Abstract
Background and Purpose: Disagreement currently exists regarding the contributions of various factors to physical activity in older adults. The purpose of this cross-sectional study was to investigate the simultaneous impact of psychological (health perception and balance perception) and physiological (gait speed, fall history, and balance performance) factors on walking activity in older adults.
Subjects and Methods: This cross-sectional secondary data analysis included 2,269 community-dwelling older adults from the Cardiovascular Health Study. A series of simultaneous linear regression models were constructed to examine the association of walking activity with health and balance perception, gait speed, fall history, and balance performance after controlling for potential confounding factors.
Results: Health and balance perception and gait speed were significantly related to walking activity after controlling for potential confounding factors. Participants who perceived both their health and their balance to be good walked more blocks per week than those who reported a discordant perception, who walked more than those who perceived both their health and their balance to be poor. Participants who walked at a normal speed walked more blocks per week than those who walked at a slow speed.
Discussion and Conclusion: The measure of physical activity used in this study included only walking, not other low- to moderate-intensity activities that are common in older adults. Health and balance perception and gait speed were associated with walking activity more so than fall history or balance performance after controlling for potential confounding factors.
A physically active lifestyle is associated with a decreased risk for a variety of chronic diseases and health conditions.1–9 According to the Centers for Disease Control and Prevention, 60% of US adults do not achieve the Surgeon General's physical activity recommendations of 30 minutes of moderate-intensity activity on most, if not all, days of the week.9–11 One population at greatest risk of being sedentary is older adults, with nearly 51% of adults aged 65 years and older reporting no moderate-intensity physical activity.9,12 It seems that simply disseminating information on the health benefits of moderate-intensity physical activity to older adults has not sufficiently increased participation in physical activity.13 Factors that influence physical activity in older adults need to be clearly identified, investigated, and subsequently managed so that interventions with the greatest likelihood of success can be developed.14,15
Various psychological, physiological, sociological, and environmental factors have been shown to influence physical activity in older adults.16,17 Different conclusions are often drawn when clinicians and investigators do not consider the effects of these factors on people's physical activity. Some of these factors could be influenced by physical therapy or other medical interventions, whereas other factors (such as age and sex) are set and often are adjusted for in clinical and research practice. We believe that balance perception and health perception,16,18,19 gait speed,20 fall history,21 and balance performance22 are all constructs that could be influenced by physical therapy or other health care interventions but that demographic factors and cognition are more set. A perception of one's own health as being poor,18,19 a slow gait speed,20 and a history of falls21 were previously shown to correlate with reduced physical activity. However, physical activity could increase fall risk because being active involves displacing the body's center of gravity and balance,23 making it difficult to conclude that an older adult who is active is protected against falls. Balance has been positively associated with physical activity.22
The purpose of this cross-sectional study was to focus on the simultaneous impact of 2 types of factors, psychological (health perception and balance perception16,18,19) and physiological (gait speed,20 fall history,21 and balance performance22), on walking activity in older adults after controlling for potential confounding factors (demographics, cognition, and health status). The hypotheses for our study were as follows: (1) older adults who perceive their health and balance to be poor will walk less than those who do not perceive their health and balance to be poor; (2) older adults with poor mobility (gait speed), poor balance performance (tandem stance), or both will walk less than those with better mobility and balance performance; and (3) older adults who have fallen in the preceding year will walk less than those who have not fallen.
Method
Participants
Participants for this cross-sectional secondary data analysis included community-dwelling older adults from the Cardiovascular Health Study 1998–1999 clinic assessment. The Cardiovascular Health Study was a longitudinal study including 5,888 adults aged 65 years and older and recruited from a random sample of people enrolled in Medicare. This sample included 5,201 participants examined between June 1989 and June 1990 and an additional 687 African-American participants recruited in 1992–1993 and undergoing the same baseline examination. Details of the Cardiovascular Health Study design and recruitment have been published elsewhere.24,25 In brief, participants were recruited from a random sample of the Health Care Financing Administration Medicare eligibility lists in 4 US communities: Forsyth County, North Carolina; Sacramento County, California; Washington County, Maryland; and Allegheny County, Pennsylvania. The community sites obtained institutional review board approval from their respective universities. Participants were excluded if they were living in an institution, were wheelchair bound in the home, or were undergoing treatment for cancer. All measures for this cross-sectional analysis were recorded during the 1998–1999 clinic visit. Only participants who were alive during the 1998–1999 clinic visit and for whom complete data for health and balance perception, gait speed, fall history, balance performance, and walking activity were available were included in the analysis (N=2,269). Written informed consent was obtained from all study participants.
