Abstract
Background and objective
Most economic evaluations of chlamydia screening do not include costs incurred by patients. The objective of this study was to estimate both the health service and private costs of patients who participated in proactive chlamydia screening, using mailed home‐collected specimens as part of the Chlamydia Screening Studies project.
Methods
Data were collected on the administrative costs of the screening study, laboratory time and motion studies and patient‐cost questionnaire surveys were conducted. The cost for each screening invitation and for each accepted offer was estimated. One‐way sensitivity analysis was conducted to explore the effects of variations in patient costs and the number of patients accepting the screening offer.
Results
The time and costs of processing urine specimens and vulvo‐vaginal swabs from women using two nucleic acid amplification tests were similar. The total cost per screening invitation was £20.37 (95% CI £18.94 to 24.83). This included the National Health Service cost per individual screening invitation £13.55 (95% CI £13.15 to 14.33) and average patient costs of £6.82 (95% CI £5.48 to 10.22). Administrative costs accounted for 50% of the overall cost.
Conclusions
The cost of proactive chlamydia screening is comparable to those of opportunistic screening. Results from this study, which is the first to collect private patient costs associated with a chlamydia screening programme, could be used to inform future policy recommendations and provide unique primary cost data for economic evaluations.
A national screening programme to detect and treat genital Chlamydia trachomatis infections opportunistically has been introduced in England,1 and this form of screening also takes place in other developed countries.2,3 Opportunistic screening involves offering a screening test to people attending healthcare settings during a consultation for another reason. In pilot studies involving young women in various healthcare settings in England,4 each screening offer was estimated to cost £16.49 and each testing episode £24.19 (costs inflated to £UK at 2005 rates).5 Most economic evaluations of chlamydia screening have been performed from the health service perspective.6 Although most of the costs associated with any healthcare programme are borne by the health service, patients frequently incur out‐of‐pocket costs, which might deter them from participating in any screening programme.
Proactive screening7 for chlamydia can be done by using existing population registers to invite people in a target age group to mail home‐collected urine and/or vulval‐swab specimens to a laboratory. The administrative costs for this approach are thought to be higher than for opportunistic screening, but have not been widely studied.8 The objectives of this study were to estimate both the health service costs, including administration of the programme, and the private costs incurred by patients who participated in population‐based chlamydia screening as part of the Chlamydia Screening Studies (ClaSS) project.9,10 This article provides a detailed cost analysis of population screening and compares these costs with those reported by other chlamydia screening programmes.
Methods
The rationale and methods for the ClaSS project have been reported in detail elsewhere.9,10 Briefly, we sent research packs to a random sample of men and women aged 16–39 years, selected from 27 general practices in the Bristol and Birmingham areas, between February 2001 and July 2002. We asked men and women to collect a urine sample (women were also asked for a vulvo‐vaginal swab) and to post this to a Health Protection Agency laboratory in Bristol or Birmingham in a prepaid envelope. Specimens were tested with at least two different tests, including one of two nucleic acid amplification tests: Cobas Amplicor CT Test (PCR, Roche Diagnostics, Basel, Switzerland) or BD ProbeTec ET (strand displacement amplification, Becton Dickinson, Franklin Lakes, New Jersey, USA) and/or an enzyme immunoassay (IDEIA PCE, Dako, Ely, Cambridgeshire, UK). Participants with positive chlamydia test results were sent appointments to receive their test results and antibiotic treatment with single‐dose azithromycin or any other appropriate antibiotic at their general practitioner surgery. Partner notification was conducted either by a practice nurse at the surgery, or at a local genitourinary clinic as part of a randomised controlled trial.11 We informed participants with negative results by post.
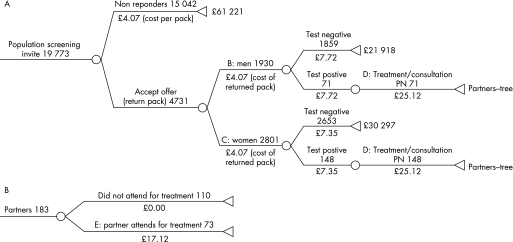
We constructed a flow diagram to describe the pathway of patients from the initial screening invitation to treatment of index cases and partners and estimated the cost of each component of the programme (fig 1).
