Abstract
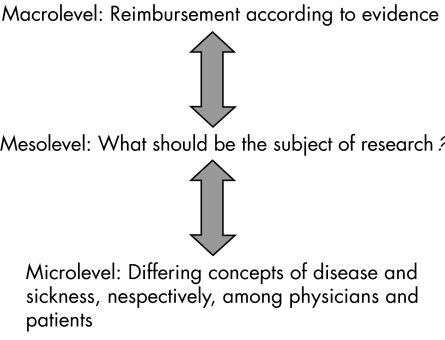
Decisions in healthcare are made against the background of cultural and philosophical definitions of disease, sickness and illness. These concepts or definitions affect both health policy (macro level) and research (meso level), as well as individual encounters between patients and physicians (micro level). It is therefore necessary for evidence‐based medicine to consider whether any of the definitions underlying research prior to the hierarchisation of knowledge are indeed compatible with its own epistemological principles.
Initially, a search on “disease”, “sickness” and “illness” and “EbM” (evidence‐based medicine) was performed in the databases Medline and EMBASE (table 1). All texts, including textbooks (English, German, French, Spanish and Italian) on EbM, were scrutinised for explicit or implicit definitions of disease or sickness and illness. In the literature on EbM, few explicit definitions could be found. After clarifying the epistemological basis of EbM, various concepts of disease, sickness or illness are presented, followed by an exploration of whether these are in accordance with the implicit epistemological rationale of EbM.
Table 1 Results of searches on evidence‐based medicine, health and disease, etc. (date of initial searches: 16–20 May 2005; additional searches: 12–19 Dec 2005).
| Source | Term 1* | Term 2 | Term 3 | Results |
|---|---|---|---|---|
| Medline | ebm† | Disease | 3000 | |
| ebm | Disease | Model | 130 | |
| ebm | Disease | Concept | 73 | |
| ebm | Disease | Definition | 44 | |
| ebm | Illness | 672 | ||
| ebm | Illness | Definition | 15 | |
| ebm | Sickness | 43 | ||
| ebm | Sickness | Definition | 0 | |
| ebm | Malady | 2 | ||
| ebm | Health | Definition | 114 | |
| EMBASE | ebm | Disease | Definition | 687 |
| ebm | Health | Definition | 776 |
*Terms were connected by AND unless otherwise indicated.
†Term 1 was “evidence‐based medicine” (ebm). Searches with “EbM” or “EBM” instead of “evidence‐based medicine” yielded a greatly decreased number of hits.
It becomes clear that, in constantly demanding the continuous revision of scientific results, transferability/particularising, transparency and the integration of patients' preferences, EbM itself is not able to form a single universal, or rather, general definition of disease. Yet, EbM has to rely on the results of research, implicitly drawing on notions of health and disease, and therefore requires a general definition of disease in order to prioritise further research. EbM thus seems to be caught in an aporia. On the one hand it must presuppose a definition of disease, while on the other hand those practising EbM know that such a universally valid definition cannot be generated.
Should EbM reflect on concepts of health and disease, and would it arrive at a definite concept?
Evidence‐based medicine has become a well‐accepted method in organising all kinds of medical knowledge as well as health promotion interventions. It is characterised by “the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients and populations” integrating “individual clinical expertise and patients' choice”.1 On account of the fact that EbM affects healthcare at all levels, there needs to be a clarification as to which concept of disease EbM should rely upon (fig 1).
Figure 1 Interdependence of levels of healthcare.
In this context, EbM is subjected to several challenges at the three levels of healthcare delivery:
When should the EbM process begin? Some hold that any issue addressed by those visiting a physician—whether they be termed patients or consumers—pertains to EbM: for example, even issues such as the behaviour of children at school. Yet, advocates of this pragmatic view do not reflect on a concept of disease, but rather include anything that is interpretable in terms of health and disease into EbM.
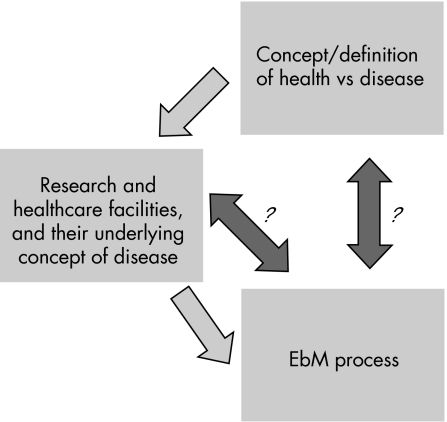
What concepts of disease have been coined by the research which EbM is to organise? Concepts of health and disease always exert a normative influence on forms of medical practice and the choice of research questions.2 Thus, EbM needs to be clear about these norms (fig 2).
