Abstract
Objective
To describe prospective transitions in smoking among young adult women who were occasional smokers, and the factors associated with these transitions, by comparing sociodemographic, lifestyle and psychosocial characteristics of those who changed from occasional smoking to daily smoking, non‐daily smoking or non‐smoking.
Design
Longitudinal study with mailed questionnaires.
Participants/setting
Women aged 18–23 years in 1996 were randomly selected from the Medicare Australia database, which provides the most complete list of people in Australia.
Main outcome measures
Self‐reported smoking status at survey 1 (1996), survey 2 (2000) and survey 3 (2003), for 7510 participants who took part in all three surveys and who had complete data on smoking at survey 1.
Results
At survey 1, 28% (n = 2120) of all respondents reported smoking. Among the smokers, 39% (n = 829) were occasional smokers. Of these occasional smokers, 18% changed to daily smoking at survey 2 and remained daily smokers at survey 3; 12% reported non‐daily smoking at surveys 2 and 3; 36% stopped smoking and remained non‐smokers; and 33% moved between daily, non‐daily and non‐smoking over surveys 2 and 3. Over the whole 7‐year period, approximately half stopped smoking, one‐quarter changed to daily smoking and the remainder reported non‐daily smoking. Multivariate analysis identified that a history of daily smoking for ⩾6 months at baseline predicted reversion to daily smoking at follow‐up. Being single and using illicit drugs were also associated with change to daily or non‐daily smoking, whereas alcohol consumption was associated with non‐daily smoking only. Compared with stopping smoking, the change to daily smoking was significantly associated with having intermediate educational qualifications. No significant associations with depression and perceived stress were observed in the multivariate analysis.
Conclusions
Interventions to reduce the prevalence of smoking among young women need to take account of occasional smokers, who made up 39% of all smokers in this study. Targeted interventions to prevent the escalation to daily smoking and to promote cessation should allow for the social context of smoking with alcohol and other drugs, and social and environmental influences in vocational education and occupational settings.
The transition to young adulthood is a critical period in establishing patterns of tobacco use, with the prevalence of smoking increasing through to the mid‐1920s.1,2 It is a time when there are opportunities to prevent smoking and to promote cessation among those who may be amenable to quitting before they become committed smokers.3 The tobacco industry also sees the passage to young adulthood as an opportune time—but for the adoption and consolidation of smoking habits.4
Among adolescents and young adults, occasional smoking is often regarded as a transitional, experimental phase preceding daily smoking, and rates of occasional smoking are generally higher among younger adults than among older adults.5,6,7 Occasional smoking in late adolescence has been associated with an eightfold increase in the probability of becoming a daily smoker after 3 years.8
A number of longitudinal studies have tracked changes in smoking behaviour among occasional smokers over periods of up to 2 years.3,5,7,9 These studies, which have mostly focused on adolescents or older adults, showed that up to one‐quarter of baseline occasional smokers became daily smokers in the follow‐up periods. Furthermore, a substantial proportion (>40%) of occasional smokers continue to smoke occasionally, while around one‐third stop smoking.3,5,9 Studies on college students have found that over the course of 4 years, up to 20% of baseline occasional smokers became daily smokers.10,11
Little is known about what differentiates occasional smokers who become daily smokers from those who continue to smoke occasionally and from those who stop smoking. In a study of 45–69‐year‐old smokers in Sweden, Lindstrom et al7 examined the sociodemographic and psychosocial characteristics of baseline occasional smokers who became daily smokers, who remained occasional smokers or who stopped smoking at the 1 year follow‐up. Those who stopped or remained occasional smokers were younger, unmarried, highly educated and were snuff consumers to a greater extent than the reference population (baseline daily smokers, ex smokers and never smokers), and those who became daily smokers had poorer psychosocial resources.7 A study examining changes in occasional smoking among college students found that positive beliefs about the functional value of smoking and the use of smoking to control negative effects predicted a change to daily smoking.11
This paper focuses on the longitudinal patterns of tobacco use among women who were occasional smokers in early adulthood. In addition to the well‐established health risks of smoking, women who smoke are also at risk of decreased fertility, increased risk of complications during pregnancy, miscarriage, stillbirth and neonatal deaths, and lower birth weight babies.12
Data from a large, prospective, population‐based study were used to describe patterns of smoking behaviour among baseline occasional smokers over a 7‐year period. Our method provided an opportunity to examine the characteristics of young women who progressed from occasional smoking to daily smoking, those who continued occasional tobacco use and those who stopped smoking.
Methods
The Australian Longitudinal Study on Women's Health (ALSWH) was initiated in 1996 with three cohorts of Australian women aged 18–23, 45–50 and 70–75 years at recruitment. The aim of this study was to examine the relationships between biological, psychological, social and lifestyle factors and women's physical and mental health, as well as their use of and satisfaction with healthcare services.13 Women were randomly selected from the Australian national healthcare database (Medicare), which includes almost all people who are citizens or permanent residents in Australia. They were recruited nationally, with intentional over sampling from rural and remote areas. Mailed questionnaires are used. Each survey comprises over 300 items, addressing issues including general health and well‐being; health service use; symptoms; stress; smoking and alcohol; weight, exercise and eating; time use; social support; demographics; and aspirations.14 Further details of the methods used in the ALSWH and characteristics of the sample have been reported elsewhere.13,15 The human research ethics committees of the University of Newcastle and the University of Queensland approved the study methods.
