Abstract
Background and Objectives: Few studies have examined the effectiveness of pelvic-floor muscle (PFM) exercises to reduce female stress urinary incontinence (SUI) over the long term. This study: (1) evaluated continence and quality-of-life outcomes of women 6 months following formalized therapy and (2) determined whether low- and high-frequency maintenance exercise programs were equivalent in sustaining outcomes.
Subjects and Methods: Thirty-six women with SUI who completed an intensive PFM exercise intervention trial were randomly assigned to perform a maintenance exercise program either 1 or 4 times per week. Urine leaks per week, volume of urine loss, quality of life (Incontinence Impact Questionnaire [IIQ] score), PFM strength (Brink score), and prevalence of urodynamic stress incontinence (USI) were measured at a 6-month follow-up for comparison with postintervention status. Parametric and nonparametric statistics were used to determine differences in outcome status over time and between exercise frequency groups.
Results: Twenty-eight women provided follow-up data. Postintervention status was sustained at 6 months for all outcomes (mean [SD] urine leaks per week=1.2±2.1 versus 1.4±3.1; mean [SD] urine loss=0.2±0.5 g versus 0.2±0.8 g; mean [SD] IIQ score=17±20 versus 22±30; mean [SD] Brink score=11±1 versus 11±1; and prevalence of USI=48% versus 35%). Women assigned to perform exercises once or 4 times per week similarly sustained their postintervention status.
Discussion and Conclusions: Benefits of an initial intensive intervention program for SUI were sustained over 6 months. However, only 15 of the 28 women provided documentation of their exercise adherence, limiting conclusions regarding the need for continued PFM exercise during follow-up intervals of ≤6 months.
Since the introduction of Kegel exercises in 1948,1 the efficacy of pelvic-floor muscle (PFM) exercise in the management of stress urinary incontinence (SUI) and mixed urinary incontinence (UI) (symptoms of stress and urge incontinence) has been supported by multiple randomized controlled studies and systematic reviews.2–7 Pelvic-floor muscle exercise has been reported to be 50% to 69% effective in reducing urine loss episodes in women.4,5,7,8 Conversely, results of studies that tested the long-term success rates of PFM exercise to manage UI are mixed.9–13 Unfortunately, these studies applied different exercise frequency and duration prescriptions, making it difficult to draw clinically relevant conclusions about how to enhance the long-term efficacy of PFM exercise for SUI.
Poor exercise adherence is recognized as a serious threat to long-term success in the management of UI. Several studies9,10,14,15 have shown that women decrease the frequency of PFM exercise over time. One study9 showed that 5 years following a 6-month program of intensive PFM strengthening, 70% of the women continued their exercise program at least 1 time per week. However, women who exercised 3 or more times per week demonstrated significantly less incontinence, as determined by pad test, compared with those who exercised less frequently.9 A 15-year follow-up study of the same women showed that only 28% performed PFM exercises at least weekly.10 In addition, 50% of the women underwent anti-incontinence surgery at some point during the 15-year follow-up period.10 In a study by Holley et al,14 1 out of 10 women continued to exercise 5 years after formalized therapy. The woman who continued to exercise reported decreased UI, whereas the other women demonstrated no improvement or underwent surgery.14 The results of these studies suggest that the initial benefits of a formalized rehabilitation program for UI diminish due to a reduction in exercise adherence.
Much effort has been taken to determine variables influencing a patient's ability to adhere to prescribed interventions. The inconvenience of the regimen14,16–19 is particularly applicable to exercise adherence. Women in the study by Holley et al14 cited not having enough time, a lack of discipline or disinterest in exercising, and interference with daily activities as reasons why they failed to exercise. Similar reasons for poor PFM exercise adherence were obtained from a study of postnatal women surveyed 1 year following a formalized PFM exercise program.13 The exercise program consisted of 8 to 10 PFM contractions, 8 to 10 times per day. The investigators speculated that the high exercise intensity (number of exercise repetitions) and frequency may have accounted for the poor exercise adherence and study withdrawal observed.13 A 5-year follow-up to a controlled PFM exercise trial for UI that initially required women to perform 10 PFM contractions, 5 to 10 times per day, also showed poor long-term adherence. Of the women diagnosed with SUI, only 39% performed exercises at least once per day or “when needed.” Fifteen percent performed exercises once per week, with 3% performing them once per month and 43% not at all.11 Again, the intensity of the exercise prescription may have contributed to the overall poor long-term adherence. Interestingly, the authors also noted that exercise adherence was the only significant factor (compared with variables such as age, parity, health locus of control, and severity of incontinence) that was shown to influence outcomes at the 5-year follow-up.
