The possibility that the completed screening information would be available to their physician did not lead to significant differences in reporting risky behaviors, and actually enhanced the participants’ desire that the physician view the survey results.
Barriers to physicians’ accurate assessment of patients’ risk include the patient’s unwillingness to disclose information, and differing perceptions of relationships and sexual behavior among patients and physicians.16 Time is another barrier as HIV is only one out of many issues/diseases for the physician to screen based on published guidelines.17 In addition, physicians are not always confident in their ability to assess risk or to counsel patients of low or uncertain risk. Risk assessment needs to incorporate both quantitative and qualitative (the patient’s beliefs and values) methods to facilitate communication.18 Vague guidelines merely serve to increase physician’s uncertainty, particularly when an individual’s risk level is ambiguous. Using clinical vignettes, one study found that physicians varied in their conceptualization of risk, used an “all or nothing” heuristic in advice about behavior change (e.g., use maximum protection regardless of level of risk), and gave incomplete statements to patients about their need for HIV testing.16 In another study, physicians recommended testing most frequently for high-risk individuals, but much less frequently for other sexually active adult patients, although they believed that these patients should be tested.19
This paper summarizes our research on young adults’ decision-making regarding sexual practices, aimed at developing evidence-based practice recommendations for physicians for HIV risk assessment.
Research on Risky Sexual Behavior and Risk Perception
In studies of risky sexual behavior, condom use has been extensively investigated in heterosexual youth.20 Personality variables, such as sensation seeking21, have also been associated with risky (sexual) behavior and risk perception of HIV and Acquired Immune Deficiency Syndrome (AIDS).22 In particular, men are more prone to sensation seeking and to display more risky behavior than women.22
Perceived risk of contracting HIV and other sexually transmitted diseases (STDs) has not been a consistently useful predictor of actual sexual behavior.23 Young adults can accurately interpret high-risk probabilities, but have difficulty with low-risk and negligible-risk probabilities.24, 25 In addition, individuals’ HIV risk perception is likely to be influenced by various heuristics and biases26, such as the affect heuristic27, relationship heuristics28, and the self-positivity bias, which reflects a tendency to be overly optimistic about one’s risk.29 There is also evidence for a reciprocal relationship between risky behavior and health beliefs.30
Failure to adopt health behaviors to prevent negative outcomes may be related to differences in how youths perceive risk that is not immediately and personally relevant. In one study, those reporting a prior experience with a specific event or risk behavior rated the likelihood of a negative outcome as lower than those with no prior experience with that behavior.31 Even after STD diagnosis, a sample of adolescent females reported no change in their number of unprotected sexual intercourse acts, attitudes toward condom use, or perceived susceptibility to STDs.32 Those who may have changed their behavior immediately after diagnosis had returned to the same level of risk behavior by the follow-up assessment.
In contrast to much of the research on sexual behavior, our framework is predominantly cognitively-oriented, based on theories and methods from cognitive science. As the work has evolved, we have incorporated socio-cultural, environmental, and emotional dimensions. The following section provides an overview of this framework.
Theoretical and Methodological Framework
Our framework emphasizes the reasoning process of how risks are perceived, understood and used to draw inferences based on a set of circumstances, leading to behavior.33–38 Such reasoning processes are closely associated but not perfectly correlated with decisions.35, 39, 40
Investigations of lay individuals’ health-related reasoning have found that they use opportunistic strategies (changing of rationale based on the situation) with a focus on their prior knowledge and beliefs, which are largely reflective of the socio-cultural context.41 The use of such strategies is even more prominent in adolescents’ reasoning, as they have less prior knowledge and construct their reality almost solely based on recent experiences.42 Youths are also more susceptible to the confirmation bias, where relevant information that conflicts with one’s hypothesis is discounted or ignored or the search for evidence is restricted to that which supports the hypothesis.43 Young adults’ reliance on these reasoning strategies could partially account for the relative ineffectiveness of past interventions to reduce risky sexual behavior in this population.