An estimated 41% (n = 14 779) of young women responded to the baseline survey in 1996.15 Response rates to the first mailed survey cannot be exactly specified, as some women selected for the sample may not have received the invitation to participate.13 A comparison of women who participated in the baseline survey with data from women in the same age from the Australian census of 1996 showed that the ALSWH participants were reasonably representative of the general population, although they were slightly more likely to be Australian born and to have a post‐school qualification.16 Despite intensive tracking procedures and follow‐up methods,14,17 retention rates for this age group were 66% for survey 2 and 61% for survey 3.
We analysed data from 7510 participants in the young cohort who completed survey 1 in 1996, survey 2 in 2000 and survey 3 in 2003, and who provided complete data on smoking at survey 1.
Measures
Outcome variable: self‐reported smoking status
In survey 1, initial smoking status was established with the question: “Which of the following best describes your smoking status NOW?”, with response options: “I have never smoked”, “I used to smoke”, “I now smoke occasionally” and “I now smoke regularly”.18 Occasional smokers were defined from survey 1 as those who reported, “I now smoke occasionally”. Between surveys 1 (1996) and 2 (2000), a national standard for tobacco use questions was developed and for surveys 2 and 3, the new questions were used19: “How often do you currently smoke cigarettes or any tobacco products?”, with response options: “Daily”, “At least weekly (but not daily)”, “Less often than weekly” and “Not at all”. Women who reported smoking “at least weekly (but not daily)” or “less often than weekly” are referred to here as non‐daily smokers.
Explanatory variables
Smoking history was examined with two variables from survey 1. The first question was “Have you ever smoked daily for six months or more?”, with response options: “Yes” or “No”, and the second question was “At what age did you start smoking?”
A range of sociodemographic, lifestyle and psychosocial variables were examined from surveys 2 and 3. Area of residence was categorised as either urban or rural/remote. Four categories were used for the highest educational qualification: university degree or higher university degree; trade, apprenticeship, certificate or diploma; completed high school (year 12 or equivalent); and did not complete high school (less than year 12).
Changes in marital status and parenthood were examined between surveys 1 and 2 and between surveys 1 and 3. Marital status at each survey was categorised as never married, living in a de facto relationship, married or separated/widowed/divorced. Transitions in marital status between surveys were derived from these categories. Participants were classified as never married at both surveys 1 and 2 (or surveys 1 and 3); married or de facto at survey 1 to married at survey 2 (survey 3); never married at survey 1 to married at survey 2 (survey 3); never married at survey 1 to de facto at survey 2 (survey 3); and all other transitions. Parenthood at each survey was categorised as follows: is a parent (ie, has given birth) and is not a parent (ie, has not given birth). Three categories for transition to parenthood were derived: not a parent at survey 1 and not a parent by survey 2 (survey 3); not a parent at survey 1 to a parent by survey 2 (survey 3); and a parent before survey 1.
For data at surveys 2 and 3, a dichotomous variable was used for illicit drug use: not used drugs in the past 12 months and used drugs in the past 12 months. On the basis of the National Health and Medical Research Council guidelines,20 a variable for alcohol consumption was derived from alcohol frequency and quantity questions in surveys 2 and 3. Three categories were defined: low‐risk drinker (⩽ 14 drinks per week); non‐drinker/rarely drinks; and risky/high‐risk drinker (⩾15 drinks per week). Physical activity was measured at surveys 2 and 3 using items from the national Active Australia campaign surveys asking about hours and minutes spent in walking, moderate and vigorous activity during the last week.21 A physical activity score was created and then divided into four categories: inactivity, low activity, moderate activity, and high activity.22
Weight dissatisfaction was obtained from the question in surveys 2 and 3: “In the past month, how dissatisfied have you felt about your weight?”, with responses: not at all dissatisfied, slightly dissatisfied, moderately dissatisfied and markedly dissatisfied. The 10‐item Center for Epidemiologic Studies Short Depression Scale self‐report depression scale developed by Andresen et al23 and completed in surveys 2 and 3 was included in the analysis. This scale, which has been widely validated, has a possible range of 0–30, with higher scores indicating more psychological distress.24 The 11‐item Perceived Stress Questionnaire for Young Women developed by Bell and Lee25 was used to examine associations between smoking and perceived stress levels from surveys 2 and 3. Items were averaged to give a mean perceived stress score with a possible range of 0–4. Higher scores indicate greater levels of perceived stress. This measure has been found to have reproducible internal reliability and validity.25
Statistical analysis
Women who were occasional smokers at baseline were divided into three groups for analysis at two time points. For smoking transitions between surveys 1 and 2, these groups were: baseline occasional smokers who became daily smokers at survey 2; those who reported non‐daily smoking at survey 2; or those who had stopped smoking (non‐smokers) at survey 2. For smoking transitions over the 7‐year period between surveys 1 and 3, the groups were baseline occasional smokers who were daily smokers at survey 3; non‐daily smokers at survey 3; and those who had stopped smoking (non‐smokers) at survey 3. χ2 tests and one‐way analysis of variance were used to identify significant univariate associations among these smoking groups for each of the explanatory variables at the two separate time points. All factors that were statistically significant at the level of ⩽0.05 were entered into a multinomial logistic regression model to compare sociodemographic, lifestyle and psychosocial characteristics between the three groups. In the first model, women who changed to daily smoking at survey 2 and those who were non‐daily smokers at survey 2 were compared with the reference population—those who had stopped smoking at survey 2. In the second model, women who changed to daily smoking at survey 3 and those who were non‐daily smokers at survey 3 were compared with the reference population—those who had stopped smoking at survey 3. A backward selection procedure was used to include all factors significantly associated at the 0.05 level in the final model. Statistical analysis was performed using SPSS V.13.0.