It is important to note that the PFM exercise intervention trials20,21 upon which the aforementioned follow-up studies9,10,11 were based did not describe whether or how women were advised to continue PFM exercises long-term. Thus, it is not known whether a specific prescribed PFM maintenance program would have enhanced long-term PFM exercise outcomes.
When prescribing maintenance PFM exercise, the physical therapist needs to consider the burden of exercise placed on the patient. To minimize this burden, the therapist would need to know the specific parameters of exercise (eg, type, number of repetitions, performance frequency) for producing the most efficacious outcome, as demonstrated by research. This information is difficult to obtain from the current literature. In published studies,22–26 the suggested exercise frequency varies from 3 or more times per day to 3 times per week. More variable is the number of exercise repetitions, from a reported 15 to 30 repetitions to 100 or more repetitions per day.22–26 Given the evidence of poor long-term PFM adherence, a research priority should be to determine the minimum exercise frequency and number of PFM exercise repetitions needed to maintain benefits of a formalized PFM exercise program.
There is evidence in the literature on muscle strengthening that the exercise frequency needed to preserve muscle strength (force-generating capacity) may be less than what is typically prescribed by the physical therapist. Graves et al27 demonstrated that reducing exercise frequency from 2 or 3 times per week to once per week afforded maintenance of knee extensor strength as long as the mode, intensity, and duration of exercise were held constant. Carpenter and colleagues28,29 demonstrated maximal isometric strength gains in lumbar extension during the first 12 weeks of training with continued training once per week or every other week as sufficient to preserve strength gains. Similar results have been shown for aerobic capacity gains.30 Whether the results of these studies can be generalized to the rehabilitation of PFMs is unknown.
Thus, given that the literature supports the efficacy of continued exercise to maintain long-term gains in decreasing UI,9,11,12 it becomes evident that further research is needed to prospectively evaluate the minimum exercise frequency essential to maintain PFM function following a formalized rehabilitation program. If reducing exercise frequency does not result in loss of function, then a potential benefit of reducing exercise demands could be enhanced long-term exercise adherence.
We previously published continence and quality-of-life (QOL) outcomes for 44 women who participated in a 9- to 12-week supervised PFM exercise program for SUI.8 The aims of the present study were: (1) to evaluate continence and QOL outcomes for these women 6 months following discharge from formalized therapy and (2) to compare the effectiveness of low-frequency (1 time per week) and high-frequency (4 times per week) PFM maintenance exercise programs on sustaining treatment outcomes over a 6-month follow-up period. We hypothesized that low- and high-frequency exercise would be equally effective in maintaining therapeutic gains over the 6-month follow-up period.
Method
Participants
Data for this study came from the 6-month postintervention examinations of women who completed a 9- to 12-week randomized intervention trial to determine the effect of PFM exercise position (supine only versus supine and upright) on continence and QOL outcomes.8 Women for the intervention trial were recruited through local newspaper advertisements, the Magee-Womens Research Institute Web site, and physician referrals from the Department of Obstetrics, Gynecology, and Reproductive Science at the University of Pittsburgh at Magee-Womens Hospital.
Women were eligible for the study if they were 38 to 70 years of age, not pregnant, ambulatory, and recorded at least one SUI episode and no urgency or urge urinary incontinence (UUI) in a 7-day bladder diary. Women were excluded from participation if they had a medical history that included pelvic cancer, severe endometriosis, use of an intrauterine device, or pacemaker; neurologic or metabolic disorders associated with bladder or sphincter dysfunction; previous medical/surgical treatments for SUI; or prior instruction in PFM exercise or a prescribed PFM exercise regimen from a physician, nurse, physical therapist, or other health care professional. Exclusion based on physical examination occurred if women had vaginal wall prolapse beyond the vaginal introitus, an inability to demonstrate a palpable PFM contraction, sensory loss below the L4 dermatome, atrophic vaginitis or skin breakdown around the perineum, lumbosacral or pelvic pain or dysfunction that would interfere with PFM exercises, or an inability to tolerate the supine position for exercise or if they demonstrated detrusor instability or an abdominal leak point pressure of less than 60 cm H2O during urodynamic testing. Additional details of participant eligibility, screening, and randomization have been reported previously.8
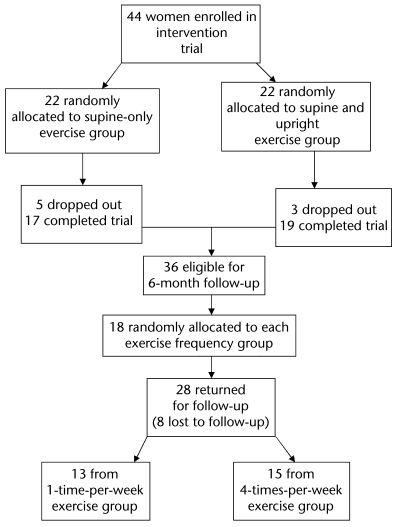
Forty-four women, with a mean age of 52.6 years (SD=8.5), enrolled in the 9- to 12-week intervention trial. Fifty-seven percent of this sample was post-menopausal, and their mean number of urine leaks per week recorded in their preintervention bladder diaries was 7.0 (SD=6.2). Thirty-six (82%) of these women completed the 9- to 12-week intervention trial (Figure).8
Figure.