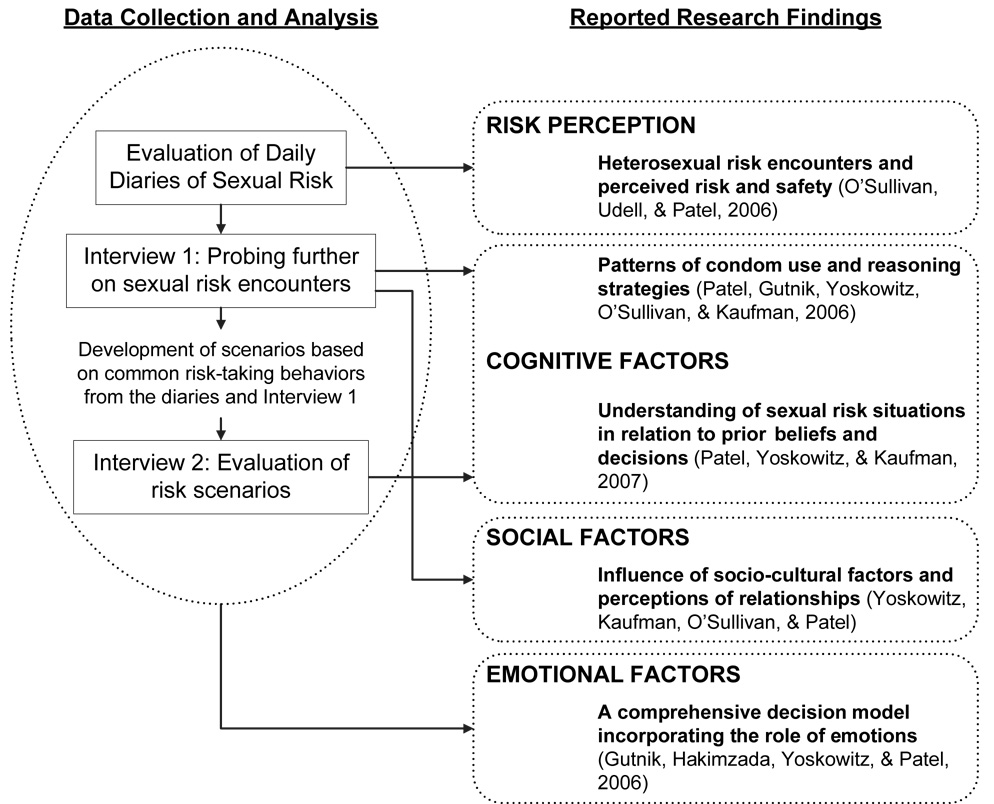
Cognitive decision research includes an in-depth analysis of how one’s knowledge is organized in the mind and how this knowledge guides decisions and behavior.35 Although cognition is central to our framework, decisions are also shaped in significant ways by the interaction of socio-cultural (e.g., group norms)44, environmental45, and emotional46 factors. An important facet of this approach is to document decisions close to the time in which they are actually made (i.e., daily diaries), as well as to supplement such data with interviews and questionnaires. Data analysis includes looking for themes and patterns that emerge across participants’ interviews, which is termed grounded theory,47 as well as looking for evidence of particular decision strategies,48 and developing visual (semantic) representations, or timelines, of the decision processes from the diary and interview data.36 The following sections present analyses, findings and implications from our research (see Figure 1).
Figure 1.
Overview of our research program, indicating data collection and analysis and reported results.
Capturing the Sexual Decision Making Process
We investigated sexual decision-making and behavior among 60 (30 females, 30 males) heterosexual urban college students (18–24 years), living in high HIV prevalence neighborhoods in Brooklyn, New York. Fifty percent of participants identified as African–American (n=30), 37% as White (n=22), 5% as Asian (n=3) and 8% as Other (n=5). Regarding ethnicity, 10% of participants identified themselves as Hispanic (n=6). The majority of participants (68%) reported a monthly income of less than $1,000. However, many lived with their parents and came from working-class and lower middle-class families.
