Abstract
Background
We hypothesized that inhalational anesthetics induced cell damage by causing abnormal calcium release from the endoplasmic reticulum via excessive activation of inositol 1,4,5-trisphosphate (IP3) receptors, with isoflurane greater potency than sevoflurane or desflurane.
Methods
We treated DT40 chicken B lymphocytes with total IP3 receptor knock-out or their corresponding wild type control cells with equipotent exposure of isoflurane, sevoflurane and desflurane. We then determined the degree of cell damage by counting the percentage of annexin V or propidium iodide positively stained cells or measuring caspase-3 activity. We also studied the changes of calcium concentrations in the endoplasmic reticulum, cytosol and mitochondria evoked by equipotent concentrations of isoflurane, sevoflurane and desflurane in both types of DT40 cells.
Results
Prolonged use of 2 minimal alveolar concentration sevoflurane or desflurane (24 hr) induced significant cell damage only in DT40 Wild type but not IP3 receptor total knock-out cells, but with significantly less potency than isoflurane. In accordance, all three inhalational anesthetics induced significant decrease of calcium concentrations in the endoplasmic reticulum, accompanied with a subsequent significant increase in the cytosol and mitochondrial calcium concentrations only in DT40 wild type but not in IP3 receptor total knock-out cells. Isoflurane treatment showed significantly greater potency of effect than sevoflurane or desflurane.
Conclusion
Inhalational anesthetics may induce cell damage by causing abnormal calcium release from the endoplasmic reticulum via excessive activation of IP3 receptors. Isoflurane has greater potency than sevoflurane or desflurane to cause calcium release from the endoplasmic reticulum and to induce cell damage.
Introduction
It is important for a surgical patient to be immunocompetent to prevent perioperative infection and related complications. Various instances of immune system dysfunction has been reported after surgery 1,2, which was associated with lymphocytopenia 3. Recent studies suggest that inhalational anesthetics commonly used for various kinds of surgery may affect the immune system by causing peripheral lymphocytopenia 4,5. Inhalational anesthetics induced cell damage by apoptosis in lymphocytes in a dose-and time-dependent manner, which may be mediated by mitochondria 4,5. Inhalational anesthetics may also cause DNA damage in human peripheral blood lymphocytes 6. However, the exact mechanisms for inhalational anesthetic mediated cell damage are still unclear.
Our recent study suggested that the commonly used inhalational anesthetic isoflurane may induce cell apoptosis by disruption of intracellular calcium homeostasis 7–9. The inositol 1,4,5-trisphosphate (IP3) and ryanodine receptors, two calcium channels located on the endoplasmic reticular (ER) membrane, play important physiological roles in normal cells including lymphocytes 10,11. However, abnormal calcium release from the ER via excessive activation of either IP3 or ryanodine receptors on the ER membrane may result in abnormal elevation of cytosolic calcium concentrations ([Ca2+]c), calcium overload in mitochondria and depletion of ER calcium, all of which can contribute to cell death 12,13. In addition, cytochrome C released from mitochondria due to calcium overload can remove the negative feedback inhibition of IP3 receptors (IP3R) by cytosolic calcium, leading to a vicious cycle of excessive calcium release from the ER via IP3R 13,14. Cytochrome C release also activates caspase-3, which in turn cleaves IP3R, resulting in a permanent leak of calcium from the ER 15,16. Furthermore, ryanodine and IP3 receptors are both calcium activated calcium release channels. Calcium release from the ER via activation of ryanodine receptors can activate IP3R and vice versa 17. Consistent with this theory, our previous studies have demonstrated that lymphocytes deficient of IP3R were resistant to isoflurane-induced cell apoptosis, as well as the elevation of calcium concentrations in cytosol and mitochondria, but thapsigargin which can release calcium from the ER independent of IP3 receptors still induced apoptosis in the lymphocytes even with total knock-out of IP3 receptors 8. This suggests an important role of IP3R activation on isoflurane-mediated cell damage. In addition, inhibition of excessive calcium release from the ER through either IP3R or ryanodine calcium channel receptors by dantrolene or xestospongin c significantly inhibited isoflurane induced cell damage 7,8.
The three commonly used inhalational anesthetics seem to have quite different potencies to cause apoptosis in different kinds of cells with an unclear mechanism. Isoflurane was significantly more toxic than sevoflurane or desflurane in different lymphocytes 4,5. We also have demonstrated that only isoflurane, but not sevoflurane nor desflurane at equipotent exposures, induce cell damage in different kinds of neurons 7,9. This unexpected phenomenon may provide an important basis for anesthesiologists to use inhalational anesthetics differently in their practice, especially for those patients vulnerable to anesthesia mediated cell damage. We have hypothesized that inhalational anesthetics have different potencies to induce calcium release from the ER via activation of IP3R and therefore have different toxic potencies. To confirm this hypothesis, we comparatively studied the effect of three commonly used inhalational anesthetics (isoflurane, sevoflurane and desflurane) on cell apoptosis, calcium concentrations in the ER, cytosol and mitochondria in the chicken B lymphocytes with total knock-out of IP3R (DT40 IP3R TKO) or its corresponding wild type (WT) control.
Materials and Methods
Cell Cultures
DT40 WT and its IP3R TKO cells were cultured in RPMI 1640 with 10% Fetal calf serum, 1% chicken serum, 50 μM 2-mercaptoethanol, 4 mM l-glutamine and antibiotics in a 95% air, 5% carbon dioxide humidified atmosphere at 38°C as we previously described 8,18.
Anesthetic exposure
DT40 cells (WT and IP3R TKO) were exposed to the equivalent of 2 MAC of isoflurane (2.4%), sevoflurane (4%) and desflurane (12%) for 24 hr in a gas-tight chamber inside the culture incubator (Bellco Glass, Inc., Vineland, NJ), with humidified 5%CO2/21%O2/balanced N2 (AirGas East, Bellmawr, NJ) going through a calibrated agent-specific vaporizer as we have previously described 7–9. Gas phase concentrations in the gas chamber were verified and maintained at the desired concentration throughout the experiments using an infrared Ohmeda 5330 agent monitor (Coast to Coast Medical, Fall River, MA). In a pilot study, the cell media was aspirated and extracted into hexane for high performance liquid chromatography measurement (System Gold, Beckmam Coulter, Fullerton, CA) to verify that the various anesthetic concentrations in the medium in mM are equivalent to the minimal alveolar concentration (MAC) concentrations in the gas phase inside the gas chamber using the concentration correlation previously described 19.