If patients' choice constitutes one of the three columns of practising EbM, to what extent should research be guided by patients' preferences? If, for instance, they request that studies on Viagra be undertaken, should resources be spent on investigations on impotence (meso level)? The question remains as to how EbM could protect itself from engaging in research on the basis of such misconceptions of health and disease. Consumers' input into research agendas is far from systematic, and all too often patients' charities end up fulfilling the role of lobbying for a particular disease or health problem”.3
Does the special position of the randomised clinical trial (RCT) essentially require a biomedical model at the core of EbM?
Figure 2 Evidence‐based medicine (EbM) primarily relies on pre‐established concepts of diseases that have induced certain research projects and the establishment of healthcare facilities. EbM, however, then enters into a process of continuous modification of the concept of disease and henceforth has to reflect on a concept of disease in order to direct further research activities.
In this paper, we will show that EbM has neither explicitly adopted nor may implicitly adopt a single concept of disease. Although an affinity of EbM may exist towards the adoption of operational concepts of disease on account of their fitting into pharmacotherapeutic RCTs, this does not, from our point of view, constitute the core concept. Rather, the major trait of EbM is the coherent and transparent hierarchisation of medical knowledge with regard to the primary question phrased in the initial encounter between patient and physician—be it, for instance, preventative, diagnostic or therapeutic—in combination with clinical experience and patients' preferences. We thus conclude that, on account of the epistemological core concepts of continuous revision and transferability, there cannot be a single concept of disease fitting into EbM.
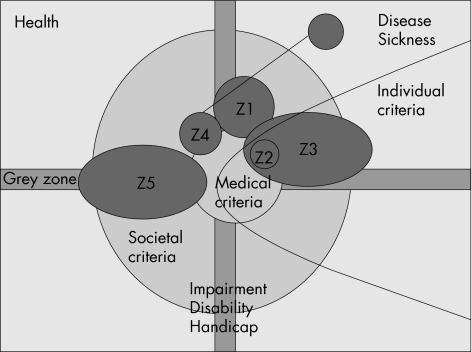
Figure 3 The so‐called landscape of health, disease and impairment shows a set of exemplarily selected conditions (Z1–Z5) that can be located on different levels of criteria‐shaping concepts of disease and health. The way in which the three concentric circles are arranged does not preclude any ranking according to their importance or exigency, but merely indicates a range of higher generalisability towards the centre. Moreover, as the figure shows, we also argue that there is a grey zone—that is, a zone where healthy and sick may not clearly be separated, blurring the discriminatory power of all three types of criteria. In addition, we draw attention to the fact that disease does not coincide with impairment. The ellipse from the right indicates that not all conditions considered as disease in any of the three perspectives—for example, Z1 or Z4—are reimbursed regardless of the system of healthcare financing.
Rather, EbM must face a threefold dilemma.
EbM has to presuppose or construct a general concept of disease, yet at the same time, due to its major traits of transferability and continuous revision, any concept of disease remains under the caveat of relative validity.
The concept of disease‐guiding research (meso level) is not necessarily congruent with the concept of disease distinguishing reimbursable from non‐reimbursable interventions (macro level) such as lifestyle and wellness (medicine). If EbM is consulted for the construction of a catalogue of reimbursable healthcare services (macro level)—that is, prioritisation—it must be clear that EbM cannot simply passively draw on research that is already underway, but must also exert an active influence on such research. Therefore, it needs a clear‐cut definition of what is to be considered a disease.4,5 EbM, nonetheless, may also be a valuable instrument in forming a hierarchy among different therapeutic options of lifestyle medicine or wellness. “A treatment may be effective at preventing something as important as coronary heart disease, or as trivial as premature greying of the hair.” But “there is no logical relationship between proof of effectiveness and the urgency/importance of the condition for which the intervention is effective”.6 Subsequently, it should be evident that, for instance, medical and pedagogical questions need to be, if possible, treated separately. Not all children demonstrating bad behaviour or failure in school are beneficially categorised as a “medical deviation”. EbM has to draw on other criteria in order to guide further research.
