Abstract
Objective
To compare trends in African‐American (AA) and non‐Hispanic white (NHW) smoking between states categorised as having three different levels of tobacco control practice in the 1990s.
Setting and participants
Analysis of 1992–3 to 2001–2 Tobacco Use Supplements to the Current Population Survey for differences in adult (20–64 years) daily smoking prevalence for AAs and NHWs across states: California (CA; high cigarette price/comprehensive programme), New York (NY) and New Jersey (NJ; high cigarette price/no comprehensive programme), and tobacco growing states (TGS; low cigarette price/no comprehensive programme).
Results
From 1992–3 to 2001–2, there were large declines in AA smoking across states (2.7–3.8% decrease/year, adjusted for age, income, education, gender; p<0.05). Adjusted NHW smoking prevalence declined significantly only in CA. AA prevalence declined significantly and did not differ across state groups. In all years, in all state groups, adjusted prevalence was either not significantly different or was lower for AAs than for NHWs. More recent cohorts of AAs appeared to have taken up smoking at lower rates than older cohorts.
Conclusion
There were uniformly large declines in AA smoking from 1992–3 to 2001–2 across states, independent of type of tobacco control strategy. Further research is needed into factors associated with smoking declines among AAs.
Historically, smoking prevalence and smoking‐related diseases have been higher in the US African‐American (AA) adult population compared with the non‐Hispanic white (NHW) population.1,2 However, in recent years the prevalence gap between AAs and NHWs has closed.3 Apparently, lower initiation rates among AAs have persisted resulting in lower adult prevalence rates.4,5 These changes in AA smoking behaviour may be due to an increased response to tobacco control measures, including higher cigarette prices. An important question is how the smoking rates have changed for AAs and for NHWs across states with different tobacco control strategies.
The first comprehensive state‐wide tobacco control programme designed to increase social norms against smoking in the US began in California (CA) in 1989.6 This programme was unique in spending an average of US$3 per person per year on a public health programme to discourage smoking through the 1990s.7 It is the largest and the longest running programme in the US and its components include mass‐media programmes, clean indoor air laws, community and school programmes, and increased excise taxes. Thus, it might be expected that CA would have shown a greater reduction in smoking than states without such a tobacco control programme.
New York (NY) and New Jersey (NJ) are adjacent states with a combined population size similar to CA. Neither state supported a major tobacco control programme in the 1990s, but both were similar to CA in the amount of excise tax levied on cigarettes8 and had similar high cigarette prices during the 1990s. It might be expected that these states would also have greater reductions in smoking than states with lower excise taxes during the study period.
There are six US states that had significant economic activity (>US$100 million/year) from tobacco‐related agriculture during the study period.9 These tobacco‐growing states (TGS) were Kentucky, Tennessee, North Carolina, South Carolina, Virginia and Georgia, which together had a population slightly larger than either CA or NY and NJ. The TGS have consistently had some of the lowest excise taxes in the nation,8 and none had a major state‐specific tobacco control programme in the 1990s. There is also evidence that social norms are more supportive of tobacco use in these tobacco‐growing regions.10
We used data from the Tobacco Use Supplements (TUS) to the Current Population Survey (TUS–CPS) from 1992–3 to 2001–2 to examine age‐specific smoking rates and particularly, how reductions in AA initiation previously reported for the 1980s and 1990s might be impacting prevalence rates compared to those among the NHW population. We compared trends for CA, a state with a comprehensive programme designed to increase social norms against smoking, with NY and NJ, states that markedly increased the price of cigarettes during this time period but limited tobacco control activity, and with the TGS, serving as a control group of states with low prices and limited state‐wide tobacco control activities.
Methods
Data sources
TUS are periodically added to the national CPS, which was the source of the data for this analysis. The CPS is a continuous survey (over 56 000 households/month) conducted by the US Bureau of the Census, primarily to monitor labour force indicators for the civilian non‐institutionalised US population aged ⩾15 . The complete CPS method is published elsewhere.11 Briefly, the CPS includes a probability sample, based on a stratified sampling scheme of clusters of four neighbouring households identified from the most recent decennial census, updated from building permits and other sources. The TUS‐CPS was included for the months of September, January and May in 1992–3, 1995–6, 1998–9, and June, November and February of 2001–2. The TUS was developed by the staff of the National Cancer Institute and pretested by trained interviewers of the Bureau of the Census prior to implementation. In this study, we use data from in‐person interviews from all respondents aged 20–64 years identified as either AA or NHW.