Imaging analysis of Annexin V and propidium iodide
Translocation of membrane phospholipid phosphatidylserine from the inner to the outer leaflet of the plasma membrane is an early indication of cell damage. Annexin V, a phospholipid binding protein with a high affinity for phospholipid phosphatidylserine, can bind to phospholipid phosphatidylserine once it is exposed to the extracellular environment. Propidium iodide (PI) can bind to nucleic acid after penetrating a breached plasma membrane, as occurs in the later stages of cell damage. We treated DT-40 cells, grown floating in the medium, with equivalent 2 MAC of isoflurane (2.4%), sevoflurane (4%) and desflurane (12%) for 24 hr. Our previous study demonstrated that the minimal exposure of 2 MAC for 24 hr of isoflurane, but not its equivalent of sevoflurane, induced cell apoptosis in the rat primary cortical neurons 7. However, it only required 1.2% isoflurane for 6 hr to induce apoptosis in DT40 WT cells 8. We hypothesized that sevoflurane or desflurane could still induce apoptosis but with much less potency than isoflurane in the vulnerable DT40 WT cells. As a result, we elected to use relatively high concentrations (2 MAC) for prolonged time (24 hr) of three inhalational anesthetics so that the possible toxic effects of sevoflurane or desflurane could be detected. Immediately after treatment, we determined Annexin V or PI positive cells by the methods we have previously described 8. Briefly, cells were dropped onto 25 mm cover slips and stained with Annexin V or PI. Annexin V, PI positive cells and normal cells were counted by two persons blinded to the treatments. The percentage of Annexin V or PI positive cells was calculated by dividing the positively stained cells by the total number of counted cells in at least four areas on each cover slip.
Detection of Caspase-3 activity
Increased caspase-3 activity is a hall marker for cell damage by apoptosis. We measured the caspas-3 activity immediately after treatment using a methods we have described previously 8,18. The assay is based on the ability of the active enzymes to cleave the fluorogenic substrates Ac-DEVD-AFC (Caspase-3, Calbiochem, San Diego, CA). DT40 cells grown on 6 well plates were treated with equipotent concentrations of isoflurane (2.4%), sevoflurane (4%) and desflurane (12%) for 24 hr and then were harvested via trypsinization and washed with phosphate buffered saline. The cell pellet was gently resuspended in CelLytic™ M lysis buffer and protease inhibitor cocktail (Sigma, St. Louis, MO), lysed, and centrifuged; the supernatant was used for the assay. Caspase substrates were added to a final concentration of 50 μM and the samples were incubated at 37°C for 45 min in caspase assay buffer. Incubated samples were measured at an excitation of 400 nm and an emission of 505 nm in a multiwavelength-excitation dual wavelength-emission fluroimeter (Delta RAM; photon Technology International, Birmingham, NJ).
Measurement of cytosolic calcium concentration ([Ca2+]c)
[Ca2+]c was measured using fura-2/AM fluorescence (Molecular probe, Eugene, OR) with a photometer coupled to an Olympus 1×70 inverted microscope (Olympus America Inc., Center Valley, PA) and the IPLab v3.7 imaging processing and analysis software (Biovision Technologies, Exton, PA). The protocol to determine [Ca2+]c was same as that we previously described 8,9. Briefly, cells attached to Cell-Tak (BD Biosciences, Bedford, MA) coated glass coverslips were washed 3 times with Krebs-Ringer buffer without addition of calcium and then loaded with 2.5 μM fura-2/AM (Molecular Probes, Eugene, OR) for 30 min at room temperature. The cells were then placed in a sealed chamber (Warner Instrument Inc., Hamden, CT) connected with multiple inflow infusion tubes and one outflow tube, which provided constant flow to the chamber. All bubbles in the chamber were flushed out at the beginning so that there was no gas phase in the sealed chamber during measurement of calcium concentration in the buffer. The cells were first washed with Krebs-Ringer buffer through one inflow tube for the baseline measurement of [Ca2+]c, and then were exposed to approximately equivalent to 2 MAC of isoflurane (0.64 mM), sevoflurane (0.96 mM) and desflurane (1.2 mM) 19 via a separate inflow infusion tubes driven by a syringe pump (Braintree Scientific Inc., Braintree, MA). The anesthetic concentrations in the buffer were determined with high performance liquid chromatography (System Gold, Beckmam Coulter, Fullerton, CA) as we described previously 9,20. The fluorescence signals were measured with excitation at 340 and 380 alternatively and emission at 510 nM for a period up to 15 min for each treatment. The ratios of F340/F380 reflected the cytosolic calcium concentrations and were used for comparison among three inhalational anesthetics. The final result of F340/F380 was averaged from the cells of at least three separate experiments. A pilot study confirmed that the cells were still viable at the end of experiments for calcium measurement.
