Abstract
Objective
To assess airborne nicotine concentrations as an indicator of second‐hand smoke (SHS) exposure in public places in both urban and rural areas of China.
Design
Measurement of vapour‐phase nicotine concentration using a common protocol in all locations. A total of 273 samplers were placed for 7 days in urban and rural areas of China, including Beijing and the capital city, and a county (rural) area of the following provinces: Sichuan (Chengdu/Mianzhu), Jiangxi (Nanchang/Anyi) and Henan (Zhengzhou/Xin'an).
Setting
Samplers were placed in hospitals, secondary schools, city government buildings, train stations, restaurants and entertainment establishments (internet cafes, mahjong parlours and karaoke bars) in each location.
Main outcome measure
The time‐weighted average airborne concentration of nicotine (μg/m3) was measured by gas chromatography.
Results
Airborne nicotine was detected in 91% of the locations sampled. Beijing had the highest nicotine concentrations in most indoor environments (median 3.01 μg/m3) and Chengdu had the lowest concentrations (median 0.11 μg/m3). Overall, restaurants and entertainment establishments had the highest nicotine concentrations (median 2.17 and 7.48 μg/m3, respectively). High nicotine concentrations were also found in government buildings and in train stations.
Conclusions
The data collected in this study provide evidence that SHS exposure is frequent in public places in China. Environmental nicotine concentrations in China provide evidence for implementation and enforcement of smoke‐free initiatives in public places in China and indicate the need for protecting the public from exposure to SHS.
Tobacco use causes death and disease not only among those who actively smoke but also among those who are exposed to second‐hand smoke (SHS) in indoor environments.1,2 Over the past two decades, evidence on the adverse health effects of SHS exposure has led to initiatives worldwide to reduce exposure in public places, workplaces, homes and transportation environments. Although cities and entire countries, including New York City and State, Italy, Ireland, Norway and Scotland, have passed legislation banning smoking in all public places, most countries and particularly the low‐income to middle‐income countries, such as China, do not have effective policies in place to reduce active and passive smoking. Making indoor environments smoke‐free has not been easy; in many countries, a majority of men smoke and the tobacco industry has vigorously attempted to counter the growing call for smoke‐free indoor environments. Industry efforts include attempts at discrediting scientific evidence on the health effects of SHS, subverting regulatory initiatives, and advancing ineffective alternatives to eliminate smoking indoors.3 In addition, many countries lack data documenting exposure of the population to SHS.
China is a particularly critical nation in the global effort to control tobacco use. China has the largest population of smokers in the world: over 350 million of its 1.2 billion people.4 Governments, including the Chinese government, are increasingly becoming aware of the significant impact of the tobacco epidemic on their citizens.5
In August 2006, the Chinese government ratified the World Health Organization's Framework Convention on Tobacco Control, and some Chinese cities, government departments and organisations have now adopted rules and regulations banning smoking in public places and workplaces. Recently, a deputy to the China legislature called for a ban on smoking in all public places.6 However, progress has been hindered by the high prevalence of smoking and a general view that smoking is acceptable.4 There is also concern about the possible negative economic impact of tobacco control policies, especially in the rural and less‐developed areas of China.
To develop the required evidence for advancing tobacco control, we measured airborne nicotine concentrations in various locations across China. In this study, we report the results of an assessment of nicotine concentrations in schools, hospitals, government offices, train stations, facilities, restaurants and entertainment establishments in urban and rural areas of China.
Methods
Design and data collection
The study was conducted over several months starting in January 2005 in Beijing, the capital city, and a county (rural) area of three provinces: Sichuan (Chengdu/Mianzhu), Jiangxi (Nanchang/Anyi) and Henan (Zhengzhou/Xin'an). In each city or rural area, the following public places were selected for monitoring airborne nicotine concentrations: hospitals, schools, the city's government building, train stations, restaurants and entertainment places (eg, internet cafes, karaoke bars and mahjong parlours).