Flow of participants through initial pelvic-floor muscle exercise intervention trial and 6-month follow-up study.
We telephoned all of the women who completed the intervention trial to participate in the 6-month follow-up. Twenty-eight women (78% who completed the intervention trial) returned for the 6-month follow-up. Reasons why women did not participate in the follow-up included: new, unrelated illness (1 woman); moved away from area (1 woman); unable to find time to participate (4 women); and did not return the investigators’ telephone calls (2 women). A t test for unequal variances assured us that there was no difference in the mean (SD) percentage reduction of SUI episodes achieved during the intervention trial between women who returned and those who did not return for the 6-month follow-up (81.0±29.0% versus 51.0±42.0%, respectively; t=1.76, P=.12).
Complete bladder diary data were obtained from all 28 participants. We obtained a complete set of bladder diary, QOL, urodynamic, pad test, and PFM strength data from 23 women. Of the remaining 5 subjects, 1 attended the reexamination but refused urodynamic testing, thus contributing only bladder diary, QOL, and PFM strength data to the study. Another 4 women were unwilling to return for the physical reexamination but agreed to mail a completed bladder diary and QOL questionnaire to the principal investigator. Therefore, bladder diary and QOL data were obtained from all 28 women, PFM strength data were obtained from 24 women, and urine leakage data from the urodynamic and pad tests were obtained from 23 women.
Randomization to Exercise Frequency Groups
During the intervention trial, women had been randomly assigned to use 1 of 2 positions (supine only versus supine and upright) for PFM exercise.8 At the last physical therapy visit (during the 9- to 12-week intervention phase), women were randomly assigned to participate in either a low-frequency (1 time per week) or a high-frequency (4 times per week) maintenance exercise program. A block randomization schedule was determined using a random number table. Four blocks with 12 assignments each that included equal representation of both exercise positions and exercise frequencies were created. Random assignment followed the block schedule when the groups became unbalanced on age or incontinence severity. We aimed to keep the groups similar on age (within 5 years) and incontinence severity. Incontinence severity was determined from the baseline bladder diary as minimal (<5 urine leakage episodes per week), moderate (5–10 urine leakage episodes per week), or severe (>10 urine leakage episodes per week).
During the study's intervention phase, the maximum number of PFM exercises prescribed was 60 repetitions (3 sets of 20 repetitions) of a 3-second PFM contraction and 30 repetitions (3 sets of 10 repetitions) of a 12-second contraction per exercise session. The women were told to perform 2 exercise sessions per day.8 The number of PFM exercises prescribed depended on the maximal exercise prescription a woman achieved at the final intervention visit. Depending on the exercise frequency assignment, the women were told to perform 1 session of exercise 1 time per week or 4 times per week.
6-Month Examination Outcomes
All participants provided informed consent to examination procedures. A nurse practitioner and a physical therapist examined all participants. Six-month study outcomes included number of urine leakage episodes recorded in a bladder diary, evidence of urine leakage during urodynamic testing, volume of urine loss during a pad test, QOL, and PFM strength. These outcomes also were obtained previously for each participant at the end of the 9- to 12-week physical therapy intervention. Data from the postintervention and 6-month follow-up examinations were compared to determine any changes in incontinence status and QOL over the maintenance period.
Bladder diary.
Participants were mailed a 1-week bladder diary prior to the 6-month examination and asked to complete it the week prior to their appointment. The 1-week urinary diary has been shown to have high test-retest reliability for diurnal and nocturnal micturition frequency and number of incontinence episodes (r=.86-.91).31 The women recorded the time of each void and incontinence episode and the circumstance of each stress incontinence episode (eg, cough, sneeze). The number of incontinence episodes per week was extracted from the diary.
Urine leakage during urodynamic testing.
