Abstract
Background
Tobacco smoking entails inhaling millions of fine particles with each puff, and it is intuitive that after smoking a cigarette it will take a certain time to washout residual tobacco smoke (RTS) from the lungs with subsequent breaths.
Objectives
To study the washout time of 0.3–1.0 µm particles after the last puff in 10 volunteer smokers by using equipment capable of measuring particle concentration in real time in the exhaled air.
Result
Mean (standard deviation (SD)) lung RTS washout time was 58.6 (23.6) s, range 18–90 s, and corresponded to 8.7 (4.6) subsequent breathings. The contribution of individual and overall RTS to indoor pollution was calculated by subtracting incremental background particle concentration from room concentration after 10 consecutive re‐entries of smokers after the last puff into a room of 33.2 m3, with an air exchange rate per hour in the range of 0.2–0.4. Mean (SD) individual RTS contribution consisted of 1402 (1490) million particles (range 51–3611 million), whereas RTS increased room 0.3–1.0 µm particle concentration from a baseline of 22 283 particles/l to a final room concentration of 341 956 particles/l, corresponding to a total increase in particulate matter (2.5) from a background of 0.56 up to 3.32 µg/m3.
Conclusion
These data reveal a definite although marginal, role of RTS as a source of hidden indoor pollution. Further studies are needed to understand the relevance of this contribution in smoke‐free premises in terms of risk exposure; however, waiting for about 2 min before re‐entry after the last puff would be enough to avoid an unwanted additional exposure for non‐smokers.
Environmental tobacco smoke (ETS) is considered to be the most important source of indoor pollution and a recognised health risk factor.1,2 Despite a putative lower exposure to toxic substances of tobacco, its effect on human tissues and organs seems to be almost as dangerous as active smoke.3 ETS monitoring carried out by means of particulate matter measurements showed that the smoke of a few cigarettes can contribute to indoor pollution up to levels exceeding outdoor limits,1,4 and even higher than those produced by recent diesel engines.5 Research in this field conducted in the past 20 years led to the enactment of smoking policy rules in many countries, whose enforcement was linked to improvement in the health status of citizens.6 Where smoking is restricted, smokers are required to smoke outdoors, and often light up in the vicinity or in front of the buildings; they then re‐enter the buildings through common entrances immediately after finishing their cigarettes. To date, the retention time of mainstream smoke in the lung residual tobacco smoke (RTS) after the last puff has been investigated for volatile organic compounds,7,8 but not yet for particulate matter, and its contribution to indoor ETS pollution has not been fully evaluated.9 New technologies in the field of aerosol analysers have recently made it possible to measure aerosol particles in the exhaled air in real time.10 We carried out this study to measure the retention time of tobacco smoke particulate matter after the last puff and to evaluate the contribution of RTS to ETS pollution.
Methods
Setting
The experiments were carried out in a laboratory in Chiavenna, in the Alpine region of northern Italy. This location was chosen for the study because of the low level of particulate matter pollution in this area. The laboratory was a non‐ventilated 33.2 m3 room, with a natural air exchange rate per hour in the range of 0.2–0.4. Two kinds of experiments were carried out: RTS lung washout time calculation and its contribution to indoor air pollution, as described below. Two kinds of cigarette brands were used by smokers, namely Italian MS Filter and Marlboro Light.
Subjects
Fifteen healthy smokers (four of them women) who consulted a general practitioner were selected, and they agreed to participate in the study aged 28–69 years, average pack‐years 18 (range 8–48), mean exhaled carbon monoxide 32.2 ppm (range 7–45)). Ten of them participated in the lung washout time studies, and five in the study to evaluate the contribution of RTS to indoor pollution.