Results
Among the 7510 participants for whom complete data on smoking were available at survey 1 and who completed surveys 2 and 3, 11% (n = 829) reported smoking occasionally, 17% (n = 1291) smoked regularly, 15% (n = 1127) were ex smokers and 57% (n = 4263) reported never smoking. Thus, 39% of all current smokers were occasional smokers. Among the baseline occasional smokers, 40% (n = 331) reported that they had smoked daily for ⩾6 months and 58% (n = 484) reported never smoking daily for ⩾6 months.
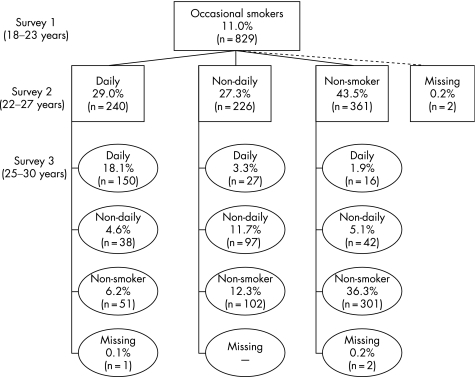
Figure 1 shows the changes in self‐reported smoking status among baseline occasional smokers from surveys 1 to 2 and from surveys 2 to 3. Approximately 12% (n = 97) of the baseline occasional smokers reported non‐daily smoking in the follow‐up surveys; 18% (n = 150) progressed to daily smoking at survey 2 and remained daily smokers at survey 3; and 36% (n = 301) had stopped smoking at survey 2 and remained non‐smokers at survey 3. Over surveys 2 and 3, 33% (n = 276) of baseline occasional smokers moved between daily, non‐daily and non‐smoking. At the 7‐year follow‐up, approximately half (55%) of those who reported occasional smoking at baseline had stopped smoking, almost one‐quarter (23%) changed to daily smoking and the rest reported non‐daily smoking.
Figure 1 Changes in smoking status between surveys 1, 2 and 3 among women who reported being occasional smokers at survey 1.
The three smoking groups compared in the subsequent analysis of smoking transitions between surveys 1 and 2 comprised those who were daily smokers at survey 2 (n = 240), those who were non‐daily smokers at survey 2 (n = 226) and those who stopped smoking at survey 2 (n = 361). The groups compared in the analysis of smoking transitions between surveys 1 and 3 comprised those who were daily smokers at survey 3 (150+27+16 = 193), those who were non‐daily smokers at survey 3 (38+97+42 = 177) and those who stopped smoking at survey 3 (51+102+301 = 454).
Table 1 shows the results of the univariate associations, with each of the explanatory variables considered in the study for the analysis of smoking transitions between surveys 1 and 3 only. Women who became daily smokers were more likely to have been daily smokers for at least 6 months before survey 1, have lower levels of education and higher depression scores. Those who were classified as non‐daily smokers were more likely to live in urban areas, not to be married or be a parent, and to be a low‐risk drinker. Those who became non‐smokers were more likely to have married and least likely to have used illicit drugs. Although not shown here, we also conducted univariate analyses with the variables shown in table 1 for smoking transitions between surveys 1 and 2. The results were similar to survey 3, except that there were weaker associations with depression and stress. Variables that were not significant (p⩾0.05) were not included in the multivariate analyses.