The nurse practitioner performed all urodynamic evaluations. Urodynamic evaluations with external water pressure transducers were performed using the EKO Urodynamics System,* a no. 7 French double lumen urethral catheter,† and a rectal balloon catheter‡ to measure intra-abdominal pressure. Post-void residual urine was removed through the urodynamic catheter prior to bladder filling. Transducers were zeroed for each participant. Post-void residual urine was documented by catheterization within 15 minutes of voiding. The bladder was retrograde filled with room-temperature sterile water at a continuous rate of 50 mL/min. Bladder filling stopped when the participant reported a strong urge to urinate, indicating maximal cystometric capacity. Any evidence of detrusor instability was recorded. Once maximal cystometric capacity was reached, the bladder catheter was removed and provocative stress maneuvers (Valsalva maneuver followed by cough) were performed. Provocative maneuvers were done first with the participant in a lithotomy position. If leakage did not occur, provocative maneuvers were repeated in a standing position. Evidence of SUI and the coincident abdominal leakpoint pressure were recorded.
Volume of urine leakage.
A modification of the 1-hour pad test recommended by the International Continence Society was used to quantify volume of urine leakage.32 We administered the pad test immediately following urodynamic testing; therefore, we assumed the participant's bladder was still at maximum cystometric capacity. At the time of testing, the woman was not menstruating and any lubricant used for urodynamic testing was removed. A calibrated Ohaus model CR 1200 Portable Advanced Scale§ was used to weigh the Depend Undergarment‖ before and after the pad test. The readability of the scale is 0.1 g, and its repeatability is 0.1 g. Participants wore the pad during the following standardized maneuvers, walking 45 m (50 yd) at a comfortable pace, followed by 5 times each of climbing a step, coughing, heel bouncing, and standing up from a sitting position. Finally, the women placed their hands under running water for 1 minute. The undergarment was removed and weighed to determine volume of urine loss.
QOL.
Quality of life was measured using the Incontinence Impact Questionnaire (IIQ).33 The IIQ is a 30-item questionnaire designed to assess the impact of UI across 4 domains: physical activity, travel, social relationships, and emotional health. Internal consistency, reproducibility, construct validity, and sensitivity of the IIQ were established in a population of community-dwelling women with SUI or UUI.33 Participants completed the IIQ at the baseline and posttreatment examinations. Scores on the IIQ range from 0 to 400, with a higher score indicating poor perceived QOL.33
PFM strength.
The PFM strength grade was determined through digital assessment using the Brink method.34 The Brink scale considers 3 muscle function dimensions: muscle contraction duration, squeeze pressure felt around the examiner's fingers, and vertical displacement of the examiner's fingers as the PFMs contract. Each variable is rated separately on a 4-point categorical scale. The 3 subscale scores are summed to obtain a composite score ranging from a low of 3 to a high of 12. Interrater reliability, test-retest reliability, and validity of this strength assessment have been reported.34,35
Exercise adherence.
The women were provided a diary to record exercise adherence during the 6-month follow-up interval. They received the diary at the last intervention visit. To minimize patient burden, the diary only required the women to indicate the number of exercise sessions they performed per week over the 6-month interval.
Data Analysis
To determine whether differences existed at the time of randomization to exercise frequency groups, we compared groups on age, number of urine leaks per week, and volume of urine loss during the pad test using independent t tests. Mann-Whitney U tests were performed to determine group differences in IIQ and Brink scores. Group differences in the proportion of women in each exercise group who experienced urine leakage during cystometric testing at the time of randomization were analyzed using chi-square analysis.
To determine long-term changes in outcome status across the entire sample (study aim 1), data from both exercise frequency groups were collapsed. Changes in the number of urine leaks per week and volume of urine loss during the pad test were analyzed using paired t tests. Changes in IIQ and Brink scores were analyzed using the Wilcoxon signed rank test. The McNemar test was used to test the change in the distribution of women who did and did not leak urine during urodynamic testing.
The effect of maintenance exercise frequency on 6-month post-intervention outcomes (study aim 2) was determined by analyzing difference scores (postintervention – 6-month follow-up) for bladder diary, pad test, QOL, and PFM strength outcomes. A one-way analysis of variance (ANOVA) was used to detect differences between the 2 groups on reductions in the number of urine leaks per week and the amount of urine loss during the pad test. The Kruskal-Wallis one-way ANOVA by ranks was used to detect group differences in changes in IIQ and Brink scores. Group differences in the proportion of women who demonstrated urine leakage during cystometric testing were determined using chi-square analysis. When expected cell frequencies were <5, the Fisher exact test was used instead of the chi-square test.
Exercise adherence was determined from the exercise diaries. Only completed diaries were used in the analysis. A percentage of exercise adherence was calculated for each woman using the following formula: (number of actual exercise sessions performed/expected number of exercise sessions) × 100%.
Results
The mean age of the women who provided data for the 6-month follow-up (n=28) was 52.8 years (SD=8.6) (Figure). Median parity was 2, and 60.7% of the sample were postmenopausal. Twenty-six women were Caucasian, and 2 were African American. Thirteen women were randomly assigned to perform exercises once a week (low-frequency exercise group) at their last intervention visit, and 15 women were randomly assigned to perform exercises 4 times per week (high-frequency exercise group).
