Abstract
The rate of habituation to food is inversely related to energy intake, and overweight children may habituate slower to food and consume more energy. This study compared patterns of sensitization, as defined by an initial increase in operant or motivated responding for food, and habituation, defined by gradual reduction in responding, for macaroni and cheese and pizza in overweight and non-overweight 8−12 year-old children. Non-overweight children habituated faster to both foods than overweight children (p = 0.03). All children recovered motivated responding for a new food (chocolate). Overweight children consumed more energy than non-overweight children (p = 0.0004). Children who showed a sensitization in responding consumed more food (p = 0.001), and sensitization moderated the effect of overweight on habituation, with slower habituation for overweight children who sensitized (p < 0.0001). This study replicates previous data on overweight/non-overweight differences in habituation of food and of energy intake, and provides new information that individual differences in sensitization and habituation of motivated responding to food cues may be associated with a sustained motivation to eat, resulting in greater energy intake.
Keywords: Habituation, motivated responding, energy intake, obesity, children
Habituation to food, as defined by a gradual reduction in responding to repeated presentations of a stimulus (Groves & Thompson, 1970) occurs in rodents, non-human primates and humans across a wide variety of responses. Habituation to food stimuli have been observed in rats using mouthing responses (Swithers-Mulvey & Hall, 1992, 1993; Swithers-Mulvey, Miller, & Hall, 1991; Swithers-Mulvey, Mishu, & Hall, 1992; Swithers, 1995, 1996; Swithers & Hall, 1994) and the electrophysiology of mouthing (Swithers, Westneat, & Hall, 1998), in non-human primates by habituation of single cell brain responses (Rolls, Sienkiewicz, & Yaxley, 1989; Rolls, Yaxley, & Sienkiewicz, 1990). Habituation to food has been observed in child and adult humans using salivation (Epstein, Rodefer, Wisniewski, & Caggiula, 1992; Epstein et al., 2003; Wisniewski, Epstein, & Caggiula, 1992), electrophysiology of mouthing in adults (Epstein & Paluch, 1997), and in motivated behavior, or operant responding to obtain food for children and adults (Epstein et al., 2003; Myers Ernst & Epstein, 2002; Temple, Giacomelli, Roemmich, & Epstein, 2008; Temple et al., 2006). In each of these studies a decrement in response was observed to repeated presentations of the same food, with a recovery of responses when a new food was presented or the inhibition of habituation if a variety of foods was presented.
The decrement in responding to repeated presentation of food provides a mechanism for processes related to a reduction in eating (Swithers, 1996; Swithers & Hall, 1994). Research has shown a reliable relationship between rate of habituation and energy intake, with greater intake associated with slower habituation in adults (Wisniewski et al., 1992). If slower rates of habituation are related to greater intake, then it would be predicted that obese persons would show slower habituation to repeated food cues than leaner persons. These obese/non-obese differences have been observed in adults using salivation (Epstein, Paluch, & Coleman, 1996), and recently with children with operant responding to obtain food, or motivated behavior to obtain food (Temple, Giacomelli, Roemmich, & Epstein, 2007). In the latter study, slower habituation was observed for overweight versus lean children to cheeseburgers, with french fries as the novel stimulus. One limitation of that study was the use of only one habituating food, which leaves open the possibility that the findings were specific to cheeseburgers. One goal of this study was to determine if these results generalize to other foods by extending the types of food used as habituating stimuli, with two different, highly palatable, main course foods studied, pizza and macaroni and cheese.
Responses often increase at the beginning of a series of stimulus presentations and then gradually decrease throughout the experimental session (Groves & Thompson, 1970). This initial increase in responding is referred to as sensitization (Groves & Thompson, 1970) and this pattern has been observed for salivary responses to olfactory cues (Wisniewski et al., 1992), salivary responses to gustatory cues (Epstein et al., 1992; Wisniewski, Epstein, Marcus, & Kaye, 1997), and facial muscle responses to gustatory cues in adults (Epstein & Paluch, 1997). While habituation involves a decrement in response after repeated exposure to stimuli, there is considerable variation in the rate of habituation, and some participants demonstrate sensitization prior to habituation to food cues. These individual differences in the pattern of responding may be relevant to understanding how habituation is related to eating and energy intake. Sensitization may be influenced by different processes than habituation. For example, Swithers showed that dopamine antagonists were associated with a reduction in the sensitization component of the habituation/sensitization curve (Swithers, 1996), but the dopamine antagonists did not disrupt the habituation component. Geyer and associates have shown that serotonin antagonists (Geyer, Swerdlow, Mansbach, & Braff, 1990; Geyer & Tapson, 1988) speed up the rate of habituation, but have no influence on sensitization. A second goal of this study was to characterize sensitization to the initial presentation of food stimuli and to assess if individual differences in the pattern of responding are related to differences in the rate of habituation or eating for lean versus overweight children.
METHODS
Participants
Participants were 33 females and 32 males age 8 −12 recruited from a pre-existing database and a direct mailing. Exclusionary criteria for the experiment were: obesity related chronic diseases (i.e., diabetes), developmental or psychological disabilities that may impair participant's ability to complete the experiment; allergies to study foods and prior participation in a laboratory study using similar methodology.
Procedures
The parents of participants were screened by telephone to ensure that the child met the above criteria. Eligible participants were scheduled for one 60-minute visit at the Behavioral Medicine Laboratory on a weekday between the hours of 2:30 and 5:30 pm. Parents were instructed to have their children eat their normal breakfast and lunch, but to not eat or drink anything (except water) three hours prior and not to consume the study foods 24 hours prior to the visit. Upon arrival to the laboratory, both parents and children completed consent and assent forms along with a same-day food recall for the child. Parents then filled out a demographic form while the child filled out food liking, hunger and food preference questionnaires. After forms were completed, the parents were escorted to the waiting area and the experimental task commenced. After the experimental task, participants filled out both a hunger scale and a Dutch Eating Behavior Questionnaire adapted for children (Hill & Pallin, 1998) which assesses dietary awareness. Height and weight were then obtained using the procedures outlined below. Finally, both parent and child were debriefed about the purpose of the study and given written materials about the rationale behind the experiment. Participants were compensated $20 US dollars for completing the experiment and parents were compensated $10 for travel and/or child care expenses. All procedures were conducted in accordance with guidelines for the ethical conduct of human research outlined by the National Institutes of Health and with the approval of the University at Buffalo Health Sciences Institutional Review Board.
