Abstract
Background
Heterozygous gain‐of‐function mutations in various genes encoding proteins of the Ras‐MAPK signalling cascade have been identified as the genetic basis of Noonan syndrome (NS) and cardio‐facio‐cutaneous syndrome (CFCS). Mutations of SOS1, the gene encoding a guanine nucleotide exchange factor for Ras, have been the most recent discoveries in patients with NS, but this gene has not been studied in patients with CFCS.
Methods and results
We investigated SOS1 in a large cohort of patients with disorders of the NS–CFCS spectrum, who had previously tested negative for mutations in PTPN11, KRAS, BRAF, MEK1 and MEK2. Missense mutations of SOS1 were discovered in 28% of patients with NS. In contrast, none of the patients classified as having CFCS was found to carry a pathogenic sequence change in this gene.
Conclusion
We have confirmed SOS1 as the second major gene for NS. Patients carrying mutations in this gene have a distinctive phenotype with frequent ectodermal anomalies such as keratosis pilaris and curly hair. However, the clinical picture associated with SOS1 mutations is different from that of CFCS. These findings corroborate that, despite being caused by gain‐of‐function mutations in molecules belonging to the same pathway, NS and CFCS scarcely overlap genotypically.
Keywords: congenital heart defect, pulmonic stenosis, short stature, ras pathway
Research data accumulated during the past few years have significantly contributed to our current understanding that constitutive activation of the Ras‐MAPK signalling cascade is most likely the common pathogenetic mechanism underlying Noonan syndrome (NS; OMIM 163950) and two related disorders, cardio‐facio‐cutaneous syndrome (CFCS; OMIM 115150) and Costello syndrome (OMIM 218040).1,2,3,4,5 These disorders share a common pattern of congenital anomalies, including typical heart defects, craniofacial dysmorphism, short stature, skeletal anomalies and varying degrees of mental retardation.6,7,8PTPN11, encoding the protein tyrosine phosphatase SHP‐2, which transduces signals from activated growth factor receptors to Ras and other signalling molecules, was first discovered as the major gene mutated in NS.1 In contrast, CFCS was found to be associated with mutations in any of the genes BRAF, MEK1 or MEK2, encoding components of the well‐known B‐Raf‐MEK‐ERK signalling cascade downstream from Ras.3,4 Mutations in the KRAS gene have been found in patients with NS and CFCS, 3,5,9,10 and specific mutations in HRAS have been detected in the vast majority of people with Costello syndrome.2 Nevertheless, no genetic defect has been found in ∼30% of paients with CFCS and in ∼50% of those with NS until recently.
To identify novel genes for these disorders, we screened additional functional candidates encoding proteins involved in the Ras‐MAPK signalling pathway, including SOS1. While this work was in progress, two other groups reported gain‐of‐function mutations of SOS1 in 17–20% of PTPN11 mutation‐negative patients with NS.11,12SOS1 encodes a guanine exchange factor (GEF) for Ras catalysing the conversion of the inactive GDP‐bound form of Ras to its active GTP‐bound form. The precise mechanisms of SOS1 activation are incompletely understood. Conformational changes within SOS1 allowing Ras to access its allosteric binding site that, in the inactive state, is blocked by an intramolecular interaction involving the Dbl homology–pleckstrin homology (DH‐PH) unit are presumed to play an important role.13,14,15 NS‐associated SOS1 mutations have been suggested to result in a release of autoinhibition, followed by an increase in GEF activity subsequently leading to enhanced levels of active, GTP‐bound Ras.11,12 Indeed, by analysing representative mutant SOS1 proteins, these NS‐associated mutations were found to cause a gain‐of‐function effect, as shown by increased Ras and ERK activation in vitro.11,12
Patients and methods
Study population
Ethics approval for this study was obtained from the Ethics Committee of the University of Erlangen‐Nuremberg, and informed consent for the genetic analyses was received from patients or their legal guardians.