If EbM seriously strives to encompass clinicians' expertise and patients' preferences (micro level), it must come to terms with at least two varying concepts of disease that are shaped by differing perceptions of diagnostics and treatment, and so on.7
Excursus: What concept of EbM forms the basis of our line of argument?
In order to develop our line of reasoning, we must clarify two crucial aspects concerning the concept of EbM and the role of the RCT.
First, there are fundamentally three different ways of defining the relationship of EbM to pre‐EbM medicine:
EbM is what we always did (relationship of continuity).
EbM is a paradigm shift (relationship of discontinuity or dichotomy).8,9
EbM is something new, but not totally different (relationship of qualified continuity)—for example, as Haynes puts it: EbM augments pre‐EbM medicine.10
Yet, none of the three positions are as such correct. We argue that any relationship that can be found between two ways of thinking needs a criterion along which it can be determined. Otherwise, it is solely “hopes, fears, and mixed record of EBM …”.11 In as much as the body of research and the way of carrying out research is considered, EbM is not totally new. Both EbM and pre‐EbM medicine are abstract at the level of the individual patient. But in establishing a “decision‐making technology that would eschew unsystematic and so‐called “intuitive” methods of individual clinical experience in favour of a more scientifically rigorous approach”,12 EbM certainly represents a “paradigm shift” in medical thinking.
Secondly, among both its proponents and its opponents, EbM is not interpreted in a consistent manner. On these grounds, we would compare two modes of interpretation. In the first, EbM is a method whose best evidence is always the RCT regardless of the question, a somewhat dogmatic implementation as Porta13 points out. Such an understanding of EbM favours pharmacotherapeutic interventions above others, and thus implicitly relies on an operational concept of disease.
The second way of interpreting the accomplishments of EbM differentiates levels of evidence according to the initial question, thus resulting in a variety of hierarchies.14 Or as Haynes attests: “Different methods … for exploring different questions.” Together with Porta,13 we favour a more “common sense approach” to the principles of EbM rather than a “dogmatic implementation” with regard to many questions that could not aptly be operationalised in an RCT or to the regimen of rare diseases that could not be investigated by means of RCTs.
It is against the backdrop of both EbM as a new method for managing different claims of truth and organising the communication of research results, and the perception that the initial question determines the level of evidence that we seek an apt concept of disease. This search for a definition does not seem to be of mere academic interest, but is rather additionally “reflected in medical practice”.2 Furthermore, it has an impact on all three levels of medical practice.15 We will examine both textbooks and journal publications on concepts of disease and health, and its relationship with EbM. If this analysis does not yield a satisfying result, we will subsequently address other concepts of disease, assessing their congruence with the epistemological principles of EbM.
Is an in‐depth debate on the definition of health or disease to be found in the literature on EbM?
Most of the English text books on EbM, obtained with the help of various search strategies on the internet, did not contain any discussion concerning health and disease.16,17,18,19,20,21,22,23,24,25,26,27 Indeed, only two dedicated a passage to the topic.28,29 The same proves true for German text books on how to practise EbM, with the exception of Zielinski, who, however, only reproduces a definition of disease provided by the German Social Court in 1972 as “an irregular condition of the body or the mind that causes the need for a treatment alone or in connection with incapacity to work or that leads to incapacity of work”.30,31,32,33,34,35 Text books from France, Spain and Italy were also surveyed, most of which were translations of original English books,36,37 and therefore did not yield any additional aspects.
Gray quotes the definition of disease offered by the Shorter Oxford English Dictionary as a “condition of the body, or of some part of organ of the body in which its functions are disturbed or deranged”.28 He then gives the example of distinguishing hypochondria from medically unexplainable physical symptoms. It would seem that the notion of disease is too strongly related to bodily aspects. Would such a notion fit into a definition of disease based on the epistemological principles of EbM? Jenicek29 admits that there are “historical and heterogeneous perceptions of disease”. He then delineates that the modern definition of disease relies on a melange of scientifically and epistemologically diverse criteria such as morphological (otitis media), biochemical (porphyria), signs (measles), symptoms (anxiety) and more. Subsequently, he postulates that four criteria must be met in order to define a status as “disease”: (1) being unusual for a given subject (illness), for a health professional (disease) and for a patient's entourage (sickness); (2) altering a patient's future (prognosis); (3) requiring some form of intervention; and (4) seeming evident, when intervention is available.
