Abstract
This paper introduces the medical factual matrix as a new and potentially valuable tool in medical ethical analysis. Using this tool it demonstrates the idea that a defined medical intervention can only be meaningfully declared futile in relation to a defined goal(s) of treatment. It argues that a declaration of futility made solely in relation to a defined medical intervention is inchoate. It recasts the definition of goal futility as an intervention that cannot alter the probability of the existence of the important outcome states that might flow from a defined intervention. The idea of value futility and the extent of physician obligations in futile situations are also addressed. It also examines the source of substantive conflicts which commonly arise within the doctor‐patient relationship and the ensuing power relations that operate between doctor and patient when questions of futility arise.
Futility is a key concept in clinical decision making. It often operates implicitly, contributing to the final clinical decision reached. There are cases, however, where it becomes explicit. In these cases it can become contentious.1,2 In this paper, I set out a conceptual model of futility derived from the fact–value distinction of Hume,3 which aims to clarify the concept of futility, identify areas where substantive conflicts might arise and locate the value judgements that are still missing in the concept of medical futility as it is presently understood. On the basis of this model, I introduce the idea of the medical factual matrix (MFM) and argue, inter alia, that declarations of medical futility require an explicit declaration of the defined goal of treatment in relation to which the defined intervention is deemed futile.
Background
There have been many attempts to encapsulate the concept of futility in a clinically useful way. Tomlinson and Brody4 examined the rationale of do‐not‐attempt‐resuscitation (DNAR) orders. Where such orders were made on the basis of “no medical benefit”, they argued that a doctor could unilaterally withhold medical treatment on grounds of futility. Where this rationale rested on the patient's quality of life, they proposed that the patient's value set should be accessed before a DNAR order could be made.4 They defend the power of doctors to determine treatment by appealing to the principles of physician integrity and physician non‐maleficence.5 In this journal Wreen6 recently identified several problems surrounding the scope of medical discretion created if we accept this approach.
As part of the continuing search for a defensible basis for the unilateral withholding of treatment by doctors, Waisel and Truog7 proposed a concept of physiological futility, which arises when a medical treatment cannot achieve its physiological objective. They argue that the power of the concept of physiological futility lies in the fact that it does not require the doctor to access the patient's value set.
This has been challenged, inter alia, by Schneiderman et al,8 who do not regard the concept as being free of value judgements. They preferred an approach based on the concepts of quantitative futility and qualitative futility.9 They defined quantitative futility as arising “when physicians conclude (either through personal experience, experiences shared with colleagues, or consideration of reported empiric data) that in the last 100 cases, a medical treatment has been useless”. Qualitative futility arises in circumstances where a medical treatment “merely preserves permanent unconsciousness or ... fails to end total dependence on intensive medical care”.
Brody and Halevy10 provide two other concepts in the arena: “imminent demise futility” (the patient will die before discharge regardless of the intervention) and “lethal condition futility” (the patient has an underlying disease that is not compatible with long‐term survival, regardless of the intervention, even if he or she could survive to be discharged from the current hospitalisation).
These and similar approaches have been criticised as being ambiguous and complex, and as granting more power than necessary to the doctor.10,11 Empirical and consensus‐based approaches have not resolved the problems that surround the use of the concept of futility in clinical decision making.12
The medical factual matrix: a model for medical futility
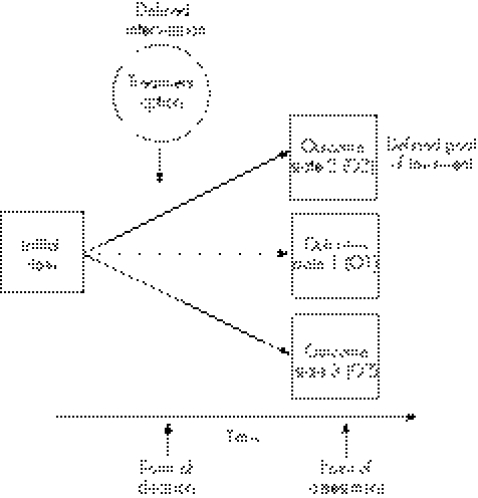
The idea of a medical factual matrix (MFM) is grounded in the fact–value distinction first described as the naturalist fallacy by Hume in his Treatise on human nature.3 We will need to explore this before moving on to the thesis of this article in the section The hidden valuation—defining the goal of treatment. The MFM requires three elements: an initial state, a defined intervention and a defined goal of treatment (see fig 1).