Measurement of ER calcium concentration ([Ca2+]e)
We measured the calcium concentrations inside the ER using dye mag-fura 2/AM (Molecular Probes) and a previously described protocol 21. Briefly, DT40 cells were incubated with 5μM mag-fura 2/AM in Modified Hanks’ balanced salt solution buffered with Hepes (HBSS-H: 137 mM NaCl, 5.4 mM KCl, 1.3 mM CaCl2, 0.41 mM MgSO4, 0.49 mM MgCl2, 0.34 mM Na2HPO4, 0.44 mM NaH2PO4, 5.5 mM glucose and 20 mM Hepes/NaOH (pH 7.4)) containing 1% bovine serum albumin for 45 min at 37°C in a dark room. The mag-fura 2/AM-loaded cells were then washed with bovine serum albumin-free HBSS-H and attached to Cell-Tak coated glass coverslips placed at the bottom of the recording chambers. The cells were then exposed to Intracellular-like medium containing 125mM KCl, 19mM NaCl, 10mM Hepes (pH7.3 with KOH), 330μM CaCl2 and 100μg/ml (w/v) saponin (Sigma) for 1–2 min to permeabilize the cells. Thereafter, the permeabilized cells were washed with intracellular-like medium and then incubated in Intracellular-like medium containing 3 mM ATP and 1.4 mM MgCl2 for at least 5 min. The coverslips were then placed in a sealed chamber (Warner Instrument Inc., Hamden, CT) connected with multiple inflow infusion tubes and one outflow tube, which provided constant flow to the chamber. The cells were washed with running buffer through one inflow tube for the baseline measurement of [Ca2+]e, at first and then were exposed to equivalent concentrations of isoflurane (0.64 mM), sevoflurane (0.96 mM) or desflurane (1.2 mM) via a separate inflow infusion tube driven by a syringe pump (Braintree Scientific Inc., Braintree, MA). The fluorescence signals were measured with excitation at 340 and 380 alternatively and emission at 510 nM for a period up to 6 min for each treatment. The ratios of F340/F380 reflected the ER calcium concentrations relatively and were used for comparison among three inhalational anesthetics. The final results of F340/F380 were averaged from the cells of at least three separate experiments and compared among three inhalational anesthetics. All these experiments were performed at room temperature.
Confocal imaging of mitochondrial Ca2+
The method used was the same as we described previously 8,18. DT40 cells (WT and IP3R TKO) were loaded with 2 μM rhod-2/AM in cell medium containing 2.0% bovine serum albumin in the presence of 0.003% pluronic acid at 37°C for 50 min, then attached to Cell-Tak coated glass coverslips. The cells were washed and placed on a stage and exposed to equivalent concentrations of isoflurane (0.64 mM), sevoflurane (0.96 mM) or desflurane (1.2 mM) dissolved in the perfusion buffer. The images were recorded using the Radiance 200 imaging system (Bio-Rad Laboratories, Hercules, CA) with excitation at 568 nm. The relative changes of fluorescence signals were determined and compared among three inhalational anesthetics.
Statistics
We used GraphPad Prism 4 software (GraphPad Software, Inc., San Diego, CA) for all statistical analysis. Annexin V and propidium iodide staining were all expressed as percentage of total cells examined. Changes of calcium concentrations in [Ca2+]e, [Ca2+]c and [Ca2+]m were expressed as a percentage of their own baseline. All data were expressed as mean±SD. We analyzed all the data with one-way analysis of variance followed by Tukey’s multiple comparison tests, P<0.05 was considered statistically significant.
Results
Isoflurane induced significantly greater cell damage than sevoflurane or desflurane only in DT40 WT cells
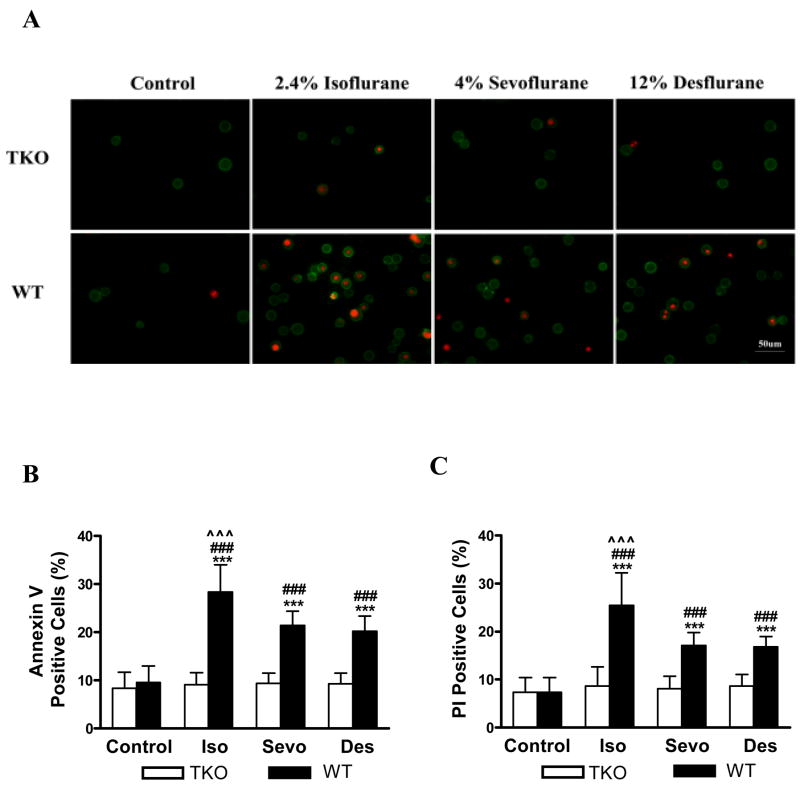
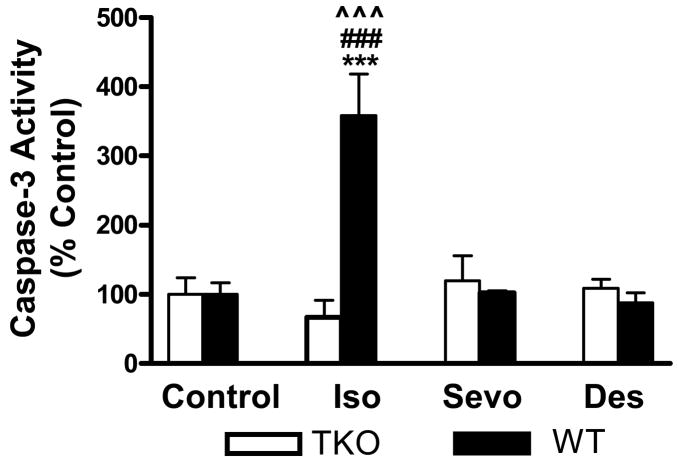
