Abstract
Background and Purpose: Studies have identified factors that contribute to functional limitations in people with knee osteoarthritis (OA), including quadriceps femoris muscle weakness, joint laxity, and reports of knee instability. However, little is known about the relationship among these factors or their relative influence on function. The purpose of this study was to investigate self-reported knee instability and its relationships with knee laxity and function in people with medial knee osteoarthritis (OA).
Participants: Fifty-two individuals with medial knee OA participated in the study.
Methods: Each participant was classified into 1 of 3 groups based on reports of knee instability. Limb alignment, knee laxity, and quadriceps femoris muscle strength (force-generating capacity) were assessed. Function was measured with the Knee Injury and Osteoarthritis Outcome Score (KOOS) and a stair-climbing test (SCT). Group differences were detected with one-way analyses of variance, and relationships among variables were assessed with the Eta2 statistic and hierarchical regression analysis.
Results: There were no differences in alignment, laxity, or strength among the 3 groups. Self-reported knee instability did not correlate with medial laxity, limb alignment, or quadriceps femoris muscle strength. Individuals reporting worse knee instability scored worse on all subsets of the KOOS. Self-reported knee instability scores significantly contributed to the prediction of all measures of function above that explained by quadriceps femoris muscle force, knee laxity, and alignment. Neither laxity nor alignment contributed to any measure of function.
Discussion and Conclusion: Self-reported knee instability is a factor that is not directly associated with knee laxity and contributes to worse function. Further research is necessary to delineate the factors that contribute to self-reported knee instability and reduced function in this population.
Tibiofemoral joint osteoarthritis (OA) is one of the most common and disabling medical conditions in the United States and worldwide.1–7 Knee OA is responsible for more chronic disability than any other medical condition and is one of the most frequent medical problems.2,3,8 Within the knee joint, the medial compartment is the most often involved.9,10
Studies8,11,12 have identified factors that contribute to disability and functional limitations in people with knee OA, and one of the most notable factors is decreased quadriceps femoris muscle strength (force-generating capacity). Quadriceps femoris muscle weakness is not only associated with diminished function8,11 but is also an important predictor of functional decline.13 Quadriceps femoris muscle strength training, therefore, is typically recommended for people with knee OA. However, recent work indicates that the relationship between quadriceps femoris muscle strength and physical function is not as strong in people with excessive frontal-plane knee laxity,14 a common characteristic in people with knee OA.15,16 Furthermore, the combination of strong quadriceps femoris muscles and excessive mediolateral knee laxity is associated with higher rates of OA progression.17 This suggests that rehabilitation interventions that focus on quadriceps femoris muscle strengthening alone may not be the most effective for all people with knee OA.
Much attention has been paid to joint laxity in people with knee OA due to its prevalence in this population15,16 and its reported relationship with functional limitations.14 Joint laxity is a clinical sign that is measured passively; however, it is presumed that excessive passive motion in the knee joint automatically leads to instability during dynamic and functional activities. Studies have shown that some individuals with increased anterior knee laxity due to anterior cruciate ligament (ACL) deficiency report no symptoms of knee instability18–21 and use different neuromuscular activation strategies compared with the strategies used by people who do report knee instability.22–25 Therefore, neuromuscular control strategies appear to play a role in stabilizing the knee even in the face of impaired passive restraints.
Recent work26–28 has suggested that self-reported knee instability (the sensation of shifting, buckling, or giving way of the knee) negatively affects the function of people with knee OA. Fitzgerald et al27 showed that a substantial number of people with knee OA report sensations of knee instability during daily activities. Furthermore, they found that self-reported knee instability significantly lowers physical function beyond the influence of pain, reduced knee range of motion, and quadriceps femoris muscle weakness.27 Other common characteristics of people with knee OA that have been associated with worse function, such as knee laxity14,29 and knee alignment,14,29 were not evaluated by Fitzgerald et al.27 The relationships among these factors with self-reported knee instability and their influences on function need to be delineated.
The relationship between medial knee laxity and self-reported knee instability in people with medial knee OA is unclear. If medial knee laxity and self-reported knee instability influence daily function independently, treatment plans should address both conditions. If, as current literature24 suggests, self-reported knee instability has a greater influence on function than laxity, then addressing self-reported knee instability should be the focus of rehabilitation. Therefore, in people with medial knee OA, the aims of this work were: (1) to investigate the relationship between self-reported knee instability and medial knee laxity, varus alignment, and quadriceps femoris muscle force; (2) to compare the level of function of participants classified by reports of knee instability; and (3) to investigate the influences of self-reported knee instability, medial laxity, varus alignment, and quadriceps femoris muscle force on function.
Method
Participants
Individuals with diagnosed medial knee OA were referred from local physicians and were recruited from the community. Participants were included if they had grade II or greater Kellgren and Lawrence (K-L) radiographic changes30 in the medial tibiofemoral compartment, with grades 0 or I in the lateral tibiofemoral and patellofemoral compartments. Radiographic changes were determined from standing bent posterior-anterior view, lateral view, and sunrise view radiographs. If a potential participant had bilateral knee OA that fit the criteria, the more symptomatic knee was identified by the individual and used in the analysis. Participants were excluded if they had a history of other orthopedic injuries in the lower extremities (eg, knee ligament injuries) or spine, used an assistive device, had a history of neurologic injury, had a history of rheumatoid arthritis, were pregnant, or had undergone a joint replacement or skeletal realignment procedure in either lower extremity. All participants signed an informed consent statement approved by the Institutional Review Board of the University of Delaware.