Our initial study population (group 1) consisted of 85 clinically well‐characterised patients with NS and CFCS, who were assessed by experienced clinical geneticists. In total, 53 patients (group 1A) were classified as having NS according to established diagnostic criteria,16,17 and 21 patients (group 1B) were given the diagnosis of CFCS, supported by the published CFC index.18 In 11 patients (group 1C), a clear‐cut assignment to one of these two syndromes was not possible. This subgroup comprised six patients with normal mental development suggestive of NS but ectodermal anomalies similar to those seen in CFCS, and five infants classified as “borderline”, as they had a phenotype that could evolve into either NS or CFCS. All study participants had previously tested negative for mutations in the genes PTPN11, KRAS and HRAS. Patients in groups 1B and 1C had been screened for mutations in BRAF, MEK1 and MEK2 with normal results.
In addition, we included a second cohort (group 2), comprising 80 patients referred for molecular diagnosis of NS and tested negative for a PTPN11 mutation. This group contained a considerable number of cases with a mild or atypical phenotype. A PTPN11 mutation detection rate of 18% in the original cohort, from which group 2 was derived, reflects the clinical and genetic heterogeneity in this group.
Molecular analysis
DNA specimens obtained from blood cells were screened for SOS1 mutations by direct sequencing of all coding exons (ABI BigDye Terminator Sequencing Kit V.2.1; Applied Biosystems, Weiterstadt, Germany) using an automated capillary sequencer (ABI 3730, Applied Biosystems). Primer pairs and PCR conditions are available on request. In group 2, we restricted analysis to those exons in which mutations have been found in this and previous studies (exons 3, 6–8, 10–14, 16 and 19).11,12 Where mutations were shown to have arisen de novo, we verified declared relationships by genotyping at 10 microsatellite loci for each patient and both parents. PCR products from one patient showing two sequence alterations in exon 10 were cloned in Escherichia coli (TOPO TA Cloning Kit; Invitrogen, Karlsruhe, Germany and One Shot, Invitrogen) to determine whether these alterations occurred on the same allele.
Structural analysis of novel SOS1 variations
The potential effects of novel SOS1 variations detected in this study were analysed in more detail using the known three‐dimensional structures of SOS114,15,19,20 and the computer program PyMOL (http://www.pymol.org). Figures were prepared using PyMOL and Adobe Photoshop (Adobe Systems Inc., USA).
Results
SOS1 variations and associated phenotypes
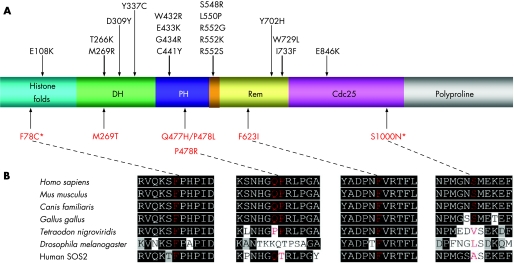
Overall, we found 18 different heterozygous SOS1 sequence variations predicting amino acid changes of the encoded SOS1 protein in 28 unrelated patients, including 25 sporadic cases and 3 patients with a positive family history for NS (table 1). Three of the observed sequence alterations represent possible polymorphisms: the variation c.1964C→T (P655L) which has previously been identified as a polymorphism12 was found in 4 of the 28 patients. In line with the assumption that this is a non‐pathogenic change, we also identified it in unaffected parents. One female patient with features of NS and significant ectodermal features (group 1C) was found to carry a novel sequence alteration, c.2999G→A (S1000N), inherited from her father, who lacked any clinical signs of NS. Based on this observation and the fact that S1000 is not highly conserved through evolution (fig 1), we regarded this variant as a probable neutral polymorphism. Another novel missense change, c.233T→G, affecting the evolutionarily conserved residue F78 (fig 1) was discovered in a male patient with many features of NS and in his mother. She was said to be clinically normal but could not be examined personally for the presence of possible minor signs of NS. Because we cannot be sure if F78C is a pathogenic mutation or polymorphism, we conservatively counted this patient among the SOS1 mutation‐negative group.