Table 1 Univariate analyses of factors associated with changes to daily smoking, non‐daily smoking and non‐smoking at survey 3 (column percentages) among women who reported being occasional smokers at survey 1.
| Daily smokers (n = 193), % | Non‐daily smokers (n = 177), % | Non‐smokers (n = 454), % | χ2 p Values | |
|---|---|---|---|---|
| Ever smoked daily ⩾6 months at survey 1 | ||||
| Yes | 61.3 | 39.2 | 32.1 | <0.001 |
| No | 38.7 | 60.8 | 67.9 | |
| Area of residence | ||||
| Urban | 53.4 | 66.7 | 60.4 | 0.036 |
| Rural/remote | 46.6 | 33.3 | 39.6 | |
| Highest educational qualification | ||||
| University degree or higher | 31.7 | 49.2 | 47.3 | 0.006 |
| Trade/apprenticeship/certificate/diploma | 32.3 | 28.8 | 25.8 | |
| Completed high school (year 12) | 24.7 | 15.8 | 20.0 | |
| Did not complete high school (year 10 or less) | 11.3 | 6.2 | 6.9 | |
| Marital status | ||||
| Never married at survey 1 and never married at survey 3 | 34.0 | 48.6 | 29.7 | <0.001 |
| Married/de facto at survey 1 to married at survey 3 | 8.8 | 6.9 | 10.9 | |
| Never married at survey 1 to married at survey 3 | 21.1 | 15.6 | 32.8 | |
| Never married at survey 1 to de facto at survey 3 | 17.0 | 18.5 | 21.7 | |
| All other transitions | 19.1 | 10.4 | 4.9 | |
| Parenthood | ||||
| Not a parent by survey 1 and not a parent by survey 3 | 67.7 | 86.4 | 70.6 | <0.001 |
| Not a parent by survey 1 to parent by survey 3 | 19.3 | 10.2 | 25.4 | |
| Parent before survey 1 | 13.0 | 3.4 | 4.0 | |
| Illicit drug use in the past 12 months | ||||
| Not used drugs | 59.9 | 50.6 | 79.0 | <0.001 |
| Used drugs | 40.1 | 49.4 | 21.0 | |
| Alcohol consumption | ||||
| Low‐risk drinker | 60.8 | 80.7 | 69.2 | <0.001 |
| Non‐drinker/rarely drinks | 30.9 | 10.2 | 27.1 | |
| Risky/high‐risk drinker | 8.2 | 9.1 | 3.7 | |
| Physical activity | ||||
| Inactivity | 11.5 | 8.8 | 6.6 | 0.56 |
| Low activity | 34.6 | 29.4 | 37.4 | |
| Moderate activity | 26.7 | 22.4 | 26.5 | |
| High activity | 27.2 | 39.4 | 29.4 | |
| Weight dissatisfaction | ||||
| Not at all dissatisfied | 12.4 | 14.7 | 15.7 | 0.961 |
| Slightly dissatisfied | 37.1 | 36.7 | 36.9 | |
| Moderately dissatisfied | 24.7 | 22.6 | 22.1 | |
| Markedly dissatisfied | 25.8 | 26.0 | 25.2 | |
| Mean (SD) | Mean (SD) | Mean (SD) | One‐way ANOVA p Value | |
| Depression (CESD‐10) | 8.2 (5.6) | 7.0 (5.1) | 6.7 (4.8) | 0.005 |
| Perceived stress | 1.02 (0.6) | 1.0 (0.5) | 0.9 (0.5) | 0.023 |
| Age when smoking was started | 15.9 (2.1) | 16.0 (2.0) | 16.2 (2.4) | 0.202 |
CESD‐10, Center for Epidemiologic Studies Short Depression Scale.
Total numbers vary slightly because of missing data.
Table 2 shows the final logistic regression models for factors statistically significantly associated with the change to daily smoking and to non‐daily smoking compared with stopping smoking. Model 1 compares baseline occasional smokers who reported daily smoking or non‐daily smoking at survey 2 with those who stopped smoking at survey 2 (reference group). Model 2 compares baseline occasional smokers who reported daily smoking or non‐daily smoking with those who had stopped smoking at survey 3 (reference group).
Table 2 Odds ratios (95% CI) show characteristics of women who reported being occasional smokers at survey 1, who changed to daily smoking and to non‐daily smoking, compared with those who stopped smoking: between surveys 1 and 2 and between surveys 1 and 3.