Smoking
The respondents of TUS survey were asked, “Have you ever smoked 100 cigarettes?” and respondents were considered ever smokers if they answered yes to this question. Ever smokers were further asked, “Do you now smoke every day, some days, or not at all?” Those who reported smoking every day were considered current daily smokers, whereas those who reported smoking on some days were considered current occasional smokers.
Statistical methods
We examined trends in the prevalence of daily smoking over time from 1992–3 to 2001–2 for AAs and NHWs aged 20–64 years for CA, NY and NJ combined and the combined TGS of Georgia, Kentucky, North Carolina, South Carolina, Tennessee and Virginia. We also compared trends in the prevalence of daily smoking by age (20–64 years) for 1992–3 and 2001–2 to see how this distribution changed over time.
All estimates were weighted by TUS‐CPS survey weights which account for selection probabilities from the sampling design and adjust for survey non‐response.11,12 All estimates were computed in SAS‐callable SUDAAN V.9.0.1, and variance estimates were computed using the published TUS‐CPS replicate weights with Fay's balanced repeated replication.11,13 We combined the unequally sized sets of replicate weights from the different surveys by appending full sample weights as necessary (details available from the authors on request). Unadjusted smoking prevalence was computed as a weighted proportion using PROC CROSSTABS. Trends in adjusted smoking prevalence were assessed using weighted logistic regression, computed using PROC RLOGIST. Time trends in prevalence were compared between state groups using a weighted logistic regression model containing separate time slopes and intercepts for each state group, fit separately for AAs and for NHWs (table 2). The relative odds of daily smoking for AAs versus NHWs was compared between state groups in 1992–3 and in 2001–2, using a weighted logistic regression model containing a state group by race by time interaction term (table 3). All logistic regression models adjusted for age (20–34, 35–49 and 50–64 years), education (less than high school, high school graduate, some college, college graduate), gender, family income in constant 2001 dollars, and a binary variable for household income above twice the Census Bureau poverty threshold (by size of family and number of children)14 using standard demographics collected on the CPS.
Table 2 Estimated annual trends in odds of daily smoking for African‐Americans and non‐Hispanic whites, 1992–3 to 2001–2, comparing California, New York and New Jersey and tobacco‐growing states.
| Change % /year in odds of daily smoking (95% CI) | ||
|---|---|---|
| AAs | NHWs | |
| CA | –3.8 (–0.7 to –6.8) | –2.2 (–0.8 to –3.4) |
| NY and NJ | –3.5 (–2.2 to –4.9) | +0.7 (0 to +1.3) |
| TGS | –2.7 (–0.6 to –4.7) | +0.4 (–0.5to +1.3) |
AA, African‐American; CA, California; NHW, non‐Hispanic white; NJ, New Jersey; NY, New York; TGS: tobacco‐growing states (Kentucky, Tennessee, North Carolina, South Carolina, Virginia and Georgia).
Estimated trends from weighted logistic regression adjusting for age, gender, education and income.
Models fit separately for AAs and for NHWs.
Table 3 Relative odds of daily smoking for African Americans and non‐Hispanic whites, 1992–3 and 2001–2, comparing California, New York and New Jersey and tobacco‐growing states.
| Adjusted odds of daily smoking (95% CI) | |||
|---|---|---|---|
| 1992–3 | 2001–2 | ||
| CA | NHW | 1.00 | 1.00 |
| AA | 0.81 (0.70 to 0.95) | 0.74 (0.60 to 0.92) | |
| NY and NJ | NHW | 1.00 | 1.00 |
| AA | 0.60 (0.54 to 0.66) | 0.47 (0.40 to 0.56) | |
| TGS | NHW | 1.00 | 1.00 |
| AA | 0.56 (0.51 to 0.62) | 0.41 (0.37 to 0.46) | |
AA, African‐American; CA, California; NHW, non‐Hispanic white; NJ, New Jersey; NY, New York; TGS, tobacco‐growing states (Kentucky, Tennessee, North Carolina, South Carolina, Virginia and Georgia).
