Abstract
Objectives
To assess the effectiveness of non‐legislative interventions in increasing bicycle helmet use among children and young people, and to identify possible reasons for differential effectiveness of interventions.
Design
Systematic review and meta‐analysis.
Data sources
10 electronic databases were searched up to October 2006. Several other sources of potentially relevant information were identified and examined.
Review methods
We included randomized controlled trials, non‐randomized controlled trials and controlled before‐and‐after studies of interventions to promote bicycle helmet use, which did not require the enactment of legislation. Participants were aged between 0 and 18 years.
Main outcome measure
Observed helmet wearing.
Results
13 studies were included in the review and 11 in the meta‐analysis. The odds of observed helmet wearing were significantly greater among children and young people in the intervention groups (OR 2.13, 95% CI 1.35 to 3.35). Subgroup analysis indicated that the effect might be greater for community‐based studies (4.57, 2.37 to 8.81) and those providing free helmets (4.60, 2.25 to 9.43) than for those providing subsidized helmets (2.11, 1.09 to 4.06) and those set in schools (1.73, 1.04 to 2.89). Evidence for the effectiveness of the interventions was stronger in studies with follow‐up periods of ⩽6 months (2.23, 1.27 to 3.90) than in those with longer‐term follow‐up (1.63, 0.91 to 2.91).
Conclusions
Non‐legislative interventions are effective in increasing bicycle helmet use among children and young people. Community‐based helmet promotion programmes that include the provision of free helmets may increase observed helmet wearing to a greater extent than those set in schools or those providing subsidized helmets.
Injuries to cyclists are a global public health problem.1 They are of particular concern in higher‐income countries where the prevalence of cycling is high, and in low‐ and middle‐income countries where cycling is one of the predominant modes of transport.1 Furthermore, injuries to cyclists are likely to become an increasing problem in low‐ and middle‐income countries as the degree of motorization increases. Even in high‐income countries, such as the US, where cycling is an uncommon mode of adult transport, travel surveys indicate that approximately 5% of children rode a bike on the survey day,2 and in the UK, the annual average cycle mileage is higher among children and young people aged 11–16 years than for any other age group.3
Most fatal injuries to cyclists result from head injury.4 Bicycle helmets provide physical protection for the face and head of their wearers. A previous systematic review has shown their effectiveness in preventing bicycle‐related head and facial injuries in cyclists involved in all types of crashes.4 However, relatively few children and young people wear helmets.5,6,7 A recent large study in 46 states and in the District of Columbia observed 42% of child cyclists aged 5–14 years wearing a helmet.5 A recent national survey in the UK found only 14% of child cyclists were observed to be wearing a helmet, with the lowest wearing rates among boys aged 7–10 and 11–16 years,6 and observations of helmet wearing in Sweden indicated that approximately one‐third of children wore helmets when cycling to school or when cycling at other times.7
Although a recent systematic review concluded that legislation seems to substantially increase bicycle helmet wearing,8 many countries do not currently enforce helmet wearing. Promotion programmes therefore remain important interventions for increasing helmet use. Although many studies have described such programmes, these have varied in terms of effectiveness and the strategies they used. It is therefore difficult for those developing bicycle helmet promotion programmes to know how effective such programmes may be and which program components contribute most to their effectiveness. The aim of this review was to identify non‐legislative interventions that are effective in promoting helmet use among children, so that future bicycle helmet promotion programmes can be designed from a firm evidence base. This paper reports an update to a review published in the Cochrane Database of Systematic Reviews.9
Methods
Search strategies
We searched 10 electronic databases from the date of inception up to October 2006 (Cochrane Central Register of Controlled Trials, Database of Abstracts of Reviews of Effectiveness, Medline, Embase, Transport Research Laboratory, CINAHL, ERIC, PsycINFO, Transport Research Information Service and British Education Index), 5 online bibliographies (http://www.cyclehelmets.org, European cyclists federation, bicycle helmet safety institute, cyclecraft and the Bicycle Helmet Initiative Trust), reference lists of systematic reviews and other key papers, the proceedings of the first 8 World Conferences on Injury Prevention and Safety Promotion and the journal InjuryPrevention up to October 2006. Details of the search strategies have been published elsewhere.9
Inclusion criteria
Studies eligible for inclusion were randomized controlled trials (RCTs), non‐RCTs and controlled before‐and‐after studies evaluating interventions to promote bicycle helmet use without the enactment of legislation and reporting observed helmet wearing as an outcome measure. This included health education programmes, subsidized, discounted or free helmet distribution programmes and media campaigns. Interventions that included legislation as a component were excluded. Participants were aged between 0 and 18 years. No language restrictions were used.