| Model 1—Smoking status at survey 2 | Model 2—Smoking status at survey 3 | |||
|---|---|---|---|---|
| Daily smokers | Non‐daily smokers | Daily smokers | Non‐daily smokers | |
| Ever smoked daily for ⩾6 months at survey 1 | ||||
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 4.38 (2.95 to 6.51) | 1.52 (1.01 to 2.29) | 3.19 (2.13 to 4.78) | 1.49 (0.98 to 2.27) |
| Highest qualification | ||||
| University degree or higher | 1.00 | 1.00 | 1.00 | 1.00 |
| Trade/apprenticeship/certificate/diploma | 2.27 (1.41 to 3.68) | 0.97 (0.60 to 1.56) | 2.07 (1.28 to 3.35) | 1.65 (1.03 to 2.64) |
| Completed high school (year 12) | 2.55 (1.55 to 4.18) | 1.43 (0.89 to 2.31) | 1.45 (0.85 to 2.49) | 1.13 (0.63 to 2.02) |
| Did not complete high school (year 10 or less) | 1.50 (0.70 to 3.18) | 1.03 (0.46 to 2.31) | 1.72 (0.79 to 3.77) | 1.41 (0.57 to 3.48) |
| Marital status | ||||
| Never married | 1.00 | 1.00 | 1.00 | 1.00 |
| Married/de facto to married | 0.53 (0.25 to 1.12) | 0.52 (0.22 to 1.19) | 0.45 (0.21 to 0.98) | 0.62 (0.27 to 1.41) |
| Never married to married | 0.46 (0.24 to 0.88) | 0.61 (0.31 to 1.18) | 0.50 (0.29 to 0.86) | 0.39 (0.23 to 0.69) |
| Never married to de facto | 0.50 (0.30 to 0.82) | 0.71 (0.44 to 1.13) | 0.60 (0.35 to 1.03) | 0.56 (0.34 to 0.95) |
| All other transitions | 0.97 (0.49 to 1.94) | 1.17 (0.57 to 2.42) | 1.58 (0.78 to 3.20) | 1.16 (0.53 to 2.51) |
| Parenthood | ||||
| Not a parent | 1.00 | 1.00 | 1.00 | 1.00 |
| Not a parent to a parent | 0.38 (0.18 to 0.79) | 0.40 (0.17 to 0.95) | 0.80 (0.46 to 1.39) | 0.57 (0.29 to 1.12) |
| Parent before survey 1 | 1.10 (0.47 to 2.61) | 0.92 (0.34 to 2.49) | 1.37 (0.59 to 3.20) | 0.36 (0.10 to 1.25) |
| Illicit drug use in the past 12 months | ||||
| Not used drugs | 1.00 | 1.00 | 1.00 | 1.00 |
| Used drugs | 1.56 (1.06 to 2.29) | 1.48 (1.02 to 2.16) | 2.32 (1.52 to 3.55) | 3.00 (1.99 to 4.53) |
| Alcohol consumption | ||||
| Low‐risk drinker | 1.00 | 1.00 | 1.00 | 1.00 |
| Non‐drinker/rarely drinks | 0.95 (0.61 to 1.47) | 0.40 (0.24 to 0.66) | 1.43 (0.93 to 2.22) | 0.38 (0.21 to 0.69) |
| Risky/high‐risk drinker | 1.23 (0.48 to 3.15) | 1.97 (0.89 to 4.36) | 2.16 (0.98 to 4.74) | 1.64 (0.77 to 3.48) |
Baseline occasional smokers who reported smoking daily for ⩾6 months before survey 1, had significantly higher odds for daily smoking and for non‐daily smoking. Compared with the university‐qualified reference group, women with a trade/apprenticeship/certificate/diploma had significantly higher odds for daily smoking. Compared with women who remained single, those who moved into a committed relationship had significantly lower odds for daily smoking or non‐daily smoking. Becoming a parent was significantly associated with lower odds for daily and non‐daily smoking at survey 2. Compared with women who had not used illicit drugs in the past year, those who had used illicit drugs had significantly higher odds for daily smoking and for non‐daily smoking at both surveys 2 and 3. Current alcohol consumption was associated with higher odds of non‐daily smoking at surveys 2 and 3, compared with stopping smoking.
Discussion
A total of 11% of young women (18–23 years) surveyed in 1996 reported being occasional smokers, equating to 39% of all smokers at the baseline survey. This proportion is higher than those found among general adult groups (10–18%) in other studies of occasional smoking,3,5,7,9 but lower than that found among adolescents (45%).3
In our study, 29% of baseline occasional smokers changed to daily smoking by survey 2 (when they were aged 22–27 years), and almost two‐thirds of these daily smokers continued smoking daily at survey 3 (aged 25–30 years). There was little escalation in tobacco use between surveys 2 and 3, with only 5% of baseline occasional smokers becoming daily smokers. The majority (61%) of those who were daily smokers at survey 3 reported daily smoking before the baseline survey. Their occasional smoking reported at survey 1 was likely to have been a phase of reduced smoking, rather than a progression towards daily smoking.
Occasional smoking as a long‐term behaviour pattern was also evident, with about 27% of baseline occasional smokers reporting non‐daily smoking at survey 2. By survey 3, 12% of these women maintained non‐daily smoking and 10% returned to non‐daily smoking at survey 3 after daily or non‐smoking at survey 2. Less than half (44%) of baseline occasional smokers stopped smoking at survey 2 and more than one‐third (36%) remained non‐smokers at both surveys 2 and 3. A further 19% stopped smoking at survey 3 after non‐daily or daily smoking at survey 2. Our study and others3,7,9 highlight the instability in tobacco use among occasional smokers. We found that one‐third of baseline occasional smokers fluctuated between daily, non‐daily and non‐smoking between surveys 2 and 3. We can only report the net change in smoking status at each follow‐up period (which does not capture the fluctuations in smoking patterns that may have occurred between survey times). Schofield et al3 showed frequent movement between smoking categories among younger occasional smokers over shorter follow‐up periods (3, 9 and 15 months after leaving high school).