Potential Factors Affecting Walking Activity
Psychological factors.
The psychological factors assessed in this study were health perception and balance perception. Health perception was assessed by asking participants the following question: “In general, is your health excellent, very good, good, fair, or poor?” The participants’ self-reports of health perception then were dichotomized into 2 groups: good (excellent, very good, or good) and poor (fair or poor). Balance perception was assessed by asking participants the following question: “Do you think your balance is poor—yes or no?” Health perception and balance perception were then combined into a composite perception score of “good perception” (perceived both health and balance to be good), “discordant perception” (perceived either health or balance to be poor), or “poor perception” (perceived both health and balance to be poor) because the 2 variables fit the definition of overlapping risk factors. Risk factors can be overlapping if: (1) the proposed risk factors are correlated, (2) there is no temporal precedence of either risk factor, and (3) the risk factors are codominant.26 All 3 criteria were met for health perception and balance perception in this study. In such situations, the factors might best be combined to obtain a risk factor that more reliably represents the shared construct which, in this study, was perception.26
Physiological factors.
The physiological factors assessed in this study were gait speed, fall history, and balance performance. Gait speed was assessed by measuring the time, in seconds, required for a participant to complete a 4.5-m (15-ft) walk from a standing start; the measurement was reported in meters per second. Gait speed then was dichotomized into 2 groups: slow (<1.0 m/s) and normal (≥1.0 m/s). Identifying a clinically meaningful cutoff point for gait speed of 1.0 m/s, Cesari et al27 reported that people who walked at less than 1.0 m/s were at greater risk for lower-extremity limitations, death, and hospitalization within 1 year. We are aware that important information can be lost when continuous variables (such as gait speed) are categorized, but the use of a clinical cutoff point often enhances the adoption of a measure.27 Fall history was measured by asking the participants the following question: “During the last year, have you had a fall—yes or no? (Do not include falls during skiing, skating, or other activities that may affect balance.)” Finally, balance performance was assessed by testing a participant's ability (able or unable) to maintain a tandem stance for 10 seconds.
Walking Activity
The outcome of interest, walking activity, was assessed by asking participants the following question: “During the last week, how many city blocks did you walk outside of your home?” Walking activity is an appropriate indicator of physical activity in older adults because walking is the most prevalent physical activity reported for older adults of all sociodemographic strata in the United States.16,17,28
Potential Confounding Factors
We controlled for various factors that have been shown to correlate highly with physical activity and that could confound the relationship between our factors of interest and walking activity. We adjusted for demographics (age, race, and sex), cognition, and health status because all have been correlated with physical activity.29–32 Cognition was assessed with the Modified Mini-Mental State Examination (3MS), with scores from 0 to 100; higher scores indicate better cognitive function. Compared with the original Mini-Mental State Examination, the 3MS was designed to sample a broader variety of cognitive functions, cover a wider range of difficulty levels, and enhance the reliability and validity of scoring.33,34 Teng and colleagues33,35 found that the sensitivities of the 3MS with cutoff scores of 79 of 100 and 80 of 100 for detecting dementia were 91% and 97%, respectively. Health status was quantified as the number of medications taken by each participant. Participants brought their medications to their clinic visits, and the medications were counted and recorded by the research staff.