Laboratory Environment
The laboratory was constructed for eating experiments and is equipped with an air delivery system that circulates new air through each room approximately 10 times per hour. The experiment rooms were interfaced with intercom and camera systems so that the participant could communicate with the experimenter, who was in an adjacent control room, throughout the duration of the experiment.
Measures
Sensitization and Habituation of Instrumental Responding
Responding on a computer controlled variable interval 120 seconds (VI-120) reinforcement schedule was used to measure instrumental responding for food. The computer task consisted of two squares, one that flashed red every time a mouse button press occurred and another square that flashed green when a point was earned after the VI interval had timed out. Participants were rewarded one point for the first response made after approximately 120s had passed and were reinforced with an 80 to 100 kcal portion of food at that time. The task was presented for 28 minutes, which provided the opportunity for each child to earn up to 14 reinforcers if they maintained responding. At the beginning of the task participants were instructed that when they no longer wanted to earn access to the food stimulus they could go to another table and engage in the alternative activities. Activities included age appropriate puzzles, crosswords, word searches, and magazines. Participants were also told that they could move freely between the computer and activity stations.
The task was divided into habituation and recovery phases. The habituation phase was one 24 minute phase during which participants could earn points on the habituation task towards access to 80 to 100 kcal portions of Kraft® Macaroni and Cheese or Domino's® cheese pizza. The recovery phase lasted for four minutes, and the phase began with a new VI 120s schedule, during which participants had the opportunity to earn points towards 100 Kcal portions of a Hershey's® chocolate bar. For the purposes of studying changes in responding over time, the habituation and recovery phases were divided into two minute blocks, but the habituation and recovery phases were continuous from the perspective of the participant. The recovery phase was used to test the stimulus specificity of responding. One test of whether the initial reduction in responding is due to habituation is to demonstrate a recovery of responding for food when a new food stimulus is presented.
The energy density of pizza, macaroni and cheese and the chocolate bar were 2.4, 2.1 and 4.9 kcal/gram. The percentage of protein, carbohydrates and fat for each food were as follows: pizza, 18.8%, 66.5% and 14.2%; macaroni and cheese, 11.7%, 63.8%, and 24.5%; and chocolate bars, 7.2%, 61%, 31.8%. Participants received the food immediately after each point was earned and could continue to work on the habituation task while eating. The energy intake of the food was determined by weighing the foods before and after the task to the nearest .1 g, and estimating energy intake based on the energy density of the food. Children consumed 94% of the food that was presented, with a correlation of r = .97, p < 0.001 between the energy of the food presented with the energy of the food that was consumed. Water was provided ad libitum throughout the duration of the experiment, but the volume of water consumed was not recorded. The primary outcome measures were the number of responses made for food during each 2-minute interval and the amount of food (g) and energy (kcal) consumed.
Experimenters wore latex gloves for all food handling and maintained careful food preparation and laboratory hygiene throughout the experiment. A freshly baked pizza was used for each session that was delivered to the laboratory uncut, with the experimenters cutting each piece to the appropriate portion size and wrapping each piece in aluminum foil, and placed in a convection oven at 175°C to maintain a constant temperature. A batch of macaroni and cheese was prepared, with individual portions placed in covered bowls. Prior to presentation to the subject each portion was microwaved for 10 s to standardize temperature. Chocolate was portion controlled and placed on covered plates at room temperature until presentation to the participants. Specifics of the food preparation were extensively pretested to provide the most appealing foods that participants would be motivated to eat.
Food Hedonics & Hunger
Liking of study foods was assessed by 5-point Likert type-scales, anchored by one “Do not like” and by five “Like very much”. Hunger/fullness was measured at the beginning and end of each session, and assessed on a 5-point Likert-type scale, anchored by one “Extremely hungry” and by five “Extremely full”.
Same-day Food Recall
Same-day food recalls were conducted by interview with both the child and parent present. This measure was included to verify adherence to the study protocol by ensuring that the participant did not report consumption of food or drink (except water) in the three hours prior to the appointment and that they had not consumed the study foods that day.
Demographics
A general demographics questionnaire was used to assess education status, annual income, race and ethnicity.
Anthropometrics
Height (cm) and weight (kg) were measured without shoes and in light clothing using a Digi-Kit™ digital stadiometer (North Bend, WA) and a Tanita™ digital weight scale (Arlington Heights, IL) after the participant had voided. These measurements were used to calculate BMI (kg/m2). Children below the 85th BMI percentile were defined as non-overweight while children greater than or equal to the 85th BMI percentile were defined as at risk for overweight or overweight (Kuczmarski et al., 2000).
Dietary Awareness
The Dutch Eating Behavior Questionnaire revised for children ages 8−12 was utilized to measure dietary restraint (Hill & Pallin, 1998). Examples of questions asked on the DEBQ are “I have tried to lose weight”; “I try not to eat between meals because I want to be thinner”. The median score on this questionnaire was 6.
Analytic Plan
Data were compared between participants who were non-overweight (< 85th BMI percentile; n=35) or at risk for overweight/overweight (≥ 85th BMI percentile; n=30). Participant characteristics (ex. age, BMI, etc), food liking, subjective hunger prior to the testing session were compared using one-way analysis of variance. Categorical variables, such as parental education, parental income, and percent minority were analyzed using Chi-Square. Amount of food (grams) and energy (Kcal) consumed during the testing session were analyzed using separate one-way ANOVA with weight status as the between subject factor. Changes in hunger/fullness from pre to post testing were assessed using separate two-way ANOVA, with overweight status as the between subject factor, and pre-post as the within subject factor.