The transition period to young adulthood is clearly an opportune time for interventions to prevent the escalation to daily smoking and to promote smoking cessation. We found that young women who were most susceptible to progressing to daily smoking had intermediate levels of education. These educational qualifications may place young women in occupational groups (eg, hairdresser, clerical and administrative worker, or sales assistant) that have higher smoking rates than the wider population.26,27 A recent study of young, non‐professional Australian workers found that 50% were current smokers, with smoking rates ranging from 38% among those working in retail or fast food outlets to 71% among hairdressers.26
Marriage and parenthood modify smoking behaviour.28 In the multivariate analysis, marriage was statistically significantly associated with not smoking at both time points, whereas the relationship between not smoking and becoming a parent was evident only for surveys 1 and 2. This may be because of a strong association between parenthood and marriage. The relationship between marriage and quitting smoking has been related in previous studies to the development of a more responsible concern with lifestyle and health29 and to an increased personal commitment to a spouse, as well as to preparation for parenthood.30 Qualitative research on life transitions and young women's smoking behaviour also suggests that around their mid‐20s, young women become more concerned about the addictive nature of cigarettes and their capacity to quit, as they consider their future health and plans for having children.31 Public communication strategies should take into account the influence of life‐stage changes such as marriage: a commitment to a partner may include a commitment to one's health and to future family health.
There are well‐known associations between tobacco, alcohol and illicit drug use: the use of one or more of these substances is associated with subsequent use of the others.32,33 In our study, current alcohol consumption was significantly associated with non‐daily smoking only; however, recent use of illicit drugs was associated with both daily and non‐daily smoking, with the strength of this association being greater for non‐daily smokers. Use of illicit drugs is generally greatest in young adulthood.1 The role of alcohol and illicit drug use in becoming a daily smoker or remaining a non‐daily smoker may be associated with the social context of cigarette smoking.34
Young adulthood is a stage of life that includes going out with friends, drinking and experimenting with drugs in settings such as private parties, raves, pubs and clubs.34 Young women regard smoking as a normative behaviour in these social settings, and as a means to meet and bond with others.31,35 Some only smoke in these circumstances, regarding themselves as “social smokers”.35 These young women may quit smoking as they mature out of this “single, partying” stage of life towards marriage and parenthood.30 The current legislative climate in several developed countries, of implementing smoke‐free policies in hospitality venues, may help to promote cessation among these socially mediated, occasional smokers.36,37 However, this may not be the case for some young women who may be susceptible to nicotine dependence.38,39
Although a history of previous daily smoking provides an explanation for the change to daily smoking among some baseline occasional smokers, in our study, lifestyle and life‐stage factors were also strongly associated with daily and non‐daily smoking. By contrast, the psychosocial factors considered (stress and depression) were not consistently associated with smoking among occasional smokers. Other studies have reported associations of stress and depression with smoking,40,41 and young women themselves cite stress as a reason for taking up and maintaining smoking.31
Strengths and limitations
The strengths of our study include the use of a large, nationally representative sample of young women. Furthermore, the longitudinal study design and the use of multivariate analysis allows in‐depth exploration of a range of demographic, lifestyle and psychosocial factors influencing young women's smoking behaviour as they move through different stages of their lives. One limitation is the survey response rate. Despite intensive tracking procedures and follow‐up methods,14,17 approximately one‐third of baseline participants were lost to follow‐up. Analysis of differences in sociodemographic and health characteristics between respondents and non‐respondents to survey 2 showed that non‐respondents were more likely to be smokers, unemployed, have difficulty managing on their available income and have lower levels of education, on the basis of information at survey 1.28 Thus, non‐response may have resulted in underestimation of the prevalence of smoking, and may have decreased the strength of some of the associations that we have reported.
What this paper adds
Previous research has examined changes in smoking patterns of occasional smokers over periods of up to 4 years.
We examined these changes over a 7‐year period in a large, population‐based cohort study of women, initially aged 18–23 years. Approximately half (55%) of the young women who were occasional smokers at baseline, stopped smoking by their mid to late 20s, almost one‐quarter changed to daily smoking and the rest reported non‐daily smoking.
Use of illicit drugs and alcohol was predictive of becoming a daily or non‐daily smoker, illustrating the influence of social activities on smoking behaviour. Life transitions such as committed relationships, marriage and becoming a parent increased the likelihood of cessation.
More than half (61%) of the women who became daily smokers had a history of daily smoking, suggesting that for them occasional smoking had been a temporary phase.
Daily smoking was also associated with intermediate levels of education consistent with specific occupational groups, which could provide settings for targeted preventive activities.