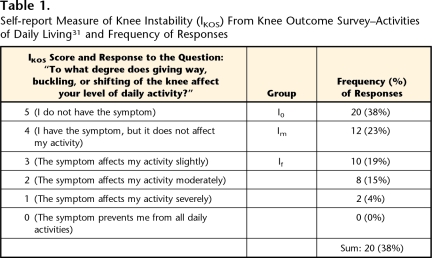
Participants were classified into groups based on their reports of knee instability. Knee instability was measured using the Knee Outcome Survey–Activities of Daily Living Scale31 (KOS-ADLS), which is a self-report measure of function. One question from the KOS-ADLS relating to functional stability of the knee (IKOS) was used to classify participants as having stable or unstable knees. The IKOS has been shown to be a reliable measure of self-reported knee instability in patients with knee OA.27 Participants rated the severity of knee instability on a 6-point scale in response to the question, “To what degree does giving way, buckling, or shifting of your knee affect your level of daily activity?” Definitions of the scores are shown in Table 1. Participants were classified into 1 of 3 self-reported knee instability groups: those with no knee instability (I0 group) (IKOS score=5), those with mild knee instability that does not affect function (Im group) (IKOS score=4), or those with knee instability that affects function (If group) (IKOS score ≤3) (Tab. 1).
Table 1.
Self-report Measure of Knee Instability (IKOS) From Knee Outcome Survey–Activities of Daily Living31 and Frequency of Responses
The sample size estimate for detecting differences in function between participants with stable knees and those with unstable knees was based on a large effect size, which was found in a previous study in our laboratory of people with medial knee OA.32 A difference in function scores between participants with self-reported knee instability and those without self-reported knee instability was 18, which is reported to reflect clinically meaningful changes in function for people with knee OA.33 Based on variability measures from the pilot work, a difference in population means of 18, and an alpha level of .05, a sample size of 12 participants per group was required to achieve 1–β=0.80.
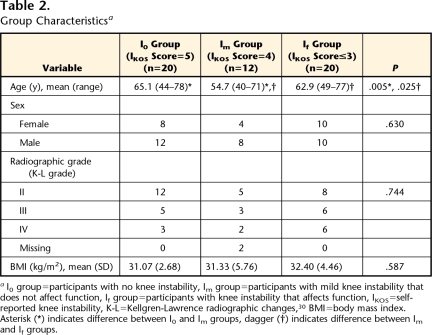
A total of 52 participants were enrolled, with at least 12 participants in each self-reported knee instability group. Group characteristics are shown in Table 2. All data were collected over 2 testing sessions. During the first session, self-assessment questionnaires were completed, physical function was assessed, and quadriceps femoris muscle strength was evaluated. During the second session, radiographic assessments of tibiofemoral joint alignment and frontal-plane laxity were completed.
Table 2.
Group Characteristicsa
I0 group=participants with no knee instability, Im group=participants with mild knee instability that does not affect function, If group=participants with knee instability that affects function, IKOS=self-reported knee instability, K-L=Kellgren-Lawrence radiographic changes,30 BMI=body mass index. Asterisk (*) indicates difference between I0 and Im groups, dagger (†) indicates difference between Im and If groups.
Self-assessment of Function
The Knee Injury and Osteoarthritis Outcome Score34,35 (KOOS) was used as a self-report measure of function. The KOOS covers 5 separate dimensions of knee function: Pain, Symptoms, Activities of Daily Living (ADL), Sport and Recreation Function (Sport), and Knee-Related Quality of Life (QOL). Each dimension, or subset, is scored separately and evaluated independently. The KOOS includes questions from the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and has been shown to be a valid, reliable, and responsive measure of overall knee joint function in people with OA.36 On the KOOS, all dimensions are scored from 0 to 4, and then scores are transformed to a percentage score of 0 to 100, with 0 representing extreme knee problems and 100 representing no knee problems.34
Performance-Based Assessment of Physical Function
A timed stair-climbing test (SCT) was used as a performance-based measure of function. Participants were timed with a stopwatch as they ascended and descended a set of 12 stairs (18 cm high). The participants were instructed to perform the task as quickly as they felt safe and comfortable. They were encouraged not to use the handrail, but were not prohibited from doing so for safety. A longer time to complete the SCT represents worse functional limitations. Excellent test-retest reliability (Pearson r=.93) was reported for a similar stair-climbing task in people with knee OA.37
Radiograph Assessment
Joint alignment.
Tibiofemoral joint alignment was measured from long cassette anterior-posterior (AP) radiographs that included the hip, knee, and ankle joints. The x-ray tube was centered at the knee at a distance of approximately 2 m. Participants stood barefoot, with the knees as straight as possible, and bearing weight on both lower extremities. They were positioned with the tibial tubercles facing anteriorly. Alignment was measured as the angle formed by the mechanical axis of the femur and of the tibia38–40 (Fig. 1). The mechanical axes of the femur and tibia were defined from lines connecting the center of the femoral head to the knee center and connecting the center of the talus to the knee center, respectively (Fig. 1). An angle of less than 180 degrees was defined as varus, and an angle of greater than 180 degrees was defined as valgus. Measurements were done by one author (LCS), and the intraclass correlation coefficient (ICC) for repeated measurements using these methods was .978.
Figure 1.