The assessment of SHS included the use of a passive monitor to obtain the indoor concentrations of airborne nicotine.7 Sample locations were selected on the basis of convenience to represent areas where people frequently work or spend time, but without knowledge on the extent of smoking taking place in the selected areas. For each public place, a representative was asked about the presence of a written policy restricting or banning smoking inside the facility. In addition, information was obtained through observation of each public place for the presence of any no‐smoking signs.
To standardise data collection, a common protocol was followed by field teams in all cities and rural counties. A training workshop was held prior to the fieldwork to acquaint study staff from each city or rural area with the methods and purpose of the protocol, procedure manuals and data collection forms. Within each public place, the fieldworkers were instructed to select a series of locations for the placement of the monitors. In the hospitals, the selected locations were doctors' rooms, nurses' stations, administration offices, cafeterias and patients' rooms. In the schools, the locations were teachers' rooms, students' dormitory, students' bathroom, cafeteria and stairwells. In the city government buildings, the locations were offices, areas open to the public, cafeteria and stairwells. In restaurants and entertainment places with smoking and non‐smoking areas, one monitor was placed in each area. In each city or rural area, the lead Chinese investigator was responsible for conducting the airborne sampling and observations.
Nicotine monitoring
The time‐weighted average concentration of SHS in each area was estimated by passive sampling of vapour‐phase nicotine using a filter badge treated with sodium bisulphate. This method was originally developed by Hammond et al.7,8 In brief, the filter is held in a plastic cassette, and nicotine passively diffuses through a windscreen to the treated filter. The samplers were assembled centrally at the Exposure Assessment Facility of the Center for Urban Environmental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA, shipped to China and then returned at the end of the sampling period. The samplers were left in each of the locations for a period of 1 week and checked periodically to verify the correct placement.
The collected nicotine was extracted from the filter and analysed by gas chromatography with nitrogen‐selective detection. The airborne nicotine concentration (μg/m3) was calculated by dividing the amount of nicotine collected by the filter during the sampling period by the effective volume of air sampled (number of minutes of sampling times the effective sampling rate). The effective sampling rate was 25 ml/min. All the filters were analysed in one batch per location. The limit of detection ranged between 0.004 μg/m3 in Chengdu City and 0.01 μg/m3 in Nanchang City. The total number of samples below the detection limit was 24 (8.9%): 0 in Beijing, 6 in Chengdu, 9 in Nanchang, 4 in Zhengzhou, 1 in Mianzhu, 2 in Anyi and 2 in Xinan. For these samples, a value equal to the detection limit divided by the square root of 2 was assigned.9 For quality control purposes, 10% of the nicotine samplers had an accompanying duplicate and a blank sampler. The intraclass correlation coefficient between duplicates was 0.94.
Statistical analysis
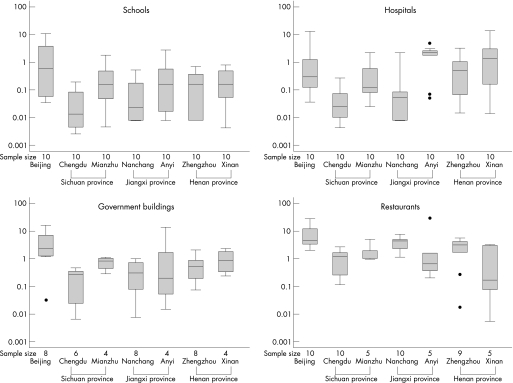
Nicotine concentrations were markedly right skewed. The median and interquartile ranges were used to describe the data, and box plots on the logarithmic scale were used to graphically present the distribution of nicotine concentrations by city or rural area for each type of public place. To compare nicotine concentrations across urban and rural areas, across public places and by the presence of written smoking regulation, the ratios of nicotine concentrations and its 95% CI versus the corresponding category with the lowest nicotine concentration were estimated using linear regression models on log‐transformed nicotine. The analyses were carried out with STATA V.8.2.
