Abstract
Background
The prevalence of lactase persistence is high in Saudi Arabia.
Objective
To identify a DNA variant for the lactase persistence/non‐persistence trait in adult Arabs in Saudi Arabia.
Methods
We sequenced DNA from 432 anonymous neonatal blood donors from five different regions of Saudi Arabia to cover the 400 bp region surrounding the previously identified lactase persistence/non‐persistence variant C/T−13910 residing in intron 13 of the MCM6 gene.
Results
Two anonymous blood donors carried the C/T−13910 genotype. One variant, T/G −13915, residing 5 bp upstream of the C/T−13910 variant, was present in 332 of 432 (76.9%) of the neonatal samples, compatible with previous prevalence figures of lactase persistence in urban Saudi populations. Determination of disaccharidase activities in 25 intestinal biopsy samples showed a highly significant correlation between lactase activity and the T/G−13915 genotypes (p<0.001; Fisher exact test) as well as between the L:S ratio and the aforementioned genotypes (p<0.001; Fisher exact test).
Conclusion
The T/G−13915 variant is the founder mutation of lactase persistence in an urban Saudi population. The results obtained here have implications for genetic testing of adult‐type hypolactasia and to analysis of human evolution, the origin of cattle domestication and migrations of the populations in the Arabian peninsula.
Keywords: DNA‐variant, lactase persistence, lactase non persistence, lactase activity, Urban Saudi population
Adult‐type hypolactasia (lactase non‐persistence; primary lactose malabsorption; OMIM 223100) is a genetically determined normal phenomenon characterised by the downregulation of lactase enzyme activity after weaning. Some human populations have retained high lactase activity throughout life that makes them able to digest milk (lactase persistence). Lactase persistence is most common in populations of northern European descent and in some nomadic populations.1 A single‐nucleotide polymorphism (SNP) C→T, residing 13910 bp upstream of the lactase gene (LCT) was first shown to be associated with lactase persistence/non‐persistence and to be correlated with the downregulation of lactase activity in intestinal biopsy specimens in both paediatric and adult populations.2,3,4,5 Molecular epidemiological studies in many European, Asian, African American, and some African and Asian populations2,4,6,7,8 have shown that the frequency of the C/C−13910 genotype, reflecting low lactase activity in adulthood, is in agreement with the previously published prevalence figures of adult‐type hypolactasia.1 Expression of the lactase mRNA in human intestinal mucosa is downregulated by the C−13910 allele during childhood,5 whereas the T−13910 allele is responsible for the increased transcription of LCT.3,5 In vitro expression studies carried out with the C/T−13910 variant have shown that the mutant T−13910 allele is responsible for increased LCT promoter activity.9,10 Electrophoretic mobility shift assays have shown strong interaction between the T−13910 allele and the Oct1 nuclear‐binding factor.11
Some other variants close to the most common variant C/T−13910 have recently been identified in nomadic pastoralist and non‐pastoralist groups from Africa and the Middle East using the indirect lactose tolerance test (LTT).12,13 Of these newly identified variants, the G/C−14010 variant, present in several small pastoralist groups from Kenya and Tanzania, has shown significant association with lactase persistence using the indirect LTT.12 Another variant, T/G−13915, has been found in Bedouin populations in Saudi Arabia and Jordan and in several pastoralist and non‐pastoralist groups from Cameroon, Ethiopia, Kenya and Sudan, but its role in lactase persistence/non‐persistence has remained unclear. C/G−13907 has been found in the Afro‐Asiatic Beja population in Kenya, Sudan and Ethiopia.12,13 In addition, a rare polymorphism, T/C−13913, has been reported from some cases in Cameroon, Sudan, Ethiopia and Bedouin population in Saudi Arabia.13 Functional studies using dual luciferase reporter assays have shown that the mutant C−14010, G−13907 and G−13915 alleles increase LCT promoter expression.12 However, Ingram et al13 did not find any interaction between the G−13915 and C−13913 alleles and Oct1, despite their location in the Oct1 binding site.
In 1975, Cook and Al‐Torki reported that 85.7% of Bedouins and 87.5% of urban Saudi Arabians are lactose tolerant by the LTT.14 In a search for causal variants for lactase persistence/non‐persistence we sequenced a 400 bp region surrounding the major C/T−13910 variant in anonymous neonatal DNA samples from Saudi Arabia. The significance of the variant was verified by determining disaccharidase activities and lactase:sucrase ratio (L:S) of intestinal biopsy specimens of patients originating from the same population.