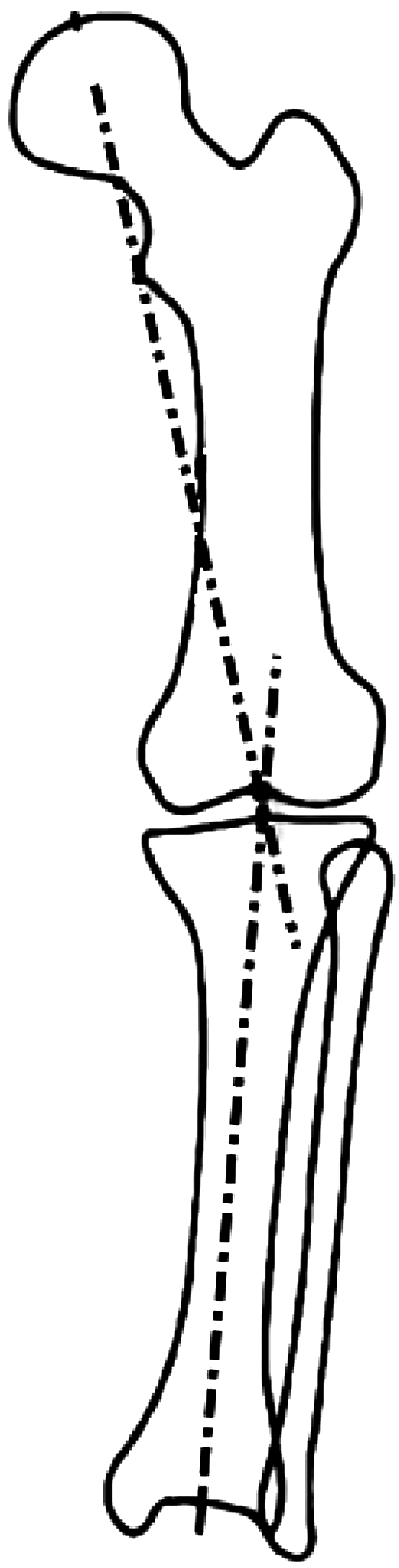
Tibiofemoral joint alignment was determined by the angle formed by the intersection of the mechanical axis of the femur and the mechanical axis of the tibia. The figure shows an angle of less than 180 degrees, indicating varus alignment.
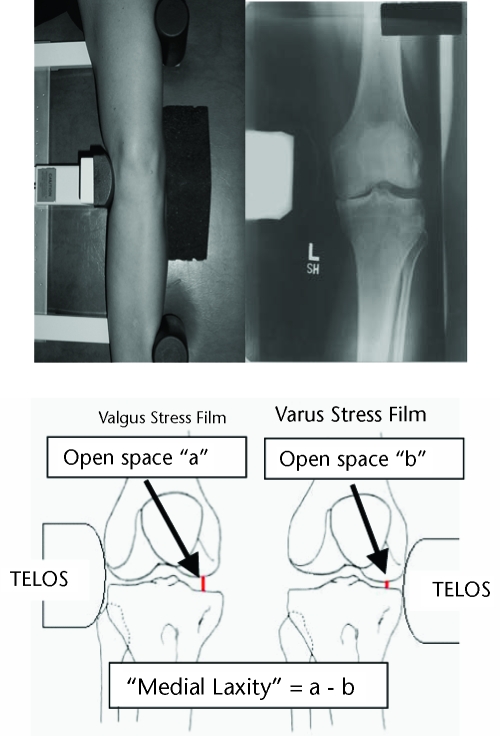
Frontal-plane knee laxity.
Medial and lateral knee joint laxities were measured using the “open-space” technique41 from stress radiographs. For the radiographs, participants were positioned supine in a TELOS stress device* with the knee flexed 20 degrees and the patella facing anteriorly to minimize limb rotation. The x-ray beam was centered approximately 91 cm above the knee joint. The TELOS device was used to apply a 150-N force to the joint line to produce opening on the opposite side of the joint (Fig. 2). Radiographs were adjusted for magnification using a known distance from the TELOS device that was visible in every image. Joint space was measured at the narrowest point in the medial and lateral compartments during the application of varus and valgus forces. Joint laxity was calculated by subtracting the measured joint space during joint closing from that during joint opening (Fig. 2). Measurements were made by one author (LCS), and ICC values for repeated measurements using these methods were .978 for medial laxity and .975 for lateral laxity.
Figure 2.
Setup for varus stress radiograph on left lower extremity, with corresponding radiograph (top). For the varus stress radiograph (shown), a consistent 150-N force was applied to the medial knee joint line. For the valgus stress radiograph (not shown), the force was applied to the lateral joint line. Calculation of medial laxity (bottom).44
Quadriceps Femoris Muscle Function
Quadriceps femoris muscle force output (in newtons) was measured during a maximal voluntary isometric contraction (MVIC), with electrical burst superimposition to ensure maximal quadriceps femoris muscle activation.42 Each participant sat in an isokinetic dynamometer (Kin Com†) with the knee flexed to 90 degrees, the joint axis aligned with the dynamometer axis, and the trunk fully supported. Chest, hip, and thigh straps secured the participant to the chair, and an ankle strap secured the shank to the dynamometer. Following skin preparation, self-adhesive gel electrodes (7.62×12.70 cm)‡ were secured proximally over the rectus femoris muscle and distally over the vastus medialis muscle. Each participant practiced producing maximal quadriceps femoris muscle contractions against the dynamometer arm while verbal encouragement and visual feedback were provided to maximize volitional efforts. For the test, participants were asked to produce an MVIC of their quadriceps femoris muscle, during which a supramaximal burst of electrical current (100 pulses per second, 600-microsecond pulse duration, 10-pulse tetanic train, 130 V) from a Grass S48 stimulator§ was delivered to the muscle. The burst of electrical current was used only to assess whether the participants were attempting maximum activation of the quadriceps femoris muscles.42 The MVIC was the highest volitional force prior to the onset of the electrical burst. Volitional force production can be influenced by both limb length and body mass, which may limit group comparisons. In our sample, there was a strong relationship between height (in meters) and force produced by the quadriceps femoris muscle during the MVIC (r=.67, P<.001). In order to accurately compare group data, quadriceps femoris muscle force was normalized by height (in newtons per meter).