Exhaled particle measurement
Particle concentration in the exhaled air was measured in real time, as shown previously.10 Subjects were asked to inhale ambient air through the nose and to exhale into a mouthpiece connected with a laser analyser. Exhaled air was heated at 45°C to avoid condensation, and diverted by a pump into a laser‐operated particle counter with a sampling time of 1 s. The analyser (model 9012, Metone, Oregon USA) can measure six different classes of particulate matter size (0.3–1.0, 1.1–2.0, 2.1–3.0, 3.1–4.0, 4.1–5.0 µm and >5.1 µm) simultaneously and can monitor particulate matter concentration during tidal breathing. We report data only for the 0.3–1.0 µm particle size class for simplicity, and because this is close to the size mostly represented in tobacco smoke.11
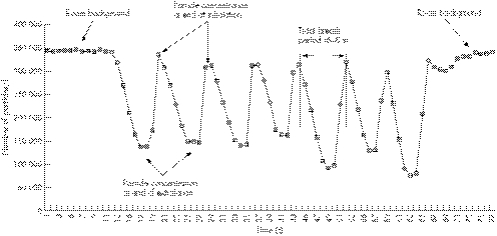
Figure 1 shows an example of exhaled tidal breathing registration for 0.3–1.0 µm ambient air particles. As the analyser needs a continuous and steady sample flow even when the breath flow stops, during the inhalation phase of tidal breathing—while air is not exhaled into the equipment—ambient air is sucked by the analyser pump through a heated pipe connected to the ambient. As the exhaled air is partially depleted from particles owing to their deposition in the lung,10,11 the tracing of exhaled particle concentration shows a sinusoidal pattern in consecutive tidal breaths, with the lower values reflecting exhaled air and the higher values representing ambient air sampled from the reservoir pipe while the subjects are inhaling through the nose. This phenomenon also explains why particle counts of exhaled breath are well below the background level of inhaled ambient air. As mainstream smoke contains an exceptionally high concentration of fine particles (several mg/m3),12 the exhaled particle concentrations during the first few respiratory cycles cannot be considered reliable as our equipment, being a standard particle counter designed to measure the low concentration of clean rooms, has a cut‐off of about 700 000 particles/l. This fact precluded the exact quantification of total RTS as area under curve for each test. However, the system allowed a precise measurement of the washout time.
Figure 1 Example of real‐time measurement of 0.3–1.0 μm particle concentration in the exhaled breath during ambient air tidal breathing.
RTS lung washout time calculation
Ten current smokers were asked to smoke a cigarette as they normally do just outside the laboratory. After taking the last puff, they entered the laboratory room, and started to breath into the equipment mouthpiece, inhaling room air through the nose. An average time (standard deviation (SD)) of 11.1 (1.1) s elapsed between the last puff taken outside and the first exhalation into the equipment, which corresponded to a mean (SD) of 2.3 (0.4) respiratory acts. The washout time was set as the moment when the exhaled particle concentration equalled the mean (SD) of the initial ambient background particle concentration.
Calculation of contribution of RTS to indoor air pollution
We asked five healthy smokers to smoke a cigarette outdoors, downwind, 5 m away from the door of a non‐ventilated laboratory room with a volume of 33.2 m3. About 5 s after the last puff, the volunteers entered the room taking 1–2 breaths outdoors, as they would normally. They closed the door after them, and spent 5 min in the room. Each smoker repeated the test twice, and each test was about 5 min apart from the previous one. The contribution of RTS to indoor pollution was monitored continuously during the 10 consecutive entrances of the smokers. Individual and cumulative increases in indoor particle concentration were measured and compared with incremental background levels. Absolute individual RTS contribution was calculated by subtracting the last background particle concentration from particle concentration after each smoker's entrance, expressed in particle/m3, and multiplied by 33.2 m3, the volume of the room. Ambient particulate matter (2.5) concentrations (μg/m3) were calculated by transforming the number of particles/l of the diameters 0.3–1.0, 1.01–2.00, 2.01–3.0 μm into mass, according to the method described by Morawska et al,13 assuming a mean (SD) density of 1.18 (0.06) g/cm3 for ETS. During the experiments, outdoor and indoor temperatures were stable, 19°C and 22°C, respectively, and indoor relative humidity was 62%.
Results
RTS lung washout time
Table 1 shows the time needed to reach the ambient background basal level for particle concentrations in the exhaled air of 10 different smokers after taking the last puff, together with the number of respiratory acts needed to complete washout. Washout time ranged from 18 to 90 s, with a mean (SD) of 58.6 (23.6) s, whereas the mean (SD) number of breaths required to wash tobacco smoke particles was 8.7 (4.6).