Data Analysis
For descriptive statistics, continuous data (blocks walked, number of medications, age, and 3MS scores) are presented as means and standard deviations, and categorical data (perception, gait speed, fall history, balance performance, and race) are presented as frequencies (percentages). An analysis of covariance was performed with age, sex, race, cognition, and health status as covariates to obtain the adjusted means of blocks walked according to perception, gait speed, fall history, and balance performance.
A series of simultaneous linear regression models were constructed to examine the association of the outcome (number of blocks walked) with the psychological (health and balance perception) and physiological (gait speed, fall history, and balance performance) factors after controlling for potential confounding factors (demographics, cognition, and health status). The potential confounding factors for walking activity were entered into model 1. In model 2, model 1 variables plus the psychological and physiological factors were entered. The goal of our data analysis was to reveal the independent contributions of health and balance perception, fall history, balance performance, and gait speed to the number of blocks walked per week after controlling for demographics, cognition, and health status (number of medications). The contribution of each variable to the regression equation was described in terms of the beta coefficient and the corresponding statistical significance. The adjusted multivariate coefficient of determination (R2) was used to describe the variability in blocks walked explained by the all of the variables of interest entered into the model. However, our purpose was not to explain as much of the variability in walking activity as possible. We realize that many other factors (such as socioeconomic status, social support, home and neighborhood layout, depression, fear of falling, strength [force-generating capacity], and vision) could influence walking activity. Additionally, an F value and statistical significance associated with the change in R2 are reported. All 2-way interactions of the independent variables were examined. A P value of ≤.05 (2-sided) was considered to represent a significant effect on walking activity.
To ensure that the reliability of the regression was not compromised by multicollinearity, we also determined the tolerance of each variable before entry into the equation; a high tolerance (>0.5) and a variance inflation factor (<10) indicated that the reliability of the estimate of the regression coefficient was not significantly affected by collinearity between the independent variables in the equation. Data analysis was conducted with SPSS statistical software, version 15.0.*
Results
The demographic characteristics of the participants are shown in Table 1. The mean age of the participants was 79.2 years (SD=4.14). There were more women (60%) in our sample than men, and most participants classified their race as white (85%). The majority of the participants perceived their health and balance as good (63%), had not fallen (82%), were able to maintain a tandem stance (64%), and had gait speeds of less than 1.0 m/s, classifying them as walking slowly (72%).
Table 1.
Demographic Characteristics of the Study Participants (N=2,269)
The outcome variable of blocks walked violated the assumption of normality for linear regression; therefore, the data were transformed by calculating the square root of blocks walked. The square root of blocks walked then was used as the outcome variable. The results obtained with the transformed data (square root of blocks walked) were similar to those obtained with the nontransformed data; as a consequence, the nontransformed variable for blocks walked was used for ease of interpretation.
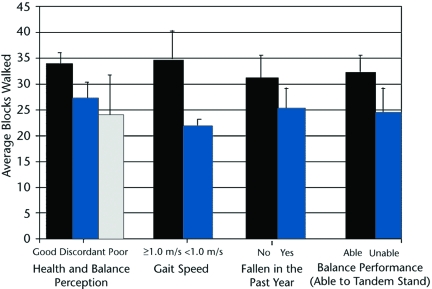
Health and balance perception and gait speed were significantly related to blocks walked after controlling for demographics, cognition, and health status (Figure). Participants with a good perception for both health and balance walked more blocks per week than those who had a discordant perception, who walked more than those with a poor perception (33.8<27.2<24.0 blocks, respectively; good versus discordant: t=3.31, P=.001; good versus poor: t=2.59, P=.010). Because there are approximately 10 city blocks in 1.6 km (1 mile), older adults with a good perception walked, on average, 10 blocks or 1.6 km (1 mile) more per week than those with a poor perception. Additionally, participants who walked at a near-normal speed (≥1.0 m/s) walked more blocks per week than those who walked at a slow speed (<1.0 m/s) (34.8 and 21.9 blocks, respectively; t=6.60, P<.001). Moreover, participants with a good perception for both health and balance had a higher mean gait speed (0.93 m/s) than those with a discordant perception (0.78 m/s), who had a higher mean gait speed than those with a poor perception (0.65 m/s). There was a moderate correlation (Spearman r=.331; P<.001) between health and balance perception groups and gait speed. Fall history and balance performance did not have significant effects on walking activity (t=−1.09, P=.28, and t=1.19, P=.23, respectively) (Tab. 2). Interaction effects were not found to be significant in this analysis (P=.42–.91).