Figure1 Index patient pathway. (A) Index patients. (B) Sexual partners. For each branch option, the number of patients who flowed through that branch is above the line and the unit cost is below. The aggregated costs of each stage are shown by the following letters: A, cost per screening invitation; B, cost per screening test in men; C, cost per screening test in women; D, cost of treatment per index case, including partner notification; and E, cost of treatment per sexual partner. PN, partner notification.
Time and motion study
We measured the time taken to complete each labour‐dependent step for the diagnostic tests. Laboratory staff collected data on a specified number of days that included times when workload was low and high, at the beginning, middle and end of the study to eliminate learning effects.
The unit cost of a test included labour, consumables, equipment and maintenance. Laboratory staff listed the consumables used in an average test procedure. We estimated costs in consultation with manufacturers, and hospital purchasing and finance departments. Hourly labour rates were based on annual salaries for 2002/3, annual leave and bank holidays were taken into account and employer's contributions to national insurance was included, superannuation and 40% overheads. We calculated the unit cost of consumable goods by dividing the total consumable costs per batch by the maximum number of specimens per batch. Annual equipment costs were estimated by the annuitisation of the initial capital outlay over the useful life of the asset to calculate the “equivalent annual cost”. The average cost of equipment per test was estimated by dividing the annual cost by the number of tests performed. We assumed optimal capacity for all equipment. Maintenance costs were estimated from maintenance contracts for each machine and added to the annual cost.
Health service costs
We estimated laboratory costs using the costs of the cheapest nucleic acid amplification test and specimen. Treatment costs included the consultation with a practice nurse and treatment with single‐dose azithromycin (using the British National Formulary cost). A general practice nurse conducted a partner notification interview on the day the patient received his or her diagnosis. A health adviser followed‐up by telephone 6 weeks later.11 We included the costs of consultation and follow‐up telephone calls along with antibiotic costs for partners, who were all treated epidemiologically. We did not include the chlamydia testing cost, as we defined this as the start of a new episode in which the partner was a new participant in screening.
We estimated the running costs of population‐based chlamydia screening by including the costs of reminders for non‐responders and non‐attenders, project management and other practice costs, including administration, overheads and training for practice nurses. Personnel costs were derived from salary costs including employer contributions directly from the study.
Patient costs
We asked all patients attending their general practice to complete a patient‐cost questionnaire, adapted from a published study.12 We did not include costs incurred by sexual partners. All participants provided information about their mode of transport, time spent travelling to and from the surgery, and out‐of‐pocket expenses such as car parking, petrol and public transport. Consultation times for participants with positive results included the time taken to receive the result, treatment, and for the practice nurse to explain the randomised controlled trial of partner notification, obtain consent, randomise and undertake partner notification herself or refer the patient to the genitourinary medicine clinic.
Costs for private car travel were calculated using published motoring costs.13 We assumed that walkers and cyclists had no travel expenses. We used www.multimap.com to estimate distances travelled between participant and surgery postcodes. The opportunity cost of time lost from work was estimated from the mean gross weekly wage rate for Great Britain in April 2003 minus tax, pension and national insurance contributions (estimated at 35% of gross salary), and at the average hourly rate for a 37.5‐h week. We assumed that employed patients <18 years, students and those looking after children had an opportunity cost approximating the minimum wage. “Other” activities foregone were classified as “leisure time” and valued at 40% of the mean average wage.12
Statistical analysis
We estimated total health service costs at each stage of screening and treatment, and used the numbers of individuals at each stage to estimate the cost (with 95% CIs) for each screening invitation and for each accepted offer. Mean travel, waiting and consultation times, and their associated costs (with 95% CI) were estimated from the cost questionnaire. Travel and surgery waiting times for patients with both positive and negative chlamydia results were virtually identical, and so we combined these to increase precision. We inflated all costs to 2005 prices using the combined hospital and community index (UK £, table 1).