Participants demonstrated moderately high HIV knowledge, as evidenced by their scores on a standard HIV knowledge measure.49 They completed daily diaries over two weeks, documenting participants’ actual sexual behavior, condom use, and risk perceptions of their sexual encounters, followed by a semi-structured interview to elaborate on the sexual encounters recorded in the diaries and their sexual history and relationships‥35, 45
Participants consistently rated their sexual encounters as low risk, regardless of the actual risk involved.50 Although most encounters consisted of unprotected sexual intercourse, participants continued to feel safe from HIV infection even when they were engaging in sexual activity with an unfamiliar partner. These results add to the growing evidence that young people fail to fully integrate their knowledge regarding HIV risk into their personal interactions.
Development of HIV Sexual Risk Patterns
Sexual behavior studies typically categorize participants into high-risk vs. low-risk, or condom-users vs. non-condom users. Findings from the initial diary analysis led us to look for patterns of condom use and associated reasoning strategies,36, 37 including the timeline of their decision processes as derived from the interview data.51
We characterized four patterns of condom use: consistent (35%), inconsistent (17%), shifting from consistent to inconsistent due to feelings of trust and comfort in one’s partner (35%), and shifting from inconsistent to consistent due to a significant negative event, such as an unwanted pregnancy or STD (13%). There were no significant differences in the gender, race, ethnicity, or socioeconomic characteristics of the participants categorized in each pattern of condom use.
Each pattern of condom use was associated with certain beliefs and behavioral tendencies. The consistent (low-risk) and inconsistent (high-risk) patterns were associated with the heuristic “use condoms all the time” and “use condoms when in doubt (e.g., lack of trust)”, respectively. In the other two patterns, the shift in behavior was due to a significant event and feelings of uncertainty causing a reevaluation of their behavior. We identified the following individuals as high-risk: (1) those shifting from consistent to inconsistent condom use and (2) those exhibiting inconsistent condom use.36, 37 Differences in rationale underlying these groups’ behavior indicate that different intervention strategies may be required: individuals in the former group use condoms when they are in a new and unfamiliar relationship, but terminate condom use once trust and feelings of comfort are established; whereas, individuals in the latter group rarely, if ever, use condoms.
Qualitative analysis48 allowed insight into the decision processes that result in risky versus safer sexual behavior in these young adults. These findings (1) have diagnostic value for determining those individuals at higher risk for contracting HIV, (2) indicate several differential risk patterns associated with different reasoning strategies, and (3) provide a basis from which to develop a validated, empirical instrument to identify young adults’ risk level. Based on our findings, we present in the conclusions our proposed screening guidelines for primary-care physicians to use in assessing young adult patients’ HIV risk.
Perceptions of Risky Sexual Behavior: Socio-Cultural Influences
We also explored associations between characteristics of participants’ relationships, social influences, and behavior.52 Results showed that participants’ condom use decisions varied by social (partner influence, condom use attitudes) and cognitive (perceptions of relationship status) factors. Lower-risk participants perceived that their partner’s attitude was to use condoms often or all of the time; whereas higher-risk participants perceived that their partner’s attitude was to use condoms sometimes, rarely, or never. There were also differences by gender across patterns of condom use. For example, males in both high-risk groups scored higher than females on sensation-seeking. High- risk males were also more influenced by their peers regarding condom use.
Some individuals expressed trust in their partners and consequently did not use condoms, in turn leading to greater perceptions of intimacy and increased trust, which served to sustain non-condom use. This example highlights the mechanism that perpetuates risky sexual behavior among this high-risk group. Intervention strategies are needed to break this feedback cycle, and direct these individuals towards healthy and protective behavior. The findings suggest that in order to intervene effectively with higher risk individuals, there is a need to identify the exact nature of the evidence used to support such decisions.