However, both textbooks neither show awareness that the EbM process is a kind of clash of different concepts of disease, nor arrive at a clear separation of health and disease.
After running through titles and abstracts from all lists, only one article exhibited a thorough discussion of the issue. Vineis tried to connect evidence to a concept of disease. In doing so, he delineated a concept of disease differentiating four fields: monothetic versus polythetic disease, and monothetic versus polythetic agent(s) of the disease.38 He restricted this to the basis of clinical signs and symptoms. Moreover, he explained that the different notions of disease lie on a continuum. Vineis thus presented four models of disease rather than an integrative concept. His approach does not aid the investigation of the initial question as to how health and disease can be distinguished.
It is obvious that EbM in its daily practice is shaped by those implicit notions of health and disease or sickness underpinning research and coined by patients and physicians, and thus implicitly guiding resource allocation. Although there is some awareness of the problem that EbM must come to terms with a definition of disease, a solution is far from being found. Further there is, no reflection on the clash of varying concepts of disease contributing to the questions asked in the EbM process.
What are the major epistemological principles of EbM with which a definition of disease should comply?
There remains relatively little research on the epistemology of EbM: “As I shall show there are many open questions to the foundations of EBM.”39 Within this article, we may only portray the epistemological rationale of EbM to the extent to which it is required in finding congruent concepts of disease and health.
Principally, it should be clear that EbM is located in the context of utilisation‐focused evaluation in the Popperian sense rather than in the context of explanation or substantiation,40 even though new knowledge might be established by means of systematic reviews or meta‐analyses, both of which are integral concepts of EbM. Yet, all this places EbM into the realm of a hermeneutical science rather than a “natural” science.41 And from this perspective, we set out to define its characteristics as a primarily hermeneutical tool. Its basic epistemological rationale is therefore continuous revision of knowledge in an ongoing process, transparency of the hermeneutical criteria and particularising.
In contrast to generally held beliefs and pre‐EbM medicine, EbM does not maintain that any results are universally valid. First of all, there is the caveat of “currently available knowledge”.
Secondly, and even more importantly, as the EbM process always begins with a question from an individual patient–physician encounter, this always includes a consideration of the transferability/particularising of knowledge.
Thirdly, knowledge is assorted along the line of probabilism—that is, whether it is more likely that a treatment may work. Thus again, EbM does not maintain that a treatment is based on a universal truth, but rather holds a scepticist view that it is currently the best available intervention.
Which concept of disease would suit the epistemological rationale of EbM? The manifold definitions of disease cannot thoroughly be presented and discussed here, owing to the fact that they result from rival theoretical frameworks and can be categorised in a variety of ways.2 For the most part, a division into naturalist (objectivist) and non‐naturalist (normativist) concepts is accepted. This is combined with a second division along the lines of a universal or relativist claim.42 However, this further division only makes sense from the viewpoint of normativist approaches, as any naturalist concept implicates a claim for universal validity. A further criterion of the differentiation of concepts of health and disease is whether the concept is positive, such as the definition provided by the World Health Organisation in 1946, or merely negative, for instance, when health is solely considered as the absence of disease. We will elucidate the different concepts and then critically assess whether they match the epistemological basis of EbM.
Naturalist concept of disease
The major trait of this concept of disease is that only “objective” criteria are considered valid when separating healthy and sick individuals. Hence, any human attribute that can be categorised in measurable parameters and subsequently departs >2SDs from the mean is considered sick. Hypertension is a good example. Yet, in the case of cavities for example, we are faced with the problem that these would not be considered a disease due to the fact that the majority of a population suffer from cavities. Furthermore, value judgements would have to constantly adapt to changing statistical averages. In order to solve the problems of statistical averaging, Boorse43,44 introduced the device of teleological function statements. Healthy denotes that an individual's “mode of functioning conforms to the natural kind of organism” of a certain species. Thus, he introduces the higher level biological goals of reproduction and survival of the species.