Selection of studies to be included in the review
Two independent reviewers assessed the eligibility of titles and abstracts of studies identified through searches. Two independent reviewers assessed full copies of papers that seemed to meet the inclusion criteria. Uncertainties concerning the appropriateness of studies for inclusion were resolved through consultation with a third reviewer. Non‐English language studies were translated before being considered for inclusion.
Data extraction
A standard data extraction form was used to record data on participants, interventions and outcomes. Data were extracted by two researchers independently, blind to the author and institution of the article. Extracted data were compared between reviewers, with any discrepancies resolved at a meeting of reviewers. Special care was taken to avoid including multiple reports pertaining to the same study. Where data were not available in the published articles, authors were contacted to supply the missing information.
Quality assessment
For RCTs, allocation concealment, blinding of outcome assessment and completeness of follow‐up were used as markers of trial quality. For non‐RCTs, blinding of outcome assessment and completeness of follow‐up were used as markers of quality and assessment of the distribution of confounders. Two reviewers, blinded to study findings assessed quality independently, and inter‐reviewer agreement was measured.
Assessing heterogeneity and publication bias
Heterogeneity between results of included studies was explored using forest plots, the I2 statistic and χ2 tests of heterogeneity (using a 10% significance level). The reasons for heterogeneity were explored with subgroup analyzes. Publication bias was assessed using a funnel plot and Egger's test.
Combining treatment effects
Pooled odds ratios (ORs) and 95% CIs were estimated using random effects meta‐analysis using STATA V.8.0 software. Where there was a zero in the 2×2 table for any study, 0.5 was added to each cell of that table before the meta‐analysis was performed. Where studies using cluster allocation were reported without adjustment for clustering, we approached authors for information on the intraclass correlation coefficient (ICC) or to obtain data from which we could calculate the ICC. None of the studies had calculated an ICC or provided data from which an ICC could be calculated. Hence, we adjusted reported treatment effects for clustering using an ICC of 0.02, as reported for a school‐based health promotion intervention,10 and undertook sensitivity analyzes using ICCs of 0.01 and 0.05. These values were chosen because we believe that they represent the extremes of the range within which the true value is likely to be found.11,12 Adjusted numerators and denominators were included in analyzes as non‐integers.
Two studies had two intervention arms (subsidized helmets and education, and education only) and only one control arm.13,14 For both these studies, the subsidized helmet and education arms were included in the main analysis as this intervention arm was most comparable to the intervention arms of other included studies. The education‐only arm of one study14 was included in the subgroup analysis assessing the effect of education alone. The second study was excluded from this analysis as no children in either arm were observed wearing helmets.13
Baseline data on observed helmet wearing were reported for nine studies, but one13 reported no children in either treatment arm wearing helmets and was therefore excluded. Follow‐up helmet wearing rates for the remaining eight studies were adjusted for baseline wearing rates by including a time by treatment group interaction term into a logistic model using grouped data for each study. Effect sizes and standards errors from this model were then used in a random‐effects meta‐analysis.