Motivated responding (mouse button presses) to obtain food across time blocks (trials) was analyzed using mixed effects regression models (MRM) that allow for the evaluation of repeated measures that take into account differences in variability of responding across time blocks that are observed as the number of time blocks increase (Hedeker & Gibbons, 2006). These models also allow for the specification of the pattern of data, such that the model can be fit as a linear model, if a linear reduction in responding is observed. The model could also be fit as a quadratic (trials * trials) function if the pattern represents a shift in the direction of the responding, as could be observed if the pattern of responding increases prior to decreasing during the habituation curve, or an increase in responding followed by a reduction in the recovery phase when a new food is presented. MRM provides for the opportunity to control for factors that may be related to responding, as well as study moderators of any difference in responding between non-overweight and at-risk for overweight or overweight children (Moderator * overweight status * trials for a linear model). All models included descriptive factors that could influence responding, including age, gender, minority status, socioeconomic status, restraint and responding during baseline as control variables. Log likelihood tests were used to determine whether a quadratic model was a better fit than a linear model for assessing responding from the final habituation to the recovery trials, and to determine whether adding sensitization as a moderator of the influence of overweight status on motivated responding improved the fit of the regression model beyond overweight status.
Sensitization was defined in two ways. First, participants were dichotomized into those who sensitized for their initial responding, or did not sensitize. To our knowledge there is no operational definition of sensitization of motivated responding to guide our choice, and we developed four definitions that fit the criteria of an increase in responding prior to the reduction in responding observed during habituation. The patterns were defined by at least a 10% increase in responding in a subsequent time block above responding during the first two minute time block, a 20% increase in responding during a 2 min time block, and either a 10 or 20% increase in responding over two 2 min time blocks. The choice of which definition to use was based on graphical examination of the patterns of responding that were associated with each definition, as well as log likelihood tests from the mixed effects regression models that tested whether adding information on sensitization to the basic regression model improved fit in comparison to the basic model without including sensitization. In addition to the analyses using dichotomous definitions of sensitization, a mixed regression was also performed to predict the pattern of responses beginning at trial 2 conceptualizing sensitization as a continuous variable, based on changes in responding from trial 1 to trial 2 as the moderator. In the absence of a standard operational definition of how much reduction in response is needed to determine that someone has habituated, we defined habituation as a reduction in responding of at least 75% from baseline responding.
The study was powered based on a previous study on differences in habituation for overweight and non-overweight adults (Epstein et al., 1996). This study showed that overweight (N = 10) adults habituated at a slower rate for food than non-overweight adults (N = 10), with an effect size of .36. Based on 10 trials, an alpha of .05 and power of .80, a difference this large can be observed with 8 subjects/group. The sample size was increased to provide a larger sample to test whether there were any differences in habituation as a function of type of food.
RESULTS
Participant characteristics
The average participant was 10.3 ± 1.3 years of age and had a BMI of 20.9 ± 5.8 (BMI = kg/m2) (Table 1). The majority of the participants' parents completed college (61.5%) and had a household income of greater than $50,000 per year (63.1%). There were no differences (p > 0.05) between the lean and overweight children in age, parental education, household income, food liking, or percentage of minority participants. The overweight group had a greater (F(1,63) = 11.54, p = 0.001; Table 1) dietary restraint score than the non-overweight group.
Table 1.
Characteristics of participants by overweight and non-overweight
| Descriptive variables | Group | |||
|---|---|---|---|---|
| Non-overweight | Overweight | |||
| Mean |
SD |
Mean |
SD |
|
| Number of participants | 35 | 30 | ||
| Age (years) | 10.4 | 1.4 | 10.3 | 1.2 |
| *BMI (kg/m2) | 16.8 | 1.9 | 25.6 | 5.2 |
| *zBMI | −0.2 | 0.8 | 1.9 | 0.4 |
| *Dietary awareness | 4.4 | 2.6 | 6.5 | 2.4 |
| Hunger | 2.2 | 0.8 | 2.6 | 0.9 |
| Pizza liking | 4.2 | 0.9 | 4.1 | 1.0 |
| Macaroni and Cheese liking | 4.0 | 1.0 | 4.0 | 1.0 |
| Chocolate Bar liking | 4.2 | 1.1 | 3.6 | 1.1 |
| Same day energy intake (kcal) | 646 | 406.8 | 736.2 | 445.5 |
| N | % | N | % | |
| Gender | ||||
| Males | 17 | 49 | 15 | 50 |
| Females | 18 | 51 | 15 | 50 |
| Race | ||||
| Caucasian | 28 | 80.0 | 18 | 60.0 |
| Minority | 7 | 20.0 | 12 | 40.0 |
| Parent's income | ||||
| Under $29,999 | 5 | 14.3 | 5 | 16.7 |
| $30,000-$49,999 | 4 | 11.4 | 10 | 33.3 |
| ≥ $50,000 | 26 | 74.3 | 15 | 50.0 |
| Parental education | ||||
| Some High School | 0 | 0.0 | 1 | 3.3 |
| High school/vocational | 11 | 31.4 | 13 | 43.3 |
| College or graduate degree | 24 | 68.6 | 16 | 53.3 |
Note. Dietary awareness was measured using the Dutch Eating Behavior Questionnaire (Hill & Pallin, 1998), hunger/fullness and liking were measured using 5 point Likert-type scales, with 1 being hungry or low in liking, 5 full or high in liking, BMI = body mass index (kg/m2); * p < >05 between groups.
Habituation
MRM showed that overweight status was a predictor of the rate of responding across the time blocks (Estimate = 14.11, p = 0.03, Figure 1A), along with the type of food that was presented during the habituation series (Estimate = 8.13, p = 0.008, Figure 1B), but there was no interaction between overweight status and the type of food over time blocks (p > .05). All of the non-overweight children (1/35 = 2.9%) but one met the definition of habituation by the final two minute block (mean = 5.7 responses), while eight (8/30 = 26.7%) of the overweight children did not meet the definition of habituation, and the average overweight child made 84.4 responses (X2 (1) = 7.68, p = 0.006). As shown in the recovery portions of Figures 1A and 1B, a quadratic change in responding characterized by an increase from time block 12 to 13 followed by a decrement in responding to the new food was observed from time blocks 13 to 14 (Estimate = −270.08, p < 0.0001), which was a significant improvement over a linear model (X2(1) = 98.72, p < 0.001). The failure to observe complete habituation in so many of the overweight children made it difficult to compare recovery of responding for overweight versus non-overweight, since it does not make sense to study recovery if the overweight child had not yet habituated.