Figure.
Average blocks walked according to health and balance perception, gait speed, fall history, and balance performance after controlling for age, race, sex, health status, and cognition (N=2,269).
Table 2.
Results of Simultaneous Linear Regression Analyses Assessing Differences in Blocks Walked According to Several Variables (N=2,269)a
After controlling for age, race, sex, health status, and cognition.
bReference group=good perception.
cSignificance was set at P<.05.
The adjusted multivariate coefficient of determination (R2) revealed that a significant 9.7% of the variability in blocks walked was explained by all of the variables of interest (demographics, cognition, health status, health and balance perception, gait speed, fall history, and balance performance) entered into the model (F=32.55; df=5,2264; P<.001). The explained variability increased by 3% when the psychological and physiological factors were added in model 2 to the confounders from model 1 (increased from 6.7% to 9.7%, P<.001). Specifically, gait speed explained 1.8% of the variability in blocks walked, and health and balance perception explained 1% of the variability in blocks walked. The reliability of the regression was not compromised by multicollinearity, as evidenced by the tolerance of each variable being greater than .5 (Tab. 2). To account for the possibility of cognitive impairment influencing the self-report measures in this study, we performed an additional simultaneous linear regression including only participants with 3MS scores of greater than 80 (n=2,232).33,35 The results of the regression did not change when participants scoring less than 80 (n=37) on the 3MS were excluded from the analysis.
Discussion and Conclusion
After controlling for demographics, cognition, and health status, we found that health and balance perception and gait speed were associated with walking activity in our sample of community-dwelling older adults, whereas fall history and balance performance were not. Specifically, a good perception for health and balance and walking at a near-normal gait speed were associated with more walking activity. Although several cross-sectional studies have demonstrated that physical activity is related to health perception21 and gait speed,20 other research has failed to show similar associations.16 For instance, for a group of independently functioning older adults residing in a nursing home, Chou et al21 found that physical activity was significantly correlated with perception of health, number of falls, falls efficacy, and fear of falling. However, for a group of 9,442 independently living older white women from the Study of Osteoporotic Fractures, Walsh et al16 found that perceived health (5-point ordinal scale) and fall history (in the preceding 12 months) were not independently associated with walking activity (number of blocks walked for exercise per week). Perhaps a fall without subsequent worry about balance or health does not change walking activity, whereas worry alone, even without a fall, does.
Few concrete conclusions inarguably can be drawn from the existing observational studies of the effects of perception, gait speed, fall history, or balance performance on physical activity. Many previous studies investigated the impact of these factors on physical activity separately, operationally defined the factors differently, or failed to control for variables confounding physical activity.16,36–38 Furthermore, various studies used small numbers of participants and relied on all self-report measures or a mixture of self-report and performance-based measures. We investigated perception, gait speed, fall history, and balance performance together, the factors were clearly operationally defined, and we controlled for demographics, cognition, and health status. Additionally, our study included 2,269 participants and a mixture of self-report measures (walking activity, perception, and fall history) and performance-based measures (3MS, gait speed, and balance performance).
Various performance-based balance tests, self-reports of fall history, or both are often used in physical therapy practice in an attempt to gain insight into patients’ abilities. However, self-reports of balance and health perception are less frequently obtained and used in physical therapy clinics. Self-report and performance-based measures provide different yet complementary information.39 Performance-based measures supplement rather than replace self-report measures.40 Health and balance perception and gait speed may provide valuable information about a participant's physical activity beyond what can be explained by demographics, cognition, and health status. Also, asking people about their health and balance perception and measuring gait speed over a short distance require no expensive equipment and very little time to complete.