Results
Description of studies
Figure 1 describes the process of study selection. A total of 13 studies were included in the systematic review, 11 of which were included in the meta‐analysis. Table 1 describes the studies included. Three studies were cluster RCTs13,15,16 and 10 were controlled before‐and‐after studies.14,17,18,19,20,21,22,23,24,25 Seven were set in the US,15,17,18,19,21,22,25 four in Canada,13,14,20,24 one in New Zealand23 and one in Australia.16 One study17 included only pre‐school children and a second included only children aged between 5 and 8 years.22 The remaining included children from a range of ages up to 18 years. The participants of two studies were from low‐income families17 or schools in low‐income areas,14 with other studies including children from families and areas with a range of income levels. Four studies involved participants in community settings,17,18,19,20 three of which were multifaceted community interventions18,19,20 and the remaining study providing a multifaceted program at home and at nursery school.17 The remaining nine studies were set in schools.13,14,15,16,21,22,23,24,25 Two interventions included the distribution of free helmets,17,20 eight provided subsidized or discounted helmets,13,14,15,18,20,22,23,24 three provided only education16,21,25 and a further two studies with three treatment arms provided only education in one arm.13,14 All studies providing free, subsidized or discounted helmets also included an educational element.
Figure 1 Flow diagram describing the process of study selection.
Table 1 Characteristics of included studies.
| Study | Type | Blinding | Completeness of follow‐up | Balanced confounders | Age range (years) | Numbers of participants* | Setting | Intervention | Measurement of outcome | Baseline observations | In meta‐analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Britt, 199817 | CBA | N | N | NR | 3–4 | I = 680 children (14 sites) | Community+School | F+E | T (1) = 2W | I = 99/230 (43.0%) | Y |
| C = 200 children (4 sites) | C = 30/71 (42.3%) | ||||||||||
| Cote, 199218 | CBA | N | NA | Median income I >C | <16 | Total observations = 328 | Community | S+E | T (1) = 9M | I = 11/140 (7.9%) | Y |
| C = 7/37 (18.9%) | |||||||||||
| DiGuiseppi, 198919 | CBA | N | NA | Y | 5–15 | Total observations = 9827 | Community | S+E | T (1) = 4M | I = 50/905 (5.5%) | Y |
| T (2) = 12M | C = 11/1052 (1.0%) | ||||||||||
| T (3) = 16M | |||||||||||
| Farley, 199620 | CBA | N | NA | NR | 5–12 | I = 50 000 children (244 schools) | Community | F+S+E | T (1) = 12M | NR | Y |
| C = 6513 children | T (2) = 24M | ||||||||||
| T (3) = 36M | |||||||||||
| Floerchinger, 200021 | CBA | N | NA | NR | 5–12 | I = 4 schools | School | E | T (1) = 5M | I = 24/59 (40.7%) | Y |
| C = 19 schools | C = 97/284 (34.2%) | ||||||||||
| Hall, 200416 | cRCT | N | Y | Y | 5–12 | I = 13 schools | School | E | T (1) = 6M | I = 455/512 (88.9%) | Y |
| C = 14 schools | T (2) = 18M | C = 559/603 (92.7%) | |||||||||
| Liller, 199522 | CBA | N | NA | NR | 5–8 | I = 3428 children (9 schools) | School | S+E | T (1) = 2W | I+C = 46/543 (8.5%) | Y |
| C = 9 schools | |||||||||||
| Moore, 199023 | CBA | N | NA | NR | 11–13 | I = 1 school | School | S+E | T (1) = 6W | NR | N |
| C = 1 school | T (2) = 10W | ||||||||||
| Morris, 199113 | cRCT | N | NR | NR | 5–13 | I (1) = 1 school | School | I(1) S+E | T (1) = 1M | I (1) = 0/22 (0%) | Y |
| I (2) = 1 school | I(2) E | I (2) = 0/25 (0%) | |||||||||
| C = 1 school | C = 0/22 (0%) | ||||||||||
| Parkin, 199324 | CBA | N | NA | Y | 5–14 | I = 1100 children (4 schools) | School | S+E | T (1) = 2M | I = 13/420 (3.1%) | Y |
| C = 18 schools | C = 15/482 (3.1%) | ||||||||||
| Parkin, 199514 | CBA | N | NA | Y | 5–14 | I = 1415 | School | I(1) S+E | T (1) = 2M | I (1) = 5/129 (3.9%) | Y |
| I(2) E | I (2) = 1/152 (0.7%) | ||||||||||
| C = 7/246 (2.8%) | |||||||||||
| Towner, 199215 | cRCT | N | NA | NR | 5–12 | I = 3 schools | School | S+E | T (1) = 2W | I = 3/556 (0.5%) | Y |
| C = 3 schools | T (2) = 4M | C = 11/369 (3.0%) | |||||||||
| Total children = 2211 | |||||||||||
| Wright, 199525 | CBA | N | NA | C older than I | 11–18 | Total observations = 741 | School | E | T (1) = 2W | NR | N |
C, control; CBA, controlled before/after study; cRCT, cluster randomized controlled trial; E, education/promotion program; F, free helmets; I (n), intervention (arm n); M, months; N, no; NA, not applicable; NR, not reported; RCT, randomized controlled trial; S, subsidized helmets; T (n), time point (n); W, weeks; Y, yes.