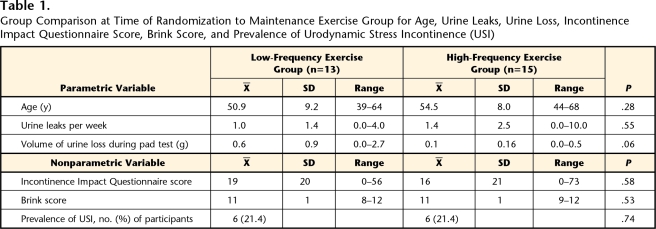
Group comparisons on study outcomes at the completion of the 9- to 12-week intervention (time of randomization to maintenance exercise group) are presented in Table 1. At randomization, there were no statistically significant differences between women assigned to either maintenance exercise group with respect to age, number of urine leaks per week, volume of urine loss during the pad test, IIQ scores, or Brink score.
Table 1.
Group Comparison at Time of Randomization to Maintenance Exercise Group for Age, Urine Leaks, Urine Loss, Incontinence Impact Questionnaire Score, Brink Score, and Prevalence of Urodynamic Stress Incontinence (USI)
Urodynamic stress incontinence (USI) was present in 60.7% of the women prior to the physical therapy intervention. Following intervention, only 42.8% of the women leaked urine during urodynamic testing, demonstrating USI. Table 1 shows that there was no difference in prevalence of USI between maintenance exercise groups at randomization (χ2=0.11, P=.74).
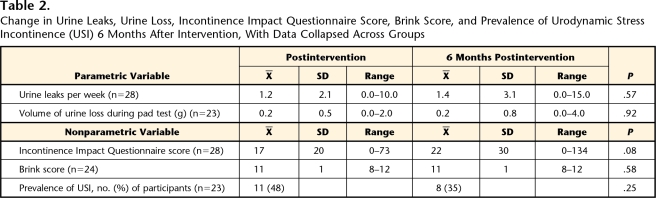
Table 2 shows the outcome results with data collapsed across all participants (regardless of exercise frequency group). Status of urine leaks, urine loss, and Brink scores were sustained over the 6-month follow-up period. Incontinence Impact Questionnaire scores worsened slightly over the 6-month period, but this change did not reach statistical significance. The percentage of women with USI at the 6-month follow-up decreased to 35%; however, this change was not statistically significant.
Table 2.
Change in Urine Leaks, Urine Loss, Incontinence Impact Questionnaire Score, Brink Score, and Prevalence of Urodynamic Stress Incontinence (USI) 6 Months After Intervention, With Data Collapsed Across Groups
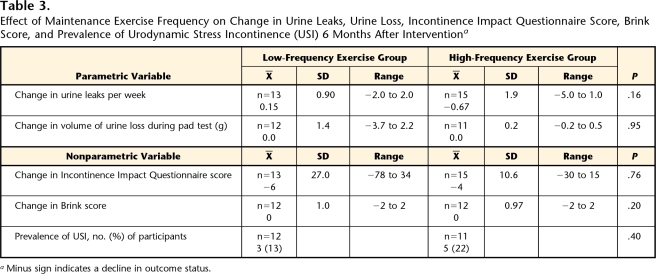
Changes in bladder diary, pad test, QOL, and PFM strength outcomes from postintervention to the 6-month follow-up examination are presented by maintenance exercise group in Table 3. Changes in the number of urine leaks per week, volume of urine loss during the pad test, IIQ scores, and Brink scores were quite small and not statistically different between the 2 maintenance exercise groups. Table 3 also shows the prevalence of USI at the 6-month examination by maintenance exercise group. The proportion of women who demonstrated USI was not statistically different between the groups (P=.40).
Table 3.
Effect of Maintenance Exercise Frequency on Change in Urine Leaks, Urine Loss, Incontinence Impact Questionnaire Score, Brink Score, and Prevalence of Urodynamic Stress Incontinence (USI) 6 Months After Interventiona
Minus sign indicates a decline in outcome status.
Only 15 women returned completed exercise adherence diaries at the 6-month follow-up examination. Seven of these women were assigned to the low-frequency exercise group, and 8 women were assigned to the high-frequency exercise group. Women in the low- and high-frequency exercise groups performed a median 83% (range=43%-100%) and 72% (range=0%-100%) of the expected exercise sessions during the 6-month follow-up period, respectively.
We obtained anecdotal information regarding exercise adherence from the remaining 13 women, including whether they exercised regularly over the 6-month period and, on average, how many times per week they exercised. We estimated their percentage adherence using the following formula: (recalled average exercise sessions per week × 26 weeks)/(expected number of exercise sessions per week × 26 weeks) × 100%. We estimated that these women performed a mean 39% (median=25%) of the expected exercises sessions during the 6-month follow-up, considerably less than the 15 women who returned exercise diaries.