Table 1 Missense variants of SOS1.
| Exon* | Nucleotide change | Amino acid change | Domain | Pathogenic change or polymorphism | Number of affected people | ||||
|---|---|---|---|---|---|---|---|---|---|
| 3 | c.233T→G | F78C | HF | Possible polymorphism | 1 sporadic case† | ||||
| 6 | c.806T→G | M269R | DH | Pathogenic | 1 sporadic case | ||||
| 6 | c.806T→C | M269T | DH | Pathogenic | 1 sporadic case | ||||
| 7 | c.925G→T | D309Y | DH | Pathogenic | 1 sporadic case | ||||
| 10 | c.1294T→C | W432R | PH | Pathogenic | 1 sporadic case | ||||
| 10 | c.1297G→A | E433K | PH | Pathogenic | 1 sporadic case | ||||
| 10 | c.1300G→A‡ | G434R | PH | Pathogenic | 1 sporadic case | ||||
| 10 | c.1322G→A | C441Y | PH | Pathogenic | 1 sporadic case | ||||
| 10 | c.[1431G→T; 1433C→T]§ | [Q477H; P478L] | PH | Pathogenic | 1 sporadic case | ||||
| 10 | c.1433C→G | P478R | PH | Pathogenic | 1 sporadic case | ||||
| 10 | c.1654A→G | R552G | PH‐Rem linker | Pathogenic | 2 sporadic cases, 1 familial observation¶ | ||||
| 10 | c.1655G→A | R552K | PH‐Rem linker | Pathogenic | 1 sporadic case, 1 familial observation¶ | ||||
| 10 | c.1656G→T | R552S | PH‐Rem linker | Pathogenic | 1 sporadic case, 1 familial observation¶ | ||||
| 11 | c.1867T→A | F623I | Rem | Pathogenic | 1 sporadic case | ||||
| 12 | c.1964C→T | P655L | Rem | Polymorphism | 4 sporadic cases | ||||
| 13 | c.2104T→C | Y702H | Rem | Pathogenic | 1 sporadic case | ||||
| 16 | c.2536G→A | E846K | Cdc25 | Pathogenic | 4 sporadic cases | ||||
| 19 | c.2999G→A | S1000N | Cdc25 | Probable polymorphism | 1 sporadic case** |
HF, histone‐like folds; DH, Dbl homology domain; PH, pleckstrin homology domain; Rem, Ras exchanger motif.
Novel variants are printed in bold type.
*Exon 1 refers to the exon containing the ATG starting codon; †unaffected mother carries the same variant; ‡novel nucleotide exchange predicting a known missense mutation on protein level; §both sequence changes occurred de novo on the same allele; ¶affected mother–child duo; **unaffected father carries the same variant.
Figure 1 (A) Domain organisation of the human SOS1 protein. Histone‐like folds, Dbl homology (DH), pleckstrin homology (PH), helical PH‐Rem linker (orange), Ras exchanger motif (Rem), Cdc25 and polyproline domains are shown along with previously described Noonan syndrome‐associated mutations (black, top of the figure) and the novel missense changes identified in this study (red, bottom). Asterisks mark those variants also detected in one of the healthy parents. (B) Partial amino acid sequence alignments of human SOS1 with its orthologues of different species and human SOS2. Amino acids surrounding the four novel altered amino acids (indicated in red) are shown.
The remaining 15 SOS1 sequence alterations observed in 22 unrelated patients were regarded as pathogenic mutations; 10 nucleotide variations identified in our cohort have been established as causative mutations previously,11,12 whereas five are novel (table 1). Of the novel ones, mutation c.1300G→A has the same impact on the protein level as a previously published mutation (c.1300G→C; G434R).11 The remaining four sequence variations predict novel amino acid changes. One of these, c.806T→C (M269T), affects the same amino acid residue as the previously reported mutation M269R.11,12 It is likely that both exchanges of the neutral methionine by a polar residue have similar consequences on SOS1 protein function. The novel variations c.1433C→G (P478R) and c.1867T→A (F623I), detected in two sporadic cases, were regarded as causative mutations based on de novo occurrence, conservation (fig. 1) and function (see below). One affected person had two sequence changes, 1431G→T (Q477H) and 1433C→T (P478L). Cloning of the amplified product and sequencing of both parents demonstrated that both changes had occurred de novo on the same allele (not shown). De novo occurrence of the respective mutations was also confirmed in all other sporadic patients except two, for whom parental samples were unavailable. These two patients carried the known SOS1 mutations c.1654A→G (R552G) and c.2536G→A (E846K). In the three patients with a positive family history of NS, previously reported SOS1 mutations were found (table 1), which were in each case inherited from an affected mother. The nucleotide changes predicting F78C, Q477H, P478L/R, F623I and S1000N were not found in >150 population‐matched controls.