Do clinicians pay enough attention to older adults’ physical activity in order to promote health benefits? If clinicians do recognize a lack of physical activity, do they then consider the factors that may influence sedentary behavior? Psychological, physiological, sociological, and environmental determinants of activity should be fully considered by professionals when educating older people about the health benefits of daily physical activity.17
Our study design had several limitations. First, our measure of balance performance (ability to maintain a tandem stance for 10 seconds) was a crude assessment of only static balance with a potential for a ceiling effect. However, if an individual is unable to maintain a tandem stance for 10 seconds—a fairly straightforward static balance task—then it is difficult to argue that the individual's balance is typical of that of people who are healthy. Second, our measure of physical activity included only walking, not other low- to moderate-intensity activities, such as swimming, cycling, and gardening, which are common in older adults.16 Various studies have shown that participation in vigorous activities decreases with age, yet there is less of a relationship between age and participation in moderate-intensity activities, such as walking.41 Therefore, we might have found that other factors, such as balance performance or fall history, played a larger role in determining physical activity had we used a measure that assessed intensity levels. In addition, our measure of walking activity was self-reported number of blocks walked. Although self-reported number of city blocks walked has been used to access physical activity in previous work,42–45 to our knowledge, this measure has not been validated. Finally, because the present study was based on the last clinic visit (1998–1999), survival bias could have been an issue. One would assume that people who were healthier were alive and able to return for this visit. We were able to investigate only a few of the many factors that have been shown to influence physical activity in older adults (ie, self-efficacy,46–49 depression,50,51 fear,37,52–55 strength,46 marital status,56 social support,16 ethnicity,57,58 seasonality, and neighborhood safety15).
Several questions and potential avenues for future work are suggested by our findings. First, the temporal order of effects on physical activity must be established. For instance, which happens first: changes in activity level, perception, or gait speed? Perhaps the relationship among perception, gait speed, and activity is adaptive and older adults limit their activity on the basis of their perception of health and balance, subsequently leading to slow walking. Additionally, people may be able to detect changes in their abilities (perception of health and balance) before they can be detected by simple clinical balance tests or a history of falls. Regardless of the direction of the association, intervention directed toward physical activity, perception, or gait speed may result in a positive change in the others. There is growing evidence that people are more likely to maintain physical activity if they feel confident about their ability to succeed and if they believe that physical activity can have a positive effect on physical function and quality of life.18
Second, perhaps barriers to physical activity differ depending on the type and intensity of the activity. For instance, in the 9,442 independent community-dwelling women included in the study by Walsh et al,16 health perception, fear of falling, alcohol consumption, and estrogen use were associated with medium- or high-intensity physical activity but not with walking activity alone. Future work could implement the use of an activity monitor or detailed physical activity questionnaire to decipher factors associated with different intensity levels of physical activity.
Finally, a longitudinal study investigating health and balance perception, balance performance, fall history, gait speed, and physical activity could begin to establish the temporal relationship of these variables. A longitudinal study could affect clinical practice by establishing which variables best predict future physical activity levels. For instance, if it is known that poor perception leads to a decreased activity level and, furthermore, to a decreased gait speed, then poor perception could be established as a physical inactivity risk factor.
Dr Talkowski, Dr Brach, and Dr Studenski provided concept/idea/research design and writing. Dr Talkowski, Dr Brach, and Dr Newman provided data analysis. Dr Newman provided fund procurement, subjects, facilities/equipment, and institutional liaisons. Dr Brach, Dr Studenski, and Dr Newman provided consultation (including review of manuscript before submission). The authors thank the people who participated in this study.
This research was funded by contracts N01-HC-35129, N01-HC-45133, N01-HC-75150, N01-HC-85079 through N01-HC-85086, N01-HC-15103, N01-HC-55222, and U01-HL-80295 from the National Heart, Lung, and Blood Institute, with an additional contribution from the National Institute of Neurological Disorders and Stroke. Additional funding was provided by the University of Pittsburgh Older American's Independence Center grant P30 AG024827-01. Dr Talkowski is supported by the University of Pittsburgh Department of Physical Therapy. Additional funding for Dr Talkowski was provided by the APTA Promotion of Doctoral Studies I and II Award and the Geriatric Section Adopt-a-Doc Scholarship from the American Physical Therapy Association. Dr Brach is supported by National Institutes on Aging and American Federation of Aging Research Paul Beeson Career Development Award K23 AG026766-01.