Discussion
Our results showed that continence, QOL, and PFM strength gains obtained during an intensive PFM exercise program were sustained over a 6-month follow-up period in women with SUI who were advised to continue PFM exercise at a reduced exercise frequency. It is important to note that 15 (54%) of the women kept an exercise diary over the 6-month follow-up period. Of these women, only 4 indicated 100% adherence. Thus, based on the exercise diaries received, women exercised at a lower frequency than assigned. However, the women in the high-frequency exercise group exercised more than twice as often per week compared with the women in the low-frequency exercise group. Although less than prescribed, we believe adherence was quite good for these 15 women (median 83% and 72% for those assigned to exercise 1 and 4 times per week, respectively). Pizzari et al36 reported a median 75% adherence to prescribed home exercises for individuals following anterior cruciate ligament reconstructive surgery.
The inability to obtain a record of exercise adherence for 13 of the 28 women in this study was a major limitation. Using anecdotal data, we determined that these women exercised considerably less than the 15 women who kept an exercise diary. Therefore, we cannot be certain whether our 6-month outcomes can be attributed to continued exercise. We explored this concern through 2 additional statistical analyses. For the first analysis, we applied the assumption that the 13 women without a diary were “nonadherent” to PFM exercise and the 15 women who kept the diary were “adherent” to PFM exercise. We compared the 2 groups on the main study outcome: change in number or urine leaks per week (measured by bladder diary) over the 6-month period. Women in the adherent group had an increase of 0.4 (SD=1.5) leaks per week compared with a reduction of 0.15 (SD=0.8) leaks per week in the nonadherent group (t=1.19, P=.25). For the second analysis, we examined the association between adherence and change in urine leaks per week over the 6-month period in the 15 women who completed and returned the exercise diary. We did not find an association between adherence and bladder diary outcomes in this group (r=.01, P=.26).
Obtaining exercise adherence from a self-report diary presents another study limitation. Asking women to return the diaries monthly over the 6-month period may have increased the quantity of adherence data for analysis and provided stronger conclusions regarding the utility of continued exercise.
Further research is needed to establish whether continued PFM exercise at a reduced exercise frequency is needed to sustain outcomes beyond a period of 6 months following an intensive, individualized PFM exercise program. Longer-term studies9,10 have shown significant increases in incontinence following formalized physical therapy for SUI. Additionally, Chiarelli et al12 reported that the continued practice of PFM exercise at any frequency significantly improved the odds of being continent at 12 months postpartum in women who had undergone a previous intensive pelvic-floor exercise program. Whether the parameters of maintenance exercise intensity and frequency used in our study would sustain postintervention outcomes for periods greater than 6 months is unknown.
Additional risk factors for SUI over time, including aging, onset of menopause, use of medications, and disease, may lessen the long-term efficacy of PFM exercise.37 Although more than half of the women in our study were postmenopausal, only 1 woman reported a change in health status during the follow-up period. Thus, our study does not add insight into the impact of aging, menopause, or changing health on long-term adherence to and efficacy of maintenance PFM exercise.
Our study did not include women with severe incontinence or mixed incontinence, women with prior treatment failures, or women who had experienced poor or unsatisfactory outcomes from a PFM intervention program. At baseline (entrance to the 9- to 12-week intensive PFM exercise intervention), the women who participated in our intervention study had mild to moderate SUI (a mean of 7.0 [SD=6.2] urine leaks per week and a mean IIQ score of 55 [SD=53]), no urgency symptoms or urge incontinence, and no previous SUI treatment. Those who completed the 9- to 12-week intervention trial achieved a mean 78.8% reduction in urine leaks per week and reported improved QOL (mean=29 [SD=42] points on the IIQ).8 Therefore, we believe it is clinically significant that these women were able to sustain improved continence and UI-specific QOL over the 6-month period. Future investigations should examine whether continued PFM exercise is necessary for women with more-severe incontinence.
Another major limitation of this study was that it did not include a control group (a no-maintenance exercise group). Because the literature strongly indicates poor long-term continence outcomes along with inadequate PFM exercise adherence following formalized intervention,9–14 we could not justify inclusion of a control group. Future prospective investigations will need to weigh the benefits of including a control group to determine whether continued exercise is necessary and, if so, the critical exercise intensity threshold needed to sustain the benefits of PFM exercise beyond 6 months.
Conclusion
The effectiveness of pelvic-floor strengthening exercise in the management of SUI is well established. The most appropriate exercise prescription related to the maintenance of improved UI outcomes has not been established. Our results demonstrated sustained benefits of formalized physical therapy for SUI over a 6-month period. Because about half of the women poorly documented exercise adherence, we could not strongly conclude whether continued exercise contributed to the positive 6-month outcomes.