Data Analysis
Group differences.
For all variables of interest, means and standard deviations or 95% confidence intervals were calculated for the self-reported knee instability groups (I0, Im, and If). One-way analyses of variance were used to evaluate differences among the knee instability groups in age, body mass index (BMI), radiograph variables, quadriceps femoris muscle force, scores on KOOS subsets, and time of SCT (dependent variables). Post hoc testing was done with least significant difference tests, when appropriate. We evaluated the frequency distribution of sex and radiograph severity (K-L grade II, III, or IV) among the knee instability groups using chi-square tests of independence.
Relationships among variables.
Relationships among variables were assessed with participants from all groups combined. The Eta2 statistic was used to evaluate the relationships between self-reported knee instability (a categorical variable) and medial laxity, limb alignment, and quadriceps femoris muscle force. Eta2 is a measure of the strength of association between independent and dependent variables and can be used when one or more variables is categorical in nature. Eta2 is calculated as: SSbetween/SStotal, where SS is sum of squares. Eta2 describes the amount of variance in the dependent variable that can be account for by the independent variable, and it is interpreted like an R2 value.
Separate hierarchical regression analyses were used to predict each of the KOOS subset scores and scores on the SCT (dependent variables). The independent variables of quadriceps femoris muscle force, limb alignment, medial laxity, IKOS score, and the interaction between medial laxity and self-reported knee instability (medial laxity × IKOS score) were entered one at a time into each regression model. Hierarchical regression is an incremental approach to multiple regression in which variables are entered into the model based on a priori hypotheses. It can be performed so that the last variable entered into the model is the independent variable whose relationship to the dependent variable is unknown. Based on the literature, relationships have been demonstrated between function and quadriceps femoris muscle strength,8,11,13 knee alignment,29 and knee laxity.14 In this study, we were interested specifically in the influence of self-reported knee instability (IKOS score) on the dependent variables. As such, the IKOS score was entered into the model last in order to assess the influence of self-reported knee instability after accounting for the influence of the other independent variables. Thus, quadriceps femoris muscle force was entered into the model first, followed by limb alignment, then medial laxity, then IKOS score, and finally the interaction term between medial laxity and IKOS score. The interaction term was calculated by multiplying the Z-scores for medial laxity and IKOS score. This technique allowed us to determine the influence of medial laxity, IKOS score or the interaction between the 2 on knee function after strength and alignment had been accounted for. For all analyses (using SPSS version 13.0‖), significance was established when the alpha level was ≤.05.
Results
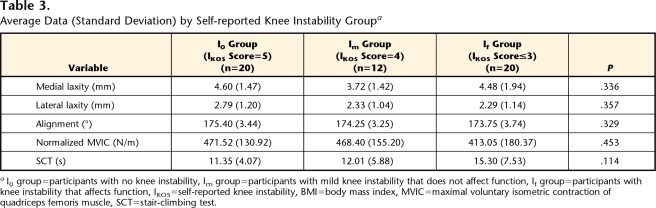
Group Differences
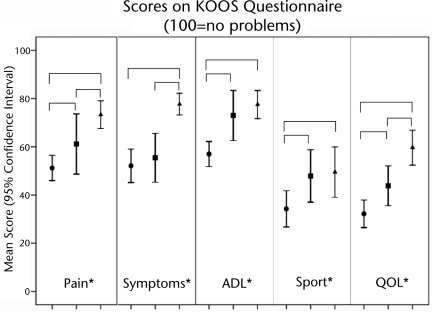
The frequency of IKOS scores is shown in Table 1. The frequency distribution of sex and K-L grade within the self-reported knee instability groups was not statistically different (Tab. 2, P=.630 and P=.744, respectively). On average, the Im group was younger than the other groups (Tab. 2, P≤.025), but there were no differences among the groups in terms of BMI (P=.587) (Tab. 2), medial laxity (P=.336), lateral laxity (P=.357), limb alignment (P=.329), or quadriceps femoris muscle force (P=.453) (Tab. 3). The If group took approximately 4 seconds longer than the I0 group to complete the SCT, but this difference was not statistically significant (P=.114) (Tab. 3). Significant group differences were observed for all subsets of the KOOS questionnaire, as those participants reporting worse knee instability also scored worse on the Pain, Symptoms, ADL, Sport, and QOL subsets (P≤.05, Fig. 3).
Table 3.
Average Data (Standard Deviation) by Self-reported Knee Instability Groupa
I0 group=participants with no knee instability, Im group=participants with mild knee instability that does not affect function, If group=participants with knee instability that affects function, IKOS=self-reported knee instability, BMI=body mass index, MVIC=maximal voluntary isometric contraction of quadriceps femoris muscle, SCT=stair-climbing test.
Figure 3.
Markers represent average scores on subsets of the Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire (Pain, Symptoms, Quality of Life [QOL], Activities of Daily Living [ADL], Sport/Recreation [Sport]), lines represent 95% confidence intervals, brackets indicate significant group differences at *P≤.05, circle=If group (participants with knee instability that affects function), square=Im group (participants with mild knee instability that does not affect function), triangle=I0 group (participants with no knee instability).