A platform presentation of this research was given at the Combined Sections Meeting of the American Physical Therapy Association; February 14–18, 2007; Boston, Massachusetts.
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
References
- 1.Barengo NC, Hu G, Lakka TA, et al. Low physical activity as a predictor for total and cardiovascular disease mortality in middle-aged men and women in Finland. Eur Heart J. 2004;25:2204–2211. [DOI] [PubMed] [Google Scholar]
- 2.Paffenbarger RS Jr, Blair SN, Lee IM. A history of physical activity, cardiovascular health and longevity: the scientific contributions of Jeremy N Morris, DSc, DPH, FRCP. Int J Epidemiol. 2001;30:1184–1192. [DOI] [PubMed] [Google Scholar]
- 3.Tuomilehto J, Lindstrom J, Eriksson J, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. [DOI] [PubMed] [Google Scholar]
- 4.Knowler W, Barrett-Connor E, Fowler S, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention of metformin. N Engl J Med. 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Slattery ML, Murtaugh M, Caan B, et al. Associations between BMI, energy intake, energy expenditure, VDR genotype and colon and rectal cancers. Cancer Causes Control. 2004;15:863–872. [DOI] [PubMed] [Google Scholar]
- 6.Yancey AK, Wold CM, McCarthy WJ, et al. Physical inactivity and overweight among Los Angeles County adults. Am J Prev Med. 2004;27:146–152. [DOI] [PubMed] [Google Scholar]
- 7.Kokkinos P, Moutsatsos G. Obesity and cardiovascular disease: the role of diet and physical activity. J Cardiopulm Rehabil. 2004;24:197–203. [DOI] [PubMed] [Google Scholar]
- 8.Blair SN, LaMonte MJ, Nichaman MZ. The evolution of physical activity recommendations: how much is enough? Am J Clin Nutr. 2004;79:913S–920S. [DOI] [PubMed] [Google Scholar]
- 9.Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services; 1996.
- 10.Physical Activity and Health Fact Sheet: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 1999.
- 11.Physical Activity and Health At-a-Glance: A Report of the Surgeon General. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion; 2001.
- 12.DiPietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Med Sci Sports Exerc. 1993;25:628–642. [PubMed] [Google Scholar]
- 13.Dunn AL, Anderson RE, Jakicic JM. Lifestyle physical activity interventions. Am J Prev Med. 1998;15:398–412. [DOI] [PubMed] [Google Scholar]
- 14.Simonsick EM, Guralnik JM, Fried LP. Who walks? Factors associated with walking behavior in disabled older women with and without self-reported walking difficulty. J Am Geriatr Soc. 1999;47:672–680. [DOI] [PubMed] [Google Scholar]
- 15.King AC, Blair SN, Bild DE, et al. Determinants of physical activity and interventions in adults. Med Sci Sports Exerc. 1992;24(suppl):S221–S236. [PubMed] [Google Scholar]
- 16.Walsh JM, Pressman AR, Cauley JA, Browner WS. Predictors of physical activity in community-dwelling elderly white women. J Gen Intern Med. 2001;16:721–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DiPietro L. Physical activity in aging: changes in patterns and their relationship to health and function. J Gerontol Ser A Biol Sci Med Sci. 2001;56:13–22. [DOI] [PubMed] [Google Scholar]
- 18.Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. J Gerontol Ser A Biol Sci Med Sci. 2001;56:23–35. [DOI] [PubMed] [Google Scholar]
- 19.Elward KS, Wagner EH, Larson EB. Participation by sedentary elderly persons in an exercise promotion session. Fam Med. 1992;24:607–612. [PubMed] [Google Scholar]
- 20.Brach JS, FitzGerald SJ, Newman AB, et al. Physical activity and functional status in community-dwelling older women: a 14 year prospective study. Arch Intern Med. 2003;163:2565–2571. [DOI] [PubMed] [Google Scholar]