Figure 1 Base medical factual matrix (MFM).
Description and definitions
Importantly, the base MFM incorporates only the medical facts. In the spirit of Hume, the value elements are added later. The MFM incorporates a factual description of the medical situation of the patient, both at present and that possible in the future, as a set of “medical states”. A single medical state is a description of the physical and mental state of the patient at a moment in time. The medical states are discrete, such that the patient can occupy only one such state at any time. Thus there are a vast number of such possible states. Each state is distinct from the other and they are therefore mutually exclusive.
The medical data required to describe these states will vary from patient to patient and will depend on the circumstances of the case. For some medical states some of the medical parameters might overlap, although the states themselves may be separate.
For the purposes of clinical decision making and the MFM, only a few important states (or groups of states) need to be considered. We will consider the initial state of the patient and some of the important possible outcome states that might arise after the point of decision.
The “initial state” is the medical factual situation of the patient at a time just before the “point of decision”. The point of decision is the time when the decision on whether to deliver the “treatment option” is made. The treatment option is a medical interventioni that may or may not be delivered depending on the conclusion reached at the point of decision. The “point of assessment” is a material point in time after the point of decision.
An outcome state is a possible medical state of the patient at the point of assessment. Many outcome states could potentially exist in a real case. The set of possible outcome states therefore comprises all the outcome states that might arise at the point of assessment of the patient.
Next, consider the connections between the initial state and the outcome states. As viewed from the point of decision, these connections are in fact probabilities, each of which carries a degree of uncertainty about its precise value. Within the limits of uncertainty, these linking probabilities declare the chance that as time progresses, the initial state will arrive at one or other of the outcome states.
Uncertainty is inherent in the quantification of these linking probabilities. This uncertainty extends to the degree of effect of the defined intervention on the linking probabilities. It is important to recognise that some of the complexity in the concept of futility derives from this factual uncertainty.
Over time, the patient moves from the initial state through several intermediate medical states, eventually arriving at one of the possible outcome states. With time elapsing, these probabilities collapse to a single path that is taken by the course of events to arrive at the final outcome state (not marked in fig 1).ii Patients and doctors view the MFM from a point in time antecedent to the final outcome state, whereas lawyers generally view the MFM retrospectively from the position of the final outcome state.
The “defined goal (or goals) of treatment” is the outcome state (or states), which the defined intervention is aimed at making more probable.
An example
For the sake of exposition, consider three possible outcome states: outcome 1 (O1), outcome 2 (O2) and outcome 3 (O3). Let O1 be the hypothetical situation that would arise if the defined treatment was not given. In reality, the content of this medical state would partly depend on the time between the point of decision and the point of assessment. O1 is an important outcome state for the purposes of futility because it defines the zero net benefit gain point.
Let O2 be an outcome state where the patient's medical situation is improved relative to O1 and let O3 be an outcome state where the patient's medical situation is worse relative to O1. At this stage in the analysis, “worse” does not connote moral or value judgements, but is only a description of the medical state. O3 must be included because there are recognised medical interventions that can result in a worse medical state for the patient. Examples include assisted suicide, which is legal in some jurisdictions, cases of healthy‐limb amputation13 and complications arising from treatments given.
For a concrete example of this, see the case example in table 1.