*Where number of children or schools is not included in the table this is due to data not reported in publications.
Data extracted from two studies23,25 were excluded from the meta‐analysis because numerators and denominators were not reported or available from the authors. Four studies provided data from more than one time point. The main analysis includes outcome data obtained at 4 months from the study by DiGuiseppi et al,19 at 12 months from the study by Farley et al,20 at 19 weeks from the study by Towner and Marvel15 and at 6 months from the study by Hall et al16 to optimize comparability. We also undertook subgroup analyzes exploring the effect of shorter (⩽6 months) and longer (>6 months) follow‐up periods on effect sizes.
Methodological quality of included studies
Table 1 presents the comments on the important methodological features of each study. Most studies measured observed helmet wearing by sampling in community settings. The completeness of follow‐up cannot be assessed with this study design. None of the studies adjusted for a clustering effect in the data presented and none that used randomization described this in sufficient detail for us to comment on the adequacy of concealment.
Inter‐reviewer agreement of study quality assessment
Two independent reviewers rated allocation concealment with 86% agreement and blinding of outcome assessors with 100% agreement.
Adverse effects of interventions
None of the included studies reported any adverse effects of interventions.
Meta‐analysis
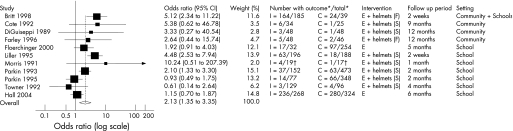
Figure 2 shows that the odds of observed helmet wearing were significantly higher among children and young people in the intervention groups (OR 2.13, 95% CI 1.35 to 3.35). There was significant heterogeneity between the effect sizes of the studies included in this analysis (χ2 = 28.43, df = 10, p = 0.002, I2 = 64.8%). These findings were robust to using an ICC of either 0.01 or 0.05. There was no evidence of publication bias (Egger's test, p = 0.56). Adjusting for baseline helmet wearing rates had little impact on the findings (OR 2.05, 95% CI 1.30 to 3.23).
Figure 2 Odds ratios for observed helmet wearing among included studies. *Numbers adjusted for clustering; †0.5 has been added to all cells in the 2×2 table. I, intervention arm; C, control arm; E, education; F, free helmet; S, subsidized or discounted helmets.
We assessed the effect of study quality by restricting analyzes to RCTs and no significant effect was shown (OR 1.15, 95% CI 0.51 to 2.62). These findings were robust to using an ICC of either 0.01 or 0.05.
Subgroup analyzes were undertaken to explore possible explanations for the heterogeneity in observed helmet wearing. These included examining the effect in community‐based studies, in school‐based studies, among programmes providing free helmets, those providing subsidized helmets, those providing education without free or subsidized helmets, those with shorter (⩽6 months) and longer (>6 months) follow‐up periods and those set in low‐income families or communities compared with those in communities with a range of income levels. We chose these subgroups as it seemed theoretically plausible that these factors might influence the effectiveness of the intervention. The effect sizes for all subgroup analyzes were robust to assuming ICCs of 0.01 or 0.05.