Another limitation is that our definition of “age started smoking” did not specify daily or less frequent smoking and the question may have been answered inconsistently. We were also unable to examine cigarette consumption at baseline among the occasional smokers or to verify that they smoked less often than daily. However, a recent Australian study found that the majority (81%) of self‐described occasional smokers reported that they were non‐daily smokers and that the majority of self‐described light (93%) and heavy (99%) smokers reported that they smoked daily.42
Furthermore, self‐reported smoking status was not confirmed with biochemical validation of tobacco consumption. Although a high degree of concordance with self‐reported smoking has been found among both adolescents43 and adults,44 self‐reports of occasional smoking may be more problematic. In a study of long‐term and transitional occasional smokers, 4% of baseline occasional smokers reported that they had never smoked at the 1‐year follow‐up.7 The authors suggested that occasional smokers may not regard themselves as ever‐smokers once they quit and consequently have a weaker smoking identity than daily smokers. Borland45 also found anomalies in smoking identity with sporadic tobacco use among a small minority of self‐ascribed non‐smokers. These findings imply that the prevalence of occasional smoking may be under‐reported.
Conclusions
This study examined transitions in smoking behaviour among young adult women who reported being occasional smokers at baseline. Our findings reinforce the need for targeted interventions to discourage the escalation to daily smoking and to promote cessation among these occasional smokers, who made up 39% of all smokers. Preventive strategies should build on understanding the social and environmental factors that make cigarette smoking an attractive option for women in young adulthood, particularly in social, educational and occupational settings. Targeted interventions in vocational training settings and non‐professional occupational settings could help prevent the escalation to daily smoking and promote cessation.
Acknowledgements
The Australian Longitudinal Study on Women's Health, which was conceived and developed by groups of interdisciplinary researchers at the universities of Newcastle and Queensland, is funded by the Australian Government Department of Health and Ageing. We thank all participants for their valuable contribution to this project. Liane McDermott is supported by a National Health and Medical Research Council Public Health Postgraduate Scholarship, and Liane McDermott and Neville Owen are partially supported through a Core Infrastructure Grant to the Cancer Prevention Research Centre from Queensland Health.
Abbreviations
ALSWH - Australian Longitudinal Study on Women's Health
Footnotes
Competing interests: None declared.
References
- 1.Australian Institute of Health and Welfare 2004 National Drug Strategy Household Survey: first results. AIHW Catalogue number. PHE 57. Canberra, ACT: AIHW, 2005
- 2.West P, Sweeting H, Ecob R. Family and friends' influences on the uptake of regular smoking from mid‐adolescence to early adulthood. Addiction 1999941397–1412. [DOI] [PubMed] [Google Scholar]
- 3.Schofield P, Borland R, Hill D.et al Instability in smoking patterns among school leavers in Victoria, Australia. Tob Control 19987149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ling P, Glantz S. Why and how the tobacco industry sells cigarettes to young adults: evidence from industry documents. Am J Public Health 200292908–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hennrikus D, Jeffery R, Lando H. Occasional smoking in a Minnesota working population. Am J Public Health 1996861260–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Husten C, McCarty M, Giovino G.et al Intermittent smokers: a descriptive analysis of persons who have never smoked daily. Am J Public Health 19988886–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindstrom M, Isacsson S, The Malmo Shoulder‐Neck Study Group Long term and transitional intermittent smokers: a longitudinal study. Tob Control 20021161–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patton G, Carlin J, Coffey C.et al The course of early smoking: a population‐based cohort study over three years. Addiction 1998931251–1260. [DOI] [PubMed] [Google Scholar]
- 9.Zhu S, Sun J, Hawkins S.et al A population study of low‐rate smokers: quitting history and instability over time. Health Psychol 200322245–252. [DOI] [PubMed] [Google Scholar]
- 10.Kenford S, Wetter D, Welsch S.et al Progression of college‐age cigarette samplers: what influences outcome. Addict Behav 200530285–294. [DOI] [PubMed] [Google Scholar]
- 11.Wetter D, Kenford S, Welsch S.et al Prevalence and predictors of transitions in smoking behavior among college students. Health Psychol 200423168–177. [DOI] [PubMed] [Google Scholar]
- 12.US Department of Health & Human Services Women and smoking: a report of the Surgeon General‐2001. Rockville, MD: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2001
- 13.Lee C, Dobson A, Brown W.et al Cohort profile: The Australian Longitudinal Study on Women's Health. Int J Epidemiol 200534987–991. [DOI] [PubMed] [Google Scholar]
- 14.Lee C.Women's Health Australia: progress on the Australian Longitudinal Study on Women's Health 1995–2000. Brisbane: Australian Academic Press Pty, 2001
- 15.Brown W, Bryson L, Byles J.et al Women's Health Australia: recruitment for a national longitudinal cohort study. Women Health 19982823–40. [DOI] [PubMed] [Google Scholar]
