Abstract
An increasing number of elderly individuals are now undergoing coronary artery bypass surgery. Elderly patients, compared with patients of a younger age group, present for surgery with a greater burden of risk factors and reduced functional levels. Short‐term outcomes are hence poorer in them. But symptom relief occurs in most survivors and is accompanied by excellent rates of long‐term survival and a good quality of life. Therefore, an individualised risk–benefit profile must be carefully constructed by clinicians, taking into account several different factors and not just age alone. This review summarises the current concepts of coronary artery bypass surgery from the perspective of the very old.
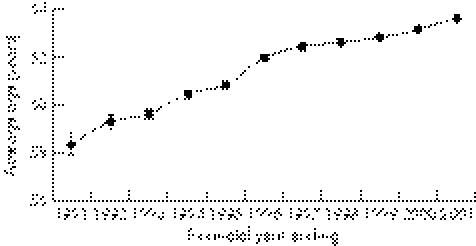
There have been remarkable advancements in the strategies for prevention and treatment of coronary artery disease. Use of drugs like statins and angiotensin‐converting enzyme inhibitors has reduced death and disability in millions. This, coupled with state‐of‐the‐art catheter‐based interventions, mainly stent technology, have advanced the age at which patients present for coronary artery bypass grafting (CABG) operations (fig 1).1,2,3 The age group defined as “elderly” in the literature has gradually increased from ⩾65 years to ⩾80 years. The greatest increase in numbers undergoing heart surgery has occurred in the oldest group of persons, those aged ⩾85 years.4 Among the 25 000 CABG operations performed every year in the UK, almost a quarter of the patients are aged >70 years, and 8% are >75 years.3 This ageing surgical population, not unexpectedly, has a relatively greater prevalence of cerebrovascular disease, left ventricular dysfunction, diabetes mellitus, chronic obstructive pulmonary disease, renal impairment and peripheral arterial disease.5,6,7 Therefore, such elderly people with multiple comorbidities tend to have a high rate of complications after CABG.5 Indeed, old age alone (ie, >75 years) is an independent risk factor for poor outcomes after CABG.6
Figure 1 Graph depicting the advancing age of patients presenting for coronary artery bypass surgery. Reproduced from the National Adult Cardiac Surgical Database Report 2000–1.3
Age‐related changes in cardiovascular physiology
In all, 80% of patients >80 years have identifiable cardiovascular disease.7 Age‐related changes occur in small and large vessels and in the heart itself, reducing physiological reserves. Most patients show no signs of impaired haemodynamic performance at baseline, but stresses of anaesthesia will often uncover their limited cardiac reserve.7
Changes in the vessel wall
The intimal layer becomes less smooth with age, resulting in endothelial damage and turbulent flow patterns. An increased number of potential sites for lipid deposition are created. A complex cascade is then initiated, leading to intimal deposition of connective tissue, calcium and lipid, and deposition in the media of elastic fibres and smooth muscle cells in the media. This leads to stiffening of the vascular wall and increased peripheral vascular resistance, which in turn results in elevated diastolic blood pressures.
Changes in the myocardium
On prolonged exposure to high afterloads, myocyte turnover through apoptosis is accelerated, with subsequent hypertrophy of the remaining cells and development of interstitial fibrosis. The resultant ventricular hypertrophy and non‐compliance leads to diastolic dysfunction of the heart.8 The ventricle remains stiff during the early passive phases of diastolic filling when the mitral valve opens, which reduces the end diastolic volume. Compared with that of 20‐year‐olds, the early diastolic filling of 80‐year‐old individuals is reduced by one third to one half.8
The overall cardiovascular function at rest in most healthy elderly people is adequate to meet the body's needs. The resting heart rate is unchanged. Heart size is essentially no different in older adults, but heart wall thickness increases modestly, largely due to myocyte hypertrophy.8
Physical work capacity declines with advancing age, but the extent to which this can be attributed to a reduced cardiac reserve is not established. Part of the age‐related decline in maximum oxygen consumption may be due to peripheral rather than central circulatory factors—for example, due to a decrease in muscle mass with age, the ability to direct blood flow to muscles with exercise, and the ability of muscles to utilise oxygen.8 Changes in cardiac function which overshoot the identified limits for age‐related changes for healthy elderly individuals are most probably due to an interaction between physical deconditioning and cardiovascular disease.8
Coronary artery bypass surgery: then and now
CABG is considered in elderly individuals when maximal pharmacological treatment fails to limit the symptoms of angina and dyspnoea, and percutaneous coronary intervention is either not feasible or is relatively less beneficial. The compelling indications for CABG are as follows:
severe left main stem (LMS) disease, even if asymptomatic
LMS equivalent—that is, >70% stenosis of the proximal left anterior descending (LAD) and circumflex arteries
three‐vessel disease
two‐vessel disease with severe proximal LAD stenosis and left ventricular ejection fraction (LVEF) <50% or demonstrable ischaemia on non‐invasive testing
disabling angina despite maximal medical treatment
unstable angina or non‐ST elevation myocardial infarction with proximal LAD and one or two‐vessel disease.9
In many cases it may be prudent to consider percutaneous coronary intervention, especially in those with discrete proximal stenoses or in those after acute coronary syndromes, where the risk of surgery may be higher. This may prove to be a good strategy and may help to avoid the complications of surgery, although the small risk of contrast‐induced nephropathy, stroke or other acute procedural complications should not be overlooked.