Considering only those cases with bona fide mutations, 18 of 85 patients of group 1 were found to have a SOS1 mutation. A causative SOS1 alteration was identified in 14 of 53 (26%) patients in group 1A, 4 of 11 (36%) patients in group 1C, but in none of the 21 patients with CFCS (group 1B). Only four (5%) people with SOS1 mutations were identified in group 2.
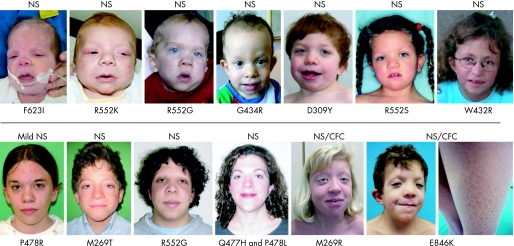
Clinically, most patients with SOS1 mutations exhibited a clear NS phenotype (fig 2). One patient from group 2, a girl carrying the de novo P478R mutation, only had very mild facial features of NS and short stature, and would not have met the published strict clinical criteria.17 Four patients with SOS1 mutations had been assigned to group 1C; three of them exhibited significant ectodermal symptoms resembling those found in CFCS, but had normal psychomotor and mental development in keeping with the diagnosis of NS, and the fourth was a young infant defying a clear‐cut diagnosis. Facial features of representative SOS1 mutation‐positive cases are illustrated in figure 2.
Figure 2 Facial appearance of 13 representative patients with Noonan syndrome (NS) carrying SOS1 mutations. The respective missense mutation is indicated below and the clinical assignment above each photograph. The female patient classified as having “mild NS” presented only with short stature and mild facial anomalies. Ichthyosiform skin changes in a patient carrying the mutation E846K are illustrated in the lower right image. Parental/guardian informed consent was obtained for publication of this figure.
For a more detailed phenotypic analysis, we included the 22 index patients with bona fide mutations and the three affected mothers with a confirmed SOS1 mutation. Comparison of clinical features in people carrying a SOS1 mutation with those of our cohort and three other cohorts of PTPN11 mutation‐positive patients21,22,23 revealed a similar spectrum of congenital heart defects, but a lower frequency of mental retardation or need for special education, easy bruising, and in males, cryptorchidism (table 2). These differences become even more obvious when combining findings of this study with data published recently.11,12 However, a significantly lower prevalence of short stature in patients with a SOS1 mutation, as indicated by previous studies,11,12 could not be confirmed in our cohort. Remarkably, patients with SOS1 mutations commonly had ectodermal manifestations, including keratosis pilaris of the face, sparse eyebrows, curly hair, and in one patient, ichthyosiform skin changes (fig 2). The incidence of ectodermal manifestations in patients with NS with PTPN11 mutations has not yet been well documented. By reviewing a cohort (n = 42) of clinically well documented PTPN11 mutation‐positive people mainly derived from our previous study,17 we could confirm a significantly higher prevalence of keratosis pilaris/hyperkeratotic skin and curly hair in patients with SOS1 mutations compared with those with PTPN11 alterations (58% vs 6% and 78% vs 34%, respectively). Moreover, ocular ptosis was observed more frequently in patients with NS with SOS1 mutations than in patients with a PTPN11 alteration (80% vs 54%).