Materials and methods
Participants
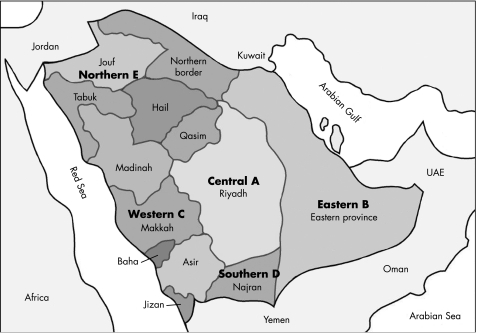
In total, 432 DNA samples isolated from anonymous neonatal blood samples covering five different regions: the (A) Central, (B) Eastern, (C) Western, (D) Southern and (E) Northern regions of Saudi Arabia (fig 1) were included in this study. Also included were 36 intestinal biopsy specimens taken from adult patients undergoing endoscopic examination for a variety of gastrointestinal problems in King Faisal Hospital, Riyadh. Both studies were approved by the ethics committee of the King Faisal Specialist Hospital and Research Centre, Riyadh. All patients or their relatives gave informed consent.
Figure 1 The five regions of Saudi Arabia from which the anonymous blood donor samples were collected.
Genotyping
DNA was isolated and whole‐genome amplification was performed from dried blood spots as previously described.15 DNA from intestinal biopsy specimen was isolated using standard procedures. The 400 bp PCR fragment surrounding the previously identified C/T−13910 variant2 was analysed by direct sequencing (primer sequences available upon request) from both datasets covering all the aforementioned variants.12,13
Assay of intestinal disaccharidases
The activities of lactase, sucrase and maltase were determined from the duodenal biopsies using a method based on that of Dahlqvist.16 All disaccharidase measurements were carried out by one researcher (AS) at the King Faisal Specialist Hospital and Research Centre. Samples with low maltase (<100 U/g of protein) and/or saccharase activity (<40 U/g of protein) were excluded from the study (n = 11). A false‐positive result of adult‐type hypolactasia is obtained if the biopsy is taken above the postbulbar duodenum, as variation in lactase activity can only be detected below the postbulbar duodenum and in jejunum, depending on the lactase persistence/non‐persistence status. We used a cut‐off point of 10 U/g of protein for lactase activity and <0.2 for L:S ratio to determine adult‐type hypolactasia.4,5,17
Results
The prevalence of lactase genotypes in samples from newborns from the five regions in Saudi Arabia are shown in table 1. Of the 432 neonatal samples, 332 (76.9%) had the hypothetical lactase persistence G −13915 allele. In addition,the most common variant, C/T−13910,2 was identified in two samples. No other variants, including G/C−14010, C/G−13907 and T/C−13913, were found. Bearing in mind the inaccuracy of the LTT18 the frequency of the T/G−13915 genotypes (T/T−13915 associated with adult‐type hypolactasia and T/G−13915 and G/G−13915 with lactase persistence) is reasonably in agreement with previously published figures of lactase persistence in urban Saudi populations.14 There were only two people among the anonymous blood donors who had the most common variant C/T−13910: one was heterozygous for both the lactase‐persistence genotypes T/G−13915 and C/T−13910, and the other had the hypolactasia genotype T/T−13915 and the lactase‐persistence genotype C/T−13910. These results show that the C/T−13910 variant is very rare in Saudi Arabia, and support the existence of different DNA variants of lactase persistence in Arab and African populations.7,12,13
Table 1 Number of genotypes from DNA isolated from blood spots for the T/G –13915 and C/T−13910 variants in five different regions of Saudi Arabia.
| Region | Cases, n | T/G −13915 | C/T−13910 | ||||
|---|---|---|---|---|---|---|---|
| T/T, n (%) | T/G, n (%) | G/G, n (%) | C/C, n (%) | C/T, n (%) | T/T, n (%) | ||
| A (Central) | 90 | 24 (27) | 23 (24) | 43 (48) | 90 (100) | 0 (0) | 0 (0) |
| B (Eastern) | 82 | 15 (18) | 33 (40) | 34 (41) | 82 (100) | 0 (0) | 0 (0) |
| C (Western) | 86 | 14 (16) | 33 (38) | 39 (45) | 85 (99) | 1 (1)* | 0 (0) |
| D (Southern) | 92 | 21 (23) | 36 (39) | 35 (38) | 92 (100) | 0 (0) | 0 (0) |
| E (Northern) | 82 | 26 (32) | 26 (32) | 30 (36) | 81 (99) | 1 (1)† | 0 (0) |
*Genotype of this patient for each SNP: T/G and C/T.
†Genotype of this patient for each SNP: T/T and C/T.