Relationships Among Variables
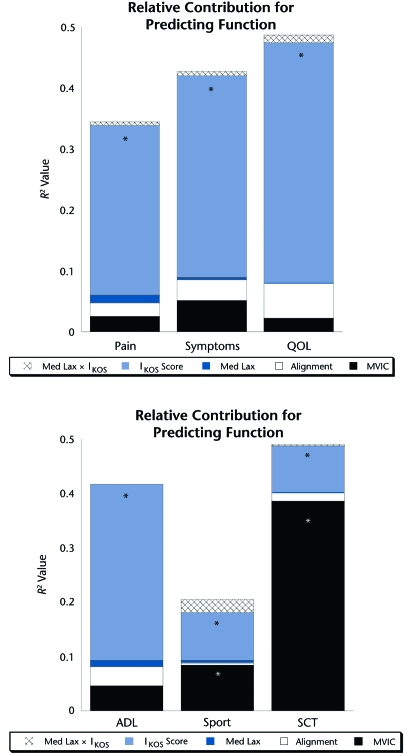
The IKOS score did not relate to medial laxity (Eta2=0.045, P=.336), limb alignment (Eta2=0.044, P=.329), or quadriceps femoris muscle force (Eta2=0.032, P=.453). Results of hierarchical regressions are shown in Figure 4. The IKOS score significantly contributed to the prediction of all KOOS subset scores, even after controlling for quadriceps femoris muscle force, limb alignment, and medial laxity (Fig. 4). In fact, the IKOS score was the only significant predictor of Pain, Symptoms, QOL, and ADL subset scores. Both IKOS score and quadriceps femoris muscle force influenced the prediction of scores on the Sport subset as well as the SCT. Medial laxity, limb alignment, or the interaction between medial laxity and IKOS score did not significantly influence the prediction of any functional score.
Figure 4.
Results of hierarchical regression analysis showing the relative contribution (R2 value) of each variable (vertical bars) in the prediction of scores on subsets of the Knee Injury and Osteoarthritis Outcome Score (KOOS) questionnaire (Pain, Symptoms, Quality of Life [QOL], Activities of Daily Living [ADL], Sport/Recreation [Sport]) and on the stair-climbing test (SCT). Asterisk indicates that the addition of the independent variable to the regression yielded a significant change in the R2 value at P<.05. Med Lax=medial laxity, IKOS score=self-reported knee instability score, MVIC=normalized maximal voluntary isometric contraction of quadriceps femoris muscle.
Discussion
In people with medial knee OA, the aims of our study were: (1) to investigate the relationship between self-reported knee instability and medial knee laxity, varus alignment, and quadriceps femoris muscle force; (2) to compare the level of function of participants classified by reports of knee instability; and (3) to investigate the influences of self-reported knee instability, medial laxity, varus alignment, and quadriceps femoris muscle force on function. The results show that self-reported knee instability is not related to medial knee laxity, mechanical axis, or quadriceps femoris muscle force. The results also demonstrate that function is worse in individuals who report worse knee instability and that function scores are predicted by self-reported knee instability, not laxity, even after accounting for the contribution of quadriceps femoris muscle force. This study is one of the few to investigate self-reported knee instability in patients with knee OA, and our findings suggest that further investigation of the causes and impact of self-reported knee instability is warranted.
“Instability” is a term often used clinically to describe the symptom of buckling, shifting, or giving way of a joint, such as the knee.43 Instability is a sensation experienced by the patient during dynamic activities, and, in order to evaluate its presence, clinicians rely on patient reports of buckling, shifting, or giving way. In the biomedical literature, the term “instability” often is used interchangeably with the term “laxity”; however, their meanings are not the same. Laxity represents a clinical sign that describes the condition of passive joint structures43 and is assessed in a static position using an arthrometer or stress device. A positive finding of increased knee laxity leads many clinicians to presume functional instability; however, prior to this study, this relationship had not been investigated in people with knee OA. Our results show no direct relationship between medial laxity and self-reported knee instability. Furthermore, our results show that the amount of medial knee laxity is similar between people reporting knee instability and those without knee instability.
Self-reported knee instability, or knee buckling, has been identified only recently as a significant factor in people with knee OA,26–28 so studies of the mechanisms underlying knee instability have only just begun. Factors such as increased BMI, ligament laxity, diminished muscle control, and structural joint changes could contribute to sensations of knee instability, hence our inclusion of these measures in our work. Our results show no differences among the self-reported knee instability groups in terms of medial laxity, quadriceps femoris muscle strength, or tibiofemoral joint alignment. Furthermore, our data showed no direct relationships between severity of self-reported knee instability and medial laxity, quadriceps femoris muscle force, or alignment. These findings are in contrast to the findings of Felson et al,26 who showed that quadriceps femoris muscle weakness and knee pain predicted knee buckling in people over age 50 years. It is possible that our sample size limited the detection of differences in quadriceps femoris muscle force, medial laxity, or tibiofemoral alignment among the instability groups. However, the study by Felson et al included individuals with and without radiographic evidence of knee OA, so it is possible that different factors may predict knee buckling in people with OA. It also is likely that self-reported knee instability is a multifactorial problem, and further investigation of underlying mechanisms is warranted.