Among the four community‐based studies,17,18,19,20 the odds of observed helmet wearing were significantly greater among children and young people in the intervention groups (OR 4.57, 95% CI 2.37 to 8.81; χ2 = 0.53, df = 3, p = 0.91; I2 = 0%). These findings were robust to excluding the study17 in which the intervention was provided in the community and at nursery school (3.48, 1.05 to 11.61). Interventions were provided at school in seven studies,13,14,15,16,21,22,24 and these showed a significant, but possibly smaller effect (1.73, 1.04 to 2.89) with significant heterogeneity between effect sizes (χ2 = 20.97, df = 6, p = 0.002; I2 = 71.4%). These findings were robust to including the study17 in which the intervention was partly provided at nursery school (2.00, 1.20 to 3.23).
Pooling the results of the two studies providing free helmets17,20 showed that the odds of observed helmet wearing were significantly greater among children and young people in the intervention groups (OR 4.60, 95% CI 2.25 to 9.43; χ2 = 0.44, df = 1, p = 0.51; I2 = 0%). Pooling the results of the seven studies providing subsidized or discounted helmets13,14,15,18,19,22,24 showed a significant but possibly smaller effect (2.11, 1.09 to 4.06), with significant heterogeneity between effect sizes (χ2 = 17.69, df = 6, p = 0.007; I2 = 66.1%). Four studies included in the meta‐analysis evaluated educational interventions without helmet provision,13,14,16,21 one of which was excluded from the analysis as no children were observed wearing helmets in either treatment arm.13 Only educational interventions were found to have a smaller effect than those providing free helmets (OR 1.40, 95% CI 1.01 to 1.94; χ2 = 1.38, df = 2, p = 0.50; I2 = 0%).
Seven studies only reported helmet wearing at ⩽6 months13,14,15,17,21,22,24 and four at >6 months of follow‐up.16,18,19,20 There was some evidence that the effect may be greater among those with shorter (OR 2.23, 95% CI 1.27 to 3.90; χ2 = 21.49, df = 6, p = 0.001; I2 = 72.1%) than longer follow‐up periods (1.63, 0.91 to 2.91; χ2 = 3.37, df = 3, p = 0.34; I2 = 10.9%). Finally, effect sizes were similar, but 95% CIs wider, in the two studies involving low‐income families or areas14,17 (2.14, 0.40 to 11.46) than in those in communities with a range of income levels13,15,16,18,19,20,21,22,24 (2.13, 1.33 to 3.39).
Four studies considered the effect of interventions by social group.14,19,20,24 One study19 seemed to be effective in low‐income communities where helmet use in the intervention group increased from 3.4% at baseline to 11.1% at follow‐up, whereas helmet use by the control group did not change over the same period. One study20 found the intervention to be three times more effective in more affluent than in less affluent areas. A third study24 found that helmet use increased more in high‐ than in low‐income intervention areas (29% vs 12%, p<0.01), whereas the final study14 reported significant increases in helmet use in all income groups, and a graphical comparison of trends suggesting that the intervention may be more effective in higher‐income areas.
Data not included in the meta‐analysis
The study by Moore and Adair23 reported a significant increase in observed helmet wearing in the intervention arm from 3.5% at baseline to 33.3% at 10 weeks and a non‐significant increase in the control arm from 6.3% to 10.9%. The study by Wright et al25 reported only 22 observations of helmet use, and none of the changes in use over time were significant.
Discussion
Main findings
Non‐legislative interventions are effective in increasing bicycle helmet use among children and young people. Community‐based helmet promotion programmes including the provision of free helmets may increase observed helmet wearing to a greater extent than those set in schools or those providing subsidized or discounted helmets, although these also significantly increased helmet use. Unfortunately, we were unable to disentangle the effect of study setting from that of the provision of free helmets, as both studies providing free helmets were community based. Interventions set in schools increased observed helmet wearing, and given that those studies showing the most positive effect were those including the youngest participants,17,22 this may reflect a tendency for interventions to be more effective among younger children. There was evidence of a significant but smaller effect in interventions that were purely educational and that did not provide free, subsidized or discounted helmets. There was some evidence that the effect of interventions may decrease with increasing follow‐up periods.