Our findings also suggest that the so-called “monogamous” population could possibly be at higher risk for infection than they realize. For example, trusting, monogamous partners usually perceive their relationship as low risk, in terms of contracting HIV or other STDs. In our study, women defined monogamy as having one partner, whereas most men defined monogamy as having only one primary partner. Thus, if one partner engages in sexual activity outside the relationship, does not use a condom, and contracts HIV from the encounter, the partner then brings the infection back to his or her primary partner, increasing that partner’s chances of infection (with repeated exposure). Therefore, inconsistent or no condom use, even among monogamous couples, can dramatically increase the risk of HIV among a seemingly low risk population.53 Primary care physicians need to avoid discounting the possibility of risky behavior among monogamous individuals.
Sexual Risk, Prior Beliefs, and Decisions
Six months after the first interview, the same young adults participated in a second interview, where they read and responded to sexual encounter scenarios, designed to test the validity of the patterns of condom use identified. Scenarios were developed that reflected the most common behaviors reported in participants’ diaries and interviews. Analysis of responses revealed that comprehension (understanding) of the sexual scenario mediated the relationship between participants’ prior beliefs and decisions.38 Higher-risk individuals paid more attention to content related to the “heat of the moment,” whereas lower-risk individuals paid more attention to content related to the high risks involved in unprotected intercourse. This suggests that emotion-related content is a primary source of evidence used in making condom use decisions.
Summary
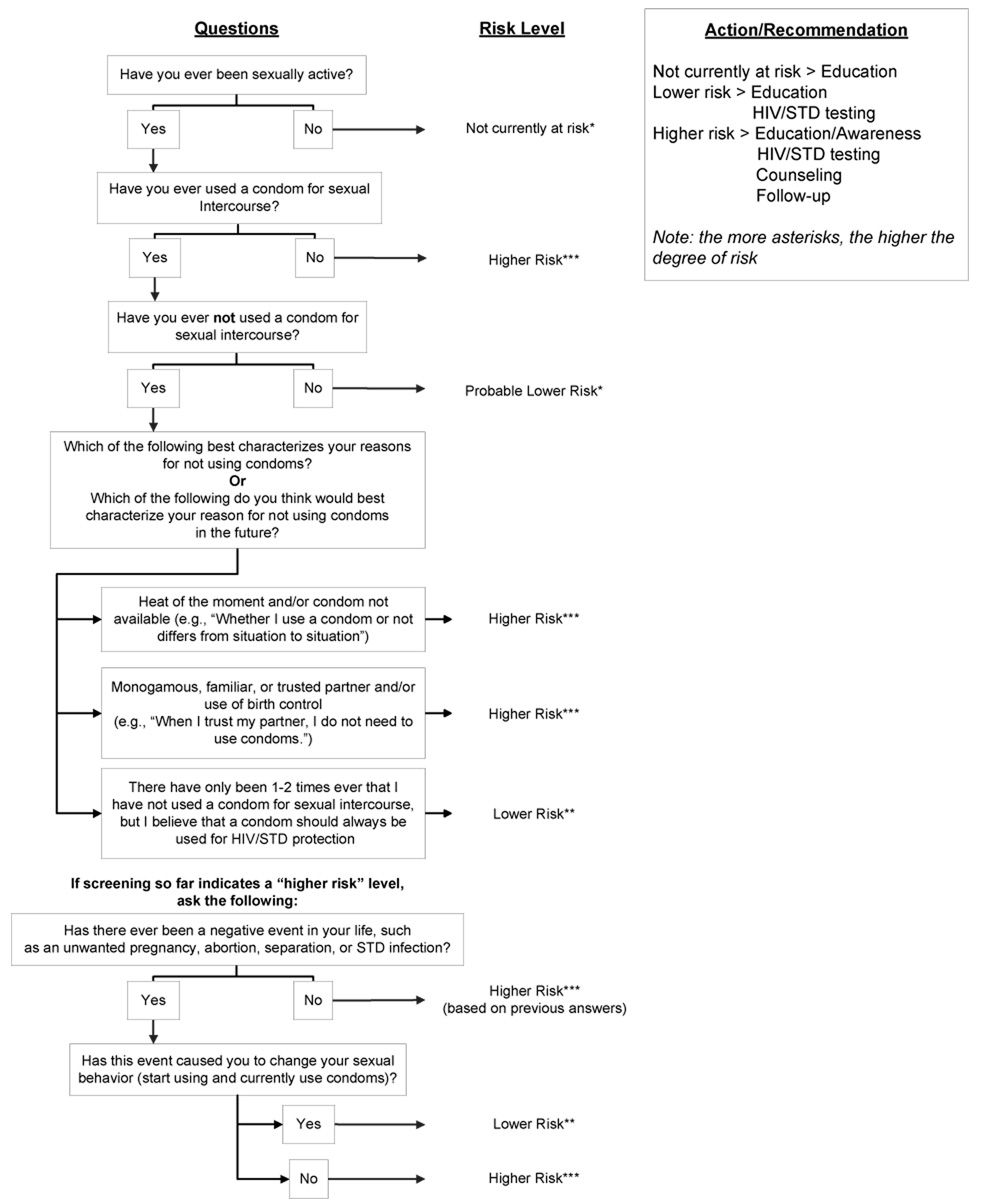
Our research on young adults’ sexual decision-making suggests that custom-tailored strategies are needed to target individuals at different risk levels. Rapid screening measures should be developed for classifying individuals according to their risk profile (e.g. inconsistent condom use), which can then guide the selection of an intervention strategy. Specific strategies include (1) giving young people tools