We have previously demonstrated that isoflurane induced apoptosis only in DT40 WT but not IP3R TKO in a dose and time dependent manner 8. Since sevoflurane and desflurane, at equipotent exposure to isoflurane, seemed not to induce cell damage in neuronal cultures in our previous studies 7,9, we investigated whether the three inhalational anesthetics also have different potencies to induce apoptosis. All three inhalational anesthetics induced significant cell damage determined by both Annexin V and PI staining only in DT40 WT but not IP3R TKO (fig. 1A). Isoflurane significantly increased percentage of Annexin V and PI positive cells from 9.1%±2.4 and 8.7%±3.9 in controls to 28.4%±5.6 and 25.4%±6.7 respectively after treatments only in DT40 WT cells (fig. 1B and C, P<0.001, N=29 for all controls, N=28 for all treatments). Compared to control, sevoflurane and desflurane also significantly increased percentage of Annexin V positive cell from 9.4%±2.2 and 9.2%±2.3 in controls to 21.4%±2.9 and 20.2%±3.1 respectively after treatment only in DT40 WT cells (fig. 1B, P<0.001 for all, N=29 for all controls, N=28 for all treatments). Similarly, sevoflurane and desflurane significantly increased percentage of PI positive cells from 8.1%±2.6 and 8.6%±2.4 in controls to 17%±2.7 and 16.9%±2.1 respectively after treatments (fig. 1C, P<0.001 for all, N=29 for all controls, N=28 for all treatments) only in WT DT40 cells. Consistent with our previous finding 7,9, isoflurane, at equipotent exposure to sevoflurane and desflurane, induced significantly greater cell damage than either sevoflurane or desflurane in WT DT40 cells (fig. 1 B and C, P<0.001 for both Annexin V and PI). We also compared the potency of three commonly used inhalational anesthetics on induction of apoptosis in chicken B lymphocytes by measuring the caspase-3 activity which is one of the hall markers for cell death by apoptosis. Isoflurane dramatically increased caspase-3 activity as a percentage of control to 358%±60 (fig. 2, P<0.001, N=8 for control, N=9 for isoflurane treatment) only in WT DT40 cells, while sevoflurane and desflurane did not increase caspase-3 activity significantly (102%±2.6 and 87%±14 respectively as a percentage of control, fig. 2, P>0.05, N=4 for both controls and treatments). Isoflurane at equipotent concentrations caused a markedly greater caspase–3 activity in comparison to sevoflurane and desflurane (fig. 2, P<0.001) only in DT40 WT cells. All three inhalational anesthetics did not induce significant increases of caspase-3 activity in DT40 IP3R TKO cells.
Figure 1.
Isoflurane induced significantly greater cell damage than sevoflurane or desflurane only in DT40 wild type cells. The early stage of cell damage by apoptosis was determined by the externalization of anionic phospholipid, phosphatidyl serine-annexin V binding (annexin V). The late stage of cell damage was determined by propidium iodide (PI) staining, representing loss of plasma membrane integrity. All three inhalational anesthetics induced significantly increase of Annexin V positive (green circle) and PI positive (red dot) cells. (A). Scale bar=50 μM. Isoflurane (Iso) also induced significantly more early (Annexin V, 1B) and late cell damage (PI, 1C) than either sevoflurane (Sevo) or desflurane (Des). B and C. Data represents mean±SD from at least three separate experiments.*** and ### means P<0.001 compared to DT40 IP3 receptor total knock-out (TKO) cells or the DT40 wild type (WT) cells controls respectively. means P<0.001 compared to DT40 WT cells treated with either Sevo or Des (B and C).
Figure 2.
Isoflurane but not sevoflurane or desflurane significantly elevated caspase-3 activity only in wild type DT40 cells. Data represents mean±SD from minimum 4 repeats. *** and ### means P<0.001 compared to DT40 IP3 receptor total knock-out (TKO) cells or the DT40 wild type (WT) cell controls respectively.^ ^ ^ means P<0.001 compared to DT40 WT cells treated with either Sevo or Des.