At first sight, the biomedical concept of disease might be seen to match EbM in substantially facilitating the carrying out of RCTs. Yet, this represents a misunderstanding of EbM. It is not the dominant position of the RCT in the hierarchy of evidence, but the primordial clinical question that guides the EbM process. Moreover, all types of naturalist concepts carry the epistemological flaw of having to define what should be considered in the framework of disease beforehand via value judgement. A thorough critique of the normativist turn within Boorse's writings is well laid out by Fulford.45 And as the term naturalist indicates, these positions fit into the Catholic way of arguing (Thomas of Aquino): what is a deviation in “nature” is morally and now medically a deviation. Moreover, there are positions that claim that Boorse's concept might be gender biased when it comes to the impact of reproduction on males' and females' health.46 Thus, the naturalist concept with its claim of universal validity does not adhere to EbM's principles of transferability and particularising., 2,47
Normativist concepts of disease
These concepts share the conviction that a concept of disease or sickness is not primarily determined by “objective” criteria, but by values. Positions differ in how far the concept should be considered to be the result of a process of consensus in a society or even solely subjective.48,49 Still others maintain that any concept of disease is actually the result of a negotiation between patient and physician, implicating that there is a continuously fluctuating concept of disease.50 With regard to the claim of validity, Margolis as well as Nordenfelt argue that concepts of disease only function in their context—that is, they are of relative validity, whereas Fedoryka sets out to (re)establish a theory of a universal concept of disease.51,52
Looking at these concepts from the perspective of EbM, any merely subjective concept would be of no help to research that also draws on different measurable parameters in order to find the best treatment. Those concepts that rely on “consensus” may hold for different societies; these too must, according to the basic principles of EbM, be subjected to the criteria of transferability and particularising.
EbM in a dilemma: universally measurable parameters versus societally defined concepts of geographical and chronological limitation
As could be shown, there are no objective criteria in itself that are sufficient in separating healthy from diseased conditions, but rather they are all man‐made in so far as it is our need to separate the states of health and disease in order to plan research and substantiate decisions of allocation such as reimbursement or incapacity to work. 4,41 Thus, there is both ontologically and epistemologically a precedence of society's values that, however, combine descriptive and normative elements in order to obtain a feasible concept of disease. To put it into the words of Virchow, one of the founders of the pathophysiologic view of medicine: “What we call disease is solely an abstract concept with the help of which we separate particular phenomena of daily life from all others, without there being such a separation in nature itself.”53 (“Was wir Krankheit nennen, ist nur eine Abstraction ... womit wir gewisse Erscheinungscomplexe ... des Lebens aus der Summe der uebrigen heraussondern, ohne dass in der Natur selbst eine Sonderung bestaende.”) There are objective criteria in so far as they can be exactly measured, yet epistemologically they are also based on other values such as reproduction43,44 and length of life.54
And as any concept of health or disease is sensitive to the emergence of new methods and techniques, EbM should be clear about its influence on the concepts of health and disease.2
Even the so‐called “objective” criteria that we purposively named “medical” in order to question whether they are indeed as “objective” as they seem to be are of relative validity when it comes to history and situation—for example, hypertension.
EbM, with its principles of contextuality and historicity (continuous revision), does not allow for any singular universal concept of disease, yet it must find a common denominator in order to be applicable when defining research projects. These may include both medical and societal criteria, and even subjective criteria in so far as EbM may ask for individual assessment of patients' conditions. Yet, as EbM comprises the continuous revision of knowledge as an integral component, it may even ask whether the dichotomy of health and disease in the structuralist sense of disjunct opposites blocks other views on the phenomena of divergence from healthy states. This, however, would complicate both research and allocation. EbM would thus rely on the currently adopted dichotomy of health and disease for feasibility, but may stay open for an alteration in the concept of health and disease.
In returning to the different levels of healthcare, macro, meso and micro levels, it is clear that EbM must deal with different concepts of disease on all levels. This finally leads to an aporia for EbM in so far as it wishes to encompass patients' perspectives on health and disease, as well as the physicians' concepts that have been guiding their work and research.
Conclusions
The literature on EbM did not provide any indications that EbM itself has developed a concept of disease on the basis of its epistemological rationale. In fact, only scarce publications on EbM deal with the issue of defining disease. Yet, EbM is forced to rely on research that has been initiated by specific concepts of disease. It is therefore essential that EbM should consider how its epistemological principles match the concepts of disease in the research which it assembles and appraises. Moreover, it must draw a line between medicine and other fields of professional help such as psychology or pedagogy.
Faced with this endeavour, EbM finds itself in a threefold dilemma:
EbM must construct a general concept of disease, yet at the same time, due to its major traits of transferability and continuous revision, EbM also places all concept of disease under the caveat of relative validity.