Results
General characteristics
Demographic and economic characteristics varied across the different cities and rural areas of the study (table 1). Populations in the cities ranged from about 2 million inhabitants in Nanchang to nearly 14 million in Beijing, and in the rural areas from 220 000 in Anyi County to >500 000 in Mianzhu County. The gross domestic product per capita ranged from US$580 (RMB 4637, £295.33, €434.33) in Anyi to almost US$2249 (RMB 18 000, £1145.18, €1684.29) in Beijing. Smoking prevalence rates among adults ranged from 20.5% in Beijing to 35.8% in Mianzhu. Most of the cities had regulations restricting smoking in public places with variation in the extent of public places covered and the level of enforcement. None of the three rural counties had no smoking regulations for public places. Restaurants and entertainment places were not covered by smoke‐free regulations at all.
Table 1 Characteristics of the participating provinces, China 2005.
| Population size1 | Socioeconomic variables* | Smoking prevalence rates† (%) | Smoking regulation in public places‡ | ||
|---|---|---|---|---|---|
| Illiterate (%) | GDP per capita ($) | ||||
| Province | |||||
| Beijing | 13 819 000 | 4.9 | 2249 | 20.5 | Yes |
| Sichuan | |||||
| Chengdu City | 10 133 000 | 3.7 | 1621 | 22.5 | Yes |
| Mianzhu County | 515 830 | 5.2 | 1246 | 35.8 | No |
| Jiangxi | |||||
| Nanchang City | 4 329 576 | 4.4 | 1257 | NA | Yes |
| Anyi County | 220 358 | 6.2 | 580 | 28.6 | No |
| Henan | |||||
| Zhengzhou City | 6 280 197 | 3.7 | 1470 | NA | Yes |
| Xin'an County | 483 000 | 4.3 | 902 | 27.4 | No |
GDP, gross domestic product; NA, not applicable.
*Population and socioeconomic information are from the 2000 Population Census of China.10
†The smoking prevalence rates (in a population aged 15–69 years) of Beijing and Chengdu are from the Report of internal evaluation of the World Bank Loan Health Promotion Project in China, 2002.11 The smoking prevalence rates (in a population aged 20–69 years) of Mianzhu, Anyi and Xin'an counties are from unpublished data from the baseline survey of the Fogarty project entitled “Building epidemiology, surveillance, and intervention capacity in China”, funded by the Fogarty International Center of the National Institutes of Health.11,12
‡Beijing banned smoking in public places on 15 May 1995, Chengdu on 1 January 1997, Nanchang on 1 October 1995, and Zhengzhou on 1 September 1998. Not applicable in Mianzhu County, Anyi County and Xin'an County. These regulations do not include restaurants and entertainment places. Smoking is banned in public transportation vehicles and in waiting rooms in the whole country, including rural areas.
Indoor airborne nicotine concentrations
A total of 273 monitors were placed, but 3 (1%) were lost during the fieldwork, leaving 270 air samples. Airborne nicotine was detected in 91% of the samples, ranging from 78% in Nanchang to 100% in Beijing (table 2). Overall, the median airborne nicotine concentration was 0.49 μg/m3 (interquartile range 0.07–2.28 μg/m3). Beijing had the highest median airborne nicotine concentration (3.01 μg/m3) compared with the other urban and rural areas. In the rural areas, the county with the highest median concentration was Anyi (1.04 μg/m3).
Table 2 Airborne nicotine concentrations in public places, China 2005.