Table 1 Health service costs of chlamydia screening using mailed, home‐collected specimens.
| Resources used | Cost item | Unit cost £* | Number | Total cost £ (95% CI)* |
|---|---|---|---|---|
| Screening invitation | 19773 | |||
| Invitation letter | Per letter | 0.09 | 1779.57 | |
| Postage | Per stamp | 0.21 | 4152.33 | |
| Study packs | Per pack | 3.39 | 67030.47 | |
| Result/appointment letter and postage | Per letter postage | 0.38 | 7513.74 | |
| A: Cost per screening invitation | 4.07 | 80 476.11 | ||
| Laboratory costs | ||||
| Accepted screening offer† | 4731 | |||
| B: Cost per screening test for males | Per urine specimen | 7.72 | 1930 | 14 899.60 (13 122.22 to 21 175.42) |
| C: Cost per screening tests for females | Per swab specimen | 7.35 | 2801 | 20,587.35 (17 590.16 to 28 477.33) |
| Treatment costs | ||||
| Index case | 219 | |||
| Antibiotics (azithromycin) | Per dose | 12.71 | 2783.49 | |
| Nurse consultation, including PN | Per consultation | 12.41 | 2717.79 (2405.13 to 3033.66) | |
| D: Treatment of index case, including PN | 25.12 | 5501.28 (5188.30 to 5816.83) | ||
| Sexual partners | 183 | |||
| Antibiotics (azithromycin) | Per dose | 12.71 | 2325.93 | |
| Consultation‡ | Per consultation | 4.41 | 807.03 | |
| E: Treatment of partners | 17.12 | 3132.96 | ||
| Total cost of screening episode (A+B+C+D+E) | 124 597.30 (121 243.45 to 134 827.95) | |||
| Screening programme costs | ||||
| Reminder letters | Per letter | 0.09 | 11462 | 1031.58 |
| Postage | Per stamp | 0.21 | 11462 | 2407.02 |
| Reminder packs | Per pack | 3.39 | 809 | 2742.51 |
| Phone calls§ | Per call | 1.55 | 124 | 192.20 |
| Visits¶ | Per visit | 31.77 | 17 | 540.09 |
| General practice costs** | 16 127.50 | |||
| Project manager†† | 120 299.72 | |||
| F: Study expenditure cost | 143 340.62 |
PN, partner notification.
*Costs were inflated to UK£ at 2005 rates.
†Cost of returning pack (£0.63) is included here.
‡Personal social services research unit cost of health adviser consultation at a genitourinary clinic (personal social services research unit 2004).
§Cost of telephone calls to people with positive chlamydia tests who defaulted from appointment to receive results (unit cost based on data from Bristol site only).
¶Cost of follow‐up visits to people with positive chlamydia tests who did not respond to appointments or phone calls (unit cost based on data from Bristol site only).
**Includes training of practice nurses and payments made to general practices to cover administration, running costs and overheads.
††Labour costs associated with the screening invitation are included in the study expenditure costs under the project manager.
Sensitivity analyses were conducted to explore the effects of applying the average wage rate to all participants; the minimum wage rate to all participants; the average wage to leisure time; and the current job seekers allowance rate to all those not in employment. We also examined the effect of increasing the uptake rate because this had a major influence on the cost of opportunistic chlamydia screening.5
Results
Health service costs
Figure 1 shows the numbers of participants and aggregated costs at each stage of the screening process. Table 1 shows the detailed costs of each stage of screening. Laboratory time and motion forms were completed on 7 separate days for BD probe Tec strand displacement amplification, on 8 days for Cobas PCR and on 11 days for PCE enzyme immunoassay. Information relating to general activities was collected on 11 different occasions across the two laboratories. The observations covered 208 specimens (129 urines and 79 swabs). For the nucleic‐acid amplification tests, the processing times for vulvo‐vaginal swabs and urine specimens and for the two tests were similar. We used the costs of the Cobas PCR for urine specimens in men (£7.72) and vulvo‐vaginal swabs for women (£7.35) in our calculations.