Table 2 Clinical manifestations in patients with Noonan syndrome with SOS1 and PTPN11 mutations.
| Patients with: | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SOS1 mutations | PTPN11 mutations | |||||||||
| Present study | Tartaglia et al.12 | Roberts et al.11 | Total | Combined data† | ||||||
| Pulmonic stenosis | 20/25 | 10/16 | 11/15 | 41/56 (73%) | 125/171 (73%) | |||||
| Hypertrophic cardiomyopathy | 1/25 | 2/16 | 3/15 | 6/56 (11%) | 10/171 (6%) | |||||
| Atrial septal defect | 4/25 | 4/16 | 2/15 | 10/56 (18%) | 41/170 (24%) | |||||
| Thorax deformity | 17/24 | 16/16 | ND | 33/40 (83%)* | 110/171 (64%) | |||||
| Easy bruising | 3/25* | 5/16 | 5/15 | 13/56 (23%)* | 46/90 (51%)‡ | |||||
| Mental retardation/need for special education | 5/24* | 1/16 | 3/11 | 9/51 (18%)* | 71/164 (43%) | |||||
| Short stature (<3rd centile) | 13/25 | 2/15 | 4/13 | 19/53 (36%)* | 122/171 (71%) | |||||
| Cryptorchidism | 5/11* | ND | 5/10 | 10/21 (48%)* | 75/94 (80%) | |||||
Structural assessment of novel SOS1 variants
We analysed in more detail the potential effects of the novel predicted SOS1 variants F78C and F623I, as well as those of substitutions at residues Q477 and P478, using the known three‐dimensional structures of SOS1.14,15,19,20 The invariant residue F78 is located in the N‐terminal histone folds domain. This residue is predicted to interact indirectly with R552, the most commonly mutated residue, and substitutions of F78 may therefore have similar effects to those of mutations at R552. Q477 and P478 are not located in one of the known mutation clusters. We were unable to predict the precise consequences of substitutions of these residues based on structural modelling. Most likely, they do not directly affect the autoinhibited conformation. The highly conserved F623 residue is considered to play an important role in stabilising the Rem domain by forming an aromatic interaction with F958. Interestingly, substitution of F623 by glutamate in a SOS1 mutant protein composed of the Rem‐Cdc25 module has been shown to decrease exchange activity.24 Substitution of F623 by isoleucine presumably also abolishes aromatic interaction between F958 and F623 and may therefore lead to a reduced guanine nucleotide exchange activity of SOS1 (see supplementary information for further details; available online at http://jmg.bmj.com/supplemental).
Discussion
By screening genes encoding proteins involved in the Ras‐MAPK signalling pathway we have independently discovered SOS1 mutations in patients with classic features of NS (group 1A) and people with NS with more florid ectodermal symptoms and signs (group 1C). Taking these two subgroups of our core study population (group 1) together, our mutation detection rate reaches 28% among clinically well‐characterised patients who lacked mutations in the previously reported NS and CFCS genes. This proportion exceeds those in previously published cohorts (Tartaglia et al 17%; Roberts et al 21%).11,12 In aggregate, the two published studies and our study establish SOS1 as the second major gene for NS. A SOS1 mutation detection rate of 5% in group 2 corresponds to the low PTPN11 mutation rate of 18% in this heterogeneous cohort. It is evident that established clinical criteria for NS are valid for patients with SOS1 mutations, as only one patient with an SOS1 mutation did not meet strict diagnostic criteria. Thus, our findings do not support SOS1 as an important gene for people presenting with a mild or even atypical NS phenotype.
People with SOS1 mutations typically display a distinctive form of NS characterised by frequent ptosis, ectodermal symptoms and generally normal intelligence, an observation that has also been made by Tartaglia et al.12 However, the clinical spectrum is broad (as shown in fig 2) making it difficult to predict the genetic defect of a person with NS based on clinical appearance, thus we will not change our diagnostic strategy of first analysing PTPN11 in any patient with NS. In contrast to previous reports, we did not find a significantly lower prevalence of short stature in subjects with SOS1 mutations compared with those with PTPN11 mutations. Differences in patient selection may account for this apparent discrepancy, as several of our patients were recruited from a paediatric endocrinology department where they were seen for growth retardation.