Relative odds from weighted logistic regression adjusting for age, gender, education and income.
Results
Table 1 presents the demographic characteristics of the study population from each CPS . The AA population in each CPS year increased slightly from 17.0% (±95% CI 0.5%) in 1992–3 to 18.8% (0.8%) in 2001–2, whereas the proportion of NHWs decreased slightly from 83.1% (0.5%) to 81.2% (0.8%). The average age of AA respondents in each CPS year was slightly less than that of NHWs. Although the gender distribution among NHWs was fairly equal in each CPS year, there were significantly fewer male respondents among the AA population in each year.
Table 1 Characteristics of study population in the Tobacco Use Supplement of the Current Population Survey.
| 1992–3 | 1995–6 | 1998–9 | 2001–2 | |||||
|---|---|---|---|---|---|---|---|---|
| AA (±95% CI) | NHW (±95% CI) | AA (±95% CI) | NHW (±95% CI) | AA (±95% CI) | NHW (±95% CI) | AA (±95% CI) | NHW (±95% CI) | |
| n (unweighted) | 6255 | 37 100 | 4931 | 27 931 | 4511 | 24 302 | 4338 | 21 781 |
| % study population (weighted) | 17.0 (0.5) | 83.1 (0.5) | 17.5 (0.6) | 82.5 (0.6) | 18.3 (0.6) | 81.7 (0.6) | 18.8 (0.8) | 81.2 (0.8) |
| Average age (years) | 38.3 (0.2) | 40.1 (0.1) | 38.4 (0.3) | 40.7 (0.2) | 39.1 (0.4) | 41.4 (0.2) | 39.4 (0.4) | 41.6 (0.2) |
| Gender | ||||||||
| Male | 44.6 (0.8) | 49.1 (0.3) | 44.7 (1.0) | 49.5 (0.4) | 44.3 (1.3) | 49.3 (0.5) | 46.1 (1.1) | 49.2 (0.5) |
| Female | 55.5 (0.8) | 50.9 (0.3) | 55.3 (1.0) | 50.5 (0.4) | 55.7 (1.3) | 50.7 (0.5) | 53.9 (1.1) | 50.8 (0.5) |
| Smoking prevalence* | ||||||||
| CA | 28.4 (2.4) | 23.7 (0.9) | 25.2 (4.1) | 22.1 (1.3) | 24.0 (3.8) | 21.4 (1.6) | 20.7 (4.1) | 18.7 (1.5) |
| NY and NJ | 26.3 (1.4) | 25.4 (0.8) | 26.1 (2.1) | 24.9 (1.2) | 23.2 (3.0) | 25.7 (1.1) | 21.1 (3.2) | 23.2 (1.2) |
| TGS | 29.7 (1.4) | 31.0 (1.0) | 24.1 (1.9) | 30.3 (1.0) | 21.6 (2.1) | 27.9 (0.9) | 21.9 (1.9) | 28.5 (1.0) |
AA, African‐American; CA, California, NHW, non‐Hispanic white; NJ, New Jersey; NY, New York; TGS, tobacco‐growing states (Georgia, Kentucky, North Carolina, South Carolina, Tennessee and Virginia).
*Daily and occasional smoking.
Trends in current smoking prevalence
Overall unadjusted current smoking prevalence rates (daily and occasional smoking combined) for AAs and for NHWs are included in table 1. During 1992–3, in CA, the unadjusted current smoking rate for AAs was significantly higher than for NHWs (28.4% (2.4%) vs 23.7% (0.9%)) but not in subsequent survey years as rates declined (2002 prevalence 20.7% (4.1%) vs 18.7% (1.5%)). In NY and NJ, unadjusted smoking rates also declined over time, and there were no significant differences between AAs and NHWs in any year, as indicated by overlapping CIs (2002 prevalence 21.1% (3.2%) vs 23.2% (1.2%)). Although unadjusted smoking rates in TGS were not significantly different between AAs and NHWs in 1992–3 (29.7% (1.4%) vs 31.0% (1.0%)), as rates declined in subsequent years, they became significantly lower for AAs as compared with NHWs (2002 prevalence 21.9% (1.9%) vs 28.5% (1.0%)).
