Abstract
Objectives
To assess the impact of interventions targeted towards female sex workers (FSWs) and their male clients on client HIV/STI prevalence and sexual behaviour.
Methods
From 1993 to 2006, an HIV/STI preventive intervention focusing on condom promotion and STI care was implemented among FSWs in Cotonou, Benin, and then expanded to cover their male sexual partners in 2000. The interventions were scaled up to five other cities of Benin in 2001–2002. Serial cross‐sectional surveys of HIV/STI prevalence and sexual behaviour were carried out among clients in Cotonou in 1998, 2002 and 2005; and in the five other cities (O/Cotonou) in 2002 and 2005.
Results
Significant declines in gonorrhoea prevalence among clients of FSWs: Cotonou, from 5.4% in 1998 to 1.6% in 2005; O/Cotonou: from 3.5% in 2002 to 0.59% in 2005. Chlamydia prevalence also declined O/Cotonou, from 4.8% to 1.8%, while HIV prevalence remained stable. Reported condom use by clients with both FSWs and casual non‐FSW partners, but not regular partners, increased significantly. While condom use at last sex with an FSW was similar in Cotonou to O/Cotonou around the time of implementation of the interventions (56% in 1998 vs 49% in 2002, respectively), it had risen to similar levels by 2005 (95% and 96%, respectively).
Conclusions
These results demonstrate that it is possible to implement preventive and clinical services for clients of FSWs, and suggest that such interventions, integrated with those targeted towards FSWs, can have a significant effect on sexual behaviour and STI prevalence (particularly gonorrhoea) among this population.
Benin (population ∼6 million), in West Africa, has experienced a relatively low‐level, concentrated HIV epidemic, with high differentials in HIV prevalence between high‐risk groups (FSWs and their clients) and the “general” population.1 The first case of AIDS was reported in 1985, and subsequently there was a gradual progression of HIV/AIDS throughout the country during the 1990s, with increases in yearly numbers of reported cases as well as in sentinel prevalence figures from pregnant women. Since 2002, sentinel HIV prevalence in pregnant women has remained stable at around 2%, varying from 0.3% to 3.3% according to region.2
HIV prevalence levels have been 10–20 times higher in female sex workers (FSWs) than in women in the general population. Prevalence is also several‐fold higher in male clients of FSWs than in men in the general population. For example, in 1998, HIV prevalence in Cotonou (population ∼800 000: the main city of Benin and an important port) among FSWs was 41%, among clients 8.4%, among regular partners of FSWs 16.1%, and among men and women in the general population, 3.3% and 3.4%, respectively.3,4,5 Data from other West African countries, notably Ghana and Senegal, show similar patterns,6,7,8 while data from Cote d'Ivoire, where the HIV epidemic is more mature, indicate a smaller differential in HIV prevalence between clients and the general population.9
Previous studies have indicated that a very high proportion of HIV infections in the general population in Cotonou are likely to be due to commercial sex, with male clients forming a bridge for HIV transmission from FSWs to low‐risk (mainly monogamous) women in the general population.1 In Cotonou, results of surveys among FSWs and their clients suggest that up to 30% of the male population may visit FSWs in any one year, and that the population attributable fraction of exposure to FSWs for prevalent HIV in men may be as high as 76%.10,11
Mathematical modelling of preventive interventions directed towards FSWs (gonorrhoea screening and condom use) indicates that in an epidemiological context such as Cotonou, core group interventions can significantly reduce HIV incidence and prevalence among FSWs themselves and in the general population of low‐risk women.12 Evidence from countries in southern and eastern Africa indicates that even in generalised epidemics, the contribution of commercial sex to the HIV epidemic, and thus the implementation of interventions directed towards both FSWs and clients, continues to be important.13,14
This paper describes the results of a pilot intervention targeted to male clients of FSWs in Cotonou, which was subsequently implemented in Cotonou in 2001, and later in other main cities in Benin. Data from serial integrated biological and behavioural surveys (IBBS) suggesting positive effects of the intervention on risky sexual behaviour and STI rates, in both Cotonou and other main cities in Benin, are then presented.