Furthermore, the concept of disease guiding research might not be congruent with the concept of that which is reimbursable. EbM can give advice on the most effective treatment in questions of lifestyle and wellness although these interventions are not considered reimbursable.
In the individual encounter between physician and patient, EbM would allow for telling a patient that he or she is not sick in the sense of the knowledge currently available, or the society's concept of disease, while the patient nonetheless has the right to feel ill. On this basis, neither action nor reimbursement would be justified.
Abbreviations
EbM - evidence‐based medicine
RCT - randomised clinical trial
Footnotes
iWe use the terms “concept” and “definition” of health or disease interchangeably throughout this article. We do not enter the discussion on the relationship between concept and model(s) of disease (cp Hofmann, p 228).
iiWe would like to affirm at this point that we are certainly in favour of patients'/consumers' involvement in research, as we are aware that patients can indeed push for very valuable questions to be studied. It should however be clear that this requires an agenda detailing how and which patients' preferences are to be incorporated into the planning and conducting of research projects (fig 3 ).
iiiThis also holds for pre‐EbM medicine, though with EbM the situation is tapered, since here research from different backgrounds is collected.
ivWe refer to “traditional” medicine that relies on individual clinical experience and/or on non‐structured or subjectively structured bodies of medical knowledge. Pre‐EbM medicine seems to be the term with the least pejorative connotations.
vWe cannot enter the whole debate on philosophy of science with the controversy of critical rationalism.
viWe are aware that this is a new approach to the philosophical evaluation of EbM in relation to medical knowledge. We are currently working on a contribution to the different concepts of EbM held by adherents and opponents.
viiWe admit that nowadays pathophysiologists and, especially, pharmacologists also stress that there are mechanisms that are not universal but are unique to age groups, ethnic groups, etc.
viiiIn how far the so‐called biomedical and naturalist concepts of disease rather favour a paternalistic mode of practising medicine should be subject to further research, as EbM is discussed in the context of shared decision making.
ixA further discussion of the ethical implications of differing concepts of disease would be an interesting topic, yet cannot be analysed on the grounds of our initial question.
xThe German language only has the term “Krankheit,” in contrast to the English concepts of disease, sickness and illness.
xiAt this point, we cannot problematise Virchow's concept of “nature”.
Competing interests: None.
References
- 1.Sackett D L, Rosenberg W M C, Gray J A M.et al Evidence based medicine: what it is and what it isn't. BMJ 199631271–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hofmann B. Complexity of the concept of disease as shown through rival theoretical frameworks. Theor Med 200122211–236. [DOI] [PubMed] [Google Scholar]
- 3.Liberati A, Vineis P. Defining a proper background for discussing evidence‐based medicine. In: Meulen RT, Biller‐Andorno N, Lenk C, et al, eds. Evidence‐based practice in medicine and health care. A discussion of ethical issues. Berlin: Springer, 2005
- 4.Bobbert M. Die Problematik des Krankheitsbegriffs und der Entwurf eines moralisch‐informativen Krankheitsbegriffs im Anschluss an die Moralphilosophie von Alan Gewirth. Ethica 20008405–440. [Google Scholar]
- 5. In: Mazouz N, Werner MH, Wiesing U, eds. Krankheitsbegriff und Mittelverteilung. Beiträge zum Gesundheitsmanagement Bd. 8. Baden‐Baden: Nomos Verlagsgesellschaft, 2004
- 6.Rogers W. Evidence‐based medicine and equity: the exclusion of disadvantaged groups. In: Meulen RT, Biller‐Andorno N, Lenk C, et al, eds. Evidence‐based practice in medicine and health care. A discussion of ethical issues. Berlin: Springer, 2005
- 7.Vos R, Willems D, Houtepen R. Coordinating the norms and values of medical research, medical practice and patient worlds. The ethics of evidence‐based medicine in “boundary fields of medicine”. In: Meulen RT, Biller‐Andorno N, Lenk C, et al, eds, Evidence‐based practice in medicine and health care. A discussion of ethical issues. Berlin: Springer 200587–95.