| Samples (n) | Samples with nicotine detected* (%) | Median (IQR) nicotine concentration (μg/m3) | |
|---|---|---|---|
| Province | |||
| Beijing | 44 | 100.0 | 3.01 (0.47–7.35) |
| Sichuan | |||
| Chengdu City | 38 | 84.2 | 0.11 (0.01–0.36) |
| Mianzhu County | 37 | 97.3 | 0.57 (0.10–1.77) |
| Jiangxi | |||
| Nanchang City | 40 | 77.5 | 0.32 (0.02–1.99) |
| Anyi County | 36 | 94.4 | 1.04 (0.13–2.90) |
| Henan | |||
| Zhengzhou City | 39 | 92.3 | 0.56 (0.14–1.75) |
| Xin'an County | 36 | 94.4 | 0.48 (0.11–2.26) |
| Urbanisation | |||
| Beijing | 44 | 100.0 | 3.01 (0.47–7.35) |
| Other city | 117 | 84.6 | 0.27 (0.03–1.07) |
| County | 109 | 95.4 | 0.52 (0.10–2.28) |
| Public places | |||
| Hospital | 70 | 91.4 | 0.17 (0.05–1.73) |
| School | 70 | 78.6 | 0.10 (0.02–0.45) |
| Government | 42 | 97.7 | 0.48 (0.21–1.23) |
| Transportation | 12 | 91.7 | 0.68 (0.06–1.81) |
| Restaurant | 54 | 100.0 | 2.17 (1.02–4.63) |
| Entertainment | 22 | 100.0 | 7.48 (5.64–12.05) |
| Written regulation | |||
| Yes | 93 | 85.0 | 0.11 (0.03–0.72) |
| No | 177 | 94.9 | 1.00 (0.19–3.27) |
| Overall | 270 | 91.5 | 0.49 (0.07–2.28) |
IQR, interquartile range.
*Nicotine concentration above the limit of detection.
Nicotine was detected in most indoor public places surveyed, ranging from 70% of schools and hospitals to 100% of restaurants and entertainment places. Consistently across cities and rural areas, schools had the lowest nicotine concentrations (median 0.10 μg/m3), whereas restaurants (median 2.17 μg/m3) and entertainment places (7.48 μg/m3) had the highest (figure 1). Beijing consistently had the highest concentrations of nicotine in all public places, including schools and hospitals. Nicotine concentrations in schools and hospitals in rural counties exceeded concentrations found in the capital cities of the respective provinces. In government buildings, nicotine concentrations in Beijing greatly exceeded concentrations in other cities and rural areas. Nicotine concentrations in restaurants were high in all the cities and counties considered in the study, with highest concentrations in Beijing. Nicotine concentrations were highest in entertainment places, with median concentrations of 1.53 μg/m3 in Xinan County, 7.02 μg/m3 in Beijing, 7.48 μg/m3 in Mianzhu County and 12.36 μg/m3 in Anyi County. Entertainment places were not sampled in the other three cities.
Figure 1 Nicotine concentrations by type of public place and location in China. Horizontal lines within boxes indicate medians; boxes, interquartile ranges; error bars, values within 1.5 times the interquartile range; solid circles, outlying data points.
Overall, places with written smoking regulations had lower nicotine concentrations than places with no regulations. Lower nicotine concentrations were also found in schools and hospitals with written regulations (median 0.08 μg/m3) compared than in schools and hospitals with no regulations (median 0.31 μg/m3).
After adjustment for type of public place and presence of written regulations, nicotine concentrations in samples from Beijing were 7.4 times higher than in samples from Sichuan, the province with the lowest nicotine concentrations (table 3).
Table 3 Ratio of nicotine concentrations by location characteristics.
| Crude ratio (95% CI) | Adjusted* ratio (95% CI) | |
|---|---|---|
| Province | ||
| Sichuan | 1.00 | 1.0 |
| Beijing | 8.24 (3.58 to 18.97) | 7.4 (3.52 to 15.45) |
| Jiangxi | 1.94 (0.95 to 3.97) | 1.7 (0.94 to 3.10) |
| Henan | 1.89 (0.92 to 3.87) | 2.1 (1.11 to 3.79) |
| Public place | ||
| School | 1.00 | 1.0 |
| Hospital | 2.39 (1.26 to 4.54) | 2.4 (1.29 to 4.51) |
| Government | 4.98 (2.37 to 10.45) | 2.9 (1.31 to 6.46) |
| Transportation | 3.87 (1.18 to 12.69) | 3.4 (1.04 to 11.01) |
| Restaurant | 18.61 (9.35 to 37.06) | 11.0 (5.15 to 23.45) |
| Entertainment | 70.93 (28.00 to 179.69) | 38.4 (14.70 to 100.43) |
| Written regulation | ||
| Yes | 1.00 | 1.0 |
| No | 5.14 (2.92 to 9.04) | 2.3 (1.28 to 4.21) |
*Adjusted for other variables in the table.