In our recent work in patients with medial knee OA, we identified self-reported knee instability as an important predictor of movement and muscle activation patterns during walking activities.28,44 In the present study, our results show that self-reported knee instability is also an important predictor of function. We found that self-reported knee instability significantly influenced function even after accounting for variables (ie, laxity, alignment, quadriceps femoris muscle strength) that previously had been associated with decreased function and disability.8,11,12,29 We utilized the KOOS questionnaire to measure function because each subset (Pain, Symptoms, ADL, Sport, and QOL) is evaluated as an independent score. In our sample, individuals with the worse self-reported knee instability (If group) scored worse on all 5 subsets. Clinically meaningful score changes for the KOOS subsets have not been established. However, clinically meaningful score changes have been reported to be 9.7, 9.3, and 10.0 mm for the WOMAC pain, physical function, and stiffness subscales, respectively.45 Given the close association between the KOOS and the WOMAC, our results indicate that the difference in scores between the self-reported knee instability groups (range=10–27 points) represent clinically meaningful differences in function and quality of life.
Our findings are consistent with those of Fitzgerald et al,27 who reported that a large percentage of people with medial tibiofemoral, lateral tibiofemoral, and patellofemoral OA report knee instability that influences function beyond pain, range of motion, and weakness. Similarly, Felson et al26 reported that people who experienced knee buckling had higher disability scores on the WOMAC questionnaire independent of pain, weakness, age, and BMI. Our findings, along with those of Felson et al26 and Fitzgerald et al27 strongly indicate that self-reported knee instability, or buckling, is an important factor in people with knee OA. The collective findings signify the importance of assessing and addressing self-reported knee instability in people with knee OA in order to maximize functional outcomes. Felson et al26 recommended that knee buckling be included in the list of common symptoms in people with knee problems or OA in medical and rheumatology textbooks.
In this study, participants were classified based on reports of knee instability during activities of daily living, so it is not surprising that the If group scored worse on the ADL and Sport subsets of the KOOS questionnaire or that self-reported knee instability was involved in the prediction of these scores. We defined self-reported knee instability as a sensation of “shifting, buckling, or giving way” of the knee,31 and none of these items are addressed by any dimension of the KOOS. Therefore, although both instability and function were evaluated with self-report measures, we assert that items assessed by the KOOS are separate and independent from our measure of knee instability and that group differences in function measured by the KOOS subsets are meaningful. We used the SCT as a performance-based measure of function. Although small, self-reported knee instability scores significantly contributed to SCT scores even after accounting for the large influence of quadriceps femoris muscle force. The If group took approximately 4 seconds longer to complete the task compared with those participants without self-reported knee instability (I0 group), but this difference was not statistically significant. There are a number of performance-based measures of function available to clinicians that were not used in this study, and further investigation is needed to understand the impact of knee instability on performance-based measures of function.
Declines in function in people with knee OA have been attributed to both frontal-plane laxity and knee alignment.14,29 However, we did not find any relationship between medial laxity or varus alignment with any measure of function. Several methodological differences may explain the varying results. Work by Sharma and colleagues14 showed that total frontal-plane laxity was related to decreased function in individuals with medial tibiofemoral, lateral tibiofemoral, and patellofemoral OA. In the present study, we included only individuals with medial tibiofemoral OA, so the more homogeneous sample may have influenced the ability to find a relationship between frontal-plane laxity and knee function. We measured laxity using stress radiographs during which we applied a 150-N force to the knee joint line with the knee flexed approximately 20 degrees and the femur and tibia stabilized in a TELOS device. Sharma et al14 used a custom-designed device that stabilized the thigh, and they produced varus-valgus motion by applying a 40-N force to the foot, which may have resulted in different frontal-plane laxity measurements. In the present study and in the study by Lewek et al,46 stress radiographs were used to allow the medial and lateral sides of the joint to be assessed separately. It often is presumed that excessive frontal-plane motion is the result of ligament strain on the lateral side of the joint and cartilage erosion on the medial side. Lewek et al46 demonstrated, however, that lateral laxity is no different in people with medial knee OA, whereas medial laxity is greater than that in age and sex-matched control subjects. It is important to identify the source of increased frontal-plane motion in this patient population.
In our sample, those participants who reported knee instability (Im and If groups) reported worse knee symptoms, such as clicking/grinding and swelling, than those who never experience knee instability. This finding may suggest that patients with worse instability also have more-severe OA, based on clinical presentation. Clinical severity of knee OA does not always correlate with radiographic severity of the disease, and we did not find any differences among the groups in terms of frequency of radiographic severity of OA. However, joint instability can be associated with higher shear forces in the knee that are particularly damaging to articular cartilage.47,48 Longitudinal investigations with larger sample sizes are necessary to further understand the relationship between self-reported knee instability and joint integrity.
Our sample was inclusive of individuals with only medial knee OA of an idiopathic origin. We do not know whether the disease course of idiopathic (or primary) OA differs from that of secondary OA, so we excluded those individuals who reported a history of a possible ligament injury in order to ensure a more homogeneous sample. Idiopathic knee OA is more prevalent in women49; however, this was not reflected in the distribution of men and women in our sample. Our inclusion of individuals with only medial knee OA may have altered the expected distribution of male and female participants. Although the exact nature of self-reported knee instability in this patient population is unknown, we chose to exclude potential participants with patellofemoral joint disease in order to limit the possibility of instability arising from the patellofemoral joint. Despite the homogeneity of our sample, these findings may provide insight into the influence of self-reported knee instability for individuals with knee OA in other or multiple compartments.