- 8.Guyatt C H. Evidence‐based medicine. ACP J Club 1991114A16. [PubMed] [Google Scholar]
- 9.Evidence‐based working group Evidence‐based medicine. JAMA 19922682420–2425. [DOI] [PubMed] [Google Scholar]
- 10.Haynes B. What kind of evidence is it that evidence‐based medicine advocates want health car providers and consumers to pay attention to? BMC Health Serv Res. 2002;2: 3, http://www.biomed.com/1472‐6963/2/3 [DOI] [PMC free article] [PubMed]
- 11.Timmermans S, Mauck A. The promises and pitfalls of evidence‐based medicine. Health Aff 20052418–28. [DOI] [PubMed] [Google Scholar]
- 12.Goldenberg M J. Evidence‐based ethics? On evidence‐based practice and the “empirical turn” form normative bioethics. BMC Med Ethics. 2005;6, 11 http://www‐biomedcentral.com/1472‐6939/6/11 [DOI] [PMC free article] [PubMed]
- 13.Porta M. Is there life after evidence‐based medicine? J Eval Clin Pract 200410147–152. [DOI] [PubMed] [Google Scholar]
- 14.Phillips B, Ball C, Sackett D.et alOxford Centre for evidence‐based medicine levels of evidence. Oxford: Centre for evidence‐based medicine levels of evidence, 2001, http://www.cebm.net/downloads/Oxford_CEBM_Levels_5.rtf (accessed 2 Mar 2005)
- 15.Emanuel E J. Gesundheitsversorgung im Alter—die Perspektive eines liberalen Kommunitarismus. In: Marckmann G, ed. Gesundheitsversorgung im Alter. Zwischen ethischer Verpflichtung und ökonomischem Zwang. Stuttgart, NY: Schattauer, 2003203–218.
- 16. Moyer VA, Elliott EJ, eds. Evidence‐based pediatrics and child health. London: BMJ Books, 2004
- 17.Greenhalgh T.Einfuehrung in die Evidence‐based medicine. Kritische Beurteilung klinischer Studien als Basis einer rationalen Medizin. 2. vollstaendig ueberarbeitete Auflage. Aus dem Englischen von Beifuss K, Bartens W Bern, Goettingen, Toronto: Verlag Hans Huber, 2003
- 18. Friedlander DJ, ed. A framework for clinical practice. Evidence‐based medicine. New York: Lange Medical Books/McGraw‐Hill, 2002
- 19. Stout CE, Hayes RA, ed. The evidence‐based practice. Methods, models, and tools for mental health professionals. Hoboken, NJ: John Wiley and Sons, 2001
- 20.Straus S E, Lancaster T.Practising evidence‐based primary care. Hrsg von Straus S. Abingdon. Oxon: Radcliffe Medical Press, 1999
- 21.Sackett D L, Richardson W S, Rosenberg W.et alEvidence‐based medicine. How to practice and teach EBM? New York: Churchill Livingstone, 1997
- 22.Badenoch D, Heneghan C.Evidence‐based medicine toolkit. London: BMJ Publishing Group, 2005
- 23.Brettle A.Finding the evidence for practice—a workbook for health professionals. New York: Churchill Livingstone, 2004
- 24. Geyman JP, Deyo RA, Ramsey SD, eds. Evidence‐based clinical practice. Woburn, MA: Butterworth‐Heinemann, 2000
- 25.Mayer D.Essential evidence‐based medicine. Cambridge: University Press, 2005
- 26.McKibbon A, Eady A, Marks S.PDQ: evidence based principles and practice. Hamilton: Decker, 1999
- 27.Glasziou P, Del Mar C, Salisbury J.Evidence‐based medicine workbook. Finding and applying the best research evidence to improve patient care. London: BMJ Books, 2003
- 28.Gray J A M.Evidence‐based healthcare. Edinburgh: Churchill Livingstone, 2001
- 29.Jenicek M.Foundations of evidence‐based medicine. Boca Raton: The Parthenon Publishing Group, 2003
- 30.Ollenschlaeger G, Bucher H C, Donner‐Banzhoff N.et alKompendium evidenzbasierte Medizin. Clinical evidence concise. Aus dem Englischen von Hermann M, Joas A, Stahl K Bern, eds Goettingen, New York: Verlag Hans Huber, 2004
- 31. Antes G, Bassler D, Forster J, eds. Evidenz‐basierte Medizin. Praxis‐Handbuch für Verstaendnis und Anwendung der EBM. Stuttgart, NY: Georg Thieme Verlag, 2003