- 21.Chou KL, Yeung FK, Wong EC. Fear of falling and depressive symptoms in Chinese elderly living in nursing homes: fall efficacy and activity level as mediator or moderator? Aging Ment Health. 2005;9:255–261. [DOI] [PubMed] [Google Scholar]
- 22.Kuh D, Bassey EJ, Butterworth S, et al. Grip strength, postural control, and functional leg power in a representative cohort of British men and women: associations with physical activity, health status, and socioeconomic conditions. J Gerontol Ser A Biol Sci Med Sci. 2005;60:224–231. [DOI] [PubMed] [Google Scholar]
- 23.Gregg EW, Pereira MA, Caspersen CJ. Physical activity, falls, and fractures among older adults: a review of the epidemiologic evidence. J Am Geriatr Soc. 2000;48:883–893. [DOI] [PubMed] [Google Scholar]
- 24.Tell GS, Fried LP, Hermanson B, et al. Recruitment of adults 65 years and older as participants in the Cardiovascular Health Study. Ann Epidemiol. 1993;3:358–366. [DOI] [PubMed] [Google Scholar]
- 25.Fried LP, Borhani NO, Enright PL, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. [DOI] [PubMed] [Google Scholar]
- 26.Kraemer HC, Stice E, Kazdin A, et al. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158:848–856. [DOI] [PubMed] [Google Scholar]
- 27.Cesari M, Kritchevsky SB, Penninx BW, et al. Prognostic value of usual gait speed in well-functioning older people: results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. [DOI] [PubMed] [Google Scholar]
- 28.McPhillips JB, Pellettera KM, Barrett-Connor E, et al. Exercise patterns in a population of older adults. Am J Prev Med. 1989;5:65–72. [PubMed] [Google Scholar]
- 29.Elward K, Larson E, Wagner E. Factors associated with regular aerobic exercise in an elderly population. J Am Board Fam Pract. 1992;5:467–474. [PubMed] [Google Scholar]
- 30.Wolinsky FD, Stump TE, Clark DO. Antecedents and consequences of physical activity and exercise among older adults. Gerontologist. 1995;35:451–462. [DOI] [PubMed] [Google Scholar]
- 31.Wister AV. The effects of socioeconomic status on exercise and smoking: age-related differences. J Aging Health. 1996;8:467–488. [DOI] [PubMed] [Google Scholar]
- 32.Hovell MF, Sallis JF, Hofstetter CR, et al. Identifying correlates of walking for exercise: an epidemiologic prerequisite for physical activity promotion. Prev Med. 1989;18:856–866. [DOI] [PubMed] [Google Scholar]
- 33.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 34.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 35.Teng EL, Chui HC, Schneider LS, Metzger LE. Alzheimer's dementia: performance on the Mini-Mental State Examination. J Consult Clin Psychol. 1987;55:96–100. [DOI] [PubMed] [Google Scholar]
- 36.Kaplan MS, Newsom JT, McFarland BH, Lu L. Demographic and psychosocial correlates of physical activity in late life. Am J Prev Med. 2001;21:306–312. [DOI] [PubMed] [Google Scholar]
- 37.Bruce DG, Devine A, Prince RL. Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc. 2002;50:84–89. [DOI] [PubMed] [Google Scholar]
- 38.Lim K, Taylor L. Factors associated with physical activity among older people: a population-based study. Prev Med. 2005;40:33–40. [DOI] [PubMed] [Google Scholar]
- 39.Reuben DB, Valle LA, Hays RD, Siu AL. Measuring physical function in community-dwelling older persons: a comparison of self-administered, interviewer-administered, and performance-based measures. J Am Geriatr Soc. 1995;43:17–23. [DOI] [PubMed] [Google Scholar]
- 40.Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the Short Physical Performance Battery. J Gerontol Ser A Biol Sci Med Sci. 2000;55:M221–M231. [DOI] [PubMed] [Google Scholar]