Strengths and weaknesses of this review
This systematic review included 13 studies of non‐legislative interventions to promote helmet wearing. The studies varied widely in a number of important characteristics including setting, age of participants, components of the intervention, length of follow‐up and outcomes reported. This “clinical” heterogeneity was reflected to some extent in statistical heterogeneity when results were pooled in some of the meta‐analyzes. We explored this heterogeneity in subgroup analyzes and have identified some features of interventions that are associated with significant increases in helmet wearing, but have not been able to fully explain it. A lack of RCTs in this area means that most included studies were potentially at risk of bias and confounding. However, 8 of the 10 non‐randomized studies either presented data to confirm, or commented, that treatment arms were balanced with respect to measured potential confounders or matched control and intervention areas with respect to potential confounders at the design stage.
Despite the size of the problem of injuries to cyclists in low‐ and middle‐income countries, all the studies included in our review were undertaken in high‐income countries. Caution must therefore be exercised in extrapolating our findings to low‐ and middle‐income countries. In addition, as most of the studies included in our review were undertaken >10 years ago, changes in helmet cost and in the prevalence of helmet wearing may mean that the interventions included in our review may no longer produce effect sizes as large as those shown. However, helmet wearing rates among children are still low in many countries,5,6,7 suggesting considerable capacity for their increase. Social gradients in helmet ownership and use persist,26,27 and recent research has shown that providing free helmets reduces inequalities in helmet ownership,28 suggesting that cost remains an important issue in relation to helmet use.
Key points
Systematic review data suggest that bicycle helmets are effective in preventing bicycle‐related head and facial injuries in cyclists involved in all types of crashes.
Legislation seems to substantially increase bicycle helmet wearing, but many countries do not currently enforce helmet wearing.
We found non‐legislative interventions to be effective in increasing bicycle helmet use among children and young people.
Community‐based helmet promotion programmes that include the provision of free helmets may increase helmet wearing to a greater extent than those set in schools or those providing subsidized helmets.
Implications for research
Further research is required to investigate whether providing subsidized helmets is as effective as providing free helmets in community settings, whether the effect of bicycle helmet promotion programmes differs by social group and whether longer‐term effects can be shown. In addition, research is needed to explore the transferability of findings relating to cycle helmet use from high‐ to low‐ and middle‐income countries. As there is concern that strategies to increase bicycle helmet use may reduce cycling,29 programmes that promote bicycle helmet use should also monitor cycling activity.
Implications for prevention
Agencies and organizations with a responsibility for child health or injury prevention should consider providing bicycle helmet promotion programmes. Such programmes may have the greatest effect if they are provided in the community rather than in schools and if they provide free rather than subsidized helmets.
Abbreviations
ICC - intraclass correlation coefficient
RCT - randomized controlled trial
Footnotes
Competing interests: None.
Contributors: SR and DK conceived this review and coordinated its preparation. SR, DK and TC contributed to discussions about core ideas, the design of the study and the interpretation of data. SR and DK undertook the statistical analysis. SR, DK and TC collected the data and carried out quality scoring. SR wrote the paper with the assistance of DK and TC. SR had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.World Health Organization World report on roads traffic injury prevention. Geneva: World Health Organization, 2004
- 2.Barnes G.The benefits of bicycling in Minnesota. Minnesota: Minnesota Department of Transportation Research Services Section, 2004
- 3.Gill T.Cycling and children and young people: a review. London: National Children's Bureau, 2005
- 4.Thompson D C, Rivara F P, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database Syst Rev 1999CD001855. [DOI] [PMC free article] [PubMed]