for evaluating their perceptions of the benefits and risks of their unique experiences that provide the context for risky sexual behavior; (2) addressing the potential for discrepancies between perceived risk and actual risk, including ways to identify and weigh pertinent evidence and ways to counter unsupported beliefs; and (3) Using personalized interactive scenarios (congruent with their own beliefs and experiences). In line with these suggestions, we have created a brief set of guidelines for primary care physicians to use when screening adolescent and young adult patients for their level of risk (see Figure 2).
Figure 2.
Guidelines for primary care physicians for identifying the risk level of their patients, based on our research findings.
Conclusions
The main objective of the studies reported in this paper has been to understand the nature of the decision process that leads to risky behaviors. Results show that different patterns of condom use are associated with differing levels of risk. One’s prior beliefs influence decisions based on their personal understanding of the nature of such risks. This understanding is influenced by the evidence used, with emotional evidence playing a bigger role in high-risk situations.
Patterns of behavior and beliefs develop early in individuals’ sexual lives. This suggests that there is high potential value for interventions aimed at early prevention to target youth at different risk levels. Primary-care physicians are the first line of contact for many youths in the health care system. These physicians are accordingly in the best position to screen for at-risk youth. Given time demands and other barriers, we have proposed easy-to-use, evidence-based guidelines for such screening.
Acknowledgments
This research was supported by NIMH Grant R01 MH65851 to Vimla Patel.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.CDC. [Accessed April 13, 2008];HIV/AIDS surveillance report: Cases of HIV infection and AIDS in the United States and Dependent Areas. 2005 http://www.cdc.gov/hiv/topics/surveillance/resources/reports/2005report/default.htm.
- 2.CDC. [Accessed April 13, 2008];HIV/AIDS Surveillance in Adolescents and Young Adults (through 2004) http://www.cdc.gov/hiv/topics/surveillance/resources/slides/adolescents/index.htm.