We examined associations between the T/G−13915 genotypes and disaccharidase activities and L:S ratio in 25 intestinal‐biopsy specimens. Sequencing of the DNA from these specimens (n = 36) resulted in the identification of the T/G−13915 variant in all analysed samples; no other DNA variants were found. The genotypes, lactase activities and L:S ratios of the biopsy‐sample specimens are shown in table 2. There were eight biopsies homozygous for the T/T−13915 genotype, which all had very low lactase activity (mean 4.8 U/g of protein, range 3 to 6) and L:S ratio (mean 0.08, range 0.04 to 0.11 ) compatible with the hypothesis that T−13915 is the original allele of adult‐type hypolactasia. Biopsy specimens from 15 subjects heterozygous for T/G−13915 showed mean lactase activity of 19.7 U/g of protein (range 12 to 37) and L:S ratio >0.12, and specimens from two subjects homozygous for the G/G−13915 genotype had a high lactase activity (32 and 39 U/g of protein, respectively) and high L:S ratios, consistent with lactase persistence.2,3,4,5,17,19 A trimodal distribution of lactase activity was seen; there was a significant correlation between lactase persistence and non‐persistence genotypes (p<0.01; Fisher exact test) and between L:S ratio and the aforementioned genotypes (p<0.001; Fisher exact test). These results do not exclude the existence of other possible functional variants outside the 400 bp region.
Table 2 Correlation of the T/G−13915 genotypes with disaccharidase activities and L:S‐ratio.
| Patient | T/G−13915 genotypes | Enzyme activity | |||
|---|---|---|---|---|---|
| 100–700 | 40–250 | 20–140 | <0.2 | ||
| Maltase, U/g protein | Saccharase (S), U/g protein | Lactase (L), U/g protein | L:S (R) | ||
| 1 | T/G | 228 | 65 | 17 | 0.27 |
| 3 | T/G | 292 | 51 | 30 | 0.59 |
| 4 | T/G | 364 | 93 | 15 | 0.16 |
| 6 | T/G | 223 | 63 | 29 | 0.45 |
| 7 | T/G | 159 | 67 | 16 | 0.24 |
| 8 | T/G | 140 | 46 | 12 | 0.26 |
| 9 | T/T | 193 | 64 | 5 | 0.08 |
| 10 | G/G | 226 | 93 | 32 | 0.35 |
| 11 | T/G | 148 | 45 | 26 | 0.58 |
| 12 | T/T | 177 | 50 | 5 | 0.10 |
| 13 | T/T | 154 | 55 | 5 | 0.09 |
| 14 | T/T | 160 | 45 | 5 | 0.11 |
| 18 | T/G | 171 | 47 | 14 | 0.3 |
| 19 | G/G | 138 | 40 | 39 | 0.98 |
| 20 | T/G | 227 | 83 | 16 | 0.19 |
| 21 | T/G | 238 | 84 | 37 | 0.44 |
| 22 | T/T | 188 | 59 | 6 | 0.10 |
| 23 | T/G | 239 | 64 | 27 | 0.41 |
| 29 | T/G | 181 | 44 | 12 | 0.26 |
| 30 | T/G | 343 | 120 | 14 | 0.12 |
| 32 | T/T | 356 | 104 | 4 | 0.04 |
| 33 | T/T | 232 | 66 | 5 | 0.07 |
| 34 | T/T | 192 | 45 | 3 | 0.08 |
| 35 | T/G | 190 | 43 | 17 | 0.41 |
| 36 | T/G | 200 | 57 | 14 | 0.24 |
Discussion
Sequencing of the DNA of a total of 25 subjects from Saudi Arabia enabled us to identify one single nucleotide polymorphism T→G residing 13915 bp upstream of the lactase gene (LCT) that shows excellent correlation with lactase enzyme activity and L:S ratio in intestinal biopsy specimens. Significant correlation of the T/G−13915 genotypes with lactase activity and L:S ratio in the intestinal biopsy specimens demonstrated in this study show that this variant is associated with lactase persistence trait. The lactase activities in this study were of the same range as those obtained with the most common variant C/T−13910.2,3,4,5 Based on the results obtained in this study determination of the T/G−13915 variant can be used as a primary screening test for adult‐type hypolactasia in urban Saudi populations. Identification of only one major variant of lactase persistence demonstrates the homogeneity of the current population: the prevalence of the T/T−13915 genotype was 23.1% among the anonymous blood donors and 31% in the patients undergoing endoscopy. The higher proportion of subjects with lactase non‐persistence in the endoscopy group can be explained by selection bias; low lactase activity predisposes to abdominal symptoms and leads to affected people seeking medical care.20
The inaccuracy of the LTT in the diagnosis of adult‐type hypolactasia18 and the poor correlation between indirect diagnostic tests and the symptoms caused by lactose‐containing milk21,22 has made it difficult to verify the significance of the DNA variants in lactase persistence/non‐persistence in different populations.7,12,13 Diagnosis of adult‐type hypolactasia is based on the measurement of lactase, sucrase and maltase activities and the lactase and sucrase (L:S) ratio in intestinal biopsies. A recent study of a paediatric population showed 100% specificity and 93% sensitivity of the C/T−13910 genotypes detecting adult‐type hypolactasia from intestinal biopsy sample specimens from patients >12 years of age.4 Although endoscopy is a routine diagnostic method in industrialised countries, it is a technically demanding and invasive method which is unpleasant for the patient and unsuitable for conditions outside a medical facility. The prevalence of the T/G−13915 variant has been found to be much lower in Middle Eastern and African than in urban Saudi populations.13 This may be a result of poor genotype–phenotype correlation of the lactase persistence/non‐persistence trait,20 a relatively small number of analysed individuals and a more mixed ethnic background of non‐pastoralist versus pastoralist groups.