Methods
Background
From 1993 to 2006, a HIV/STI preventive intervention project was implemented in Cotonou, Benin, funded by the Canadian International Development Agency. This intervention initially targeted FSWs, and included STI care using clinical screening algorithms applied at regular clinic visits, condom promotion, and activities aiming at capacity building, community development and empowerment.
In 2000, following a study among clients and regular partners of FSWs in Cotonou, which demonstrated high HIV prevalence among these men as well as high levels of sexual risk behaviour, notably unprotected sex and concurrency with both FSWs and “low‐risk” women,5 a pilot intervention targeting these men was set up.
Interventions targeting both FSWs and clients were progressively scaled up to five other cities of Benin (Porto‐Novo, Abomey‐Bohicon, Parakou, Kandi, Malanville) in 2001–2002. The six cities where the intervention was implemented comprise approximately 25% of the population of Benin, and around 70% of all FSWs enumerated in Benin in 2004.15
Pilot intervention targeted towards male clients of FSW
Outreach work at prostitution venues and surrounding areas was carried out mainly at night by trained male peer outreach workers/educators (MPEs). The latter approached male clients at prostitution venues, either singly or in groups, and, with the aid of flip charts and other supports, discussed HIV and STI transmission risks with them and carried out condom demonstrations with a wooden penis.
A confidential, free STI clinic specifically for men [the Clinique des Amis de Cotonou (CAC)] was set up near one of the main prostitution areas in Cotonou, where men were offered physical examinations, a leucocyte esterase dipstick (LED) test for urethritis, syndromic treatment, risk‐reduction counselling and education about STIs and condom use.
MPEs also administered simple questionnaires to a convenience sample of clients in the field, collecting data on basic demographics and condom use, and on whether the client had been previously exposed to the intervention (either in the field or by visiting the STI clinic). They also assessed the ability of clients to correctly put a condom on a wooden penis.
During the pilot, approximately 15 000 individual contacts were made with men at sex work sites, and leaflets and condoms were distributed. Film projections were made in public places where appropriate, and stickers, calendars, caps, leaflets and posters (promoting the CAC) were distributed.
Following a positive evaluation, 1 year after its implementation, the intervention was then progressively scaled up.
IBBS
Within the project, serial cross‐sectional surveys of HIV/STI prevalence and sexual behaviour were carried out among clients of FSWs in Cotonou in 1998, 2002 and 2005, as well as in the five other cities in 2002 and 2005.
Clients were defined as men who came to one of the prostitution venues included in the study, and who paid to have sex with an FSW there. The design and implementation of IBBS among male clients has been previously described in detail.5 Ethical approval for the study protocol was given by the Ethics Committee of the Centre hospitalier affilié universitaire de Quebec and by the Ministry of Health, Benin.
Before commencing IBBS, a census of prostitution venues in each town was carried out, to map the sites and estimate the size of the FSW population at each site. In the 1998 study in Cotonou, clients were recruited from a diversified sample of prostitution venues.5 In the 2002 and 2005 studies, venues were randomly selected using probability proportional to the size of the FSW population at each site. The universe of prostitution venues sampled in Cotonou was the same, in terms of both sex work typology and geographical spread, in all three surveys.
Data and sample collection were carried out for several nights from about 8 pm to 1 am at each site. Male clients, who were about to enter the room of the FSW with whom they were going to have sex, were individually approached by an MPE, who, with the aid of the FSW, explained the purpose of the study to the client and invited him to participate. At any given recruitment site during a specific data‐collection period, collaboration to recruit clients was obtained from all the FSWs present.