Table 1 Case example.
| Initial state | Hypoglycaemic diabetic coma |
| Treatment option | 50 ml 50% dextrose given intravenously |
| Time gap between point of decision and assessment of outcome states | Short |
| Outcome state 1 | Hypoglycaemic diabetic coma without brain damage |
| Outcome state 2 | Recovery of consciousness without any brain damage and with normoglycaemia |
| Outcome state 3 | Continuing coma secondary to hypoglycaemic brain damage but with normoglycaemia |
Goal futility
Let us start by defining goal futility in relation to the defined intervention.10,11,12 Let the defined intervention be goal futile if it cannot alter the magnitude of the linking probabilities. If the linking probabilities cannot be modified, then the defined intervention is de facto goal futile. It cannot affect the course of events. Goal futility is linked to the degree of effect of the defined intervention on the linking probabilities. This differs from quantitative futility, which is associated with the magnitude of the linking probabilities.
I argue that goal futility defined in this way can ground the unilateral withholding of treatment.14 This is because the value of the defined goal simply does not enter the equation. This is not a common situation, however, because if there is any potential modification of the linking probabilities by the defined intervention, this invites valuation of the MFM, effectively excluding this definition of goal futility.6,15
The nature of the factual uncertainty surrounding the linking probabilities means that the doctor is usually (although not always) better placed than the patient to determine whether the defined intervention can possibly alter the probabilities connecting the initial state and the outcome states.
In this view futility is not predicated on previous experiences; our only concern is regarding the present facts.16 Our previous experiences do contribute to the assessment of futility to the extent that they contribute to the assessment of the linking probabilities. Their contribution to the valuation of the MFM is open to debate. It is to this valuation of the MFM that we now turn.
Valuation of the MFM
The next step is to build a values dimension on the base MFM. Virtually all the elements of the MFM are open to valuation. These include the net benefit gain relative to O1 for each potential outcome state, the cost of the medical intervention and the route taken over time to reach a particular outcome state. The overall net benefit is the integral sum of the valuation of the various elements of the MFM, taking into account the magnitude of the linking probabilities and their relationship to the defined intervention.iii
It is important to realise that multiple valuations of the base MFM may operate. These can be:
Evaluation in different dimensions, in particular moral valuation and financial valuation. All dimensions are valued by each actor, but the main valuation encountered by patients in the National Health Service (NHS) is the moral valuation. However, recently, fee payers and their representatives—for example, the National Institute of Clinical Excellence in the UK—have increased the weight placed on questions of cost effectiveness.17
The deployment of different value sets in a particular dimension. For example, in the moral dimension available value sets include those of the patient (where competent), the relatives, general medical professional values, the particular professional and personal values of the doctor concerned, the values of other stakeholders such as the National Institute of Clinical Excellence,18 researchers19 and, on occasion, the courts.v
Such valuations can vary as the perspective of a particular party alters. For example, a patient may view a particular intervention differently when viewed antecedent to its delivery compared with the same intervention viewed retrospectively.
A potential source of substantive conflict is that each party can take a different view of the same defined intervention and base MFM elements. For example, an NHS patient with a health problem and a Hohfeld claim right20 to NHS care will probably value the same base MFM differently from that of an NHS trust manager who has a legal obligation to provide care but faces resource constraints.
Moral valuations can interact with financial valuations because they are both made in relation to the same defined intervention. For example, it is possible for a treatment option to be both regarded by the patient as one likely to carry net benefit and simultaneously regarded as not being cost effective by the fee payer.21 This can arise because no clear, uncontroversial calculus exists, which allows translation between the moral and financial valuations of the base MFM.
Value futility
Let us label as value futility the situation where the defined intervention may modify the linking probabilities, but there is still a likely net zero benefit gain.iv This can arise in situations where the defined intervention may achieve the defined goal of treatment but where that defined goal is deemed not worth achieving. A clear example of this is the decision of the House of Lords in Airedale NHS Trust v Bland,22 where artificial hydration and nutrition was held to be futile for a patient in a persistent vegetative state. This case can be analysed as a situation where the defined intervention, artificial hydration and nutrition, was held to be value futile in relation to the defined goal of treatment: prolonging life.