Table 1 Mainstream smoke washout time in 10 consecutive smokers coming back into the laboratory after smoking outdoors.
| Subject | Complete washout time from last puff (s) | Number of respiratory acts to complete washout |
|---|---|---|
| 1 | 31 | 4 |
| 2 | 18 | 3 |
| 3 | 70 | 9 |
| 4 | 49 | 7 |
| 5 | 53 | 7 |
| 6 | 78 | 12 |
| 7 | 90 | 15 |
| 8 | 66 | 8 |
| 9 | 45 | 5 |
| 10 | 86 | 17 |
| Average | 58.6 | 8.7 |
| SD | 23.6 | 4.6 |
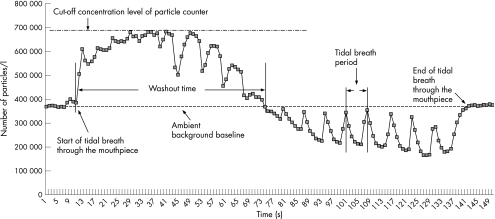
Figure 2 shows a representative graph of particles measured in the exhaled breath after the last puff: particle concentration increased dramatically after starting exhaling into the equipment, reaching the analyser cut‐off value of about 700 000 particles/l that was maintained up to the seventh tidal breathing. In the next few breaths, exhaled particle concentration decreased steadily, reaching background levels at the 10th respiratory act, with a washout time of 66 s after the first exhalation into the instrument, to which about 11 s should be added, considering the time needed to start exhaling into the equipment after the last puff. A high air change per hour rate was maintained to keep particle background concentration levels stable during the whole experiment and to avoid possible interferences on the measurements.
Figure 2 Washout time of 0.3–1.0 μm‐sized particles in the exhaled breath after smoking the last puff, real‐time measurements at tidal breathing.
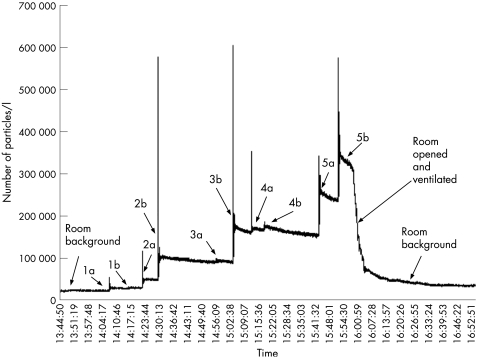
Contribution of RTS to indoor pollution
Figure 3 shows the individual RTS contribution to indoor particulate matter pollution for each entrance of five different smokers after the last puff taken just outside the laboratory room. Variable increments in 0.3–1.0 μm particle concentrations were observed for each subject and for each test, with wide differences that ranged from a few thousand particles/l to about 100 000 particles/l. Table 2 show the subjects' characteristics and their contribution to ETS. Wide variations were found in the individual RTS absolute number of particles, with a mean (SD) of 1402 (1490) million particles (range 51–3611 million). The biggest variation between the two tests of the same subject were observed in subject 3, with a contribution of 96 and 3243 million particles in test a and test b, respectively. The same subject, although showing the smallest vital capacity (3.43 l), was able to contribute a RTS higher than subject 2, who showed the largest lung volume. In addition, no relationship was apparent between RTS and the number of breaths elapsing between the last puff and the test in the same subject.
Figure 3 Increase of indoor 0.3–1.0 μm particle concentration due to RTS. Contribution from five different smokers (two tests each, a and b).
Table 2 Subject characteristics and individual and total contribution of residual tobacco smoke to enviromental tobacco smoke.
| Subject and test | Sex | FEV1(%) | FVC (%) | FVC (l) | Breaths before entrance | Puff number/cigarette | 0.3–1.0 µm particles individual contribution (millions) |
|---|---|---|---|---|---|---|---|
| 1a* | F | 122.1 | 128 | 4.63 | (1) | 8 | 242 |
| 1b† | (2) | 7 | 51 | ||||
| 2a | M | 113 | 129 | 7.02 | (1) | 7 | 676 |
| 2b | (2) | 8 | 2193 | ||||
| 3a | F | 106 | 117 | 3.43 | (2) | 7 | 96 |
| 3b | (1) | 7 | 3243 | ||||
| 4a | M | 101 | 109 | 5.71 | (2) | 8 | 396 |
| 4b | (1) | 9 | 268 | ||||
| 5a | M | 106 | 101 | 4.57 | (1) | 7 | 3245 |
| 5b | (3) | 8 | 3611 | ||||
| Total particle/L supply to the room after 10 re‐entries | 14 026 | ||||||
F, female; FEV1, forced expiratory volumes in 1 s; FVC, forced vital capacity; M, male.
*a, first; and †b, second individual test.
Table 3 shows the size of RTS contribution to the laboratory room with regard to the variation in indoor pollution. Starting from a mean (SD) background of 22 283 (943) particles/l of size 0.3–1.0 μm, the incremental addition of RTS contributed to a final 341 956 (51 973) particles/l after 10 entrances (p<0.001). When expressed in mass concentration, RTS increased room pollution from 0.56 to 3.32 µg/m3, with a net increase of 2.76 µg/m3, wheras the average (SD) RTS emission rate per smoker was 11.47 (9.59) µg, ranging from 2.25 to 26.69 µg (independently from gravitational sedimentation and room air exchange rate).