The average costs for the health service, including the cost of running the study, were £13.55 (95% CI £13.15 to 14.33) per individual screening invitation and £20.65 (95% CI £19.87 to 23.69) per person screened (table 2). If the uptake of home‐based screening had been 64%,5 the average cost per screening offer would have been £18.54 (95%CI £17.38 to 18.96).
Table 2 Average costs of screening invitation and offer.
| Number of individuals | Average cost, £ (95% CI)* | |
|---|---|---|
| NHS cost per individual screening invitation† | 19 773 | 13.55 (13.15 to 14.33) |
| NHS cost per accepted screening offer‡ | 4731 | 20.65 (19.87 to 23.69) |
| Patient cost§ | 411 | 6.82 (5.48 to 10.22) |
| Total cost per screening invitation | 19 773 | 20.37 (18.94 to 24.83) |
| Total cost per accepted screening offer | 4731 | 27.47 (23.24 to 29.55) |
NHS, National Health Service.
*Costs inflated to UK£ 2005.
†Includes, from table 1, A+B+C+D+E+F÷19 773 patients invited.
‡Includes, from table 1, ((A÷19773)*4731+B+C+D+E+(F÷19773)*4731)÷4731.
§411 from 479 people invited completed patient cost questionnaires.
Patient costs
We received responses from 411 of 479 people invited (147 chlamydia‐positive, 264 negative, response rate 86%; table 3). Most participants travelled to the general practice by car or on foot. We estimated the average cost of a return car journey at £1.49 (95%CI £1.46 to 1.57) per patient, and of public transport at £1.06 (95%CI £0.77 to 1.40) per patient. The overall average out‐of‐pocket expense per patient for all modes of transport was £0.26 (95%CI £0.16 to 0.72).
Table 3 Baseline and sensitivity analysis for patient time and travel costs.
| Activity | Base case | Average wage rate applied*† to all, £ (95% CI) | Average wage rate* ‡ applied to leisure time, £ (95% CI) | Minimum wage rate* § applied to all, £ (95% CI) | Benefit rate* ¶ applied to all those not in employment, £ (95% CI) | |
|---|---|---|---|---|---|---|
| Minutes (95% CI) | £ (95% CI)* | |||||
| Travel time | 27.98 (26.40 to 29.55 | 2.45 (2.16 to 2.73) | 3.97 (3.74 to 4.19) | 3.08 (2.77 to 3.39) | 2.09 (0.56 to 4.03) | 1.80 (1.61 to 2.08) |
| Surgery waiting time** | 10.47 (9.27 to 11.68) | 0.90 (0.23 to 2.03) | 1.49 (0.21 to 3.20) | 1.16 (1.02 to 1.31) | 0.78 (0.12 to 1.68) | 0.62 (0.36 to 1.61) |
| Surgery consultation time | 36.74 (35.67 to 42.20) | 3.21 (2.88 to 3.56) | 5.23 (4.89 to 5.57) | 4.25 (3.90 to 4.62) | 2.73 (2.54 to 2.91) | 2.48 (2.11 to 2.87) |
| Out‐of‐pocket expenses | 0.26 (0.16 to 0.72) | 0.26 (0.16 to 0.72) | 0.26 (0.16 to 0.72) | 0.26 (0.16 to 0.72) | 0.26 (0.16 to 0.72) | |
| Total lost income†† | 6.56 (5.76 to 7.77) | 10.69 (8.57 to13.93) | 8.49 (8.01 to 9.00) | 5.60 (3.92 to 7.75) | 4.90 (4.63 to 6.36) | |
| Total patient cost‡‡ | 6.82 (5.48 to10.22) | 10.95 (8.34 to13.92) | 8.75 (8.26 to 10.77) | 5.86 (4.19 to 8.77) | 5.16 (4.63 to 7.40) | |
*Costs inflated to £UK 2005.
†Average wage rate £8.26.
‡Weekly job seeker's allowance rate 2003 (37 h/week).