- 16.Brown W, Dobson A, Bryson L.et al Women's Health Australia: on the progress of the main cohort studies. J Women's Health Gender‐based Med 19998681–688. [DOI] [PubMed] [Google Scholar]
- 17.Adamson L, Chojenta C, Lee C. Telephone contact of existing participants in longitudinal surveys. Aust NZ J Public Health 200529188–189. [DOI] [PubMed] [Google Scholar]
- 18.National Heart Foundation of Australia Risk factor prevalence study survey 3 1989. Canberra: National Heart Foundation of Australia and Australian Institute of Health, 1990
- 19.Australian Institute of Health and Welfare National health data dictionary. Version 9. AIHW Catalogue number. HWI 24. Canberra: AIHW, 2000
- 20.National Health and Medical Research Council Australian alcohol guidelines: health risks and benefits. Endorsed October 2002. Canberra, ACT: Commonwealth of Australia, 2001
- 21.Armstrong T, Bauman A, Davies J.Physical activity patterns of Australian adults: results of the 1999 National Physical Activity Survey. Canberra: Australian Institute of Health and Welfare, 2000
- 22.Brown W, Trost S. Life transitions and changing physical activity patterns in young women. Am J Prev Med 200325140–143. [DOI] [PubMed] [Google Scholar]
- 23.Andresen E, Carter W, Malmgren J.et al Screening for depression in well older adults: evaluation of a short form of the CES‐D. Am J Prev Med 19941077–84. [PubMed] [Google Scholar]
- 24.France C, Lee C, Powers J. Correlates of depressive symptoms in a representative sample of young Australian women. Aust Psychol 200439228–237. [Google Scholar]
- 25.Bell S, Lee C. Development of the Perceived Stress Questionnaire for Young Women. Psychol Health Med 20027189–201. [Google Scholar]
- 26.Lindsay J. Health risks in the social lives of young workers. Youth Studies Aust 20012011–18. [Google Scholar]
- 27.Setter C, Peter R, Siegrist J.et al Impact of school and vocational education on smoking behaviour: results from a large‐scale study on adolescents and young adults in Germany. Soz Praventivmed 199843133–140. [DOI] [PubMed] [Google Scholar]
- 28.McDermott L, Dobson A, Russell A. Changes in smoking behaviour among young women over life stage transitions. Aust NZ J Public Health 200428330–335. [DOI] [PubMed] [Google Scholar]
- 29.Backett K, Davison C. Lifecourse and lifestyle: the social and cultural location of health behaviours. Soc Sci Med 199540629–638. [DOI] [PubMed] [Google Scholar]
- 30.Bachman J, Wadsworth K, O'Malley P.et al Marriage, divorce, and parenthood during the transition to young adulthood: impacts on drug use and abuse. In: Schulenberg J, Maggs J, Hurrelmann K, eds. Health risks and developmental transitions during adolescence. Cambridge: Cambridge University Press, 1997
- 31.McDermott L, Dobson A, Owen N. From partying to parenthood: young women's perceptions of cigarette smoking across life transitions. Health Educ Res 200621428–439. [DOI] [PubMed] [Google Scholar]
- 32.Jackson K, Sher K, Cooper M.et al Adolescent alcohol and tobacco use: onset, persistence and trajectories of use across two samples. Addiction 200297517–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richter K, Ahluwalia H, Mosier M.et al A population‐based study of cigarette smoking among illicit drug users in the United States. Addiction 200297861–869. [DOI] [PubMed] [Google Scholar]
- 34.Miller B, Furr‐Holden D, Voas R.et al Emerging adults' substance use and risky behaviors in club settings. J Drug Issues 200535357–378. [Google Scholar]
- 35.Lennon A, Gallois C, Owen N.et al Young women as smokers and non‐smokers: a qualitative social identity approach. Qual Health Res 2005151345–1359. [DOI] [PubMed] [Google Scholar]
- 36.Siegel M, Albers A, Cheng D.et al Effect of local restaurant smoking regulations on progression to established smoking among youths. Tob Control 200514300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trotter L, Wakefield M, Borland R. Socially cued smoking in bars, nightclubs, and gaming venues: a case for introducing smoke‐free policies. Tob Control 200211300–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Owen N, Kent P, Wakefield M.et al Low‐rate smokers. Prev Med 19952480–84. [DOI] [PubMed] [Google Scholar]
- 39.Shiffman S, Paty J, Kassel J.et al Smoking behavior and smoking history of tobacco chippers. Exp Clin Psychopharmacol 19942126–142. [Google Scholar]
- 40.Kassel J, Stroud L, Paronis C. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull 2003129270–304. [DOI] [PubMed] [Google Scholar]
- 41.Sheahan S, Latimer M. Correlates of smoking, stress, and depression among women. Health Values 19951929–36. [Google Scholar]
- 42.Morley K, Hall W, Hausdorf K.et al ‘Occasional' and ‘social' smokers: potential target groups for smoking cessation campaigns? Aust NZ J Public Health 200630550–554. [DOI] [PubMed] [Google Scholar]
- 43.Post A, Gilljam H, Rosendahl I.et al Validity of self reports in a cohort of Swedish adolescent smokers and smokeless tobacco (snus) users. Tob Control 200514114–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Vartiainen E, Seppälä T, Lillsunde P.et al Validation of self reported smoking by serum cotinine measurement in a community‐based study. J Epidemiol Community Health 200256167–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Borland R. Population estimates of occasional smoking among self‐described smokers and non‐smokers in Victoria, Australia. Tob Control 1994337–40. [Google Scholar]