- 5.Cody B E, Quraishi A Y, Mickalide A D.Headed for injury: an observational survey of helmet use among children ages 5 to 14 participating in wheeled sports. Washington, DC: National SAFE KIDS Campaign, 2004
- 6.Inwood C, Whitley C, Sexton B.Cycle helmet wearing in 2004. TRL Report TRL644. Wokingham: Transport Research Laboratory, 2005
- 7.Nolen S, Ekman R, Lindqvist K. Bicycle helmet use in Sweden during the 1990s and in the future. Health Promot Int 20052033–40. [DOI] [PubMed] [Google Scholar]
- 8.Karkhaneh K, Kalenga J ‐ C, Hagel B E.et al Effectiveness of bicycle helmet legislation to increase helmet use: a systematic review. Inj Prev 20061276–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Royal S T, Kendrick D, Coleman T. Non‐legislative interventions for the promotion of cycle helmet wearing by children. Cochrane Database Syst Rev 2005CD003985. [DOI] [PubMed]
- 10.Murray D, Cattelier D, Hannan P.et al School‐level intra‐class correlation coefficient for physical activity in adolescent girls. Med Sci Sports Exercise 200436876–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams G, Gulliford M C, Ukoumunne O C.et al Patterns of intra‐cluster correlation from primary care research to inform study design and analysis. J Clin Epidemiol 200457785–794. [DOI] [PubMed] [Google Scholar]
- 12.Ukoumunne O C, Gulliford M C, Chinn S.et al Methods for evaluating area‐wide and organisation‐based interventions in health and health care: a systematic review. Health Technol Assess 19993iii92. [PubMed] [Google Scholar]
- 13.Morris B A, Trimble N E. Promotion of bicycle helmet use among schoolchildren: a randomized clinical trial. Can J Public Health 19918292–94. [PubMed] [Google Scholar]
- 14.Parkin P C, Hu X, Spence L J.et al Evaluation of a subsidy program to increase bicycle helmet use by children of low‐income families. Pediatrics 199596283–287. [PubMed] [Google Scholar]
- 15.Towner P, Marvel M K. A school‐based intervention to increase the use of bicycle helmets. Fam Med 199224156–158. [PubMed] [Google Scholar]
- 16.Hall M, Cross D, Howat P.et al Evaluation of a school‐based peer leader bicycle helmet intervention. Inj Control Saf Promot 200411165–174. [DOI] [PubMed] [Google Scholar]
- 17.Britt J, Silver I, Rivara F P. Bicycle helmet promotion among low income preschool children. Inj Prev 19984280–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cote T R, Sacks J J, Lambert‐Huber D A.et al Bicycle helmet use among Maryland children: effect of legislation and education. Pediatrics 1992891216–1220. [PubMed] [Google Scholar]
- 19.DiGuiseppi C G, Rivara F P, Koepsell T D.et al Bicycle helmet use by children. Evaluation of a community‐wide helmet campaign. JAMA 19892622256–2261. [PubMed] [Google Scholar]
- 20.Farley C, Haddad S, Brown B. The effects of a 4‐year program promoting bicycle helmet use among children in Quebec. Am J Public Health 19968646–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Floerchinger‐Franks G, Machala M, Goodale K.et al Evaluation of a pilot program in rural schools to increase bicycle and motor vehicle safety. J Community Health 200025113–124. [DOI] [PubMed] [Google Scholar]
- 22.Liller K D, Smorynski A, McDermott R J.et al The more health bicycle safety project. J Sch Health 19956587–90. [DOI] [PubMed] [Google Scholar]
- 23.Moore D W, Adair V. Effects of a school‐based education programme on safety helmet usage by 11‐ to 13‐year‐old cyclists. Educ Psychol 19901073–78. [Google Scholar]
- 24.Parkin P C, Spence L J, Hu X.et al Evaluation of a promotional strategy to increase bicycle helmet use by children. Pediatrics 199391772–777. [PubMed] [Google Scholar]
- 25.Wright M, Rivara F P, Ferse D. Evaluation of the think tirst head and spinal cord injury prevention program. Inj Prev 1995181–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Towner E, Dowswell T, Burkes M.et alBicycle helmets—a review of their effectiveness: a Critical Road Safety Research Report 30. London: Department for Transport, 2002
- 27.Kendrick D, Royal S, “Lids for Kids” project team Inequalities in cycle helmet use: cross sectional survey in schools in deprived areas of Nottingham. Arch Dis Child 200388876–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kendrick D, Royal S, “Lids for Kids” project team Cycle helmet ownership and use; a cluster randomised controlled trial in primary school children in deprived areas. Arch Dis Child 200489330–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bryan‐Brown K, Taylor S.Cycle helmet wearing in 1996. TRL Report 286. Wokingham: Transport Research Laboratory, 1997