Dr Borello-France, Dr Downey, and Dr Zyczynski provided concept/idea/research design and writing. All authors provided data collection. Dr Borello-France provided data analysis and fund procurement. Dr Borello-France and Ms Rause provided project management. Dr Zyczynski and Ms Rause provided participants and facilities/equipment. Dr Borello-France, Dr Zyczynski, and Ms Rause provided institutional liaisons.
All study procedures were approved by the University of Pittsburgh and Duquesne University institutional review boards.
This research, in part, was presented at the Combined Sections Meeting of the American Physical Therapy Association; February 23–27, 2005; New Orleans, Louisiana.
This work was supported by the National Institutes of Health, National Institute on Aging (grant R15 AG15488-03), and by a Magee-Womens Health Foundation grant.
Laborie Medical Technologies, 310 Hurricane Ln, Williston, VT 05495.
Cook Urological Inc, 1100 W Morgan St, PO Box 227, Spencer, IN 47460.
Rusch Inc, 2917 Weck Dr, Durham, NC 27709.
Ohaus Corp, 19A Chapin Rd, PO Box 2033, Pine Brook, NJ 07058.
Kimberly-Clark Worldwide Inc, Texas Commerce Tower Bldg, Irving, TX 75062.
References
- 1.Kegel AH. Progressive resistance exercises in the functional restoration of the perineal muscles. Am J Obstet Gynecol. 1948;56:238–248. [DOI] [PubMed] [Google Scholar]
- 2.Burns PA, Pranikoff K, Nochajski TH, et al. A comparison of effectiveness of biofeedback and pelvic muscle exercise treatment of stress incontinence in older community-dwelling women. J Gerontol. 1993;48:M167–M174. [DOI] [PubMed] [Google Scholar]
- 3.Bø K, Talseth T, Holm I. Single blind, randomized controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in the management of genuine stress incontinence in women. BMJ. 1999;318:487–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henalla SM, Hutchins CJ, Robinson P, et al. Non-operative methods in the treatment of female genuine stress incontinence of urine. J Ob Gyn. 1989;9:222–225. [Google Scholar]
- 5.Goode P, Burgio KL, Locher JL, et al. Effect of behavioral training with or without pelvic floor electrical stimulation on stress incontinence in women: a randomized controlled trial. JAMA. 2003;290:345–352. [DOI] [PubMed] [Google Scholar]
- 6.Berghmans LCM, Hendriks HJM, Bø K, et al. Conservative treatment of stress urinary incontinence in women: a systematic review of controlled clinical trials. Br J Urol. 1998;82:181–191. [DOI] [PubMed] [Google Scholar]
- 7.Hay-Smith EJC, Dumoulin C. Pelvic floor muscle training versus no treatment, or inactive control treatments for urinary incontinence in women for urinary incontinence. Cochrane Database Syst Rev. 2007: 2.
- 8.Borello-France DF, Zyczynski HM, Downey PA, et al. Effect of pelvic-floor muscle exercise position on continence and quality-of-life outcomes in women with stress urinary incontinence. Phys Ther. 2006;86:974–986. [PubMed] [Google Scholar]
- 9.Bø K, Talseth T. Long-term effect of pelvic floor muscle exercise 5 years after cessation of organized training. Obstet Gynecol. 1996;87:261–265. [DOI] [PubMed] [Google Scholar]
- 10.Bø K, Kvarstein B, Nygaard I. Lower urinary tract symptoms and pelvic floor muscle adherence after 15 years. Obstet Gynecol. 2005;105(5 Pt 1):999–1005. [DOI] [PubMed] [Google Scholar]
- 11.Lagro-Janssen T, Van Weel C. Long-term effect of treatment of female incontinence in general practice. Br J Gen Pract. 1998;48:1735–1738. [PMC free article] [PubMed] [Google Scholar]
- 12.Chiarelli P, Murphy B, Cockburn J. Promoting urinary continence in postpartum women: 12-month follow-up data from a randomised control trial. Int Urogynecol J. 2004;15:99–105. [DOI] [PubMed] [Google Scholar]
- 13.Wilson P, Herbison G. A randomized controlled trial of pelvic floor muscle exercises to treat postnatal urinary incontinence. Int Urogynecol J. 1998;9:257–264. [DOI] [PubMed] [Google Scholar]
- 14.Holley R, Varner E, Kerns D, Mestecky P. Long-term failure of pelvic floor musculature exercises in treatment of genuine stress incontinence. South Med J. 1995;88:547–549. [DOI] [PubMed] [Google Scholar]
- 15.Mouritsen L, Frimodt-Moller C, Moller M. Long-term effect of pelvic floor exercises on female urinary incontinence. Br J Urol. 1991;68:32–37. [DOI] [PubMed] [Google Scholar]
- 16.Haynes R. Compliance in Health Care. Baltimore, MD: John Hopkins University Press; 1979.