Isoflurane induced a significantly greater decrease of ER calcium than sevoflurane or desflurane only in DT40 WT cells
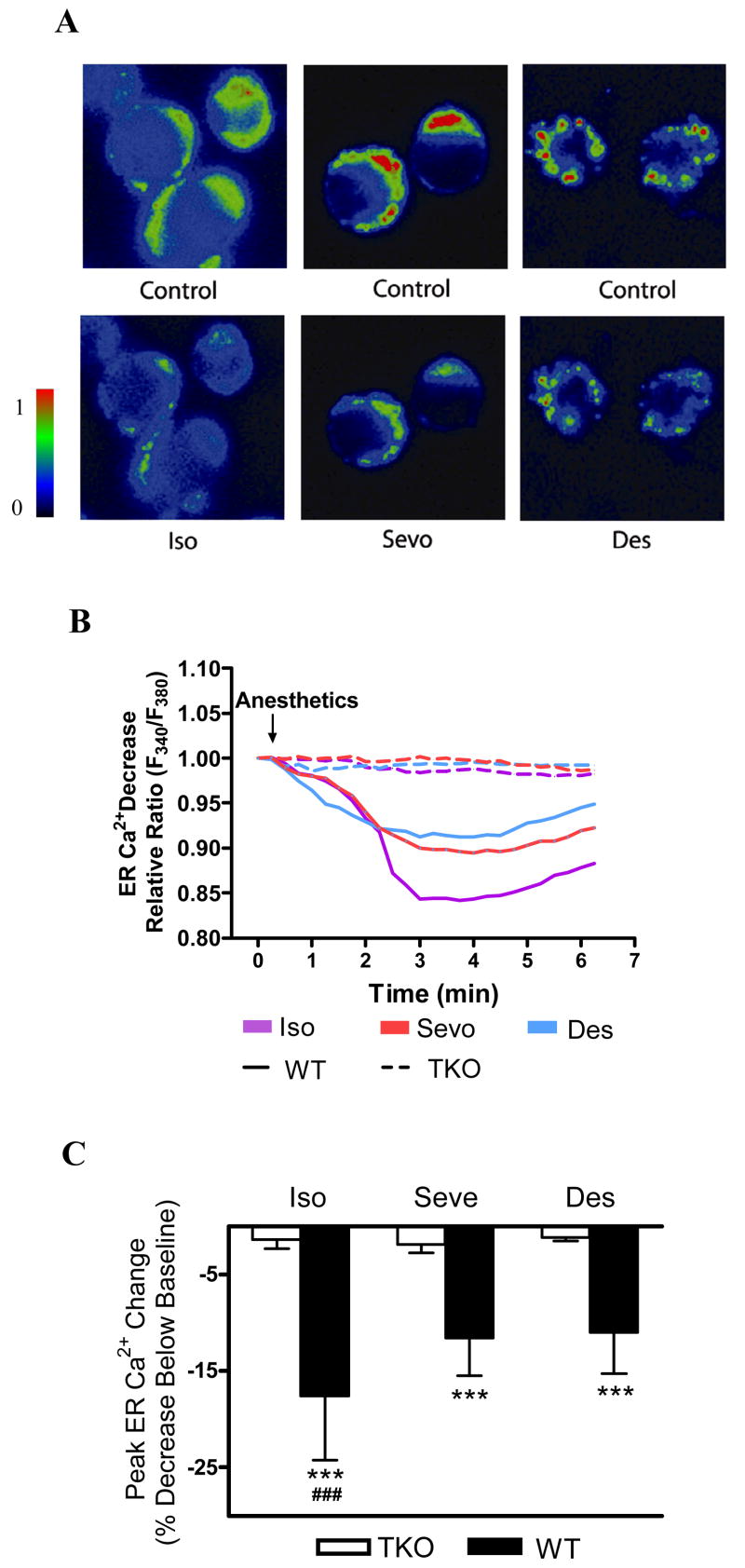
To support our hypothesis that inhalational anesthetics can induce cell damage by causing calcium release from the ER via activation of IP3R, we measured the change of ER calcium after exposure of DT40 cells to these anesthetics at equipotent concentrations. All three inhalational anesthetics significantly decreased ER calcium selectively only in DT40 WT but not IP3R TKO cells (fig. 3A), indicating calcium is released from the ER via activation of IP3R. Isoflurane, sevoflurane and desflurane significantly reduced ER calcium concentration as percentage decrease below their initial baseline maximally by 17.6%±6.6 (N=21), 11.6%±3.8 (N=18) and 11%±4.2 (N=22) respectively (fig. 3B and C, P<0.001 for all) in DT40 WT cells. However, isoflurane, sevoflurane and desflurane only reduced ER calcium level as percentage decrease below their baseline level by 1.4%±0.9 (N=18), 1.9%±0.8 (N=21) and 1.2%±0.3 (N=35) respectively in DT40 IP3R TKO cells, significantly less than in their corresponding WT DT40 cells (fig. 3C, P<0.001 for all). These results were consistent with the greater potency of isoflurane than the sevoflurane or desflurane to induce cell damage by apoptosis (fig. 1 and 2).
Figure 3.
Isoflurane induced significantly greater decrease of the endoplasmic reticulum (ER) calcium than sevoflurane or desflurane only in DT40 wild type cells. DT40 wild type (WT) cells were permeabilized with saponin to allow the dye mag-fura 2/AM loaded into ER and then exposed to three inhalational anesthetics of isoflurane (Iso), sevoflurane (Sevo) and desflurane (Des) to induce calcium release from the ER (A). B and C. Isoflurane induced significantly more peak ER calcium decrease over its own baseline represented by the relative ratio (F340/F380) than Sevo or Des only in DT40 WT cells. Data represents mean±SD from at least three separate experiments. ***means P<0.001 compared to IP3 receptor total knock-out (TKO) DT40 cells. ### means P<0.001 compared to WT DT40 cells treated with either Sevo or Des.
Isoflurane induced a significantly greater increase of cytosolic and mitochondria calcium than sevoflurane or desflurane only in DT40 WT cells
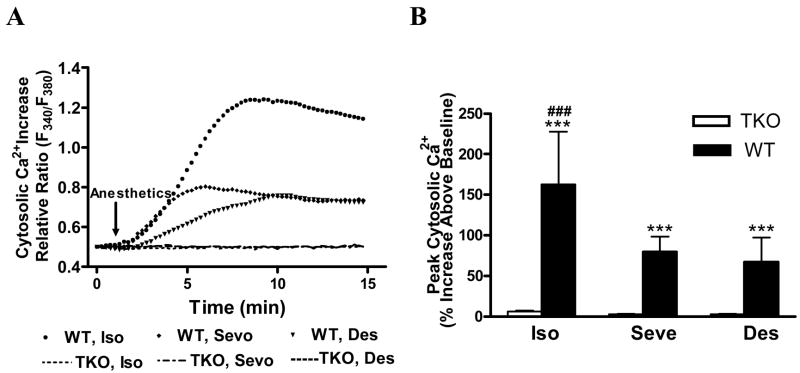
To confirm that the calcium released from the ER by inhalational anesthetic mediated activation of IP3R was transferred into mitochondria via the cytosolic space, we measured the changes of calcium concentrations in both the cytosolic space and mitochondria. Isoflurane, sevoflurane and desflurane significantly increased peak cytosolic calcium (F340/F380 ratio) as percentages above their own baseline controls to 162.7%±64 (N=39), 79.4%±19 (N=15) and 67.5%±29 (N=21) (fig. 4 A and B, P<0.001 for all) only in DT40 WT cells, which were also significantly higher than their effects in DT40 IP3R TKO cells (6.3%±3.5, N=23, 3%±1.4, N=38 and 3%±1.4, N=39 respectively, fig. 4A and B, P<0.001 for all). Similarly, all three inhalational anesthetics significantly increased mitochondrial calcium concentrations only in DT40 WT cells (fig. 5). Isoflurane, sevoflurane and desflurane significantly raised mitochondrial calcium concentrations as percentages of increase above their own baseline control to 121.1%±80 (N=26), 51.5%±22.5 (N=25) and 64.8%±34 (N=27) (fig. 5A and B, P<0.001 for all) only in DT40 WT cells, which were also significantly higher than their effects in DT40 IP3R TKO cells (2.7%±2.7, N=27, 1.4%±2.8, N=28 and 1.3%±2.3, N=28 respectively, fig. 5A and B, P<0.001 for all). These results were consistent with their effects on decreasing ER calcium (fig. 3), increasing cytosolic calcium (fig. 4) and inducing cell damage (fig. 1 and 2).
Figure 4.