Figure 1.
Differences in motivated responding (mean ± SEM) on variable ratio 120 second schedules of reinforcement for non-overweight versus overweight children (Figure 1A) and for pizza and macaroni and cheese (Figure 1B). Mixed regression models showed both overweight status (p = 0.03) and type of food (p = 0.008) influenced the rate of habituation. Recovery of responding was shown when chocolate was presented as a novel food after the 12th 2 minute time block (p < 0.001).
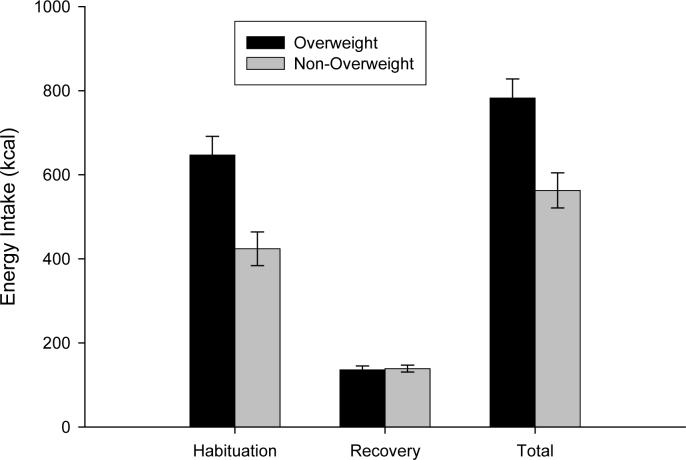
Energy intake was greater for the overweight compared to non-overweight children during the habituation time blocks (F (1,61) = 14.04, p = 0.0004, Figure 2), but there were no differences in energy intake as a function of food (p = 0.33) or the interaction of overweight status by food (p = 0.88). No differences in energy intake were observed during the recovery time blocks as a function of overweight status (p = 0.82), type of habituating food (p = 0.69), or the interaction of overweight status with the type of habituating food (p = 0.50). When total energy intake for both habituating and recovery time blocks was considered, overweight children consumed more energy (F(1,61) = 12.87, p = 0.0007), but no differences were observed as a function of type of habituating food (P = 0.31) or the interaction of type of habituating food by overweight status (p = 0.77). The average overweight child earned 7.5 ± 2.8 portions of food during habituation in comparison to 5.2 ± 3.0 portions earned by non-overweight children (p < 0.002), and a total of 9.3 ± 2.8 versus 6.9 ± 3.1 portions of food (p < 0.002). There was a significant increase in fullness for all participants from pre- to post-testing (F(1,63) = 152.22, p < 0.001), but no interaction of fullness with weight.
Figure 2.
Energy consumption (mean ± SEM) during the habituation and recovery phases, and total energy intake across both phases for overweight and non-overweight children. Overweight children consumed greater energy during the habituation phase (p < 0.001) and for total energy consumption (p < 0.001).
Sensitization
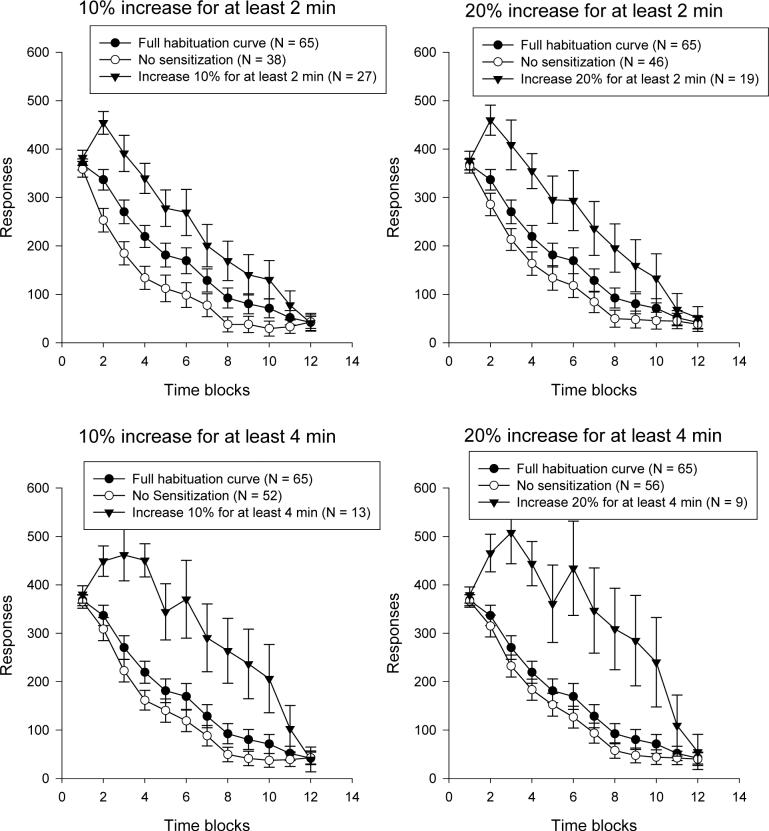
While the average child showed a gradual reduction in responding over time, there was variability in responding, with some children showing a gradual decrease in responding, but other children showing an increase in responding before showing a decrease. The increase can be interpreted as sensitization of responding (Swithers, 1996). The pattern of responding based on different definitions of sensitization are shown in Figure 3. Significant differences in responding were observed for the children who first sensitized and then habituated for each analysis (p's < 0.0001) based on the different definitions of sensitization. The numbers of participants who met criteria for sensitization were reduced as the criteria became more stringent, with 27 meeting the criteria of a 10% increase for at least one two minute block, while only 9 participants met the criteria of a 20% increase for 2 two minute blocks. Mixed models to assess whether adding sensitization as a moderator improved the fit of the models predicting the patterns of responding showed that the largest effect was for the 10% one 2 min block criteria (X2(3) = 40.14, p < 0.001), with smaller effects for the 20% increase for one 2 minute block (X2(3) = 37.88, p < 0.001) , 10% for 2 two minute blocks (X2(3) = 35.80, p < 0.001), or 20% for 2 two minute blocks (X2(3) = 34.82, p < 0.001). Since the definition of a 10% increase for one two minute block included the most participants and improved the fit of the model the most, this definition was used to study how sensitization moderated responding.