Futility and duty of care owed by the doctor to the patient
If the defined intervention operates to increase the likelihood of a net negative benefit gain above a de minimis level (ie, amounting to harm), then the defined intervention is detrimental. The duty of the doctor then is not to deliver the intervention. Conversely, if a net benefit gain is likely to result from the defined intervention, the duty of the doctor is to deliver the intervention. The key point here is that the treatment can be regarded as futile only if it is neither beneficial nor detrimental—that is, the likely net benefit gain is zero.
Where the defined intervention is declared futile because it is assessed to generate a zero gain in net benefit, the duty of care to treat or not to treat disappears, and there is simply an absence of any obligation to treat or not treat.22 This is not the same as an obligation not to treat, which arises when an intervention results in harm. Technically, the doctor has a Hohfeld privilege20 in relation to the defined intervention as applied to the patient in these circumstances. Therefore, although the intervention may be undertaken or not undertaken, interestingly, the grounds for either choice cannot be grounded in the duty of care.v
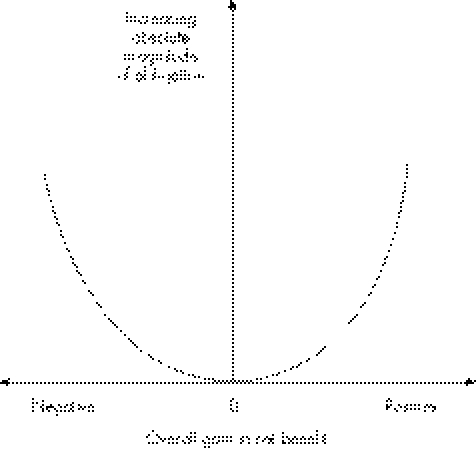
Another way to see this is to make the analogy with a mathematical turning point. Let us accept that the magnitude of the obligation to treat or not to treat is proportional to a function of the net benefit gain resulting from the defined intervention. The absolute magnitude of that obligation to treat or not to treat is plotted against the net benefit gain. The plot arrived at is shown in fig 2.
Figure 2 At zero net benefit gain (futility), the absolute magnitude of the obligation to treat is zero. This is the turning point of the curve.
The point at which the net benefit gain is zero is also the point at which the magnitude of the obligation to treat is zero. At points on either side of this zero point there is an obligation in relation to the defined intervention. If the net benefit gain is positive, the obligation is to treat; if the net benefit gain is negative, the obligation is not to treat. Part of the difficulty with futility is that it is a single point surrounded on each side by opposing duties. Even a small change in the calculation can drive the solution towards a positive or negative duty. Uncertainty present at any level can make resolution of the situation very complex.
The hidden valuation: defining the goal of treatment
The thesis of this article is that to make a declaration that a defined intervention is futile requires an explicit declaration of the defined goal in relation to which that intervention is futile.23,24 This is most important when there is more than one possible outcome state that may carry a net benefit gain, because in those circumstances a simple declaration that an intervention is futile is ambiguous. Because of this potential ambiguity, I argue that to simply declare a defined intervention as futile is to make an inchoate statement.
Consider the following case initially described by Spritz.25 A patient had a newly diagnosed disseminated hepatoma causing massive upper gastrointestinal bleeding.vi Although transfusions could not alter the eventual outcome, the responsible doctor decided to undertake transfusions to provide the patient time to come to terms with his terminal condition.
The defined intervention here was blood transfusion. It was goal futile in relation to the defined goal of preventing patient death in the near future.2 However, in relation to the defined goal of prolonging life for a short time, the defined intervention was not goal futile. For the patient, the value of allowing time to adjust to the sudden change in circumstance was extremely high. In this case, the doctor agreed, implicitly accepting that the defined goal of treatment should be the prolongation of life rather than prevention of death.
I argue that this decision in relation to the choice of the defined goal(s) of treatment is made more transparent and less difficult when it is made in two stages. Firstly, make an explicit declaration of the possible defined goal (or goals) of treatment. Then, make a statement of the agreement reached between the doctor and patient declaring which defined goal (or goals) is appropriate in the circumstances. Although there is clearly potential for substantive conflict, in most cases this approach would probably make subsequent management easier.