- 3.Falzer PR. Cognitive schema and naturalistic decision making in evidence-based practices. J Biomed Inform. 2004;37(2):86–98. doi: 10.1016/j.jbi.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Kahneman D. New challenges to the rationality assumption. J Inst Theor Econ. 1994;150:18–36. [Google Scholar]
- 5.Stanovich KE. Rationality and the adolescent mind. Psychological Science in the Public Interest. 2006;7:i–ii. doi: 10.1111/j.1529-1006.2006.00025.x. [DOI] [PubMed] [Google Scholar]
- 6.Reyna VF, Farley F. Risk and rationality in adolescent decision making: implications for theory, practice, and public policy. Psychological Science in the Public Interest. 2006;7:1–44. doi: 10.1111/j.1529-1006.2006.00026.x. [DOI] [PubMed] [Google Scholar]
- 7.Dushoff J, Fitzpatrick S, Buchman TG, et al. Battling bad behavior. Scientist. 2006;20(2):51. [Google Scholar]
- 8.US Department of Health and Human Services. [Accessed April 13, 2008];Healthy people 2010: understanding and improving health. http://www.healthypeople.gov/Document/tableofcontents.htm#volume1.
- 9.Chou R, Huffman LH, Fu R, Smits AK, Korthuis T. Screening for HIV: a review of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2005;143:55–73. doi: 10.7326/0003-4819-143-1-200507050-00010. [DOI] [PubMed] [Google Scholar]
- 10.Paltiel AD, Walensky RP, Schackman BR, et al. Expanded HIV screening in the United States: Effect on clinical outcomes, HIV transmission, and costs. Ann Intern Med. 2006;145:797–806. doi: 10.7326/0003-4819-145-11-200612050-00004. [DOI] [PubMed] [Google Scholar]
- 11.CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55(RR14):1–17. [PubMed] [Google Scholar]
- 12.Chen Z, Branson B, Ballenger A, Peterman TA. Risk assessment to improve targeting of HIV counseling and testing services for STD clinic patients. Sex Transm Dis. 1998;25:539–543. doi: 10.1097/00007435-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Peterman TA, Todd KA, Mupanduki I. Opportunities for targeting publicly funded human immunodeficiency virus counseling and testing. J Acquir Immune Defic Syndr. 1996;12:69–74. doi: 10.1097/00042560-199605010-00010. [DOI] [PubMed] [Google Scholar]
- 14.Freedberg KA, Samet JH. Think HIV: why physicians should lower their threshold for HIV testing. Arch Intern Med. 1999;159:1994–2000. doi: 10.1001/archinte.159.17.1994. [DOI] [PubMed] [Google Scholar]
- 15.Gerbert B, Bronstone A, McPhee S, Pantilat S, Allerton M. Development and testing of an HIV-risk screening instrument for use in health care settings. Am J Prev Med. 1998;15:103–113. doi: 10.1016/s0749-3797(98)00025-7. [DOI] [PubMed] [Google Scholar]
- 16.Haidet P, Stone DA, Taylor WC, Makadon HJ. When risk is low: primary care physicians' counseling about HIV prevention. Patient Educ Couns. 2002;46:21–29. doi: 10.1016/s0738-3991(01)00154-9. [DOI] [PubMed] [Google Scholar]
- 17.Yarnall KSH, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention. Am J Public Health. 2003;93:635–641. doi: 10.2105/ajph.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schechtel J, Coates T, Mayer K, Makadon H. HIV risk assessment: physician and patient communication. J Gen Intern Med. 1997;12:722–723. doi: 10.1046/j.1525-1497.1997.07152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simmons E, Roberts M, Mindy, Beckwith C, Carpenter C, T F. Routine testing for HIV in the United States: the intersection between recommendations and practice. AIDS Patient Care STDs. 2006;20:79–83. doi: 10.1089/apc.2006.20.79. [DOI] [PubMed] [Google Scholar]