Figure 3.
Motivated responding (mean ± SEM) on variable ratio 120 second schedules of reinforcement for children who sensitized and those who did not for the four definitions of sensitization. In each case there were significant differences in the rate of habituation comparing those who sensitized versus those who did not sensitize (p < 0.001). The n that met criteria for each definition is shown in each graph, along with the average habituation curve of all participants.
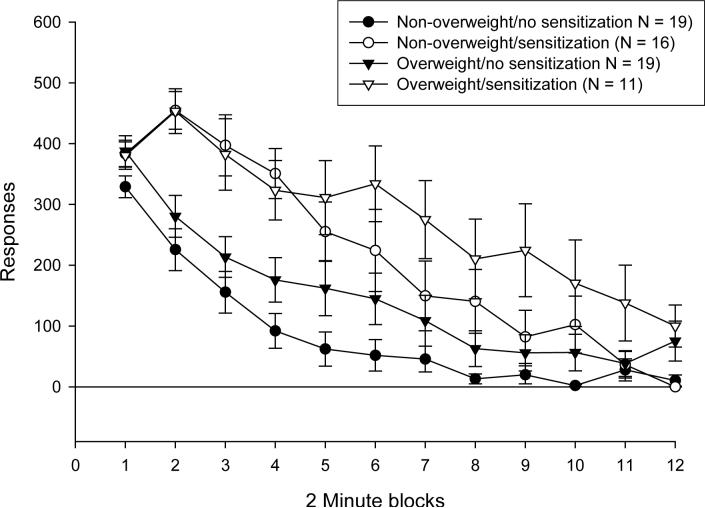
Sensitization was a moderator of responding as a function of overweight status. The interaction of sensitization × time blocks (estimate = −15.07, p < 0.0001) and the interaction of overweight × sensitization × time blocks (estimate = 11.81, p = 0.006) significantly improved the fit of the model predicting responding for food beyond the interaction of overweight × time blocks (X2(3) = 40.14, p < 0.001, Figure 4). Sensitization did not interact with the type of food to influence responding (p > 0.05). The differences in motivated responding between overweight and non-overweight children were greater when comparing those who sensitized (estimate = 28.41, p = 0.01) with those who did not sensitize (estimate = −6.70, p = 0.39). Similar effects were observed if sensitization was considered a continuous variable, with a significant interaction of sensitization × time blocks (estimate = −.11, p < 0.0001) and the interaction of overweight × sensitization × time blocks (estimate = 0.07, p < 0.0001) significantly improved the fit of the model predicting responding for food beyond the interaction of overweight × time blocks (X2(3) = 63.76, p < 0.001).
Figure 4.
Motivated responding (mean ± SEM) on variable ratio 120 second schedules of reinforcement for overweight or non-overweight children who did or did not sensitize. Sensitization interacted with overweight status to influence responding across time blocks (p < 0.001). No differences in the rate of habituation were observed between overweight and non-overweight children who did not sensitize, but slower habituation was observed for the overweight in comparison to the non-overweight children (p = 0.003).
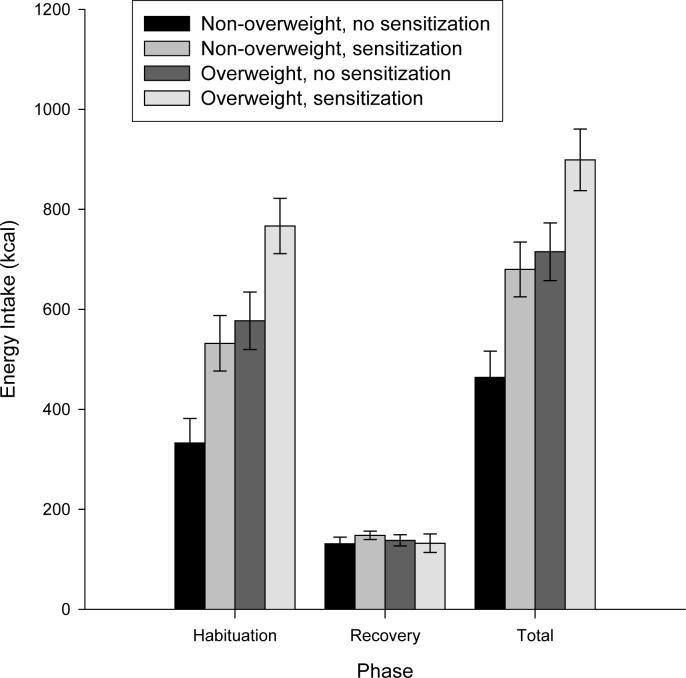
As shown in Figure 5, there was a main effect of sensitization on energy intake across the habituation time blocks (F(1,61) = 11.80, p = 0.001) and for total energy intake (F(1,61) = 11.72, p = 0.001), as well as a main effect of overweight status during habituation (F(1,61) = 17.92, p < 0.0001 and for total energy intake (F(1,61) = 16.22, p < 0.001). There was no interaction (p = 0.93), as sensitizing increased the energy intake of both non-overweight and overweight children. Children who sensitized earned 7.6 ± 2.8 versus 5.3 ± 3.0 portions of food (P = 0.005). Non-overweight children who did not sensitize consumed the fewest total calories (463.9 ± 228.5 kcals), while non-overweight children who sensitized consumed a similar number of calories (679.9 ± 219.2 kcals) as those overweight children who did not sensitize (715.2 ± 251.6 kcals). Overweight children who sensitized consumed the most energy (899.0 ± 203.8 kcals).