- 17.Oldridge N. Compliance and exercise in primary and secondary prevention of coronary heart disease: a review. Prev Med. 1982;11:56–70. [DOI] [PubMed] [Google Scholar]
- 18.Sluijs E, Kok G, van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther. 1993;11:771–782. [DOI] [PubMed] [Google Scholar]
- 19.Alewinjnse D, Mesters I, Metsemakers J, van den Borne B. Program development for promoting adherence during and after exercise therapy for urinary incontinence. Patient Educ Couns. 2001;48:147–160. [DOI] [PubMed] [Google Scholar]
- 20.Bø K, Hagen RH, Kvarstein B, et al. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence, III: effects of two different degrees of pelvic floor muscle exercises. Neurol Urodyn. 1990;9:489–502. [Google Scholar]
- 21.Tchou DCH, Adams CA, Varner RE, Denton B. Pelvic-floor musculature exercises in treatment of anatomical urinary stress incontinence. Phys Ther. 1988;68:652–655. [DOI] [PubMed] [Google Scholar]
- 22.Dougherty M, Bishop K, Abrams R, et al. The effect of exercise on the circumvaginal muscles in postpartum women. J Nurs Midwifery. 1989;34:8–14. [DOI] [PubMed] [Google Scholar]
- 23.Dougherty M, Bishop K, Mooney R, et al. Graded pelvic muscle exercise: effect on stress urinary Incontinence. J Reprod Med. 1993;38:684–693. [PubMed] [Google Scholar]
- 24.Burns P, Pranikoff K, Nochajski T, et al. Treatment of stress incontinence with pelvic floor exercises and biofeedback. J Am Geriatr Soc. 1990;38:341–344. [DOI] [PubMed] [Google Scholar]
- 25.McIntosh L, Frahm J, Mallett V, Richardson D. Pelvic floor rehabilitation in the treatment of incontinence. J Reprod Med. 1993;38:662–666. [PubMed] [Google Scholar]
- 26.Sussett J, Galea G, Read L. Biofeedback therapy for female incontinence due to low urethral resistance. J Urol. 1990;143:1205–1208. [DOI] [PubMed] [Google Scholar]
- 27.Graves J, Pollock M, Leggett S, et al. Effect of reduced training frequency on muscular strength. Int J Sports Med. 1988: 316–318. [DOI] [PubMed]
- 28.Carpenter D, Graves J, Pollock M, et al. Effect of 12 and 20 weeks of resistance training on lumbar extension torque production. Phys Ther. 1991;71:580–588. [DOI] [PubMed] [Google Scholar]
- 29.Tucci J, Carpenter D, Pollock M, et al. Effect of reduced frequency of training and detraining on lumbar extension strength. Spine. 1992;17:1407–1501. [DOI] [PubMed] [Google Scholar]
- 30.Houmard J, Costill D, Mitchell J, et al. Reduced training maintains performance in distance runners. Int J Sports Med. 1990;11:41–45. [DOI] [PubMed] [Google Scholar]
- 31.Wyman JF, Choi SC, Harkins SW, et al. The urinary diary in evaluation of incontinent women: a test-retest analysis. Obstet Gynecol. 1988;71:812–817. [PubMed] [Google Scholar]
- 32.Fantl JA, Harkins SW, Wyman JF, et al. Fluid loss quantification test in women with urinary incontinence: a test-retest analysis. Obstet Gynecol. 1987;70:739–743. [PubMed] [Google Scholar]
- 33.Shumaker SA, Wyman JF, Uebersax JS, et al. Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Qual Life Res. 1994;3:291–306. [DOI] [PubMed] [Google Scholar]
- 34.Brink CA, Sampselle CM, Wells TJ, et al. A digital test for pelvic muscle strength in older women with urinary incontinence. Nurs Res. 1989;38:196–199. [PubMed] [Google Scholar]
- 35.Sampselle CM, Brink CA, Wells TJ. Digital measurement of pelvic muscle strength in childbearing women. Nurs Res. 1989;38:134–138. [PubMed] [Google Scholar]
- 36.Pizzari T, Taylor NF, McBurney H, Feller JA. Adherence to rehabilitation after anterior cruciate ligament reconstructive surgery: implications for outcome. J Sport Rehabil. 2005: 14:201–214. [Google Scholar]
- 37.Bump RC, Norton P. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 1998;25:723–746. [DOI] [PubMed] [Google Scholar]