- 32.Perleth M, Antes G (Hrsg) Evidenzbasierte Medizin. Wissenschaft im Praxisalltag. 3. aktualisierte und erweiterte Auflage. Muenchen: Urban und Vogel, 2002
- 33.Kunz R, Ollenschlaeger G, Raspe H.et alLehrbuch Evidenzbasierte Medizin in Klinik und Praxis. Köln: Deutscher Ärzte‐Verlag, 2000
- 34.Fischer M R, Bartens W.Zischen Erfahrung und Beweis. Medizinische Entscheidungen und evidence‐based medicine. Bern: Hans Huber, 1999
- 35.Zielinski W.Evidence‐based medicine: Einsatzmoeglichkeiten in der stationären Versorgung. Schriften der Gesellschaft für sozialen Fortschritt e. V Bd 25. Berlin: Duncker und Humblot, 2002
- 36.Marchetta F, Iovine R, Bobbio M. In: Esercizi per una medicina basata sull'evidenza, edn. italiana. Torino: Centro Scientifico, 1999
- 37.Bobbio M, Sackett D L.La medicina basata sulle evidenze scientifiche: come practicare e insegnare l'EBM. 2nd edn. riv. e ampliata, edn. italiana. Torino: Centro Scientifico, 2001
- 38.Vineis P. Evidence‐based medicine and ethics: a practical approach. J Med Ethics 200430126–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ashcroft R E. Current epistemological problems in evidence‐based medicine. In: Meulen RT, Biller‐Andorno N, Lenk C, et al, eds. Evidence‐based practice in medicine and health care. A discussion of ethical issues. Berlin: Springer, 200578–85.
- 40.Popper K.Die Logik der Forschung. Tübingen: JCB Mohr, 1934
- 41.Gerber A, Lungen M, Lauterbach K W. Evidence‐based medicine is rooted in protestant exegesis. Med Hypothes 2005641034–1038. [DOI] [PubMed] [Google Scholar]
- 42.Werner M H. Krankheitsbegriff und Mittelverteilung: Beitrag zu einer konservativen Therapie. In: Mazouz N, Werner MH, Wiesing U, eds. Krankheitsbegriff und Mittelverteilung. Beiträge zum Gesundheitsmanagement Bd. 8. Baden‐Baden: Nomos Verlagsgesellschaft, 2004139–156.
- 43.Boorse C. On the distinction between disease and illness. Philos Public Aff 1975549–68. [Google Scholar]
- 44.Boorse C. Health as a theoretical concept. Philos Sci 197744542–573. [Google Scholar]
- 45.Fulford K W M. What is (mental) disease? “An open letter to Christopher Boorse. ” J Med Ethics 20012780–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Problems with the biomedical model of health. 2003. http://web.aanet.com.au/cmcdonald/Articles/Problems%20with%20the%20biomedical%20model%20of%20health.htm (accessed 2 Mar 2005)
- 47.Edwards A, Elwyn G.Evidence‐based patient choice. Inevitable or impossible? Oxford: Oxford University Press, 2001
- 48.Margolis J. The concept of disease. J Med Philos 19761238–255. [Google Scholar]
- 49.Hesslow G. Do we need a concept of disease. Theor Med. 1993;14:1–14. doi: 10.1007/BF00993984. [DOI] [PubMed] [Google Scholar]
- 50.Lanzerath D, Honnefelder L. Krankheitsbegriff und aerztliche Anwendung der Humangenetik. In: Duewell M, Mieth D, eds. Ethik in der Humangenetik. Die neueren Entwicklungen in der genetischen Frühdiagnostik aus ethischer Perspektive. Tuebingen: Francke, 199851–77.
- 51.Nordenfelt L. On the nature of health: an action‐theoretic approach. In: Engelhardt HT Jr, Spicker SF, eds. Philosophy and medicine. Dordrecht: D Reidel, 198726 [Google Scholar]
- 52.Fedoryka K. Health as a normative concept: towards a new conceptual framework. J Med Philos 199722143–160. [DOI] [PubMed] [Google Scholar]
- 53.Virchow R.Handbuch der speciellen pathologie und therapie. Bd. 1: allgemeine stoerungen. Erlangen: Enke, 1854
- 54.Lenk C. Therapie und enhancement. Ziele und grenzen der modernen medizin. In: Siep L, et al, eds, Muensteraner bioethische schriften. Vol 2. Muenster: Lit Verlag 2001