After giving informed verbal consent, the client provided a urine sample in a plastic container, just before having sex with the FSW, which was subjected to an LED test (Boehringer Mannheim Chemstrip 10A; Quebec, Canada). After having had sex with the FSW, the client was interviewed using a structured questionnaire, and underwent a genital examination. Free syndromic STI treatment for urethritis and genital ulcers was provided based on symptoms, signs and results of the LED test (a + or ++ reading).
Urine samples were tested for HIV‐1 antibodies using an enzyme immunoassay, with confirmation of initially positive results by urine western blot (Calypte Biomedical Corporation, Berkeley, CA);16,17 and for Neisseria gonorrhoeae (NG) and Chlamydia trachomatis (CT) using nucleic acid amplification tests (Amplicor CT/NG dual detection assay; Roche Diagnostics, Branchburg, NJ), in all surveys.
Coded data were double‐entered and verified in Epi‐Info (Centers for Disease Control and Prevention, Atlanta, GA; World Health Organisation, Geneva); statistical analyses were performed using Epi‐Info and SAS (SAS Institute, Cary, NC).
Results
Pilot intervention results
After one year of implementation in Cotonou, data from client interviews suggested that the intervention had had at least a short‐term impact on knowledge and sexual behaviour among clients of FSW, and particularly on rates of correct condom use in this population (table 1). Among clients who had been exposed to the intervention (either in the field or through visiting the STI clinic), compared with those who had not, significantly higher proportions had used a condom with the FSW they had just had sex with, had put the condom on themselves and were able to demonstrate correctly how to put a condom on a wooden penis (table 1).
Table 1 Relationship between exposure to the pilot intervention and condom use among clients of FSWs in Cotonou, July 2000 to April 2001.
| Whole sample (n = 355) (%) | Not exposed to intervention (n = 266)* (%) | Exposed to intervention (n = 89)* (%) | Odds ratio | p value† | |
|---|---|---|---|---|---|
| Condom use with FSW just had sex with | 65 | 62 | 74 | 1.7 | 0.044 |
| Client put condom on | 22 | 18 | 32 | 2.1 | 0.023 |
| Accept to demonstrate how to put condom on wooden penis | 59 | 50 | 87 | 6.3 | <0.001 |
| Correct condom demonstration on wooden penis | 37 | 22 | 65 | 6.7 | <0.001 |
*Exposed to intervention: in the field through contact with a male peer outreach worker and/or by visiting the STI clinic. †chi square test
Splitting the whole sample up into three consecutive time periods from the start of the pilot intervention onwards (July–September 2000; October–December 2000; January–April 2001), there was a significant overall increase in reported condom use rates with FSW: from 52% (61/118), through 67% (84/126), to 78% (87/111), (p<0.001, test for trend).
During the period of the intervention, 625 men visited the STI clinic. This number increased from ∼30 visits/month during the first months of the intervention, to stabilise at ∼60 visits/month.
IBBS
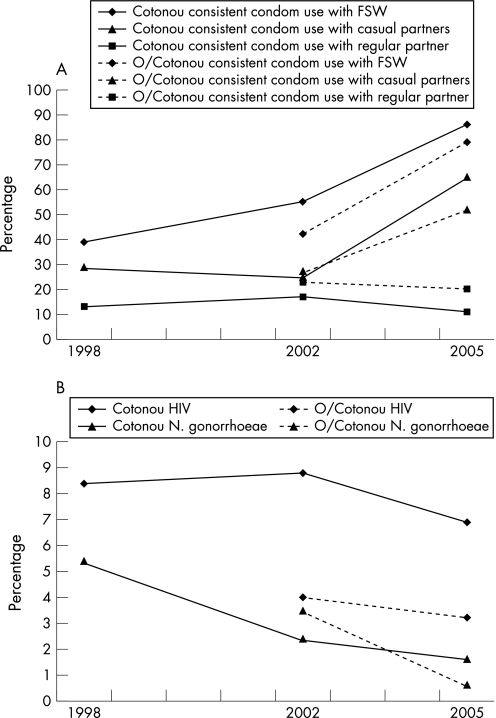
Data from serial IBBS carried out in Cotonou (1998, 2002, 2005) and in cities outside Cotonou (2002 and 2005) are presented in tables 2 and 3, respectively, and fig 1. Data from Porto Novo, Abomey‐Bohicon and Parakou are combined in table 3 due to small sample sizes. Data from Malanville and Kandi are not included, since they are available only for 2005.