Isoflurane induced significantly greater increase of cytosolic calcium than sevoflurane or desflurane only in wild type DT40 cells. Isoflurane (Iso) induced significantly more elevation of peak cytosolic calcium represented by the relative ratio (F340/F380) than sevoflurane (Sevo) or desflurane (Des) only in DT40 wild type (WT) cells (A and B). B. Data represents mean±SE from at least three separate experiments. ***means P<0.001 compared to IP3 receptor total knock-out (TKO) DT40 cells. ### means P<0.001 compared to DT40 WT cells treated with either Sevo or Des.
Figure 5.
Isoflurane induced significant greater increase of mitochondrial calcium than sevoflurane or desflurane only in wild type DT40 cells. Isoflurane (Iso) induced significantly more increase of peak mitochondrial calcium represented by the relative ratio as percentage increase above their own baselines than sevoflurane (Sevo) or desflurane (Des) only in DT40 wild type (WT) cells (A). B. Data represents mean±SD from at least three separate experiments. *** means P<0.001 compared to DT40 IP3receptor total knock-out (TKO) cells. ### means P<0.001 compared to DT40 WT cellstreated with either Sevo or Des.
Discussion
Our results suggest that inhalational anesthetics induce apoptosis in lymphocytes via excessive activation of IP3R on the ER membrane. The apoptosis induced by inhalational anesthetics was associated with a decrease of calcium concentrations in the ER, and the sequential increase of calcium concentrations in the cytosolic space and then the mitochondria. This most likely represented transfer of ER calcium into mitochondria via the cytosolic space, which is much more efficient than the calcium transfer originated from the calcium influx from the extracellular space 22. It is generally believed that calcium ions in cytosolic space are taken up by mitochondria low-affinity, high capacity calcium ions uniporter 22. The excessive cytosolic calcium originated from the ER can cause overloading of mitochondria with calcium, collapse of mitochondrial membrane potential and subsequent release of cytochrome C from mitochondria, triggering cell death by apoptosis 23. The current study provides a novel finding that all three inhalational anesthetics actually decrease ER calcium by directly measuring ER calcium concentrations. The significant decrease of ER calcium concentrations after exposing DT40 to isoflurane in wild type but not IP3R total knock out cells further supports the finding from our previous reports 8,9 that isoflurane induced calcium release from the ER via activation of IP3R. We did not test the effect of IP3 receptor antagonist xestospongin C on cell damage induced by inhalational anesthetics in the current study because xestospongin C is not behaving consistently as a selective IP3R antagonist 24 and we have previously demonstrated the inhibitory effects of xestospongin C on isoflurane-mediated cell damage in other types of cells 8. The major advantage of utilizing DT40 cell line with total knock out of IP3R is to selectively study the role of this receptor on excessive calcium release from the ER and the subsequent apoptosis mediated by inhalational anesthetics, which is a more powerful tool than the relatively less selective IP3 receptor antagonist xestospongin C. More studies are needed to investigate whether inhalational anesthetics can directly activate IP3R on the ER membrane or simply increase the production of IP3 or augment the opening probability of IP3R upon activation by their agonists.
Isoflurane seems to behave consistently throughout our studies in having greater potency to induce apoptosis and calcium release from the ER than sevoflurane or desflurane 7–9. This is especially obvious on comparison of activation of caspase-3 induced by three inhalational anesthetics, with only isoflurane but not sevoflurane or desflurane inducing remarkable elevation of caspase-3 activity, a hall maker of cell death by apoptosis in wild type DT40 cells. It is still not clear why sevoflurane and desflurane significantly increased annexin V and PI but not caspase-3 positive cells compared to their corresponding controls. Annexin V, a phospholipid binding protein with a high affinity for phospholipid phosphatidylserine, can bind to phospholipid phosphatidylserine once it is exposed to the extracellular environment during early stage of cell damage. Propidium iodide (PI) can bind to nucleic acid after penetrating a breached plasma membrane, as occurs in the later stages of cell damage. Caspase-3 activation is the hall marker of apoptosis. We speculated that Annexin V might also detect some damaged cells without apoptosis process while caspase-3 activity assay detected only apoptotic cells. It is possible that sevoflurane and desflurane might induce cell damage in somehow different mechanisms compare to isoflurane that they did not have to activate caspase-3. DT40 chicken lymphocytes with total knock-out of IP3R were resistant to the transfer of ER calcium into mitochondria via cytosolic space and apoptosis induced by all three inhalational anesthetics. Isoflurane has greater potency to induce calcium release from the ER most likely derived from its greater activation of IP3 receptors. It seems neurons are more resistant to inhalational anesthetics induced apoptosis than lymphocytes because a minimum exposure of isoflurane required to induce neuronal damage was 2 MAC for 24 hr 7,8,25. It should be noted that sevoflurane or desflurane could also induce cell damage determined by annexin V and PI staining in the vulnerable lymphocytes, but with significantly less potency than isoflurane. Our previous studies suggested that isoflurane induced apoptosis in DT40 wild type cells and primary cortical neurons in a concentration and time dependent manner 7,8. The minimal exposure for isoflurane to induce apoptosis in DT40 cells was about 1.2% for 6 hr 8. In normal human peripheral lymphocytes, only 0.85% isoflurane was needed to induce apoptosis 4. We have chosen a treatment regiment with relatively high concentrations (equivalent to 2 MAC) for a long duration (24 hr) to test the hypothesis that sevoflurane and desflurane could still induce apoptosis as isoflurane, but with much lower potencies. An intervention with low concentration and duration would be less likely to cause any detectible sevoflurane or desflurane cytotoxicity as we have demonstrated previously in other types of cells 7,25. Our results endorse the above hypothesis that sevoflurane and desflurane at equipotent exposure of 2 MAC for 24 hrs did in fact induce cell damage determined with annexin-V and PI staining in DT-40 lymphocytes, however with significantly less potency than isoflurane. In peripheral human lymphocytes, both isoflurane and sevoflurane induced apoptosis 4,5, with isoflurane greater potency than sevoflurane at same concentrations 4. Loop et al 5 also demonstrated that isoflurane and sevoflurane, but not desflurane, induced apoptosis dose-dependently in human T-lymphocytes. Further animal and clinical studies are needed to see if desflurane may be a better choice than other inhalational anesthetics in patients with peripheral lymphocytopenia.