Similarly, compared with schools, the public place with the lowest nicotine concentrations, hospitals, government buildings, train stations, restaurants and entertainment places had 2.4, 2.9, 3.4, 11.0 and 38.5 times higher nicotine concentrations, respectively. After similar adjustment, places with no written regulations had nicotine concentrations twice as high as other places.
Discussion
This study provides some of the first, large‐scale data on SHS concentrations in China. Airborne nicotine is a highly specific marker of tobacco combustion that can be detected at quite low concentrations. Findings indicate that SHS exposure in public places, including schools, hospitals, public transportation, restaurants and places of entertainment, is common across China. Key locations that should be smoke‐free—schools and hospitals—were widely contaminated with SHS. We expected SHS levels to be higher in rural areas, and indeed found SHS concentrations to be high in Anyi County and Henan Province. However, the highest SHS levels were in Beijing. In fact, some schools and hospitals in Beijing had concentrations that were comparable to those in restaurants and bars, and entertainment places. This could be related to the higher population density of Beijing compared with rural areas, which could explain the higher smoking densities in indoor places.
China has more smokers than any other country in the world.13 A majority of the male population, across the full socioeconomic gradient, are smokers. Even among physicians, for example, nearly the same percentage smoke as among farmers.4 With such a large smoking population, a high prevalence of involuntary exposure to SHS, a known cause of lung cancer, is a serious public health problem.2 China has signed and ratified the Framework Convention on Tobacco Control, which includes provisions for SHS restrictions, and thus is required to implement measures to reduce exposure. This study provides direct evidence on the nicotine concentrations to which people are exposed in different types of public places, as well as provides data comparing rural and urban areas.
Table 4 compares the nicotine concentrations in China with those measured using similar protocols in public places in European and Latin American cities.14,15 Overall, median nicotine concentrations in China were lower compared with measurements in Europe, but higher than in Latin America. However, the general patterns were similar across the three sets of measurements, and the highest concentrations were uniformly found in restaurants, bars and places of entertainment.
Table 4 Range of median nicotine concentrations in public places across cities in China, Europe and Latin America, 2001–5 .
| China*, n (range) | Europe†, n (range) | Latin America‡, n (range) | |
|---|---|---|---|
| Hospitals | 70 (0.02 to 2.21) | 93 (0.01 to 4.0) | 237 (<LD to 1.33) |
| Schools | 70 (0.02 to 0.64) | 119 (0.01 to 2.0) | 139 (<LD to 0.14) |
| Government buildings in cities | 42 (0.20 to 2.51) | — | 194 (<LD to 2.60) |
| Airports | 41 (0.04 to 5.7) | 148 (0.03 to 1.15) | |
| Train stations | 12 (0.04 to 10.22) | 39 (0.10 to 5.2) | — |
| Restaurants | 54 (0.18 to 4.91) | 100 (0.01 to 18) | 141 (0.15 to 2.52) |
| Bars/places of entertainment | 22 (1.53 to 12.36) | 40 (5 to 122)§ | 58 (1.26 to 6.21) |
*Beijing, Chengdu, Nanchang, Zhengzhou, Mianzhu, Anyi, Xinan
†Athens, Barcelona, Florence, Paris, Orebro, Vienna (Nebot et al. Tobacco Control 2005;14:60–3)
‡Asunciŏn, Buenos Aires, Ciudad de Panamá, Lima, Mexico D.F., Montevideo, Rio de Janeiro, San José, Santiago, Tegucigalpa (Navas‐Acien et al. JAMA 2004;291:2741–5 and personal communication)
§Measured only during time of occupancy.
LD, limit of detection.