Available data on the distribution of the persistent G−13915 allele in African and Arab populations12,13 suggests that the lactase‐persistence trait was most likely brought from Africa to the Arabian Peninsula.23,24 Enrichment of only one persistent allele covering most of the Arabian Peninsula is most likely due to ancient selection, which has been further strengthened by recent founder effects due to the tradition of consanguineous marriages in Saudi populations and to genetic drift. However, owing to multiple migrations between Africa and Arabia one cannot exclude the reverse possibility that the G−13915 allele was imported from the Middle East to Eastern African populations.23,24,25
Acknowledgements
We are grateful for the participants who gave their samples to the study. We thank Antti Kotamies for statistical analyses. This study was supported by the Helsinki University Hospital Research Funding, Helsinki, Finland, The Sigrid Jusélius Foundation, Helsinki Finland and the King Faisal Specialist Hospital and Research Centre.
Abbreviations
LCT - lactase gene
L:S - lactase:sucrase ratio
LTT - indirect lactose tolerance test
OMIM - Online Mendelian Inheritance in Man
SNP - single‐nucleotide polymorphism
Footnotes
Competing interests: None declared.
References
- 1.Sahi T. Genetics and epidemiology of adult‐type hypolactasia. Scand J Gastroenterol 199429(Suppl)7–20. [DOI] [PubMed] [Google Scholar]
- 2.Enattah N S, Sahi T, Savilahti E, Terwilliger J D, Peltonen L, Järvelä I. Identification of a variant associated with adult‐type hypolactasia. Nat Genet 200230233–237. [DOI] [PubMed] [Google Scholar]
- 3.Kuokkanen M, Enattah N, Oksanen A, Savilahti E, Orpana A, Järvelä I. Transcriptional regulation of the lactase‐phlorizin hydrolase gene by polymorphisms associated with adult‐type hypolactasia. Gut 200352647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasinperä H, Savilahti E, Enattah N S, Kuokkanen M, Tötterman N, Lindahl H, Järvelä I, Kolho K L. A genetic test which can be used to diagnose adult‐type hypolactasia in children. Gut 2004531571–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rasinperä H, Kuokkanen M, Kolho K ‐ L, Enattah N S, Lindahl H, Savilahti E, Orpana A, Järvelä I. Transcriptional downregulation of the lactase (LCT) gene during childhood. Gut 2005541658–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bersaglieri T, Sabeti P C, Patterson N, Vanderploeg T, Schaffner S F, Drake J A, Rhodes M, Reich D E, Hirschhorn J N. Genetic signatures of strong recent positive selection at the lactase gene. Am J Hum Genet 2004741111–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mulcare C A, Weale M E, Jones A L, Connell B, Zeitlyn D, Tarekegn A, Swallow D A, Bradman N, Thomas M G. T allele of a single‐nucleotide polymorphism 13.9 kb upstream of the lactase gene (LCT) (C‐13.9kbT) does not predict or cause the lactase‐persistence phenotype in Africans. Am J Hum Genet 2004741102–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Myles S, Bouzekri N, Haverfield E, Cherkaoui M, Dugoujon J M, Ward R. Genetic evidence in support of a shared Eurasian ‐ North African dairying origin. Hum Genet 200511734–42. [DOI] [PubMed] [Google Scholar]
- 9.Troelsen J T, Olsen J, Møller J, Sjöström J. An upstream polymorphism associated with lactase persistence has increased enhancer activity. Gastroenterology 20031251686–1694. [DOI] [PubMed] [Google Scholar]
- 10.Olds L C, Sibley E. Lactase persistence DNA variant enhances lactase promoter activity in vitro: functional role as a cis regulatory element. Hum Mol Genet 2003122333–2340. [DOI] [PubMed] [Google Scholar]