Figure 5.
Energy consumption (mean ± SEM) for overweight and non-overweight subjects who sensitized and did not sensitize during the habituation and recovery phases, as well as total energy intake. Children who sensitized consumed more food during the habituation phase (p = 0.001) and for total energy intake (p = 0.001). No interaction of sensitization and weight status on energy intake was observed.
Individual differences between children who sensitized versus those who did not sensitize were explored to determine potential factors that might explain differences in responding. No significant differences were observed between children who sensitized or did not sensitize for gender (p = 0.88), age (p = 0.19), percentage overweight (p = 0.50), restraint (p = 0.55), baseline hunger (p = .55) liking for pizza (p = 0.91), macaroni and cheese (p = 0.62) or the chocolate bar (p = 0.35), or same day energy intake prior to coming to the laboratory (p = 0.77). While overweight children showed a greater effect of sensitization on responding for food, there were no differences in the percentage of non-overweight (46%) versus overweight (37%) children who sensitized (X2 (1) = 0.54, p = 0.46).
DISCUSSION
The results support the hypothesis that overweight children habituate at slower rates to food than lean children (Temple et al., 2007), and this effect is not specific to the types of foods used as habituating stimuli. Differences in the rate of habituation have now been observed for cheeseburgers (Temple et al., 2007), pizza and macaroni and cheese. The results also show for the first time that the pattern of sensitization moderated the pattern of habituation to food, which relates to greater degree of motivation to eat, and greater energy intake. The differences in responding between the overweight versus the non-overweight children was moderated in part by the sensitization of the initial responding for food.
A reduction in motivated responding and recovery of responding when a new food is presented extends the analysis of habituation from reflexive responses such as salivation (Epstein et al., 1992; Wisniewski et al., 1992), to complex behavioral responses that are directly related to food acquisition and consumption. McSweeney and colleagues have extended principles associated with habituation to motivated responding for food (McSweeney, Hinson, & Cannon, 1996; McSweeney & Swindell, 1999), and this model may provide novel mechanisms to understand the termination of eating. It is critical when defining habituation that a recovery of responses is observed when a new food is presented. This ensures that the reduction in responding is not due to response fatigue, the reduction in need to replenish energy in an energy depletion model of eating, or a reduction in responding due to general reinforcer satiation (McSweeney & Murphy, 2000; McSweeney & Roll, 1998; Swithers, 1996). The reduction in responding with repeated presentation of one food, but recovery when another food is presented demonstrates that the pattern of motivated responding is specific to characteristics of the two foods. This could be a function of a number of characteristics of the foods, including differences in the taste, olfaction, texture, or appearance of the foods (Raynor & Epstein, 2001). Research is needed to examine factors that influence recovery after habituation has occurred. For example, if someone had habituated responding to plain cheese pizza, would they recover motivation to eat pepperoni pizza? Similarly, if someone habituated to chicken fingers without sauce, would they recover responding if a favorite dipping sauce was provided along with the chicken fingers? It is possible that overweight children will be more reactive to small differences in the recovery food than leaner children.
The demonstration of individual differences in habituation between overweight and non-overweight children to two different main course items provides confidence in the generalization of the effect across foods. However, there are many variations of foods that could be tested, including snack foods versus main course foods, foods that vary in macronutrient content, or foods that vary in palatability. The general principle of habituation is that a reduction in responding is observed as the person consumes more of the food, and recovery of responding is observed when a new food is presented. This general pattern of responding should be observed across all foods that people are motivated to consume, but there may be important individual differences in the magnitude of responding and the rates of change in habituation and recovery across foods for overweight and non-overweight children that are important in the development and/or maintenance of their weight status.
No differences in the percentage of overweight or non-overweight children who sensitized were observed, but this study demonstrated that individuals who sensitized showed differences in the subsequent pattern of motivated responding for food, and that these differences were more pronounced in the overweight than leaner children. Habituation theory has recognized that sensitization often precedes habituation, with the possibility that they represent two different behavioral processes mediated by different physiological changes (Groves & Thompson, 1970). As suggested by Swithers-Mulvey (Swithers, 1996), sensitization may be mediated by dopaminergic activity, while research by Geyer and colleagues has shown habituation may be more related to serotonergic activity (Geyer & Tapson, 1988). Geyer and colleagues have also shown that the rate of habituation of the startle response is related to schizophrenia, which is an example of how individual differences in habituation may provide important information on mechanisms related to specific behavioral disorders (Geyer et al., 1990). One model for sensitization is that it represents increased responding due to the state of arousal (Meincke, Light, Geyer, Braff, & Gouzoulis-Mayfrank, 2004) or arousing properties of the sensitizing stimulus (Swithers, 1996). In the current study there may be individual differences in the arousing or activating (Duffy, 1972) properties of food, and these individual differences may relate to an increased motivation to eat. We have shown that manipulating subjective arousal and cardiovascular arousal can alter dishabituation of salivary responses to food cues (Epstein, Mitchell, & Caggiula, 1993), but to our knowledge there has been no research that examines the arousing properties of food and motivation to eat.
While overweight children who sensitized showed a slower rate of habituation than lean children who sensitized, overweight children were no more likely to sensitize than leaner children. This suggests that sensitization and overweight may be independent. Children who sensitize consumed more food than children who did not sensitize, and these children may have greater challenges in regulating their energy intake and body weight than children who do not sensitize. This may lead to an increased risk of the development of obesity for these lean children. Additional research is needed to further examine how body weight differences are related to patterns of sensitization.