- 41.Sallis JF, Haskell WL, Fortmann SP, et al. Moderate-intensity physical activity and cardiovascular risk factors: the Stanford Five-City Project. Prev Med. 1986;15:561–568. [DOI] [PubMed] [Google Scholar]
- 42.McDermott MM, Ferrucci L, Simonsick EM, et al. The ankle brachial index and change in lower extremity functioning over time: the Women's Health and Aging Study. J Am Geriatr Soc. 2002;50:238–246. [DOI] [PubMed] [Google Scholar]
- 43.Diehr P, Johnson LL, Patrick DL, Psaty B. Methods for incorporating death into health-related variables in longitudinal studies. J Clin Epidemiol. 2005;58:1115–1124. [DOI] [PubMed] [Google Scholar]
- 44.Knudson MD, Klein R, Klein BE. Physical activity and the 15-year cumulative incidence of age-related macular degeneration: the Beaver Dam Eye Study. Br J Ophthalmol. 2006;90:1461–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simonsick EM, Guralnick JM, Volpato S, et al. Just get out the door! Importance of walking outside the home for maintaining mobility: findings from the women's health and aging study. J Am Geriatr Soc. 2005;53:198–203. [DOI] [PubMed] [Google Scholar]
- 46.Sallis JF, Hovell MF, Hofstetter CR, et al. A multivariate study of determinants of vigorous exercise in a community sample. Prev Med. 1989;18:20–34. [DOI] [PubMed] [Google Scholar]
- 47.McAuley E, Jacobson L. Self-efficacy and exercise participation in sedentary adult females. Am J Health Promot. 1991;5:185–191. [DOI] [PubMed] [Google Scholar]
- 48.McAuley E, Courneya KS, Lettunich J. Effects of acute and long-term exercise on self-efficacy responses in sedentary, middle-aged males and females. Gerontologist. 1991;31:534–542. [DOI] [PubMed] [Google Scholar]
- 49.McAuley E, Mihalko SL, Bane SM. Exercise and self-esteem in middle-aged adults: multidimensional relationships and physical fitness and self-efficacy influences. J Behav Med. 1997;20:67–83. [DOI] [PubMed] [Google Scholar]
- 50.Blumenthal JA, Babyak MA, Moore KA, et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999;159:2349–2356. [DOI] [PubMed] [Google Scholar]
- 51.Moore KA, Blumenthal JA. Exercise training as an alternative treatment for depression among older adults. Altern Ther Health Med. 1998;4:48–56. [PubMed] [Google Scholar]
- 52.Martin FC, Hart D, Spector T, et al. Fear of falling limiting activity in young-old women is associated with reduced functional mobility rather than psychological factors. Age Ageing. 2005;34:281–287. [DOI] [PubMed] [Google Scholar]
- 53.Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42:17–23. [DOI] [PubMed] [Google Scholar]
- 54.Vellas BJ, Wayne SJ, Romero LJ, et al. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997;26:189–193. [DOI] [PubMed] [Google Scholar]
- 55.Lachman ME, Howland J, Tennstedt S, et al. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFFE). J Gerontol Ser B Psychol Sci Soc Sci. 1998;53:P43–P50. [DOI] [PubMed] [Google Scholar]
- 56.Schone BS, Weinick RM. Health-related behaviors and the benefits of marriage for elderly persons. Gerontologist. 1998;38:618–627. [DOI] [PubMed] [Google Scholar]
- 57.King AC, Castro C, Wilcox S, et al. Personal and environmental factors associated with physical inactivity among different racial-ethnic groups of U.S. middle-aged and older-aged women. Health Psychol. 2000;19:354–364. [DOI] [PubMed] [Google Scholar]
- 58.Brownson RC, Eyler AA, King AC, et al. Patterns and correlates of physical activity among US women 40 years and older. Am J Public Health. 2000;90:264–270. [DOI] [PMC free article] [PubMed] [Google Scholar]