Table 2 Time trends in sexual behaviour and STI/HIV prevalence among male clients of female sex workers: Cotonou, 1998–2005.
| Cotonou | 1998 | 2002 | 2005 | p value |
|---|---|---|---|---|
| Commercial sex partners | n = 330* | n = 602* | n = 298* | |
| Frequency visit FSW/year: mean (median) | 32 (24) | 11.1 (5) | 19.8 (12) | <0.001† |
| Condom used last sex act with FSW | 55.8% | 68.1% | 94.6% | <0.001 |
| Consistent condom use with FSW | 39.0% | 55.1% | 86.2% | <0.001 |
| Non‐commercial sex partners | ||||
| Is married or has a regular girlfriend | 79.9%† | 83.3%§ | 54.8%** | NC |
| Consistent condom use regular partner | 13.1% | 16.8% | 11.4% | 0.71 |
| Has casual (non‐FSW) sex partners | 34.7%† | 68.2%§ | 16.6%** | NC |
| Condom used last sex with casual sex partner | NA | 47.3% | 85.7% | <0.001‡ |
| Consistent condom use with casual sex partners | 28.6% | 24.5% | 65.3% | <0.001 |
| HIV/STI prevalence | n = 404* | n = 630* | n = 313* | |
| HIV | 8.4% | 8.8% | 6.9% | 0.59 |
| Neisseria gonorrhoeae | 5.4% | 2.4% | 1.6% | <0.01 |
| Chlamydia trachomatis | 2.7% | 4.0% | 3.2% | 0.59 |
NA, data not available for that survey round. NC, variables not directly comparable (significance testing not carried out).
*Total sample size for each round: denominators for specific variables vary due to incomplete data, as in some cases men left before the interview was finished, or chose not to answer specific questions. Denominators for biological assays are higher than those for interview, since some men gave a a urine sample before having sex with a FSW, and then left after having had sex, having decided not to give an interview; †currently; §had sex with in last year; **had sex with in last 3 months; p value: chi square test for trend; †analysis of variance; ‡chi square test.
Table 3 Time trends in sexual behaviour and STI/HIV prevalence among male clients of female sex workers: Abomey‐Bohicon, Parakou and Porto‐Novo, 2002–2005.
| Abomey‐Bohicon. Parakou. Porto‐Novo | 2002 | 2005 | p value* |
|---|---|---|---|
| Commercial sex partners | (n = 297)† | (n = 343)† | |
| Frequency visit FSW/year: mean (median) | 10.8 (7) | 14.8 (8) | <0.001* |
| Condom used last sex act with FSW | 49.0% | 95.9% | <0.001 |
| Consistent condom use with FSW | 41.8% | 79.4% | <0.001 |
| Non‐commercial sex partners | |||
| Is married or has a regular girlfriend | 86.5%‡ | 70.8%§ | NC |
| Consistent condom use with regular partner | 22.5% | 19.9% | 0.76 |
| Has casual (non‐FSW) sex partners | 34.1%‡ | 26.6%§ | NC |
| Condom used in last sex act with casual partner | 41.5% | 68.2% | <0.001 |
| Consistent condom use with casual partners | 26.6% | 52.3% | <0.001 |
| HIV/STI prevalence | (n = 311)† | (n = 341)† | |
| HIV | 4.0% | 3.2% | 0.75 |
| Neisseria gonorrhoeae | 3.5% | 0.59% | 0.03 |
| Chlamydia trachomatis | 4.8% | 1.8% | 0.047 |
p value: chi square test; *Student t test. †total sample size for each round: denominators for specific variables vary due to incomplete data, as in some cases men left before the interview was finished or chose not to answer specific questions. Denominators for biological assays are higher than those for interview, since some men gave a a urine sample before having sex with an FSW, and then left after having had sex, having decided not to give an interview; ‡had sex with in last year; §had sex with in last 3 months.