§Minimum wage for ⩾22 years £4.50, ⩽22 years, £3.80.
¶Average lost income+out of pocket expenses.
**Estimated from participants who completed the patient cost questionnaire. Consultation time differs slightly from times estimated by practice nurse (41.9 min, 95% CI 37.0 to 46.7).
††Average cost = (travel, waiting and consultation time)×(wage rate for each patient)/total number of patients.
‡‡Including out‐of‐pocket expenses (£0.26 per person).
The average waiting time was 10.47 min (95% CI 9.27 to 11.68; table 3). Consultation times were similar for people who participated in or declined participation in the partner notification trial: the average consultation for both groups combined lasted for 36.74 (95% CI 35.67 to 42.20) min. We estimated that each individual spent 75.2 (95% CI 71.3 to 82.5) min on receiving results in the screening programme.
If patients had not been attending the general practice, 59% (n = 242) would have been in paid employment, 20% (n = 81) would have been studying and 10% (n = 42) would have been looking after children, the remaining 11% did not record any activities. Of 242 patients in paid employment, 234 reported their arrangements for taking time off work. The largest groups came outside work time (33%, n = 80) or availed paid leave (21%, n = 51). When considering out‐of‐pocket travel expenses and opportunity costs, the average estimated cost was £6.82 (95% CI £5.48 to 10.22) per patient (table 3). In sensitivity analysis, this cost varied from £5.16 (95% CI £4.63 to 7.40), when the current UK job seekers' allowance rate was applied to patients who were not in employment, to £10.95 (95% CI £8.34 to 13.92), when the average wage rate was applied to all participants (table 3).
Discussion
We estimated the average cost to the health service of a single round of proactive screening for chlamydia using home‐collected and mailed specimens to be £13.55 (95% CI £13.15 to 14.33) per individual screening invitation, and that for each person screened £20.65 (95%CI £19.87 to 23.69). Out‐of‐pocket patient expenses averaged £6.82. This is the first study to report the wider societal costs to individuals participating in chlamydia screening.
Methodological issues
The advantages of this study were that we collected cost data prospectively as part of a large screening study, which included both men and women, and included the costs of participation to patients. Whereas we included societal costs relating to private costs incurred by patients, we were unable to collect similar cost information for partners seeking treatment. In the absence of such data, we could assume that partners would incur similar costs to those of index patients. In addition, we collected data about the exact duration of consultations. This was considerably longer than that estimated in previous studies.5 One limitation was that we could not disaggregate some of the costs of the research process from those of the intervention. For example, the consultation with the practice nurse included time taken to explain a randomised controlled trial and alternative interventions, and conduct randomisation in those giving consent, so estimated costs are somewhat higher than would be in a real screening programme.
This article provides important information about the costs associated with population screening. However, it does not capture information relating to the potential costs averted by a screening programme—for example, those associated with long‐term complications such as pelvic inflammatory disease, ectopic pregnancy and infertility. The ClaSS project includes a full economic evaluation to examine the cost‐effectiveness of home‐based population screening and is presented elsewhere.15
Comparison with opportunistic chlamydia screening
Our estimate of the health services cost of proactive chlamydia screening was comparable to that estimated for opportunistic screening in England. Adams et al5 estimated the costs of the National Chlamydia Screening Programme in England using data from pilot studies in Portsmouth and the Wirral. They found that offering chlamydia screening to women in healthcare settings cost £16.49 per screening offer (at 2005 prices), if 64% accepted the screening offer. In our study, the cost was £13.55 per screening offer for an uptake of 34%, and £18.54 if the uptake was 64%. The costs of screening invitations, laboratory testing, giving results, providing treatment and administration in this study were also comparable with those estimated from a previous population‐based study in Amsterdam.8
In an opportunistic screening programme, the screening test is offered only to eligible patients who are already having a consultation, so administrative costs are presumed to be limited. Nevertheless, the opportunistic pilot screening programme required some infrastructure and incurred over £75 000 of administrative and running costs, which accounted for around 39% (£7.30) of the average cost per test offered.5 In our study, the running costs accounted for around 50% (£7.25) of the average NHS cost per screening invitation. The estimated costs of the pilot opportunistic chlamydia screening studies did not include societal costs. Our estimated patient costs could be generalised to opportunisitic screening if there is partner notification in the setting where the results and treatment are given. However, referral of index cases to a genitourinary clinic would increase patient costs because of the additional journey and time off work.