Trends in current daily smoking prevalence
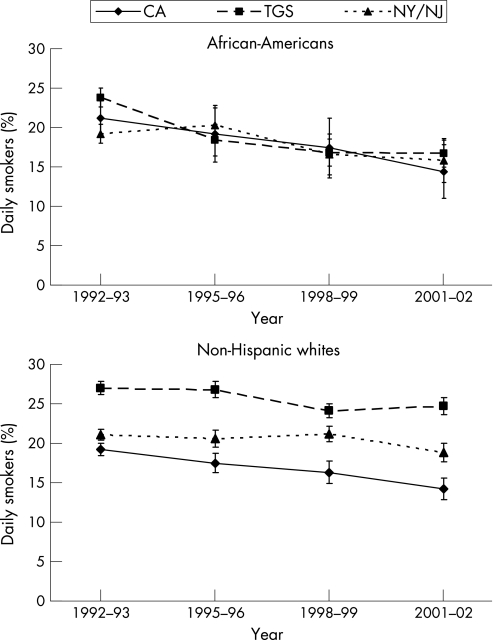
The top panel of figure 1 shows that the unadjusted daily smoking rates for AAs did not differ significantly, determined by overlapping CIs, across the groups of states during the study period. Further, in all state groups AA daily smoking showed similar strong declines over the study period. This is confirmed from logistic regression results presented in table 2, where the adjusted estimated rates of decrease in the odds of daily smoking were similar for the three groups of states (2.7–3.8% per year; combined estimate 3.3% per year, 95% CI 2.3% to 4.4%), showing no statistically significant differences (p>0.50 from the logistic regression model).
Figure 1 Unadjusted prevalence of daily smoking for African‐American and non‐Hispanic white adults (20–64 years) across states with differing tobacco control strategies, 1992–3 to 2001–2. CA, California; NJ, New Jersey; NY, New York; TGS, tobacco‐growing states.
By contrast, the bottom panel of figure 1 shows that unadjusted daily smoking prevalence for NHWs differed between the groups of states in all survey years, with rates in the TGS higher than in NY and NJ, and in NY and NJ higher than in CA. Table 2 shows that for NHWs, only CA showed a significant decline in the adjusted odds of daily smoking (2.2% per year, 95% CI 0.8 to 3.4), and the size of the trend was similar to that seen for AAs. Neither NY and NJ nor the TGS showed a decrease in the adjusted odds of daily smoking during the study period.
These differences between the state groups in time trends for the two ethnic groups are reflected in the changing adjusted odds of daily smoking for AAs relative to NHWs, as shown in table 3. In CA, the odds of daily smoking for AAs were about 70–80% of those of similar NHWs, adjusting for income, education, gender and age; and this odds ratio did not change significantly from 1992–3 to 2001–2 (p>0.50). In NY and NJ, the adjusted odds of daily smoking for AAs was 60% that of similar NHWs, and this dropped to <50% by the end of the study period (p<0.05). In the TGS, the adjusted odds changed from about 55% in 1992–3, to nearly 40% by 2001–2 (p<0.01). In each of these models, the risk for daily smoking increased as the level of education and income decreased, and males were at greater risk for daily smoking.