To show this, let us consider the situation after several hours of massive blood transfusion. At what point would the defined treatment of the next unit of blood become value or even goal futile in relation to the defined goal of prolonged life for this patient? The answer would turn on the precise facts of the case. For example, on these facts the rate of blood loss may have increased beyond the possible rate of transfusion, the patient may have become unconscious or the patient may have accepted the situation and requested that no further blood be given. In the case of the patient becoming unconscious, notice how the purpose underpinning the choice of the defined goal can also be important.
Potential sources of conflict and power relations
All elements of the base MFM and its valuation should be open to examination. Clearly this requires discourse. Although not absolute,26 the power to value the MFM has moved more and more towards the patient. This is because the objective of the doctor–patient relationship is to promote the patient's welfare, and respect for patient autonomy is a powerful and effective way to achieve this goal. This accords with general medical professional values.27 As between doctor and patient in English law, only if both valuations agree that there is likely to be net benefit gain can the defined intervention be delivered.22,26,28,29
This power to value can be usurped by the doctor in two ways. Firstly, this can arise if the doctors exercise their power over the assessment of linking probabilities to adjust down the probability of reaching a particular positive outcome and adjust up the probability of reaching a particular negative outcome. Such recalculations have the effect of moving the power of decision towards the doctor. If the doctor makes the judgement that the material linking probability is not alterable by a defined intervention, then even if the patients make their valuation of the relevant material outcome state infinite the doctor can refuse treatment on the grounds of goal futility. This translation of value futility to goal futility amounts to a shift in power over determining the choice of treatment.
The second way in which the power to value can be usurped is by the doctor deploying personal values under the guise of general professional values. Although personal values may give grounds for conscientious objection, I would submit that they should not be deployed in valuation of the MFM for the purposes of determining the likely net gain in benefit. The problem here is that it is difficult to detect such covert deployment of personal values and that general professional values are often less than clear and explicit when applied to particular medical situations.
A conflict could also arise where there is a dispute over the choice of the defined goal of treatment. This may arise where, for example, a doctor has usurped the power to value the MFM. In this case, a patient striving to regain power over the final decision may seek to redefine the defined goal of treatment. For example, in Spritz's case mentioned earlier, if the doctor had not agreed to the defined goal of treatment, such a conflict could have arisen. Interestingly, we can see here how the concept of physiological futility remains vulnerable to the charge of being value loaded precisely because it claims control over the definition of the defined goal of treatment, where this can be disputed.6,30
Other options are available to the patient. One is to place infinite value on the fact of intervention alone. This effectively translates the defined goal of treatment from the achievement of a particular outcome state into mere delivery of the defined intervention. This effectively removes the linking probabilities from the equation and disempowers the doctor. This is the “it will make me feel much better just knowing you will try” argument. Another option is to try and re‐evaluate the linking probabilities. This can be via a second medical opinion or through personal research. This approach is particularly effective when the degree of uncertainty surrounding the linking probabilities is great.
This analysis shows a fine balance of power at the heart of the doctor–patient relationship in relation to questions of futility. If we regard medicine as a mutually cooperative exercise with the aim of objectively benefiting patients, then this may not be a bad thing. Given this fine balance, conflicts will almost inevitably arise on occasion.1
Methods of conflict resolution lie beyond the scope of this paper,31 but the point here is that use of the MFM allows a clearer analysis of the actual situation and may allow a route through the minefield to be identified. The requirement to agree on the defined goal of treatment before making a declaration of futility should force doctors to deal with this heretofore hidden issue of value. If accepted into clinical practice, this should reduce both the giving of unnecessary treatments and the risk of substantive conflicts arising.
A role for third‐party ethical input at this level32 exists, and perhaps a method should be developed to generate valuation sets that are more useful to practising clinicians (eg, case‐based reasoning). The benefit for doctors is that such third‐party input can assure appropriate deployment of values, improve transparency of decision making and buttress the public perception of physician integrity.