Table 3 Increase in indoor particle and aerosol mass concentration due to individual residual tobacco smoke after 10 consecutive re‐entries after the last puff.
| 0.3–1.0 µm particles/l | PM2.5 µg/m3 | |
|---|---|---|
| Initial room concentration | 22283 | 0.56 |
| Subjects | RTS individual supply | RTS individual supply |
| 1, test a | 7316 | 0.23 |
| 1, test b | 1561 | 0.07 |
| 2, test a | 20384 | 0.25 |
| 2, test b | 66056 | 0.53 |
| 3, test a | 2916 | 0.07 |
| 3, test b | 97685 | 0.68 |
| 4, test a | 11937 | 0.11 |
| 4, test b | 8060 | 0.08 |
| 5, test a | 97767 | 0.66 |
| 5, test b | 108788 | 0.81 |
| Final room concentration | 341956 | 3.32 |
PM, particulate matter; RTS, residual tobacco smoke.
Discussion
The special health risk of fine particles for subsets of people such as children with asthma has been shown,14,15 and the contribution of ETS to indoor particulate matter (2.5) pollution has been quantified.16 Moreover, more stringent limits are invoked for fine particle concentration in the USA.17 ETS has been shown to worsen even outdoor air quality especially when smokers gather in patios or open spaces in outdoor restaurants, with definite carcinogenic risk.18 Therefore, any unwanted source of ETS should be avoided. The relevance of the particulate matter that is left behind in the lung after taking the last puff has not been previously assessed.9,12 In this paper, we could monitor particle concentration in real time in the exhaled air at tidal breathing after the last puff, by using an innovative instrument based on recent technology that allows particle count at a sampling rate of 1 s.10 Thus, excess particle concentration due to RTS could be followed in the exhaled air for each breath until the concentration returned to ambient background levels. With such a technique, we found a lung washout time in the range of 18–90 s for particles sized 0.3–1.0 μm, which are the most representative size class in tobacco smoke. This result compares with that of the clearance of volatile organic compounds from the breath of smokers, which has been estimated in the range of 0.9–3 min for the blood compartment.7,8
The contribution of RTS to indoor fine particle pollution when smokers enter enclosed spaces just after taking the last puff was considerable, both as regards the number of fine particles added to the environment and as particulate matter mass. In fact, the final indoor concentration of about 350 000 particles/l after the RTS contribution from the last smoker represented more than a 10‐fold increase over the initial background level of about 22 000 particles/l. Although our experimental setting dealt with a non‐ventilated room of small volume (33.2 m3), these figures raise concern for putatively smoke‐free workplaces and public places where many smokers are expected to enter indoors soon after smoking, as the final increase over background pollution of 2.76 µg/m3 in particulate matter (2.5) in our non‐ventilated room represents about 20% of the outdoor air quality limit (USA on yearly basis) of 15 µg/m3.17 According to our data, no relationship was found between the number of puffs taken, number of breaths after the last puff before entrance, lung capacity of the smokers and their individual contribution to ETS—as exemplified by the fact that subject 3 showed the smallest lung capacity, but was able to contribute a huge RTS particle load in the second test, and subject 5 contributed considerably to ETS even though he took three breaths before entering the room for the second test. The observed wide differences between RTS contributions of the two individual tests could be explained by the fact that RTS depends mainly on how deep is the last puff, and this event is subject to many variables. The possible contribution to the increase in particle concentration by tobacco smoke plume enveloping the smokers should be considered.18 However, as the smokers stayed outdoors, downwind, and 5 m away from the door, its role should be trivial.
What is already known on this topic
Smoking policy restrictions do not allow people to smoke in smoke‐free places to prevent indoor air pollution from environmental tobacco smoke. Consequently, smokers gather to smoke just outside public places and workplaces, and usually re‐enter immediately after drawing the last cigarette puff.
what this study adds
This study shows that, after smoking a cigarette, the lung continues to release particulate matter from tobacco smoke in the ambient for up to 90 s with each subsequent exhaled breath. This “residual tobacco smoke” is a hidden source of environmental tobacco smoke and can contribute substantially to indoor pollution.