Daily smoking prevalence by age
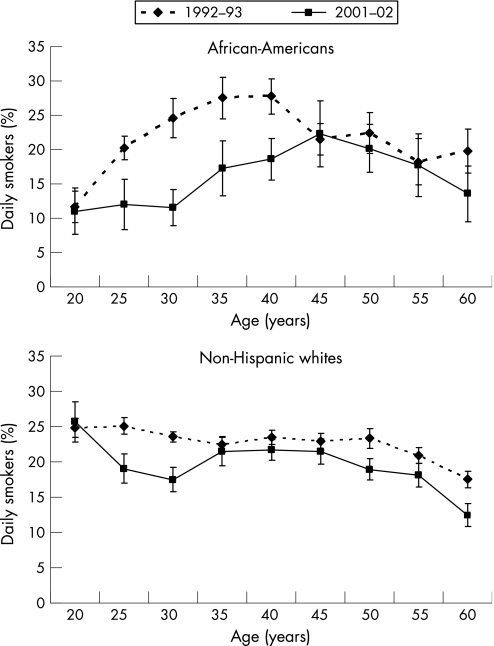
Figure 2 shows the unadjusted prevalence of daily smoking by age for AAs (top panel) and NHWs (bottom panel), for the 1992–3 survey (dotted line) and the 2001–2 survey (solid line). For AAs, in 1992–3, the peak age range of daily smoking was between 35 and 40 years, with a prevalence of about 28%. However, by 2001–2, as the earlier cohort aged, the peak age range of daily smoking shifted to between 45 and 50 years, with a prevalence of about 22%. Also, in 2001–2 the prevalence of daily smoking for AAs aged 20–30 years was stable at approximately 10% before beginning to climb at the age of 35 years. By contrast, in 1992–3, the prevalence rose strongly from age 20 to 30 years, a rise that is mirrored in 2001–2 from age 30 to 40 years. These changing patterns of prevalence with age show that recent, younger AA cohorts have daily smoking rates much lower than those of earlier cohorts. By contrast, there was no such shift in the age distribution of daily smoking for NHWs, although daily smoking prevalence rates by age were generally slightly lower in 2001–2 than a decade earlier.
Figure 2 Unadjusted prevalence of daily smoking by age for African Americans and non‐Hispanic whites for California, New York and New Jersey and tobacco‐growing states combined.
Discussion
There was a strong, sustained and uniform decline in the adjusted odds of AA adult daily smoking, by 3% per year in the decade from 1992–3 to 2001–2, across state groups with very different approaches to tobacco control. In each of these disparate state groups, rates of daily smoking among AAs are now substantially less than those for NHWs of similar age, education and income status. Further, in these states, daily smoking rates for AAs have been less than or equal to rates for NHWs since at least 1992–3.
When we compared the age‐specific rates of daily smoking, there seems to be a strong birth cohort effect that extends through the age 40 years in 2002. Importantly, there was no significant difference in occasional smoking behaviour between either group. Thus, the most likely explanation for this very large effect is that AAs aged <40 years in 2002 never became smokers in the first place. Many studies have noted that cohorts of AAs since the 1970s have had much lower initiation rates than NHWs1,5,15 and our analysis demonstrates the time that it takes for this lower initiation rate to affect prevalence. Indeed, it is only recently that the Centers for Disease Control and Prevention has documented the elimination of a long‐term higher smoking prevalence among AA and NHW adults.3
Our goal was to compare the effectiveness of a comprehensive tobacco control programme (CA) versus price‐centred programmes (NY and NJ) with the TGS as control states in reducing adult AA and NHW smoking prevalence rates over time. Given the differences in the emphasis of state tobacco control programme, we expected that the reduction in daily smoking rates would differ by state group. Indeed, for NHWs, the decreases in daily smoking rates varied by state group depending on the tobacco control strategies, with CA showing the greatest reductions even after controlling for potentially confounding demographic differences. This finding supports previous research showing the effectiveness of the California Tobacco Control Program in changing social norms and reducing both initiation and prevalence of smoking.16,17 However, we found that among AAs, there have been large and fairly uniform declines in daily smoking prevalence across the state groups we examined, regardless of the type of tobacco control strategies.
Our analysis of the age‐specific data in 1992 compared with 2002 has demonstrated that the decline in AA smoking may be coming mainly from a cohort effect of a major reduction in smoking among people born after 1960. Such a decline in AA initiation has previously been reported for CA.4 In addition, it has been observed that, throughout the 1990s, AA adult smokers were less likely to successfully quit than NHWs.4 Therefore, it is unlikely that the observed age‐specific changes could have resulted from increased rates of quitting.