Several potential limitations need consideration in interpreting our findings. First, we made measurements on a continuous basis and not during the time of occupancy only. As a result, the nicotine concentrations reported are likely to underestimate the actual concentrations during the time of occupancy. Second, the measurements were carried out by different groups of researchers, and, although trained uniformly, some variation in findings could have resulted due to variation in the way the data were collected. Researchers made decisions of where to locate the monitors, and placements may have differed with respect to proximity of the monitors to smokers. We attempted to reduce differences in data collection by providing and training researchers with a simple protocol, especially on where and how to place the monitors.
Third, building structures differ greatly from one area to another, and some of the differences in nicotine concentrations could be related to the characteristics of the structures and how open they are to the outside environment, mainly the number of doors and windows and whether they are open or closed—factors that determine the exchange of indoor air with outdoor air. Researchers did provide detailed accounts of the number and location of doors and windows in the area where the monitors were placed and we also collected information concerning whether the windows and doors were open, which would increase the mixing of air in those areas. These building characteristics were not associated with nicotine concentrations. Other factors related to differences in nicotine concentrations are the amount of smoking and the size of the space monitored. Owing to the feasibility and resources available, we did not collect information on these factors. However, our purpose was not to evaluate the determinants of exposure to SHS in public places in China. Rather, we intended to develop policy‐relevant monitoring data that would document and quantify the presence of nicotine in key locations where people work or spend time.
We also assessed the effect of having a written smoke‐free policy (tables 2 and 3). Studies in the United States and elsewhere show that such policies reduce concentrations of SHS.2 We found that having a written regulation was associated with lower levels of nicotine concentration. However, only 93 of the 270 (34%) public places included in the study were covered by a written policy on smoking. We did not assess the nature of the policy, the level of coverage and whether these policies were actually implemented or enforced. In actuality, having a written policy that is not properly implemented or enforced or just posting no smoking signs does not provide protection and is not sufficient to reduce exposure.
Beyond their direct health benefit, smoke‐free policies change social norms and the social acceptance of smoking by the population. Having smoke‐free laws and policies, especially in work sites, promotes cessation, reduces consumption and promotes a non‐smoking social norm.16,17 For China, changing the social norms around smoking is exceedingly critical at present. This is not an easy task, since it must involve the health sector as well as the economic and social sectors for change to occur. But there are indications that change is beginning to occur in China. For example, an editorial in the China Daily proposes that it is not sufficient to just tell people not to smoke in public places but that administrators of these public places should be “responsible for violations in their places”.18 The discussion of these issues in the popular press demonstrates that dialogue is happening and that there is interest in creating smoke‐free environments.
The information from this study should be useful for tobacco control programmes in China, where protection against SHS exposure is still inadequate. The data indicate the high prevalence of exposure in many public places and provide a baseline for gauging the impact of needed interventions. Shanghai had a law covering hospitals, schools and some public locations as early as 1994. In January 1997, the Ministry of Health, Ministry of Rail Transportation, Ministry of Road Transportation and Ministry of Construction and Civil Aviation Bureau issued a regulation to prohibit smoking in public transportation vehicles and in waiting rooms in the whole country. However, implementation and enforcement are incomplete. By April 2000, some provinces and 88 cities in China had passed local bans prohibiting smoking in public places, including hospitals, schools, government offices, traffic stations and transportation vehicles. However, as shown by this study, SHS exposure in public places needs to be better addressed. Currently, China is developing a new national tobacco control plan that will cover SHS. Our monitoring data indicate the need for this plan and for enforced implementation of measures to control SHS.
What this paper adds
This paper focuses on China, which has the largest population of smokers in the world, and has signed and ratified the World Health Organization's Framework Convention on Tobacco Control, but so far has had few controls to limit exposure to second‐hand smoke (SHS).
China is a particularly critical nation in the global effort to control tobacco use due to the enormity of the potential loss of life faced by China in the next decade, which is directly related to smoking.
This study provides some of the first, large‐scale data on SHS concentrations in China. The data indicate that there is high prevalence of exposure to SHS in many public places, including hospitals and government offices.