Conclusions
Our work sheds light on a hidden aspect of tobacco smoking—that is, the residual smoke in the lung—that should be considered to be an additional cause of ETS pollution in smoke‐free places. We acknowledge that, taken as an absolute value, the exposure level measured for 10 re‐entries (2.76 µg/m3 in particulate matter (2.5)) is much lower than the concentrations measured in smoke‐free environments and may not have clinical or public health significance. However, even these low concentrations may be of concern in some particularly sensitive subjects. Furthermore, even a small increase in PM concentrations may not be negligible when added to already existing raised particulate matter levels. Further studies should be carried out to investigate possible policy or practical implications, even though simply waiting about 2 min before re‐entry would be enough to avoid an unwanted additional exposure for non‐smoking people.
Abbreviations
ETS - environmental tobacco smoke
RTS - residual tobacco smoke
Footnotes
Funding: The work has been funded by National Cancer Institute and SIMG, Milan, Italy.
Competing interests: None declared.
References
- 1.Repace J L, Lowrey A H. Indoor air pollution, tobacco smoke, and public health. Science 1980208464–472. [DOI] [PubMed] [Google Scholar]
- 2.Kunzli N. The public health relevance of air pollution abatement. Eur Respir J 200220198–209. [DOI] [PubMed] [Google Scholar]
- 3.Barnoya J, Glantz S A. Cardiovascular effects of secondhand smoke: nearly as large as smoking. Circulation 20051112684–2698. [DOI] [PubMed] [Google Scholar]
- 4.Invernizzi G, Ruprecht A, Mazza R.et al Real‐time measurement of indoor particulate matter originating from environmental tobacco smoke: a pilot study. Epidemiol Prev 2002262–6. [PubMed] [Google Scholar]
- 5.Invernizzi G, Ruprecht A, Mazza R.et al Particulate matter from tobacco versus diesel car exhaust: an educational perspective. Tob Control 200413305–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allwright S, Paul G, Greiner B.et al Legislation for smoke‐free workplaces and health of bar workers in Ireland: before and after study. BMJ 2005121117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wallace L, Buckley T, Pellizzari E.et al Breath measurements as volatile organic compound biomarkers. Environ Health Perspect 1996104(Suppl 5)861–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gordon S M, Wallace L A, Brinkman M C.et al Volatile organic compounds as breath biomarkers for active and passive smoking. Environ Health Perspect 2002110689–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker M, Dixon M. The retention of tobacco smoke constituents in the human respiratory tract. Inhal Toxicol 200617255–294. [DOI] [PubMed] [Google Scholar]
- 10.Invernizzi G, Ruprecht A, Boffi R.et al Real time measurement of particulate matter deposition in the lung. Biomarkers 200611221–232. [DOI] [PubMed] [Google Scholar]
- 11.Morawska L, Barron W, Hitchins J. Experimental deposition of environmental tobacco smoke submicrometer particulate matter in the human respiratory tract. Am Ind Hygiene Assoc J 199960334–339. [DOI] [PubMed] [Google Scholar]
- 12.Bernstein D M. A review of the influence of particle size, puff volume, and inhalation pattern on the deposition of cigarette smoke particles in the respiratory tract. Inhal Toxicol 200416675–689. [DOI] [PubMed] [Google Scholar]
- 13.Morawska L, Johnson G, Ristovski Z D.et al Relation between particle mass and number for submicrometre airborne particles. Atmos Environ 1999331983–1990. [Google Scholar]
- 14.Schwartz J, Neas L M. Fine particles are more strongly associated than coarse particles with acute respiratory health effects in schoolchildren. Epidemiology 2000116–10. [DOI] [PubMed] [Google Scholar]
- 15.Delfino R J, Quintana P J E, Floro J.et al Association of FEV1 in asthmatic children with personal and microenvironmental exposure to airborne particulate matter. Environ Health Perspect 2004112932–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wallace L A, Mitchell H, O'Connor G T.et al Particle concentrations in inner‐city homes of children with asthma: the effect of smoking, cooking, and outdoor pollution. Environ Health Perspect 20031111265–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson P R, Graham J J. Fine particulate matter national ambient air quality standards: public health impact on populations in the northeastern United States. Environ Health Perspect 20051131140–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Repace J. Estimated mortality from secondhand smoke among club, pub, tavern, and bar workers in New South Wales, Australia. A report commissioned by The Cancer Council New South Wales. 7 April 2004. http://www.repace.com/pdf/NSWReport2004.pdf (accessed 5 Oct 2006)