As the window of initiation has been documented to be closed by the mid‐20s,18 this large initiation effect occurred prior to the study period under consideration (ie, started in the 1970s–1980s). Further, the effect has been so large that it probably would overpower any effect of a tobacco‐control programme or price on quitting behaviours. To address whether there was a difference in quitting among AAs requires a different analysis and will be the subject of a future study. However, the time that it has taken for this initiation effect to change the overall prevalence rate among AAs suggests that the prevalence rates among NHWs in CA will continue to decline rapidly in future years, as the programme has been shown to have had a major effect on initiation.17 Whether or not the tobacco control programme influenced AA initiation in a similar manner would also need to await future surveys.
It is also possible that the lack of difference in AA smoking trends across the states resulted from the fact that AA smoking patterns were not sensitive to price. It is possible that the effect of differences in cigarette prices between the states was muted because of the more efficient way that AAs seem to smoke their cigarettes (eg, lower daily cigarette consumption yet higher blood levels of nicotine).19 However, differences in the efficiency of smoking for AAs in various US regions have not been reported. Another possibility is that the AA community has become somewhat immune to the promotional efforts of the tobacco industry. A community‐wide AA reaction was observed before the CA campaign in response to the use of cultural images in the marketing of Uptown cigarettes.20,21,22 Additional research into tobacco industry marketing receptivity over time among AAs is necessary.
Limitations
It has been noted that young adult males (aged 20–29 years) have, for many years, had a relatively lower coverage rate in the CPS than other demographic groups, particularly among minority populations.11 This may account for the observed gender difference in the AA sample that is not present among NHWs. However, there is no evidence that relative coverage rates have changed over time,23 and the trends in smoking behaviour presented here did not differ significantly by gender. Thus, any difference in response rates by gender would have minimal effect on these results. Additionally, the CPS data that we use are from self‐reported surveys, and as such, may be affected by trends in social desirability bias. If respondents are increasingly reluctant to report smoking then this may exaggerate the actual decline in smoking prevalence. However, there was no decline in reported occasional smoking among AAs, and it is unlikely that such biases could account for the magnitude of the trends presented here.
Conclusion
This is the first study to examine the disparity in AA and NHW smoking prevalence across groups of states with varying tobacco control strategies and efforts. There were uniformly large annual rates of decline in AA adult daily smoking from 1992–3 to 2001–2 across states, regardless of the type of state‐wide tobacco control strategy. Further, the more recent cohort of AAs does not seem to take up daily smoking at the same rate as did earlier groups. Future research on factors that may have contributed to these declines is warranted. Because of these declines, we could expect that tobacco‐related disease rates for AAs will decrease more rapidly than for NHWs in the medium‐term future.
What this paper adds
Historically, smoking prevalence rates have been higher in the US African‐American (AA) adult population compared to the non‐Hispanic white (NHW) population. However, in recent years, the prevalence gap between AAs and NHWs has closed.
We examined how smoking rates have changed for AAs and for NHWs across states with differing tobacco control strategies: California (CA; high cigarette price/comprehensive programme), New York (NY) and New Jersey (NJ; high cigarette price/no comprehensive programme), and tobacco‐growing states (TGS; low cigarette price/no comprehensive programme).
There were uniformly large declines in AA smoking from 1992–3 to 2001–2 across states, independent of type of tobacco control strategy, whereas adjusted NHW smoking prevalence declined significantly only in CA.
Findings suggest that more recent cohorts of AAs appeared to have taken up smoking at lower rates than older cohorts. Further research is needed to look into factors associated with smoking declines among AAs and may be of benefit to the other population groups.
Abbreviations
AA - African‐American
CPS - Current Population Survey
NHW - non‐Hispanic white
TGS - tobacco‐growing states
TUS - Tobacco Use Supplements
TUS–CPS - Tobacco Use Supplements to the Current Population Survey
Footnotes
Funding: This study was supported by two Tobacco‐Related Disease Research Program grants (12KT‐0158, 12RT‐0082 and 15RT‐0238) from the University of California, California, USA.
Competing interests: None.
The granting agency (Tobacco‐Related Disease Research Program) did not have any role in either design or conduct of the study or preparation, review or approval of the manuscript.
References
- 1.US Department of Health and Human Services Tobacco use among US racial/ethnic minority groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: a report of the Surgeon General. pp. 017–01005274.