Conclusion
This study showed that in people with medial knee OA, self-reported knee instability is a problem that does not have a direct association with medial laxity, quadriceps femoris muscle weakness, and varus alignment. In addition, self-reported knee instability can influence function over and above that explained by laxity, weakness, and malalignment. We acknowledge that there are several other factors that may contribute to function that were not included in this study. Although our work is preliminary, the findings indicate that self-reported knee instability, or the factors that contribute to knee instability, may need to be addressed in rehabilitation of people with medial knee OA in order to maximize function. We have shown that self-reported knee instability significantly influences movement and muscle activation patterns during walking activities.28,44 Further investigation of self-reported knee instability and neuromuscular control of the knee may expound the multifactorial nature of self-reported knee instability. Further investigation also is necessary to reproduce these findings with larger sample sizes and to evaluate the long-term consequences of self-reported knee instability on joint integrity.
Supplementary Material
Dr Schmitt, Dr Fitzgerald, and Dr Rudolph provided concept/idea/research design. Dr Schmitt and Dr Rudolph provided writing and data analysis. Dr Schmitt provided data collection. Dr Rudolph provided project management, fund procurement, and facilities/equipment. Dr Reisman provided participants. Dr Fitzgerald and Dr Reisman provided consultation (including review of manuscript before submission). The authors acknowledge Papastavros Medical Imaging for assistance with radiographs and Michael Axe, MD, for assistance with participant recruitment.
This research, in part, was presented at the Combined Sections Meeting of the American Physical Therapy Association; February 1–5, 2006; San Diego, California.
This research was funded by grant P20-RR016458 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), by NIH grant T32-HD007490, and by Foundation for Physical Therapy Promotion of Doctoral Studies II (PODS II) Awards (2004-2005, 2005-2006).
Austin & Associates, 1109 Sturbridge Rd, Fallston, MD 21047.
Isokinetic International, 6426 Morning Glory Dr, Harrison, TN 37341.
ConMed Corp, 525 French Rd, Utica, NY 13502.
Grass Instrument Division, Astro-Med Inc, 600 East Greenwich Ave, West Warwick, RI 02893.
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
References
- 1.Kannus P, Järvinen M, Kontiala H, et al. Occurrence of symptomatic knee osteoarthrosis in rural Finland: a prospective follow-up study. Ann Rheum Dis. 1987;46:804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Felson DT, Zhang Y, Hannon MT, et al. Risk factors for incident radiographic knee osteoarthritis in the elderly: the Framingham Study. Arthritis Rheum. 1997;40:728–733. [DOI] [PubMed] [Google Scholar]
- 3.McAlindon TE, Wilson PW, Aliabadi P, et al. Level of physical activity and the risk of radiographic and symptomatic knee osteoarthritis in the elderly: the Framingham Study. Am J Med. 1999;106:151–157. [DOI] [PubMed] [Google Scholar]
- 4.Carmona, L, Ballina J, Gabriel R, et al. The burden of musculoskeletal diseases in the general population of Spain: results from a national survey. Ann Rheum Dis. 2001;60:1040–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghosh P, Smith M. Osteoarthritis, genetic and molecular mechanisms. Biogerontology. 2002;3:85–88. [DOI] [PubMed] [Google Scholar]
- 6.Dawson J, Linsell L, Zondervan K, et al. Epidemiology of hip and knee pain and its impact on overall health status in older adults. Rheumatology (Oxford). 2004;43:497–504. [DOI] [PubMed] [Google Scholar]
- 7.Mannoni A, Briganti MP, Di Bari M, et al. Epidemiological profile of symptomatic osteoarthritis in older adults: a population based study in Dicomano, Italy. Ann Rheum Dis. 2003;62:576–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas RH, Resnik D, Alazraki NP, et al. Compartmental evaluation of osteoarthritis of the knee: a comparative study of available diagnostic modalities. Radiology. 1975;116:585–594. [DOI] [PubMed] [Google Scholar]
- 10.Dearborn JT, Eakin CL, Skinner HB. Medial compartment arthrosis of the knee. Am J Orthop. 1996;25:18–26. [PubMed] [Google Scholar]
- 11.McAlindon TE, Cooper C, Kirwan JR, Dieppe PA. Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis. 1993;52:258–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steultjens MP, Dekker J, van Baar ME, et al. Range of joint motion and disability in patients with osteoarthritis of the knee or hip. Rheumatology (Oxford). 2000;39:955–961. [DOI] [PubMed] [Google Scholar]
- 13.Miller ME, Rejeski WJ, Messier SP, Loeser RF. Modifiers of change in physical functioning in older adults with knee pain: the Observational Arthritis Study in Seniors (OASIS). Arthritis Rheum. 2001;45:331–339. [DOI] [PubMed] [Google Scholar]
- 14.Sharma L, Hayes KW, Felson DT, et al. Does laxity alter the relationship between strength and physical function in knee osteoarthritis? Arthritis Rheum. 1999;42:25–32. [DOI] [PubMed] [Google Scholar]
- 15.Wada M, Imura S, Baba H, Shimada S. Knee laxity in patients with osteoarthritis and rheumatoid arthritis. Br J Rheumatol. 1996;35:560–563. [DOI] [PubMed] [Google Scholar]
- 16.Sharma L, Lou C, Felson DT, et al. Laxity in healthy and osteoarthritic knees. Arthritis Rheum. 1999;42:861–870. [DOI] [PubMed] [Google Scholar]
- 17.Sharma L, Dunlop DD, Cahue S, et al. Quadriceps strength and osteoarthritis progression in malaligned and lax knees. Ann Intern Med. 2003;138:613–619. [DOI] [PubMed] [Google Scholar]