One important finding of this study is the absence of SOS1 mutations in patients with the diagnosis of CFCS, who had tested negative for mutations in the established CFCS genes. Although the ectodermal manifestations in patients with SOS1 mutations are common and may be similar to those typically found in CFCS,12 the SOS1 phenotype in our study cohort is distinct from CFCS. The most important discriminating feature is the absence of significant mental retardation in patients with SOS1 mutations. Nonetheless, patients with SOS1 mutations may meet published criteria for CFCS.18 This brings into question the usefulness of the “CFC index” and emphasises the significance of intellectual functioning level in discriminating between NS and CFCS. In young children, however, clinical discrimination between these two conditions, particularly NS caused by SOS1 mutations, is difficult and may even be impossible. In such cases, determination of the molecular defect may have important prognostic implications.
SOS1 mutations associated with NS have been shown to result in a gain of function,11,12 consistent with the concept that NS and related disorders are caused by hyperactive Ras and aberrant activation of the B‐Raf‐MEK‐ERK pathway.25 However, to date, few SOS1 mutant proteins have been assessed functionally. This study provides the first hint that NS‐associated SOS1 mutations may not uniformly lead to increased GEF activity, but instead may cause a decrease in exchange activity of SOS1, as already suggested by Shannon and Bollag.26 The precise consequences of the F623I mutation remain to be determined by experimental means.
Taken together, our findings reinforce the concept that NS and CFCS scarcely overlap genotypically.27 The pathogenetic basis of this obvious genotype phenotype correlation remains to be elucidated. It has been speculated that the influence of Ras effector pathways other than B‐Raf‐MEK‐ERK or negative feedback mechanisms differentially affecting proximal and distal components may account for the phenotypic differences in patients with NS and CFCS.11,25 These emerging correlations between phenotypes and genotypes in this group of similar disorders is useful in defining new candidate genes for patients with NS or CFCS whose underlying genetic defect has yet to be discovered.
Key points
We identified mutations of SOS1 in 28% of patients with NS who had previously tested negative for mutations in PTPN11 and KRAS, but not in patients with cardio‐facio‐cutaneous syndrome.
Five novel mutations were detected, defining additional mutation hotspots and indicating possible new mechanisms of perturbed SOS1 protein function.
People with SOS1 mutations commonly show ocular ptosis, curly hair and hyperkeratotic skin, but they seem to have a lower frequency of mental retardation than patients with Noonan syndrome and mutations of PTPN11.
Electronic database information
Online Mendelian Inheritance in Man (OMIM) (for NS, CFCS and CS). http://www.ncbi.nlm.nih.gov/Omim/
Gene, for SOS1 genomic (accession number NC_000002.10) and cDNA (accession number NM_005633.2) sequences. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db = gene.
Protein Data Bank, for coordinates of DH‐PH‐Rem‐Cdc25 construct of hSOS1 (molecule B of code 1XD4), ternary Ras‐SOS1‐Ras•GppNHp complex (1NVW) and Ras‐SOS1 (1BKD). http://www.rcsb.org/pdb/home/home.do
Supplementary material is available online at http://jmg.bmj.com/supplemental.
Acknowledgements
We are grateful to the patients and families who participated in this study. We thank Angelika Diem and Inka Jantke for help with mutation screening. This work was supported by a grant from the German Research Foundation (DFG) to MZ.
Abbreviations
CFCS - cardio‐facio‐cutaneous syndrome
DH‐PH - Dbl homology–pleckstrin homology
GEF - guanine exchange factor
NS - Noonan syndrome
OMIM - Online Mendelian Inheritance in Man
Footnotes
Competing interests: None declared.
Parental/guardian informed consent was obtained for publication of figure 2.
Supplementary material is available online at http://jmg.bmj.com/supplemental.