Comparison with other patient‐cost studies
The patient costs reported in this study were similar to those reported by other studies of screening in general practice, but lower than those of screening in hospital settings (table 4). This might be partly due to the greater distances travelled to hospitals compared with those to local surgeries. The costs of screening in this study were similar to those of screening for abdominal aortic aneurysm.16 The low private costs of hospital and general practice screening might be because most men were retired. Productivity losses might also be higher where the condition screened for affects older adults in full‐time employment (eg, colon or breast cancer),17 as opposed to chlamydia, which is most common in young adults with lower incomes. The results of this study suggest that the private costs to individuals who participate in chlamydia screening using home‐collected specimens, in which positive cases are managed at general practices, are likely to be lower than those imposed by more centralised screening programmes. There was no evidence to suggest that the reduction in patient costs occurred at the expense of cost shifting to the NHS. The costs imposed on patients should be included in future economic evaluations of chlamydia screening.
Table 4 Studies reporting the private patient costs associated with screening programmes in the UK.
| Author | Year of publication | Type of screening | Setting | Cost, mean £* |
|---|---|---|---|---|
| This study | Chlamydia | General practice | 6.82 | |
| Henderson et al12 | 2002 | Fetal anomalies | Hospital | 10.61 min |
| 18.87 max | ||||
| Frew et al14 | 1999 | Colorectal cancer | Clinic | 20.62 |
| Bryan et al16 | 1995 | Aortic aneurysm | Clinic | 7.28 |
| General practice | 5.61 | |||
| Hospital | 9.15 | |||
| Sculpher and Buxton17 | 1993 | Breast cancer, diabetic retinopathy | Hospital | 9.00 min |
| 13.19 max | ||||
| General practice | 6.79 min | |||
| 13.20 min |
*All cost data inflated to £UK 2005 prices.
Implications for policy and research
Detailing the costs of different components of a screening programme is required for the rational development of screening programmes. Opportunistic screening is assumed to be a cheap option, because chlamydia testing is a small part of the cost of a consultation that would have taken place anyway. To deliver the population‐level benefits expected from screening, however, requires an effectively organised programme. This includes the costs of national coordination, quality assurance, monitoring communication and dissemination.18 The infrastructure required by the English National Chlamydia Screening Programme,19 and implemented in the pilot studies, contributed substantially to the costs of opportunistic screening. Rescreening in both opportunistic and active programmes will also need to be compared in the future. For proactive screening, the costs of the population register have already been incurred, but systematic recall in an opportunistic programme would involve additional administrative costs. Our study shows that, contrary to popular assumptions, the cost of proactive chlamydia screening is comparable to those of opportunistic screening.
Key messages
Most economic evaluations of chlamydia screening are conducted from the perspective of the health service.
In this study, we collected primary data on the labour costs associated with nucleic acid amplification testing for chlamydia and the out‐of‐pocket costs for individuals participating in a chlamydia screening programme.
The time and costs of processing vulvo‐vaginal swab and urine specimens in women were similar.
The average healthcare costs associated with a single round of active chlamydia screening using home‐collected specimens compared closely with a those of opportunistic screening.
Acknowledgements
ClaSS is funded through the NHS Research and Development HTA programme (project no. 97/32/31). Participating individuals and institutions can be viewed at www.chlamydia.ac.uk. NL was supported by an NHS career scientist award until 31 March 2005. JM is supported by a NHS career Scientist Award from the Department of Health. The views expressed here are those of the authors and not necessarily of the Department of Health.