- 18.Lephart SM, Perrin DH, Fu FH, et al. Relationship between selected physical characteristics and functional capacity in the anterior cruciate ligament-insufficient athlete. J Orthop Sports Phys Ther. 1992;16:174–181. [DOI] [PubMed] [Google Scholar]
- 19.Ciccotti MG, Lombardo SJ, Nonweiler B, Pink M. Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients: results after long-term follow-up. J Bone Joint Surg Am. 1994;76:1315–1321. [DOI] [PubMed] [Google Scholar]
- 20.Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31:210–215. [DOI] [PubMed] [Google Scholar]
- 21.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physically active individuals. Phys Ther. 2000;80:128–140. [PubMed] [Google Scholar]
- 22.Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. 1998 Basmajian Student Award Paper: movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8:349–362. [DOI] [PubMed] [Google Scholar]
- 23.Rudolph KS, Axe MJ, Buchanan TS, et al. Dynamic stability in the anterior cruciate ligament deficient knee. Knee Surg Sports Traumatol Arthrosc. 2001;9:62–71. [DOI] [PubMed] [Google Scholar]
- 24.Chmielewski TL, Rudolph GK, Fitzgerald GK, et al. Biomechanical evidence supporting a differential response to acute ACL injury. Clin Biochem (Bristol, Avon). 2001;16:586–591. [DOI] [PubMed] [Google Scholar]
- 25.Chmielewski TL, Hurd WJ, Rudolph KS, et al. Perturbation training improves knee kinematics and reduces muscle co-contraction after complete unilateral anterior cruciate ligament rupture. Phys Ther. 2005;85:740–749; discussion 750–754. [PubMed] [Google Scholar]
- 26.Felson DT, Niu J, McLenna C, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147:534–540. [DOI] [PubMed] [Google Scholar]
- 27.Fitzgerald GK, Piva SR, Irrgang JJ. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. 2004;51:941–946. [DOI] [PubMed] [Google Scholar]
- 28.Schmitt LC, Rudolph KS. Influences on knee movement strategies during walking in persons with medial knee osteoarthritis. Arthritis Rheum. 2007;57:1018–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharma L, Song J, Felson DT, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. [DOI] [PubMed] [Google Scholar]
- 30.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Irrgang JJ, Snyder-Mackler L, Wainner RS, et al. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80:1132–1145. [DOI] [PubMed] [Google Scholar]
- 32.Lewek MD. Knee Malalignment and the Progression of Knee Osteoarthritis. Newark, DE: University of Delaware; 2003.
- 33.Tubach F, Ravaud P, Baron G, et al. Evaluation of clinically relevant changes in patient reported outcomes in knee and hip osteoarthritis: the minimal clinically important improvement. Ann Rheum Dis. 2005;64:29–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roos EM, Roos HP, Lohmander LS, et al. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 35.Roos EM, Lohmander LS. The Knee Injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liang MH, Larson MG, Cullen KE, Schwartz JA. Comparative measurement efficiency and sensitivity of five health status instruments for arthritis research. Arthritis Rheum. 1985;28:542–547. [DOI] [PubMed] [Google Scholar]
- 37.Rejeski WJ, Ettinger WH Jr, Schumaker S, et al. Assessing performance-related disability in patients with knee osteoarthritis. Osteoarthritis Cartilage. 1995;3:157–167. [DOI] [PubMed] [Google Scholar]
- 38.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop. 1990;(255):215–227. [PubMed] [Google Scholar]
- 39.Chao EY, Neluheni EV, Hsu RW, Paley D. Biomechanics of malalignment. Orthop Clin North Am. 1994;25:379–386. [PubMed] [Google Scholar]
- 40.Tetsworth K, Paley D. Malalignment and degenerative arthropathy. Orthop Clin North Am. 1994;25:367–377. [PubMed] [Google Scholar]
- 41.Moore TM, Meyers MH, Harvey JP Jr. Collateral ligament laxity of the knee: long-term comparison between plateau fractures and normal. J Bone Joint Surg Am. 1976;58:594–598. [PubMed] [Google Scholar]
- 42.Kent-Braun JA, Le Blanc R. Quantitation of central activation failure during maximal voluntary contractions in humans. Muscle Nerve. 1996;19:861–869. [DOI] [PubMed] [Google Scholar]
- 43.Noyes FR, Grood ES, Torzilli PA. Current concepts review: the definitions of terms for motion and position of the knee and injuries of the ligaments. J Bone Joint Surg Am. 1989;71:465–472. [PubMed] [Google Scholar]
- 44.Schmitt LC, Rudolph KS. Muscle stabilization strategies in people with medial knee osteoarthritis: the effect of instability. J Orthop Res. 2008;26:1180–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ehrich EW, Davies GM, Watson DJ, et al. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities Osteoarthritis Index Questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000;27:2635–2641. [PubMed] [Google Scholar]
- 46.Lewek MD, Rudolph KS, Snyder-Mackler L. Control of frontal plane knee laxity during gait in patients with medial compartment knee osteoarthritis. Osteoarthritis Cartilage. 2004;12:745–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Setton LA, Mow VC, Howell DS. Mechanical behavior of articular cartilage in shear is altered by transection of the anterior cruciate ligament. J Orthop Res. 1995;13:473–482. [DOI] [PubMed] [Google Scholar]
- 48.Wu JZ, Herzog W, Epstein M. Joint contact mechanics in the early stages of osteoarthritis. Med Eng Phys. 2000;22:1–12. [DOI] [PubMed] [Google Scholar]
- 49.Srikanth VK, Fryer JL, Zhai G, et al. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769–781. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.