Data provided by this study can be used as a baseline for gauging the impact of future interventions.
In addition, information from this study should be useful for planning tobacco control programmes in China, where protection against SHS exposure is still inadequate.
Acknowledgements
This work was supported by the Fogarty International Center of the National Institutes of Health in the United States grant number R01‐HL‐73699. We thank Liu Na for her contribution to the project.
Abbreviations
SHS - second‐hand smoke
Footnotes
Competing interests: None.
References
- 1.The World Health organization The World Health Report 2002—reducing risks, promoting healthy life. Geneva, Switzerland: WHO, 2002, http://www.who.int/whr/2002/en/index.html (accessed 28 Mar 2007)
- 2.US Department of Health and Human Services The health consequences of involuntary exposure to tobacco smoke: a Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2006
- 3.Muggli M, Hurt R, Blanke D. Science for hire: a tobacco industry strategy to influence public opinion on secondhand smoke. Nicotine Tob Res 20035303–314. [DOI] [PubMed] [Google Scholar]
- 4.Yang G, Fan L, Tan J.et al Smoking in China: findings of the 1996 National Prevalence Survey. JAMA 19992821247–1253. [DOI] [PubMed] [Google Scholar]
- 5.Esson K, Leeder S.The millennium development goals and tobacco control: an opportunity for global partnership. Geneva, Switzerland: World Health Organization, 2004, http://www.who.int/tobacco/research/economics/publications/mdg_book/en/index.html (accessed 28 Mar 2007)
- 6.China Daily Lawmaker calls for ban on public smoking. China Daily 4 Mar 2006. http://www.china.org.cn/english/China/160072.htm (accessed 28 Mar 2007)
- 7.Hammond S. Evaluating exposure to environmental tobacco smoke. In: Winegar E, Keith L, eds. Sampling and analysis of airborne pollutants. Boca Raton, FL: Lewis Publishers, 1993319–338.
- 8.Hammond S, Leaderer B. A diffusion monitor to measure exposure to passive smoking. Environ Sci Technol 198721494–497. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services (USDHHS), Centers for Disease Control and Prevention Third national report on human exposure to environmental chemicals. Atlanta, GA: National Center for Environmental Health, Division of Laboratory Sciences, 2005
- 10.China National Bureau of Statistics, Department of Population, Social, Science and Technology Statistics China population statistics yearbook. Beijing, China: China Statistics Press, 2000
- 11.China Centers for Disease Control and Prevention The internal evaluation report on health promotion component of disease prevention project of China. Beijing, China: China Centers for Disease Control and Prevention, 2002, http://www.chinacdc.net.cn/n272442/n272530/n275462/n275477/n292894/appendix/total%20report%20final0526.pdf (accessed 28 Mar 2007)
- 12.Stillman F, Yang G, Figueiredo V.et al Building capacity for tobacco control research and policy. Tob Control 200615(Suppl 1)i18–i23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peto R, Chen Z, Boreham J. Tobacco—the growing epidemic in China. JAMA 19962751683–1684. [DOI] [PubMed] [Google Scholar]
- 14.Nebot M, Lopez M J, Gorini G.et al Environmental tobacco smoke exposure in public places of European cities. Tob Control 20051460–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Navas A, Peruga A, Breysse P.et al Secondhand smoke in public places in Latin America, 2002–2003. JAMA 20042912741–2745. [DOI] [PubMed] [Google Scholar]
- 16.Stillman F A, Becker D M, Swank R T.et al Ending smoking at the Johns Hopkins Medical Institutions. An evaluation of smoking prevalence and indoor air pollution. JAMA 19902641565–1569. [PubMed] [Google Scholar]
- 17.Farrelly M C, Evans W, Sfekas A. The impact of workplace smoking bans: results from a national survey. Tob Control 19998272–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weihua C. Time to kick nation's smoking addiction. China Daily. 29 Apr 2006. http://www.chinadaily.com.cn/opinion/2006‐04/29/conent_579986.htm (accessed 28 Mar 2007)