- 11.Lewinsky R H, Jensen T G, Möller J, Stensballe A, Olsen J, Troelsen J T. T‐13910 DNA variant associated with lactase persistence interacts with Oct‐1 and stimulates lactase promoter activity in vitro. Hum Mol Genet 2005143945–3953. [DOI] [PubMed] [Google Scholar]
- 12.Tishkoff S A, Reed F A, Ranciaro A, Voight B F, Babbitt C C, Silverman J S, Powell K, Mortensen H M, Hirbo J B, Osman M, Ibrahim M, Omar S A, Lema G, Nyambo T B, Ghori J, Bumpstead S, Pritchard J K, Wray G A, Deloukas P. Convergent adaptation of human lactase persistence in Africa and Europe. Nat Genet 20073931–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ingram C J E, Elamin F F, Mulcare C A, Weale M E, Tarekegn A, Raga T O, Bekele E, Elamin F M, Thomas M G, Bradman N, Swallow D M. A novel polymorphism associated with lactose tolerance in Africa: multiple causes for lactase persistence? Hum Genet 2007120779–788. [DOI] [PubMed] [Google Scholar]
- 14.Cook G C, al‐Torki M T. High intestinal lactase concentrations in adult Arabs in Saudi Arabia. BMJ 19753135–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al‐Sayed M, Imitiaz F, Alsmadi O A, Rashed M S, Meyer B F. Mutations underlying 3‐hydroxy‐3‐methylglutaryl CoA lyase deficiency in the Saudi population. BMC Med Genet 2006786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahlqvist A. Assay of intestinal disaccharidases. Scand J Clin Lab Invest 198444169–172. [DOI] [PubMed] [Google Scholar]
- 17.Kuokkanen M, Myllyniemi M, Vauhkonen M, Helske T, Kääriäinen I, Karesvuori S, Linnala A, Härkönen M, Järvelä I, Sipponen P. A biopsy‐based quick test in the diagnosis of duodenal hypolactasia in upper gastrointestinal endoscopy. Endoscopy 200638708–712. [DOI] [PubMed] [Google Scholar]
- 18.Arola H. Diagnosis of hypolactasia and lactose malabsorption. Scand J Gastroenterol 1994202(Suppl)26–35. [DOI] [PubMed] [Google Scholar]
- 19.Maiuri L, Rossi M, Raia V, Paparo F, Coletta S, Mazzeo F, Breglia A, Auricchio S. Morphological method for the diagnosis of human adult type hypolactasia. Gut 1994351042–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anthoni S R, Rasinperä H A, Kotamies A J, Komu H A, Pihlajamäki H, Kolho K L, Järvelä I. Molecularly defined adult‐type hypolactasia among working age people with reference to milk consumption and gastrointestinal symptoms. World J Gastroenterology 2007131230–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carroccio A, Montalto G, Cavera G, Notarbatolo A. Lactose intolerance and self‐reported milk intolerance: relationship with lactose maldigestion and nutrient intake. J Am Coll Nutr 199817631–636. [DOI] [PubMed] [Google Scholar]
- 22.de Vrese M, Stegelmann A, Richter B, Fenselau S, Laue C, Schrezenmeir J. Probiotics ‐ compensation for lactase insufficiency. Am J Clin Nutr 200173(Suppl)421–429. [DOI] [PubMed] [Google Scholar]
- 23.Richards M, Rengo C, Cruciani F, Gratrix F, Wilson J F, Scozzari R, Macaulay V, Torroni A. Extensive female‐mediated gene flow from Sub‐Saharan Africa into near eastern Arab populations. Am J Hum Genet 2003721058–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kivisild T, Reidla M, Metspalu E, Rosa A, Brehm A, Pennarun E, Parik J, Geberhiwot T, Usanga E, Villems R. Ethiopian mitochondrial DNA heritage: tracking gene flow across and around the gate of tears. Am J Hum Genet 200475752–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanotte O, Bradley D G, Ochieng JW Verjee Y, Hill E W, Rege J E. African pastoralism: genetic imprints, origins and migrations. Science 2002296336–339. [DOI] [PubMed] [Google Scholar]