NC, variables not directly comparable (significance testing not carried out)
Figure 1 (A) Time trends in sexual behaviour among male clients of female sex workers: Benin, 1998–2005. O/Cotonou: outside Cotonou. (B) Time trends in HIV/STI prevalence among male clients of female sex workers: Benin, 1998–2005. O/Cotonou: outside Cotonou.
About 300–400 clients took part in each round of the IBBS in and outside Cotonou, except in Cotonou in 2002 where ∼600 clients participated. Participation rates were similar between survey rounds and varied between 60% and 75% according to study site. Median age of clients varied between 25 and 26 years in Cotonou, and between 23 and 24 years in the other cities. Between 98.0% and 99.7% of clients reported being circumcised.
Men reported visiting FSWs on average between 11 and 32 times per year in Cotonou, and between 11 and 15 times per year outside Cotonou (tables 2 and 3). After an initial drop in Cotonou, the visit frequency increased from 2002 to 2005 in both sites.
Reported condom use rates with all partner types were similar in Cotonou in 1998 to those outside Cotonou in 2002 (eg, condom used in last sex act with FSW: 56% vs 49%, respectively; consistent condom use with casual partners: 29% vs 27%, respectively). Both in and outside Cotonou, reported condom use rates with FSW, and with casual non‐FSW partners, increased significantly over time (tables 2 and 3; fig 1A). By 2005, rates were similar in both sites for FSWs (eg, condom used in last sex act with FSW: 95% vs 96%, respectively); while condom use rates with casual partners were higher in Cotonou (eg, condom use last casual partner: 86% vs 68%, p = 0.042), although not significantly so for consistent condom use with casual partners (65% vs 52%, p = 0.20).
In contrast, reported condom use rates with regular partners did not increase over time either in or outside Cotonou.
Both in and outside Cotonou, significant declines in gonorrhoea prevalence occurred over time, whereas HIV prevalence did not change significantly. Chlamydia prevalence did not change significantly over time in Cotonou, although there was a borderline significant decrease in prevalence outside Cotonou (tables 2 and 3; fig 1B).
Discussion and conclusions
In this paper, we present data from observational studies of male clients of FSWs in Cotonou and other main cities in Benin. IBBS data from studies with clients carried out in 1998 (Cotonou only), 2002 and 2005 (all towns) indicate that over the period of implementation of the intervention in both sites, condom use rates with both FSWs and other (non‐FSW) casual female partners increased significantly over time, while rates of gonorrhoea decreased significantly.
While recognising the limitations of observational data in providing conclusive evidence of the effectiveness of HIV/STI preventive interventions, the internal consistency of the data (in terms of different indicators giving the same trends), as well as their consistency over time and in different sites, lends weight to the hypothesis that the interventions themselves, as opposed to other factors, have contributed to positive changes in indicators of behavioural risk and STI prevalence among clients. In particular, the later time of implementation of the project outside Cotonou allows the examination of the data as if resulting from a natural experiment. While reported condom use rates with FSWs were similar in Cotonou to those outside Cotonou around the time of implementation of the interventions (1998 and 2002, respectively), by 2005 rates had risen to very similar levels in both sites. This is also the case for decreases in gonorrhoea prevalence.