Contributors
SMR was the principal economic researcher for the project and, with TER, was responsible for collecting data, conducting the analysis and interpreting the results. SMR prepared the manuscript as the lead writer. AMcC helped in the collection of data, ES helped with statistical analysis and PB was involved in the data analysis. TER was Chair of the ClaSS Economics Working Group and designed the economic evaluation for the study. NL was acting principal investigator and a member of the Economics Working Group and helped to revise the manuscript. JM was responsible for coordinating the project in Birmingham. SB was an advisor to the ClaSS study. ME was principal investigator. TER, NL, JM and ME are members of the team of coapplicants that designed the ClaSS study. All authors read and approved the manuscript and provided comments on the final paper.
Abbreviations
ClaSS - Chlamydia Screening Studies
NHS - National Health Service
Footnotes
Competing interests: None.
References
- 1.La Montagne D S, Fenton K A, Randall S.et al Establishing the National Chlamydia Screening Programme in England: results from the first full year of screening. Sex Transm Infect 200480335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kamwendo F, Forslin L, Bodin L.et al Programmes to reduce pelvic inflammatory disease—the Swedish experience. Lancet 1998351(Suppl 3)25–28. [DOI] [PubMed] [Google Scholar]
- 3.Low N. Current status of chlamydia screening in Europe. Eurosurveillance 200455 [Google Scholar]
- 4.Pimenta J M, Catchpole M, Rogers P A.et al Opportunistic screening for genital chlamydial infection. II: prevalence among healthcare attenders, outcome, and evaluation of positive cases, Sex Transm Inf 20037922–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adams E J, La Montagne D S, Johnston A R. Modelling the heathcare costs of an opportunistic Chlamydia screening programme. Sex Transm Infect 200480362–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Honey E, Augood C, Templeton A.et al Cost effectiveness of screening for Chlamydia trachomatis: a review of published studies. Sex Transm Infect 200278406–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray J A.Screening. Evidence‐based healthcare. How to make health policy and managment Decisions London: Churchill Livingstone, 199746–53.
- 8.Van Valkengoed I G M, Postma M J, Van den Brule A J C.et al Cost effectiveness analysis of a population based screening programme for asymptomatic Chlamydia trachomatis infections in women by means of home obtained urine specimens. Sex Transm Infect 200177276–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Low N, McCarthy A, MacLeod J.et al The chlamydia screening studies: rationale and design. Sex Transm Dis 200480342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacLeod J, Salisbury C, Low N.et al Coverage and uptake of systematic screening for genital Chlamydia trachomatis and prevalence of infection in the United Kingdom general population: cross‐sectional study. BMJ 2005330940–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Low N, McCarthy A, Roberts T E.et al Partner notification for chlamydia in primary care: randomised controlled trial and analysis of resource use. BMJ 200633214–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henderson J, Bricker L, Roberts T.et al British National Health Service's and women's costs of antenatal ultrasound screening and follow‐up tests. Ultrasound Obstet Gynecol 200220154–162. [DOI] [PubMed] [Google Scholar]
- 13.Automobile Association Motoring costs. 2005. http://www.theaa.com
- 14.Frew E, Wolstenholme J L, Arkin W.et al Estimating time and travel costs incurred in clinic based screening: flexible sigmoidoscopy screening for colorectal screening. J Med Screen 19996119–123. [DOI] [PubMed] [Google Scholar]
- 15.Low N, McCarthy A, Macleod J, Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection: the Chlamydia Screening Studies Project et alHealth Technol Assess. 2007;11. In press [DOI] [PubMed]
- 16.Bryan S, Buxton M, McKenna M.et al Private costs associated with abdominal aortic aneurysm screening: the importance of private travel and time costs. J Med Screen 1995262–66. [DOI] [PubMed] [Google Scholar]
- 17.Sculpher M, Buxton M.The private costs incurred when patients visit screening clinics: the cases of screening for breast cancer and for diabetic retinopathy. Uxbridge: Health Economics Research Group, Brunel University, 1993
- 18.Department of Health The National Screening Committee criteria. London: The Stationery Office, 1998
- 19.Department of Health Chlamydia screening programme roll out. Core requirements. London: Department of Health, 2003