Conclusion
The concept of medical futility can be illuminated by using the fact–value distinction of Hume. The core medical facts can be extracted as the base MFM. This has a series of physical states linked by probabilities. Each probability has a degree of uncertainty surrounding it. Goal futility flows from the base MFM alone. Value futility flows from the valuation of the base MFM.
A defined intervention is goal futile when it cannot alter the likelihood of the defined goal emerging into reality. A defined intervention is value futile when it can alter the probability of the defined goal entering reality but the defined goal is deemed a goal not worth achieving. It is possible for the defined intervention to be unable to alter the likelihood of the defined goal arising and, at the same time, for that defined goal to be deemed not worth achieving.
Declarations of futility are presently made in relation to defined interventions. I argue that a declaration that a defined intervention is futile is inchoate unless it also explicitly declares the defined goal in relation to which it is futile. The defined goal of treatment should be agreed at least between the doctor and the patient before making a declaration of futility. In making a declaration of futility, it is also necessary to declare whether the defined intervention is deemed goal or value futile.
Conflicts can arise in several areas: (1) dispute over the magnitude of the linking probabilities and their relationship to the defined intervention; (2) the choice of outcome states; (3) the choice of the defined goal of treatment; (4) the content of the defined intervention; and (5) the valuation of the outcome states and the defined goal of treatment. These remain to be resolved, but it is hoped that by adopting a clear declaration of futility as set out above, such conflicts can be pre‐empted and the use of unnecessary treatments can be reduced. Such an approach should reduce misunderstandings and narrow the questions at issue if substantive conflict does arise. Further research is required at all these levels. The medical factual matrix is a powerful tool and will have broad application.
Acknowledgements
I thank two unnamed reviewers whose helpful comments have improved the text.
Abbreviations
DNAR - do not attempt resuscitation
MFM - medical factual matrix
NHS - National Health Service
Footnotes
iHere, medical intervention means a possible action that may affect the physical or mental state of the patient, which is under consideration by medically qualified people responsible for the care of the patient.
iiThis view has analogies in quantum mechanics—for example, Schrödinger's cat.
iiiNet benefit = (probability of benefit×amount of benefit)−(probability of harm×amount of harm)−cost of intervention. Each valuer will view this equation from his or her own particular perspective.
vThe House of Lords in Bland (footnote iii) seems to have applied the Bolam test here (Bolam v Friern Hospital Management Committee [1957] 2 All ER 118), essentially importing medical professional values (effectively both general professional values and the personal professional values of the clinical team responsible).
ivThis situation may arise, for example, if the net benefit calculation is affected by the cost of treatment, there are multiple valuations of the MFM in operation or the uncertainty surrounding the accuracy of the linking probabilities is large.
viNote facts cf In re Storar (1981) 420 US 858, where blood transfusions were given for anaemia secondary to bladder cancer.
Competing interests: None.
References
- 1. Wyatt v Portsmouth NHS Trust And Wyatt (By Her Guardian) (No 3) [2005] EWHC 693, Fam
- 2. An NHS Trust v Baby MB [2006] EWHC 507. http://www.bailii.org/ew/cases/EWHC/Fam/2006/507.html (accessed 13 Jun 2006)
- 3.Hume D.Treatise of human nature. book III, part 1. London: JM Dent & Sons, 1738
- 4.Tomlinson T, Brody H. Ethics and communication in do‐not‐resuscitate orders. N Engl J Med 198831843–46. [DOI] [PubMed] [Google Scholar]
- 5.Tomlinson T, Brody H. Futility and the ethics of resuscitation. JAMA 19902641276–1280. [PubMed] [Google Scholar]