References
- 1.Tartaglia M, Mehler E L, Goldberg R, Zampino G, Brunner H G, Kremer H, van der Burgt I, Crosby A H, Ion A, Jeffery S, Kalidas K, Patton M A, Kucherlapati R S, Gelb B D. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP‐2, cause Noonan syndrome. Nat Genet 200129465–468. [DOI] [PubMed] [Google Scholar]
- 2.Aoki Y, Niihori T, Kawame H, Kurosawa K, Ohashi H, Tanaka Y, Filocamo M, Kato K, Suzuki Y, Kure S, Matsubara Y. Germline mutations in HRAS proto‐oncogene cause Costello syndrome. Nat Genet 2005371038–1040. [DOI] [PubMed] [Google Scholar]
- 3.Niihori T, Aoki Y, Narumi Y, Neri G, Cave H, Verloes A, Okamoto N, Hennekam R C, Gillessen‐Kaesbach G, Wieczorek D, Kavamura M I, Kurosawa K, Ohashi H, Wilson L, Heron D, Bonneau D, Corona G, Kaname T, Naritomi K, Baumann C, Matsumoto N, Kato K, Kure S, Matsubara Y. Germline KRAS and BRAF mutations in cardio‐facio‐cutaneous syndrome. Nat Genet 200638294–296. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez‐Viciana P, Tetsu O, Tidyman W E, Estep A L, Conger B A, Cruz M S, McCormick F, Rauen K A. Germline mutations in genes within the MAPK pathway cause cardio‐facio‐cutaneous syndrome. Science 20063111287–1290. [DOI] [PubMed] [Google Scholar]
- 5.Schubbert S, Zenker M, Rowe S L, Boll S, Klein C, Bollag G, van der Burgt I, Musante L, Kalscheuer V, Wehner L E, Nguyen H, West B, Zhang K Y, Sistermans E, Rauch A, Niemeyer C M, Shannon K, Kratz C P. Germline KRAS mutations cause Noonan syndrome. Nat Genet 200638331–336. [DOI] [PubMed] [Google Scholar]
- 6.Allanson J E. Noonan syndrome. J Med Genet 1987249–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hennekam R C. Costello syndrome: an overview. Am J Med Genet C Semin Med Genet 200311742–48. [DOI] [PubMed] [Google Scholar]
- 8.Roberts A, Allanson J, Jadico S K, Kavamura M I, Noonan J, Opitz J M, Young T, Neri G. The cardio‐facio‐cutaneous (CFC) syndrome: a review. J Med Genet 2006 [DOI] [PMC free article] [PubMed]
- 9.Carta C, Pantaleoni F, Bocchinfuso G, Stella L, Vasta I, Sarkozy A, Digilio C, Palleschi A, Pizzuti A, Grammatico P, Zampino G, Dallapiccola B, Gelb B D, Tartaglia M. Germline missense mutations affecting KRAS Isoform B are associated with a severe Noonan syndrome phenotype. Am J Hum Genet 200679129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zenker M, Lehmann K, Schulz A L, Barth H, Hansmann D, Koenig R, Korinthenberg R, Kreiss‐Nachtsheim M, Meinecke P, Morlot S, Mundlos S, Quante A S, Raskin S, Schnabel D, Wehner L E, Kratz C P, Horn D, Kutsche K. Expansion of the genotypic and phenotypic spectrum in patients with KRAS germline mutations. J Med Genet 200744131–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roberts A E, Araki T, Swanson K D, Montgomery K T, Schiripo T A, Joshi V A, Li L, Yassin Y, Tamburino A M, Neel B G, Kucherlapati R S. Germline gain‐of‐function mutations in SOS1 cause Noonan syndrome. Nat Genet 20073970–74. [DOI] [PubMed] [Google Scholar]
- 12.Tartaglia M, Pennacchio L A, Zhao C, Yadav K K, Fodale V, Sarkozy A, Pandit B, Oishi K, Martinelli S, Schackwitz W, Ustaszewska A, Martin J, Bristow J, Carta C, Lepri F, Neri C, Vasta I, Gibson K, Curry C J, Siguero J P, Digilio M C, Zampino G, Dallapiccola B, Bar‐Sagi D, Gelb B D. Gain‐of‐function SOS1 mutations cause a distinctive form of Noonan syndrome. Nat Genet 20073975–79. [DOI] [PubMed] [Google Scholar]