- 2.US Department of Health and Human Services Reducing Tobacco use. A report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2000 (S/N 017–01–0544–4),
- 3.Centers for Disease Control and Prevention Prevalence of cigarette use among 14 racial/ethnic populations—United States, 1999–2001. Morbid Mortal Wkly Rep 20045349–52. [PubMed] [Google Scholar]
- 4.Trinidad D R, Gilpin E A, White M M.et al Why does adult African‐American smoking prevalence in California remain higher than for non‐Hispanic whites? Ethn Dis Summer 200515505–511. [PubMed] [Google Scholar]
- 5.Trinidad D R, Gilpin E A, Lee L.et al Has there been a delay in the age of regular smoking onset among African Americans? Ann Behav Med 200428152–157. [DOI] [PubMed] [Google Scholar]
- 6.Bal D G, Kizer K W, Felten P G.et al Reducing tobacco consumption in California. J Am Med Assoc 19902641570–1574. [PubMed] [Google Scholar]
- 7.Tobacco Education and Research Oversight Committee Toward a tobacco‐free California: strategies for the 21st Century 2000–2003. 2000.
- 8.Orzechowski W, Walker R C.The tax burden on tobacco. Historical compilation. Vol 39. Arlington, VA: Orzechowski & Walker, 2004
- 9.US Department of Agriculture Trends in U.S. tobacco farming. pp. TBS257–NaN02.
- 10.Noland M P, Kryscio R J, Hinkle J.et al Relationship of personal tobacco‐raising, parental smoking, and other factors to tobacco use among adolescents living in a tobacco‐producing region. Addict Behav 199621349–361. [DOI] [PubMed] [Google Scholar]
- 11.Bureau of Labor Statistics, US Census Bureau Current population survey: design and methodology. Washington, DC: US Department of Commerce, 2002, Technical paper 63RV,
- 12.US Department of Commerce Census Bureau, National Cancer Institute and Centers for Disease Control and Prevention Co‐sponsored Tobacco Use Supplement to the Current Population Survey (2001–2002): Current Population Survey, June 2001, November 2001, and February 2002: Tobacco Use Supplement file technical documentation Appendix 17. http://www.census.gov/apsd/techdoc/cps/capJun01Nov01Feb02.pdf (accessed 7 Feb 2007)
- 13.Judkins J R. Fay's method for variance estimation. J Official Stat 19906223–239. [Google Scholar]
- 14.US Census Bureau Housing and Household Economic Statistics Division. http://www.census.gov/hhes/www/poverty/threshld.html (accessed 9 Feb 2007)
- 15.Anderson C, Burns D M. Patterns of adolescent smoking initiation rates by ethnicity and sex. Tob Control 20029(Suppl 2)II4–II8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilpin E A, Lee L, Pierce J P. Changes in population attitudes about where smoking should not be allowed: California versus the rest of the USA. Tob Control 20041338–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pierce J P, White M M, Gilpin E A. Adolescent smoking decline during California's Tobacco Control Program. Tob Control 200514207–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilpin E A, Lee L, Evans N P.et al Smoking initiation rates in adults and minors: United States, 1944–88. Am J Epidemiol 1994140535–543. [DOI] [PubMed] [Google Scholar]
- 19.Perez‐Stable E J, Herrera B, Jacob P I I I.et al Nicotine metabolism and intake in black and white smokers. JAMA 1998280152–156. [DOI] [PubMed] [Google Scholar]
- 20.Robinson R G. Community development model for public health applications: overview of a model to eliminate population disparities. Health Promot Pract 20056338–346. [DOI] [PubMed] [Google Scholar]
- 21.Gardiner P S. African American teen cigarette smoking: a review. Changing adolescent smoking prevalence. Smoking Tob Control Monogr 200114213–226. [Google Scholar]
- 22.Balbach E D, Gasior R J, Barbeau E M. R.J. Reynolds' targeting of African Americans: 1988–2000, Am J Public Health 200393822–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biener L, Garrett C A, Gilpin E A.et al Consequences of declining survey response rates for smoking prevalence estimates. Am J Prev Med 200427254–257. [DOI] [PubMed] [Google Scholar]