- 6.Wreen M. Medical futility and physician discretion. J Med Ethics 200430275–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waisel D B, Truog R D. The cardiopulmonary resuscitation‐not‐indicated order: futility revisited. Ann Intern Med 1995122304–308. [DOI] [PubMed] [Google Scholar]
- 8.Schneiderman L J, Jecker N S, Jonsen A R. Medical futility: response to critiques. Ann Intern Med 1996125669–674. [DOI] [PubMed] [Google Scholar]
- 9.Schneiderman L J, Jecker N S, Jonsen A R. Medical futility: its meaning and ethical implications. Ann Intern Med 1990112949–954. [DOI] [PubMed] [Google Scholar]
- 10.Brody B A, Halevy A. Is futility a futile concept? J Med Philos 199520123–144. [DOI] [PubMed] [Google Scholar]
- 11.Gillon R. “Futility”—too ambiguous and pejorative a term? J Med Ethics 199723339–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Helft P R, Siegler M, Lantos J. The rise and fall of the futility movement. N Engl J Med 2000343293–296. [DOI] [PubMed] [Google Scholar]
- 13.Johnston J, Elliott C. Healthy limb amputation: ethical and legal aspects. Clin Med 20022431–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Veatch R M, Spicer C M. Medically futile care: the role of the physician in setting limits. Am J Law Med 19921815–36. [PubMed] [Google Scholar]
- 15.Schneiderman L J, Jecker N S, Jonsen A R. Medical futility: response to critiques. Ann Intern Med 1996125669–674. [DOI] [PubMed] [Google Scholar]
- 16.Schneiderman L J, Jecker N S, Jonsen A R. Medical futility: its meaning and ethical implications. Ann Intern Med 1990112949–954. [DOI] [PubMed] [Google Scholar]
- 17.Rawlins M D. 5 NICE years. Lancet 2005365904–908. [DOI] [PubMed] [Google Scholar]
- 18.Rawlins M D, Culyer A J. National Institute for Clinical Excellence and its value judgments. BMJ 2004329224–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harper W. The role of futility judgments in improperly limiting the scope of clinical research. J Med Ethics 199824308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hohfeld W N. In: Cook WW, ed. Fundamental legal conceptions as applied in judicial reasoning. New Haven, CT: Yale University Press, 1919 (reprint 1964),
- 21.Ferriman A. UK government finalises restrictions on viagra prescribing. BMJ 19993181305A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Airedale NHS Trust v Bland [1993] AC 789, HL. Contrast this with In re Baby K. Fed. Report. 1994;16: 590–599 where an anencephalic baby received life prolonging treatment,
- 23.Kite S, Wilkinson S. Beyond futility: to what extent is the concept of futility useful in clinical decision‐making about CPR? Lancet Oncol 20023638–642. [DOI] [PubMed] [Google Scholar]
- 24.Wilson B E. Futility and the obligations of physicians. Bioethics 19961043–55. [DOI] [PubMed] [Google Scholar]
- 25.Spritz N. Physicians and medical futility: experience in the setting of general medical care. In: Zucker M, Zucker ED, eds. Medical futility and the evaluation of life‐sustaining interventions. Cambridge: Cambridge University Press, 199741–42.
- 26. R v General Medical Council ex parte Burke [2005] EWCA 1879, CA. http://www.bailii.org/ew/cases/EWCA/Civ/2005/1003.html (accessed 13 Jun 2006)
- 27.General Medical Council Withholding and withdrawing life‐prolonging treatments: good practice in decision‐making. London: GMC, 2002
- 28. St George's Healthcare NHS Trust v S [1998] 3 All ER 673, CA
- 29. An NHS Trust v Baby MB [2005] EWHC 507. http://www.bailii.org/ew/cases/EWHC/Fam/2006/507.html (accessed 13 Jun 2006)
- 30.Waisel D B, Truog R D. The cardiopulmonary resuscitation‐not‐indicated order: futility revisited. Ann Intern Med 1995122304–308. [DOI] [PubMed] [Google Scholar]
- 31.Bloche M G. Managing conflict at the end of life. N Engl J Med 20053522371–2373. [DOI] [PubMed] [Google Scholar]
- 32.Schneiderman L J, Gilmer T, Teetzel H D.et al Effect of ethics consultations on nonbeneficial life‐sustaining treatments in the intensive care setting: a randomized controlled trial. JAMA 20032901166–1172. [DOI] [PubMed] [Google Scholar]