Introduction of a new food after habituation was associated with recovery of responding, with the motivation to eat the chocolate greater after habituation than the initial motivation to consume the main course. Not surprisingly, the motivation to consume the chocolate was reduced over time, and presumably would have also reduced to very low levels, another example of habituation. It would be interesting to determine whether there are individual differences in recovery as a function of weight status, or due to the type of food. It may have been necessary to include more time in recovery, since the differences between overweight and non-overweight children became more different over time. It is expected that the motivation to consume the recovery food would also habituate, and this shift in responding may follow the same pattern as change to the habituating stimulus, with a slower rate of habituation for overweight compared to leaner children. It is worth considering differences in recovery to different foods, since greater recovery of responding when a new food is presented would lead to greater energy intake for overweight compared to non-overweight children.
There are methodological issues that must be considered in research that focuses on patterns of response during recovery. First, it is necessary to start all subjects at the same place prior to presentation of the recovery stimulus. In the present study the overweight children were responding more than the leaner children during the last two minutes of observation, and a substantial number of overweight children (8/30 = 27%) showed little evidence of habituation at the last observation. It is conceptually difficult to consider recovery for children who never showed habituation. The most straightforward methodological solution is to continue presenting habituation trials until each subject has habituated, and to use the number of trials to habituation as a dependent measure comparing individual differences (Wisniewski et al., 1992).
An alternative paradigm to the habituation/recovery paradigm used in this study is to vary the foods during each trial in comparison to repeatedly presenting the same foods. When foods are varied on each trial, participants show a reduction in the rate of habituation, and consume more food (Temple et al., 2008). This paradigm is closer to usual eating for many people, in that food presentations usually are mixed, rather than presented in sequential order. Research is needed to compare the rate of habituation to food variety in overweight versus non-overweight children.
Habituation may provide insight into sensory specific satiety (Epstein, Temple, & Roemmich, 2008; Raynor & Epstein, 2001), another approach that studies changes in eating behaviors when a new food is introduced (Hetherington & Rolls, 1996; Rolls et al., 1981). The usual paradigm for sensory specific satiety is to measure food hedonics for a variety of foods, feed the participant one food to satiety, and retest hedonics. Sensory specific satiety is observed when liking for the food that was consumed decreases, while liking of other foods is maintained. Sensory specific satiety paradigms do not usually test the pattern of change in liking over trials, and we are not familiar with research that might assess increases in liking followed by decreases using the sensory specific satiety paradigm. It would be interesting to test whether sensitization of liking would be observed if liking was repeatedly measured when food cues were presented repeatedly, and whether a different pattern of change in eating would be observed for those who showed an initial increase in liking versus those who showed a gradual decrease in liking over repeated food presentations.
This study suggests that food acquisition and eating are more complex than once thought. The slower rate of habituation to food in overweight versus leaner children does not provide an indication of the direction of the effect. It is possible that being overweight may produce slower habituation, as people are more motivated to consume food if they are overweight, and require more food before they are satisfied. If this is the direction of the effect, then research is needed to identify specific characteristics related to being overweight that could cause slower rates of habituation. It is also possible that slower rates of habituation may precede and contribute to overweight and obesity, and those who habituate slower to food cues may be at greater risk for developing weight problems than people who habituate at faster rates. This exciting possibility would need to be tested by a prospective design that studies children who differ in their rate of habitation and who are not yet overweight, and follows them over time to assess whether these individual differences predict who will become obese later in childhood or in adulthood. The reliable finding that there are differences in the rate of habituation between overweight and non-overweight children warrants additional research to assess how habituation may be related to the development or persistence of obesity in children.
Acknowledgements
Dr. Epstein is a consultant to Kraft foods and to Griffin Hospital, Yale University. The other authors do not have any potential conflict of interests. This research was funded in part by a grant from the National Institute of Child Health and Human Development, R01 HD044725 awarded to Dr. Epstein.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Duffy E. Activation. In: Greenfield NS, Sternbach RA, editors. Handbook of Psychophysiology. Holt, Rinehart and Winston, Inc.; New York: 1972. pp. 577–622. [Google Scholar]
- Epstein LH, Mitchell SL, Caggiula AR. The effect of subjective and physiological arousal on dishabituation of salivation. Physiology and Behavior. 1993;53:593–597. doi: 10.1016/0031-9384(93)90158-c. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Paluch R, Coleman KJ. Differences in salivation to repeated food cues in obese and nonobese women. Psychosomatic Medicine. 1996;58:160–164. doi: 10.1097/00006842-199603000-00011. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Paluch RA. Habituation of facial muscle responses to repeated food stimuli. Appetite. 1997;29:213–224. doi: 10.1006/appe.1997.0102. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Rodefer JS, Wisniewski L, Caggiula AR. Habituation and dishabituation of human salivary response. Physiology and Behavior. 1992;51:945–950. doi: 10.1016/0031-9384(92)90075-d. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Saad FG, Handley EA, Roemmich JN, Hawk LW, McSweeney FK. Habituation of salivation and motivated responding for food in children. Appetite. 2003;41:283–289. doi: 10.1016/s0195-6663(03)00106-5. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Temple JL, Roemmich JN. Habituation as a determinant of human food intake. Manuscript submitted for publication. 2008 doi: 10.1037/a0015074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geyer MA, Swerdlow NR, Mansbach RS, Braff DL. Startle response models of sensorimotor gating and habituation deficits in schizophrenia. Brain Research Bulletin. 1990;25:485–498. doi: 10.1016/0361-9230(90)90241-q. [DOI] [PubMed] [Google Scholar]