- 20.Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: a meta-analysis. Psychol Bull. 1999;125(1):90–132. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- 21.Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: reliability, validity, and predicting HIV risk behavior. J Pers Assess. 1995;65:586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- 22.Rolison MR, Scherman A. College Student Risk-Taking from Three Perspectives. Adolescence. 2003;38(152):689–704. [PubMed] [Google Scholar]
- 23.Kershaw TS, Ethier KA, Milan S, et al. The influence of pregnancy, sexually transmitted diseases, and human immunodeficiency virus perceived susceptibility patterns on sexual risk reduction for adolescent females. J Community Psychol. 2005;33:313–331. [Google Scholar]
- 24.Patel VL, Branch T, Gutnik L, Arocha J. Shaping understanding of HIV through negotiation and conflict resolution during peer group discussion. Adv Health Sci Educ Theory Pract. 2006;11:185–207. doi: 10.1007/s10459-005-2399-9. [DOI] [PubMed] [Google Scholar]
- 25.Kershaw TS, Ethier KA, Niccolai LM, Lewis JB, Ickovics JR. Misperceived risk among female adolescents: social and psychological factors associated with sexual risk accuracy. Health Psychol. 2003;22:523–532. doi: 10.1037/0278-6133.22.5.523. [DOI] [PubMed] [Google Scholar]
- 26.Tversky A, Kahneman D. Judgment under uncertainty: Heuristics and biases. Science. 1974;185:1124–1131. doi: 10.1126/science.185.4157.1124. [DOI] [PubMed] [Google Scholar]
- 27.Slovic P, Finucane ML, Peters E, MacGregor DG. Risk as Analysis and Risk as Feelings: Some Thoughts about Affect, Reason, Risk, and Rationality. Risk Anal. 2004;24(2):311–322. doi: 10.1111/j.0272-4332.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- 28.Misovich SJ, Fisher JD, Fisher WA. Close relationships and elevated HIV risk behavior: Evidence and possible underlying psychological processes. Review of General Psychology. 1997;1:72–107. [Google Scholar]
- 29.Whaley AL. Differential risk perceptions for unintended pregnancy, STDs, and HIV/AIDS among urban adolescents: Some preliminary findings. J Genet Psychol. 2000;161(4):435–452. doi: 10.1080/00221320009596723. [DOI] [PubMed] [Google Scholar]
- 30.Gerrard M, Gibbons FX, Benthin AC, Hessling RM. A longitudinal study of the reciprocal nature of risk behaviors and cognitions in adolescents: what you do shapes what you think, and vice versa. Health Psychol. 1996;15:344–354. doi: 10.1037//0278-6133.15.5.344. [DOI] [PubMed] [Google Scholar]
- 31.Halpern-Felsher BL, Millstein SG, Ellen JM, Adler NE, Tschann JM, Biehl M. The role of behavioral experience in judging risks. Health Psychol. 2001;20:120–126. [PubMed] [Google Scholar]
- 32.Kershaw TS, Ickovics JR, Lewis JB, Niccolai LM, Milan S, Ethier KA. Sexual risk following a sexually transmitted disease diagnosis: the more things change the more they stay the same. J Behav Med. 2004;27:445–461. doi: 10.1023/b:jobm.0000047609.75395.62. [DOI] [PubMed] [Google Scholar]
- 33.Patel V, Groen G. Knowledge-based solution strategies in medical reasoning. Cogn Sci. 1986;10:91–116. [Google Scholar]
- 34.Patel VL, Arocha JF, Zhang J. Thinking and reasoning in medicine. In: Holyoak K, editor. Thinking and reasoning. MA: Cambridge University Press; 2005. pp. 727–750. [Google Scholar]
- 35.Patel VL, Kaufman DR, Arocha JF. Emerging paradigms of cognition in medical decision-making. J Biomed Inform. 2002;35(1):52–75. doi: 10.1016/s1532-0464(02)00009-6. [DOI] [PubMed] [Google Scholar]