A more rapid increase in condom use rates with FSW, and corresponding decrease in gonorrhoea prevalence, occurred outside Cotonou. Also, the rate of increase in condom use with FSWs was significantly higher in Cotonou from 2002 to 2005 than from 1998 to 2002. One possible explanation for these findings is that scaling up of the intervention to a high proportion of clients and FSWs in Benin accelerated changes in behaviour and STI prevalence. FSWs, and to some extent clients, are highly mobile populations, and thus expanding the intervention to most large cities in Benin may have avoided re‐seeding infections from one city to another; as well as affecting condom use rates. It is also possible that the simultaneous implementation of interventions targeted towards both FSWs and their clients may have accelerated the rate of decline in STI prevalence and the increase in condom use rates in commercial sex encounters.
Given the long incubation period of AIDS, a stable HIV prevalence may well indicate a decrease in incidence over time. However, the stable chlamydia prevalence observed, compared with the decrease in gonorrhoea prevalence, may indicate a phase‐specific effect of the intervention. In contrast to gonorrhoea, the differential between chlamydia prevalence in high‐risk groups and the general population is small in Cotonou.1,3,4 Chlamydia may therefore be in a more endemic phase than gonorrhoea, where transmission among the low‐risk population may account for persistence, even in the presence of reduced transmission among high‐risk groups.
In addition to its observational nature, there are a number of potential limitations to this study. First, activities implemented by the National AIDS Programme, especially global AIDS awareness campaigns, may have partly contributed to the increase in condom use and subsequent decrease in STIs, although they cannot easily account for the differences observed between Cotonou and the other majn cities in Benin in 2002. Second, self‐reporting of condom use is prone to social desirability bias; it is however recognised that clients report lower condom use than FSWs.6 In a study carried out in Cotonou in parallel to the 2002 IBBS, we observed that, while FSWs and their clients usually gave the same answer about condom use in the sexual intercourse they had just had, most of the discrepancies were related to lower reported condom use by the clients.18 Finally, 25–40% (depending on the surveys) of the clients contacted did not participate, which could result in selection bias. However, participation rates were similar to those reported in other studies on clients of FSWs7,9 and to those reported in the National Survey of Sexual Attitudes and Lifestyle carried out in the UK from 1999 to 2001.19,20 In addition, non‐participation was in part due to a lack of sufficient staff to ensure that all clients approached would have their urine sample collected and their interview administered without waiting, particularly in very busy prostitution venues.
It is not possible to separate out the extent to which the decreased STI rates or increased condom use rates with FSWs among the clients were due to the interventions directed towards the FSWs themselves21 or to the male clients. Studies in other settings have shown declines in client STI prevalence as a result of interventions directed towards FSWs.22,23 However, in this study, the findings from the pilot intervention concerning the ability of the clients themselves to correctly put a condom on a wooden penis, and the proportions of clients who had put the condom on themselves (as opposed to the FSW putting it on), do suggest at least some direct effects on the clients' behaviour. The reported increases in condom use rates by clients with casual non‐FSW partners also suggest that behavioural change occurred among the clients themselves. It is also possible that focusing on “both sides of the equation” is a more effective way of achieving behavioural change than focusing only on FSWs. Given the prevailing nature of gender power relations, particularly in developing countries, as well as the high mobility and turnover rates characteristic of FSW populations in many settings, if both male clients and FSWs can be reached by preventive interventions, the likelihood that sustainable behavioural change during commercial sex will be achieved may be considerably enhanced.
Key messages
At least in some areas of sub‐Saharan Africa, it is possible to reach male clients of female sex workers (FSWs) for HIV/STI preventive and clinical services
Preventive interventions directed towards both FSWs and their clients may be synergistic in achieving a significant effect on sexual risk behaviour, as well as on STI rates (particularly gonorrhoea), in these populations
Scaling up coverage to the country level may enhance the impact of interventions targeted towards FSWs and clients in any particular setting covered
Acknowledgements
The authors are grateful to all the men who agreed to participate in the different surveys, and to the personnel of the Projet SIDA‐1/2/3‐Benin, particularly the male peer outreach workers.