- Geyer MA, Tapson GS. Habituation of tactile startle is altered by drugs acting on serotonin-2 receptors. Neuropsychopharmacology. 1988;1:135–147. doi: 10.1016/0893-133x(88)90005-x. [DOI] [PubMed] [Google Scholar]
- Groves PM, Thompson RF. Habituation: A dual-process theory. Psychological Review. 1970;77:419–450. doi: 10.1037/h0029810. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal data analysis. John Wiley & Sons; Hoboken, N.J.: 2006. [Google Scholar]
- Hetherington MM, Rolls BJ. Sensory-specific satiety: Theoretical frameworks and central characteristics. In: Capaldi ED, editor. Why we eat what we eat: The psychology of eating. American Psychological Association; Washington, D.C.: 1996. pp. 267–290. [Google Scholar]
- Hill AJ, Pallin V. Dieting awareness and low self-worth: related issues in 8-year-old girls. International Journal of Eating Disorders. 1998;24:405–413. doi: 10.1002/(sici)1098-108x(199812)24:4<405::aid-eat7>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC Growth Charts: United States. Vol. 314. National Center for Health Statistics; Hyattsville,MD: 2000. pp. 24–25. [Google Scholar]
- McSweeney FK, Hinson JM, Cannon CB. Sensitization-habituation may occur during operant conditioning. Psychological Bulletin. 1996;120:256–271. [Google Scholar]
- McSweeney FK, Murphy ES. Criticisms of the satiety hypothesis as an explanation for within-session decreases in responding. Journal of the Experimental Analysis of Behavior. 2000;74:347–361. doi: 10.1901/jeab.2000.74-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McSweeney FK, Roll JM. Do animals satiate or habituate to repeatedly presented reinforcers? Psychonomic Bulletin and Review. 1998;53:428–442. [Google Scholar]
- McSweeney FK, Swindell S. General-process theories of motivation revisited: The role of habituation. Psychological Bulletin. 1999;125:437–457. [Google Scholar]
- Meincke U, Light GA, Geyer MA, Braff DL, Gouzoulis-Mayfrank E. Sensitization and habituation of the acoustic startle reflex in patients with schizophrenia. Psychiatry Research. 2004;126:51–61. doi: 10.1016/j.psychres.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Myers Ernst M, Epstein LH. Habituation of responding for food in humans. Appetite. 2002;38:224–234. doi: 10.1006/appe.2001.0484. [DOI] [PubMed] [Google Scholar]
- Raynor HA, Epstein LH. Dietary variety, energy regulation, and obesity. Psychological Bulletin. 2001;127:325–341. doi: 10.1037/0033-2909.127.3.325. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Rowe EA, Rolls ET, Kingston B, Megson A, Gunary R. Variety in a meal enhances food intake in man. Physiology and Behavior. 1981;26:215–221. doi: 10.1016/0031-9384(81)90014-7. [DOI] [PubMed] [Google Scholar]
- Rolls ET, Sienkiewicz ZJ, Yaxley S. Hunger modulates the responses to gustatory stimuli of single neurons in the caudolateral orbitofrontal cortex of the macaque monkey. European Journal of Neuroscience. 1989;1:53–60. doi: 10.1111/j.1460-9568.1989.tb00774.x. [DOI] [PubMed] [Google Scholar]
- Rolls ET, Yaxley S, Sienkiewicz ZJ. Gustatory responses of single neurons in the caudolateral orbitofrontal cortex of the macaque monkey. Journal of Neurophysiology. 1990;64:1055–1066. doi: 10.1152/jn.1990.64.4.1055. [DOI] [PubMed] [Google Scholar]
- Swithers-Mulvey SE, Hall WG. Control of ingestion by oral habituation in rats. Behavioral Neuroscience. 1992;106:710–717. doi: 10.1037//0735-7044.106.4.710. [DOI] [PubMed] [Google Scholar]
- Swithers-Mulvey SE, Hall WG. Integration of oral habituation and gastric signals in decerebrate rat pups. American Journal of Physiology. 1993;34:R216–R219. doi: 10.1152/ajpregu.1993.265.1.R216. [DOI] [PubMed] [Google Scholar]
- Swithers-Mulvey SE, Miller GL, Hall WG. Habituation of oromotor responding to oral infusions in rat pups. Appetite. 1991;17:55–67. doi: 10.1016/0195-6663(91)90084-6. [DOI] [PubMed] [Google Scholar]
- Swithers-Mulvey SE, Mishu KR, Hall WG. Oral habituation in rat pups is in the brainstem. Physiology and Behavior. 1992;51:639–642. doi: 10.1016/0031-9384(92)90189-9. [DOI] [PubMed] [Google Scholar]
- Swithers SE. Effects of physiological state on oral habituation in developing rats: cellular and extracellular dehydration. Developmental Psychobiology. 1995;28:131–145. doi: 10.1002/dev.420280302. [DOI] [PubMed] [Google Scholar]
- Swithers SE. Effects of oral experience on rewarding properties of oral stimulation. Neuroscience and Biobehavioral Reviews. 1996;20:27–32. doi: 10.1016/0149-7634(95)00031-9. [DOI] [PubMed] [Google Scholar]
- Swithers SE, Hall WG. Does oral experience terminate ingestion? Appetite. 1994;23:113–138. doi: 10.1006/appe.1994.1041. [DOI] [PubMed] [Google Scholar]
- Swithers SE, Westneat MW, Hall WG. Electromyographic analysis of oral habituation in rat pups. Physiology and Behavior. 1998;63:197–203. doi: 10.1016/s0031-9384(97)00421-6. [DOI] [PubMed] [Google Scholar]
- Temple JL, Giacomelli AM, Roemmich JN, Epstein LH. Overweight children habituate slower than non-overweight children to food. Physiology and Behavior. 2007;91:250–254. doi: 10.1016/j.physbeh.2007.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Giacomelli AM, Roemmich JN, Epstein LH. Dietary variety impairs habituation in youth. Health Psychology. 2008;27:S10–S19. doi: 10.1037/0278-6133.27.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple JL, Kent KM, Giacomelli AM, Paluch RA, Roemmich JN, Epstein LH. Habituation and recovery of salivation and motivated responding for food in children. Appetite. 2006;46:280–284. doi: 10.1016/j.appet.2006.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisniewski L, Epstein LH, Caggiula AR. Effect of food change on consumption, hedonics, and salivation. Physiology and Behavior. 1992;52:21–26. doi: 10.1016/0031-9384(92)90428-5. [DOI] [PubMed] [Google Scholar]
- Wisniewski L, Epstein LH, Marcus MD, Kaye W. Differences in salivary habituation to palatable foods in bulimia nervosa patients and controls. Psychosomatic Medicine. 1997;59:427–433. doi: 10.1097/00006842-199707000-00013. [DOI] [PubMed] [Google Scholar]