- 36.Patel VL, Gutnik LA, Yoskowitz NA, O'Sullivan LF, Kaufman DR. Patterns of reasoning and decision making about condom use by urban college students. AIDS Care. 2006;18(8):918–930. doi: 10.1080/09540120500333509. [DOI] [PubMed] [Google Scholar]
- 37.Patel VL, Yoskowitz NA, Kaufman DR, Gutnik L, Shortliffe EH. AMIA Annu Symp Proc. Washington, DC: 2005. Risky decisions despite counter evidence: Modeling a culture of safer sexual practices; pp. 594–598. [PMC free article] [PubMed] [Google Scholar]
- 38.Patel VL, Yoskowitz NA, Kaufman DR. Comprehension of sexual situations and its relationship to risky decisions by young adults. AIDS Care. 2007;19:916–922. doi: 10.1080/09540120701203303. [DOI] [PubMed] [Google Scholar]
- 39.Leprohon J, Patel VL. Decision-making strategies for telephone triage in emergency medical services. Med Decis Making. 1995;15:240–253. doi: 10.1177/0272989X9501500307. [DOI] [PubMed] [Google Scholar]
- 40.Keselman A, Kaufman DR, Kramer S, Patel VL. Fostering conceptual change and critical reasoning about HIV and AIDS. Journal of Research in Science Teaching. 2007;44:844–863. [Google Scholar]
- 41.Sivaramakrishnan M, Patel VL. Reasoning about childhood nutritional deficiencies by mothers in rural India: A cognitive analysis. Soc Sci Med. 1993;37:937–952. doi: 10.1016/0277-9536(93)90148-w. [DOI] [PubMed] [Google Scholar]
- 42.Brown JS, Collins A, Dugid P. Situated cognition and the culture of learning. Educational Researcher. 1988;18:32–42. [Google Scholar]
- 43.Kuhn D. Children and adults as intuitive scientists. Psychol Rev. 1989;96(4):674–689. doi: 10.1037/0033-295x.96.4.674. [DOI] [PubMed] [Google Scholar]
- 44.Bajos N. Social factors and the process of risk construction in HIV sexual transmission. AIDS Care. 1997;9:227–238. doi: 10.1080/09540129750125244. [DOI] [PubMed] [Google Scholar]
- 45.Fischhoff B. The real world: what good is it? Organ Behav Hum Decis Process. 1996;65:232–248. [Google Scholar]
- 46.Ariely D, Loewenstein G. The heat of the moment: The effect of sexual arousal on sexual decision making. Journal of Behavioral Decision Making. 2006;19:87–98. [Google Scholar]
- 47.Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2nd ed. xiii. Thousand Oaks, CA, US: Sage Publications, Inc (1998); 1998. 312 pp. [Google Scholar]
- 48.Miles MB, Huberman A. Qualitative data analysis: An expanded sourcebook. 2nd ed. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- 49.Koopman C, Ried H. Assessment of knowledge and beliefs about HIV/AIDS among adolescents. In: Davis CM, Yarber WL, Bauserman R, et al., editors. Handbook of sexuality-related measures. Thousand Oaks, CA: Sage; 1998. pp. 321–324. [Google Scholar]
- 50.O'Sullivan LF, Udell W, Patel VL. Young urban adults’ heterosexual risk encounters and perceived risk and safety: A structured diary study. The Journal of Sex Research. 2006;43:343–351. doi: 10.1080/00224490609552333. [DOI] [PubMed] [Google Scholar]
- 51.Arocha JF, Wang D, Patel VL. Identifying reasoning strategies in medical decision making: a methodological guide. J Biomed Inform. 2005;38(2):154–171. doi: 10.1016/j.jbi.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 52.Yoskowitz NA, Kaufman DR, O'Sullivan LF, Patel VL. The slippery slope of sexual decision making in urban young adults: A socio-cognitive analysis. 2008 April; Under review. [Google Scholar]
- 53.Alexander B. Is monogamy dead? A look at the influence of ‘non-connected sex,’ Clinton and Kobe. 2005;vol 2006 [Google Scholar]