Contributions
CML was the principal investigator of the study in 1998, was in charge of the evaluation of the pilot intervention, carried out the data analyses presented in this paper and drafted the manuscript. MA was the director of Projets SIDA‐1, ‐2 and ‐3 in Benin; he was principal investigator for the 2005 survey, commented on the initial version of the manuscript and reviewed it following the reviewers' comments. ACL was the principal investigator for the 2002 survey; she was also in charge of laboratory testing for gonorrhoea and chlamydia in the 2002 and 2005 surveys. CG was responsible for the data collection in 1998 and contributed to data analysis. MB supervised all the logistical aspects of the studies and managed the implementation of the scaled‐up intervention. LM supervised the pilot intervention and contributed to the design of the studies. HM coordinated data collection in 2002. MN coordinated data collection in 2005. SA was director of the Benin National AIDS Control Programme during the 1998 and 2002 surveys and in charge of HIV testing for these surveys. AG was the director of the Benin National AIDS Control Programme during the 2005 surveys and in charge of HIV testing for these surveys. All the authors reviewed the manuscript and approved its content.
Abbreviations
CAC - Clinique des Amis de Cotonou
FSW - female sex worker
IBBS - integrated biological and behavioural surveys
LED - leucocyte esterase dipstick
Footnotes
Sponsorship: This study was funded in part by the Canadian International Development Agency through its West African AIDS Project (Project SIDA‐1/2/3) executed by the Centre de Coopération Internationale en Santé et Développement Inc. (Québec, Canada). Diagnostic kits for HIV‐1 for the 1998 study were provided by Calypte Biomedical Corporation, Berkeley, California, USA. MA is a National Researcher of the Fonds de la Recherche en Santé du Québec, Canada (grant # 8722). CG was the recipient of an MSc training award from the World Health Organization.
Competing interests: None declared.
References
- 1.Lowndes C M, Alary M, Meda H.et al Role of core and bridging groups in the transmission dynamics of HIV and sexually transmitted infections in Cotonou, Benin, West Africa. Sex Transm Infect. 2002;78(Suppl 1)i69–i77. [DOI] [PMC free article] [PubMed]
- 2. République du Bénin, Ministere de la Santé, Direction Nationale de la Protection Sanitaire, Programme National de Lutte contre le SIDA. Rapport de Surveillance de l'Infection à VIH et de la Syphilis au Bénin—Année 2006
- 3.Alary M, Mukenge‐Tshibaka L, Bernier F.et al Decline in the prevalence of HIV and sexually transmitted diseases among female sex workers in Cotonou, Benin, 1993–99. AIDS 2002161–8. [DOI] [PubMed] [Google Scholar]
- 4.Buvé A, Caraël M, Hayes R J.et al Multicentre study on factors determining differences in rate of spread of HIV in sub‐Saharan Africa: methods and prevalence of HIV infection. AIDS. 2001;15(Suppl 4)5–14S. [DOI] [PubMed]
- 5.Lowndes C M, Alary M, Gnintoungbé C A B.et al Management of sexually transmitted diseases and HIV prevention in men at high risk: targeting clients and non‐paying sexual partners of female sex workers in Benin. AIDS 2000142523–2534. [DOI] [PubMed] [Google Scholar]
- 6.Côté A M, Sobela F, Dzokoto A.et al Transactional sex is the driving force in the dynamics of HIV in Accra, Ghana. AIDS 200418917–925. [DOI] [PubMed] [Google Scholar]
- 7.Espirito Santo M E, Etheredge G D. How to reach clients of female sex workers: a survey by surprise in brothels in Dakar, Senegal. Bull World Health Organ 200280709–713. [PMC free article] [PubMed] [Google Scholar]
- 8.Gomes do Espirito Santo M E, Etheredge G D. Male clients of brothel prostitutes as a bridge for HIV infection between high risk and low risk groups of women in Senegal. Sex Transm Infect 200581342–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vuylsteke B L, Ghys P D, Traoré M.et al HIV prevalence and risk behavior among clients of female sex workers in Abidjan, Côte d'Ivoire. AIDS 2003171691–1694. [DOI] [PubMed] [Google Scholar]
- 10.Lowndes C M, Alary M, Labbe A ‐ C.et al Male clients of female sex workers in Cotonou, Benin (West Africa): Contribution to the HIV epidemic and effect of targeted interventions. 15th Biennial Congress of the International Society for Sexually Transmitted Diseases Research, Ottawa, 27–30 July 2003 [abstract 0729].