All inhalational anesthetics evidently affect intracellular calcium homeostasis. A transient and moderate elevation of cytosolic calcium by isoflurane may provide cytoprotection through upregulation of host preconditioning responses 26,27, but prolonged exposure to higher concentrations of isoflurane, such as this study, may maintain the IP3R in an open state, in turn excessively elevating [Ca2+]c and [Ca2+]m, depleting ER calcium, and ultimately leading to cell damage 28,29. It seemed that the potency for inhalational anesthetics to induce cell apoptosis correlated with their potency to decrease ER calcium concentrations and subsequently their capacity to increase cytosolic and mitochondrial calcium. The greater likelihood of isoflurane to induce calcium release from ER than sevoflurane may also contribute to its greater ability to precondition neurons and provide neuroprotection against neurotoxicity induced by the prolonged use of isoflurane as demonstrated in our previous study 25. Future studies are needed to quantify the amount of ER calcium decrease required to convert the short exposure neuroprotective effects into neurotoxic effects by a prolonged isoflurane exposure.
This study has several limitations which should influence in vivo interpretations: 1). DT40 chicken lymphocytes are from immortal transformed cell lines. While clearly different from normal cells, in general, such cells are more resistant to stressors, making the results of our study somewhat more relevant to the in vivo situation. Although the mechanisms for this vulnerability variance among different types of cells are elusive, it seems that neurons in cell cultures are relatively less vulnerable to isoflurane-mediated neurotoxicity 7–9,25; 2). Because the DT40 cells are chicken lymphocytes, not the human lymphocytes, it is difficult to refer the finding in this study to clinical importance. Previous studies have demonstrated that inhalational anesthetics induced apoptosis in human lymphocytes with different potencies 4,5, while the current study provided mechanisms of how the inhalational anesthetics induce apoptosis in lymphocytes. 3). We have used inhalational anesthetics at relatively high concentrations for prolonged time, which is less ideal to mimic clinical scenario in patients. Further studies are needed to compare the potency of three commonly used inhalational anesthetics on intracellular calcium homeostasis and apoptosis in animals and patients in the future.
Taken together, our findings suggest that the commonly used inhalational anesthetic isoflurane may induce apoptosis in lymphocytes by significantly decreasing ER calcium and subsequently increasing cytosolic and mitochondria calcium, which was associated with an excessive activation of IP3R. Sevoflurane and desflurane have significantly less potency to induce calcium release from the ER and apoptosis in these lymphocytes.
Acknowledgments
Funding: National Institute of General Medical Science, National Institute of Health, Baltimore, Maryland, K08 grant (1-K08-GM-073224, to H.W.), March of Dimes Birth Defects Foundation Research Grant (12-FY05-62, to H.W.), White Plains, New York, and the Research Fund at the Department of Anesthesiology and Critical Care, University of Pennsylvania (to H.W.), Philadelphia, Pennsylvania.
The authors would like to thank Tomohiro Kurosaki, M.D. Ph.D., Professor, from the Institute of Physical and Chemical Research, Research Center for Allergy and immunology, Turumi-ku, Yokohama, Kanagawa, Japan for providing us with total IP3 receptor knock out chicken lymphocytes. We appreciate the technical support from Qingcheng Meng, Ph.D., Senior Research Scientist from the Department of Anesthesiology and Critical Care, University of Pennsylvania, Philadelphia, Pennsylvania. We appreciate the discussions with Roderic Eckenhoff, M.D., Professor of Anesthesia, Maryellen Eckenhoff, Ph.D., Research Associate and Randall Pittman, Ph.D., Professor of Pharmacology from the University of Pennsylvania, Philadelphia, Pennsylvania.
Footnotes
The research work was performed in and should be attributed to the Department of Anesthesiology, University of Pennsylvania, Philadelphia, Pennsylvania
Reference List
- 1.Riddle PR, Berenabu MC. Postoperative Desression of Lymphocyte Response to Phytohaemagglutinin. Lancet. 1967;1:746–8. doi: 10.1016/s0140-6736(67)91364-5. [DOI] [PubMed] [Google Scholar]
- 2.Slade MS, Simmons RL, Yunis E, Greenberg LJ. Immunodepression After Major Surgery in Normal-Patients. Surgery. 1975;78:363–72. [PubMed] [Google Scholar]
- 3.Oka M, Hirazawa K, Yamamoto K, Iizuka N, Hazama S, Suzuki T, Kobayashi N. Induction of Fas-mediated apoptosis on circulating lymphocytes by surgical stress. Ann Surg. 1996;223:434–40. doi: 10.1097/00000658-199604000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsuoka H, Kurosawa S, Horinouchi T, Kato M, Hashimoto Y. Inhalation anesthetics induce apoptosis in normal peripheral lymphocytes in vitro. Anesthesiology. 2001;95:1467–72. doi: 10.1097/00000542-200112000-00028. [DOI] [PubMed] [Google Scholar]
- 5.Loop T, Dovi-Akue D, Frick M, Roesslein M, Egger L, Humar M, Hoetzel A, Schmidt R, Borner C, Pahl HL, Geiger KK, Pannen BH. Volatile anesthetics induce caspase-dependent, mitochondria-mediated apoptosis in human T lymphocytes in vitro. Anesthesiology. 2005;102:1147–57. doi: 10.1097/00000542-200506000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Karpinski TM, Kostrzewska-Poczekaj M, Stachecki I, Mikstacki A, Szyfter K. Genotoxicity of the volatile anaesthetic desflurane in human lymphocytes in vitro, established by comet assay. J Appl Genet. 2005;46:319–24. [PubMed] [Google Scholar]