- 13.Corbalan‐Garcia S, Margarit S M, Galron D, Yang S S, Bar‐Sagi D. Regulation of Sos activity by intramolecular interactions. Mol Cell Biol 199818880–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Margarit S M, Sondermann H, Hall B E, Nagar B, Hoelz A, Pirruccello M, Bar‐Sagi D, Kuriyan J. Structural evidence for feedback activation by Ras.GTP of the Ras‐specific nucleotide exchange factor SOS. Cell 2003112685–695. [DOI] [PubMed] [Google Scholar]
- 15.Sondermann H, Soisson S M, Boykevisch S, Yang S S, Bar‐Sagi D, Kuriyan J. Structural analysis of autoinhibition in the Ras activator Son of sevenless. Cell 2004119393–405. [DOI] [PubMed] [Google Scholar]
- 16.van der Burgt I, Berends E, Lommen E, van Beersum S, Hamel B, Mariman E. Clinical and molecular studies in a large Dutch family with Noonan syndrome. Am J Med Genet 199453187–191. [DOI] [PubMed] [Google Scholar]
- 17.Zenker M, Buheitel G, Rauch R, Koenig R, Bosse K, Kress W, Tietze H U, Doerr H G, Hofbeck M, Singer H, Reis A, Rauch A. Genotype‐phenotype correlations in Noonan syndrome. J Pediatr 2004144368–374. [DOI] [PubMed] [Google Scholar]
- 18.Kavamura M I, Peres C A, Alchorne M M, Brunoni D. CFC index for the diagnosis of cardiofaciocutaneous syndrome. Am J Med Genet 200211212–16. [DOI] [PubMed] [Google Scholar]
- 19.Boriack‐Sjodin P A, Margarit S M, Bar‐Sagi D, Kuriyan J. The structural basis of the activation of Ras by Sos. Nature 1998394337–343. [DOI] [PubMed] [Google Scholar]
- 20.Sondermann H, Nagar B, Bar‐Sagi D, Kuriyan J. Computational docking and solution x‐ray scattering predict a membrane‐interacting role for the histone domain of the Ras activator son of sevenless. Proc Natl Acad Sci U S A 200510216632–16637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tartaglia M, Kalidas K, Shaw A, Song X, Musat D L, van der Burgt I, Brunner H G, Bertola D R, Crosby A, Ion A, Kucherlapati R S, Jeffery S, Patton M A, Gelb B D. PTPN11 mutations in Noonan syndrome: molecular spectrum, genotype‐phenotype correlation andphenotypic heterogeneity. Am J Hum Genet 2002701555–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Musante L, Kehl H G, Majewski F, Meinecke P, Schweiger S, Gillessen‐Kaesbach G, Wieczorek D, Hinkel G K, Tinschert S, Hoeltzenbein M, Ropers H H, Kalscheuer V M. Spectrum of mutations in PTPN11 and genotype‐phenotype correlation in 96 patients with Noonan syndrome and five patients with cardio‐facio‐cutaneous syndrome. Eur J Hum Genet 200311201–206. [DOI] [PubMed] [Google Scholar]
- 23.Jongmans M, Sistermans E A, Rikken A, Nillesen W M, Tamminga R, Patton M, Maier E M, Tartaglia M, Noordam K, van der Burgt I. Genotypic and phenotypic characterization of Noonan syndrome: new data and review of the literature. Am J Med Genet A 2005134165–170. [DOI] [PubMed] [Google Scholar]
- 24.Hall B E, Yang S S, Boriack‐Sjodin P A, Kuriyan J, Bar‐Sagi D. Structure‐based mutagenesis reveals distinct functions for Ras switch 1 and switch 2 in Sos‐catalyzed guanine nucleotide exchange. J Biol Chem 200127627629–27637. [DOI] [PubMed] [Google Scholar]
- 25.Bentires‐Alj M, Kontaridis M I, Neel B G. Stops along the RAS pathway in human genetic disease. Nat Med 200612283–285. [DOI] [PubMed] [Google Scholar]
- 26.Shannon K, Bollag G. Sending out an SOS. Nat Genet 2007398–9. [DOI] [PubMed] [Google Scholar]
- 27.Kratz C P, Schubbert S, Bollag G, Niemeyer C M, Shannon K M, Zenker M. Germline mutations in components of the ras signaling pathway in Noonan syndrome and related disorders. Cell Cycle 200651607–1611. [DOI] [PubMed] [Google Scholar]