- 11.Alary M, Lowndes C M. Editorial: the central role of clients of female sex workers in the dynamics of heterosexual HIV transmission in sub‐Saharan Africa. AIDS 200418945–947. [DOI] [PubMed] [Google Scholar]
- 12.Boily M ‐ C, Lowndes C M, Alary M. The impact of past and future core group interventions in low and high HIV prevalence epidemics: insights from mathematical models. Sex Transm Infect. 2002;78(Suppl 1)i78–i90. [DOI] [PMC free article] [PubMed]
- 13.Cowan F M, Langhaug L F, Hargrove J W.et al Is sexual contact with sex workers important in driving the HIV epidemic among men in rural Zimbabwe? J Acquir Immune Defic Syndr 200540371–376. [DOI] [PubMed] [Google Scholar]
- 14.Morris C N, Ferguson A G. Estimation of the sexual transmission of HIV in Kenya and Uganda on the trans‐Africa highway: the continuing role for prevention in high risk groups. Sex Transm Infect 200682368–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vandepitte J, Lyerla R, Dallabetta G.et al Estimates of the number of female sex workers in different regions of the world. Sex Transm Infect. 2006;82(Suppl III)iii18–iii25. [DOI] [PMC free article] [PubMed]
- 16.Berrios D C, Avins A L, Haynes‐Sanstad K.et al Screening for human immunodeficiency virus antibody in urine. Arch Pathol Lab Med 1995119139–141. [PubMed] [Google Scholar]
- 17.Oelemann W M, Lowndes C M, Veríssimo da Costa G C.et al Diagnostic detection of human immunodeficiency virus type 1 antibodies in urine: a Brazilian study. J Clin Microbiol 200240881–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geraldo N, Labbé A C, Meda H.et al Condom use in Cotonou and Porto Novo (Bénin): How different are self‐reports by female sex workers (FSW) and by their clients? Proceedings of the 15th Annual Congress of the International Society for Sexually Transmitted Diseases Research; Ottawa, 27–30 July 2003
- 19.Johnson A M, Mercer C H, Erens B.et al Sexual behaviour in Britain: partnerships, practices, and HIV risk behaviours. Lancet 20013581835–1842. [DOI] [PubMed] [Google Scholar]
- 20.McCadden A, Fenton K A, McManus S.et alChlamydia trachomatis testing in the second British national survey of sexual attitudes and lifestyles: respondent uptake and treatment outcomes. Sex Transm Dis 200532387–394. [DOI] [PubMed] [Google Scholar]
- 21.Alary M, Lowndes C M, Labbe A ‐ C.et al Interventions aimed at sex workers in Cotonou, Benin (West Africa): Ongoing decline of STDs over a decade. 15th Biennial Congress of the International Society for Sexually Transmitted Diseases Research, Ottawa, 27–30 July 2003 [Abstract 0728].
- 22.Steen R, Vuylsteke B, DeCoito T.et al Evidence of declining STD prevalence in a South African mining community following a core‐group intervention. Sex Transm Dis 2000271–8. [DOI] [PubMed] [Google Scholar]
- 23.Wi T, Ramos E R, Steen R.et al STI declines among sex workers and clients following outreach, one time presumptive treatment, and regular screening of sex workers in the Philippines. Sex Transm Infect 200682386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]