- 7.Wei H, Kang B, Wei W, Liang G, Meng QC, Li Y, Eckenhoff RG. Isoflurane and sevoflurane affect cell survival and BCL-2/BAX ratio differently. Brain Res. 2005;1037:139–47. doi: 10.1016/j.brainres.2005.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Wei HF, Liang G, Yang H, Wang QJ, Hawkins B, Madesh M, Wang SP, Eckenhoff RG. The common inhalational anesthetic isoflurane induces apoptosis via activation of inositol 1,4,5-trisphosphate receptors. Anesthesiology. 2008;108:251–60. doi: 10.1097/01.anes.0000299435.59242.0e. [DOI] [PubMed] [Google Scholar]
- 9.Liang G, Wang QJ, Li Y, Kang B, Eckenhoff MF, Eckenhoff RG, Wei HF. A presenilin-1 mutation renders neurons vulnerable to isoflurane toxicity. Anesth Analg. 2008;106:492–500. doi: 10.1213/ane.0b013e3181605b71. [DOI] [PubMed] [Google Scholar]
- 10.Berridge MJ. Inositol trisphosphate and calcium signalling. Nature. 1993;361:315–25. doi: 10.1038/361315a0. [DOI] [PubMed] [Google Scholar]
- 11.Lewis RS. Calcium signaling mechanisms in T lymphocytes. Annu Rev Immunol. 2001;19:497–521. doi: 10.1146/annurev.immunol.19.1.497. [DOI] [PubMed] [Google Scholar]
- 12.Lindholm D, Wootz H, Korhonen L. ER stress and neurodegenerative diseases. Cell Death Differ. 2006;13:385–92. doi: 10.1038/sj.cdd.4401778. [DOI] [PubMed] [Google Scholar]
- 13.Hanson CJ, Bootman MD, Roderick HL. Cell signalling: IP3 receptors channel calcium into cell death. Curr Biol. 2004;14:R933–5. doi: 10.1016/j.cub.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 14.Sedlak TW, Snyder SH. Messenger molecules and cell death: therapeutic implications. JAMA. 2006;295:81–9. doi: 10.1001/jama.295.1.81. [DOI] [PubMed] [Google Scholar]
- 15.Assefa Z, Bultynck G, Szlufcik K, Nadif KN, Vermassen E, Goris J, Missiaen L, Callewaert G, Parys JB, De Smedt H. Caspase-3-induced truncation of type 1 inositol trisphosphate receptor accelerates apoptotic cell death and induces inositol trisphosphate-independent calcium release during apoptosis. J Biol Chem. 2004;279:43227–36. doi: 10.1074/jbc.M403872200. [DOI] [PubMed] [Google Scholar]
- 16.Szlufcik K, Missiaen L, Parys JB, Callewaert G, De Smedt H. Uncoupled IP3 receptor can function as a Ca2+-leak channel: cell biological and pathological consequences. Biol Cell. 2006;98:1–14. doi: 10.1042/BC20050031. [DOI] [PubMed] [Google Scholar]
- 17.Ehrlich BE, Kaftan E, Bezprozvannaya S, Bezprozvanny I. The pharmacology of intracellular Ca(2+)-release channels. Trends Pharmacol Sci. 1994;15:145–9. doi: 10.1016/0165-6147(94)90074-4. [DOI] [PubMed] [Google Scholar]
- 18.Madesh M, Hawkins BJ, Milovanova T, Bhanumathy CD, Joseph SK, Ramachandrarao SP, Sharma K, Kurosaki T, Fisher AB. Selective role for superoxide in InsP3 receptor-mediated mitochondrial dysfunction and endothelial apoptosis. J Cell Biol. 2005;170:1079–90. doi: 10.1083/jcb.200505022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franks NP, Lieb WR. Temperature dependence of the potency of volatile general anesthetics: implications for in vitro experiments. Anesthesiology. 1996;84:716–20. doi: 10.1097/00000542-199603000-00027. [DOI] [PubMed] [Google Scholar]
- 20.Li Y, Liang G, Wang S, Meng Q, Wang Q, Wei H. Effect of fetal exposure to isoflurane on postnatal memory and learning in rats. Neuropharmacology. 2007;53:942–50. doi: 10.1016/j.neuropharm.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morita T, Tanimura A, Nezu A, Kurosaki T, Tojyo Y. Functional analysis of the green fluorescent protein-tagged inositol 1,4,5-trisphosphate receptor type 3 in Ca2+ release and entry in DT40 B lymphocytes. Biochem J. 2004;382:793–801. doi: 10.1042/BJ20031970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rutter GA. Moving Ca2+ from the encloplasmic reticulum to mitochondria: is spatial intimacy enough? Biochem Soc Trans. 2006;34:351–5. doi: 10.1042/BST0340351. [DOI] [PubMed] [Google Scholar]
- 23.Green DR, Kroemer G. The pathophysiology of mitochondrial cell death. Science. 2004;305:626–9. doi: 10.1126/science.1099320. [DOI] [PubMed] [Google Scholar]
- 24.De Smet P, Parys JB, Callewaert G, Weidema AF, Hill E, De Smedt H, Erneux C, Sorrentino V, Missiaen L. Xestospongin C is an equally potent inhibitor of the inositol 1,4,5-trisphosphate receptor and the endoplasmic-reticulum Ca2+ pumps. Cell Calcium. 1999;26:9–13. doi: 10.1054/ceca.1999.0047. [DOI] [PubMed] [Google Scholar]
- 25.Wei H, Liang G, Yang H. Isoflurane preconditioning inhibited isoflurane-induced neurotoxicity. Neurosci Lett. 2007;425:59–62. doi: 10.1016/j.neulet.2007.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bickler PE, Zhan X, Fahlman CS. Isoflurane preconditions hippocampal neurons against oxygen-glucose deprivation: role of intracellular Ca2+ and mitogen-activated protein kinase signaling. Anesthesiology. 2005;103:532–9. doi: 10.1097/00000542-200509000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Bickler PE, Fahlman CS. The inhaled anesthetic, isoflurane, enhances Ca2+-dependent survival signaling in cortical neurons and modulates MAP kinases, apoptosis proteins and transcription factors during hypoxia. Anesth Analg. 2006;103:419–29. doi: 10.1213/01.ane.0000223671.49376.b2. [DOI] [PubMed] [Google Scholar]
- 28.Paschen W, Mengesdorf T. Endoplasmic reticulum stress response and neurodegeneration. Cell Calcium. 2005;38:409–15. doi: 10.1016/j.ceca.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 29.Orrenius S, Zhivotovsky B, Nicotera P. Regulation of cell death: the calcium-apoptosis link. Nat Rev Mol Cell Biol. 2003;4:552–65. doi: 10.1038/nrm1150. [DOI] [PubMed] [Google Scholar]