Left ventricular function must be considered at an early stage in the decision to operate. A low LVEF, if irreversible in the short term, can negate the benefits of surgery and is a powerful risk factor for perioperative mortality.9 Saphenous vein grafts have been traditionally used as the bypass conduits in CABG. The delayed return of angina and the fact that approximately half of the survivors of CABG eventually die of cardiac‐related causes identifies the “Achilles heel” of this procedure: late vein‐graft atherosclerosis.10 This tends to occur more frequently between 5 and 10 years after the operation.10 Use of left internal mammary artery grafts has helped to overcome this and many other problems associated with vein grafts. When they were used in combination with vein grafts, better long‐term patency rates were observed. Use of left internal mammary artery grafts along with vein grafts in people aged >70 years11 and in octogenarians12 has resulted in improved long‐term outcomes. Total arterial revascularisation (bilateral internal mammary artery grafts), may have even greater benefit.13 Radial arteries have now been added to the armamentarium of surgeons. They have certain advantages, in that they are easily harvested, versatile and have excellent handling characteristics.14 Excellent long‐term angiographic patency rates have been reported with radial grafts.15
Off‐pump coronary artery bypass surgery
Off‐pump coronary artery bypass surgery (OPCAB), in recent years, has emerged as an effective surgical technique, and may be of particular benefit in high‐risk populations. Conventional CABG using cardiopulmonary bypass and cardioplegic arrest has, for many years, represented the “gold standard” in coronary revascularisation. Now, OPCAB is being performed with increasing frequency. The chief advantage of OPCAB is the avoidance of the effects of cardioplegic arrest. For example, frequency of occurrence of systemic inflammatory response syndrome (SIRS) may be significantly less with OPCAB.16 SIRS results from a cascade of events generated by the contact of plasma proteases and blood cells with the gaseous interface and bioincompatible surfaces of the cardiopulmonary bypass machine. Patients with reduced LVEF are particularly susceptible to damage by these inflammatory mediators.17 There is a general consensus from randomised trials and prospective cohort studies that OPCAB is associated with a lesser degree of myocardial injury than traditional on‐pump CABG.18,19,20 OPCAB may also attenuate renal damage as compared with on‐pump surgery.21,22 In addition, OPCAB may reduce the incidence of neurological complications, especially stroke, in octogenarians.2 Randomised clinical trials, as well as analyses of several large registries, have shown that OPCAB achieves similar multi‐vessel revascularisation as conventional on‐pump surgery with better or equivalent short‐term and mid‐term outcomes.2,18,23,24 OPCAB, in elderly people with concomitant risk factors, has been found to be superior to on‐pump surgery.2,24,25 Therefore, OPCAB is a surgical technique with the potential to offer a lesser incidence of complications, superior short‐term and mid‐term outcomes, and comparable graft patency. However, long‐term outcomes will have to be evaluated to determine whether it will ultimately challenge conventional on‐pump revascularisation in elderly people.16
Predictors of a poor outcome after CABG
Euroscore and Parsonnet risk stratification systems provide a relatively robust estimation of post‐operative risk, and are widely used.3 They assist surgeons in making decisions and provide useful information for patients to consider during the process of informed consent. Of note, both systems incorporate patients' age as a risk factor. The following conditions have been found to amplify the risk of mortality and morbidity as a result of CABG in the elderly people.9,26,27
Preoperative: reduced LVEF (especially if <30%), diabetes mellitus, recent (<30 days) myocardial infarction, LMS or three‐vessel disease, atrial fibrillation, renal dysfunction, obesity, chronic obstructive pulmonary disease, smoking and female gender.
Intraoperative: long cardiopulmonary bypass time, emergency operation, reoperation and use of bilateral internal mammary artery grafting.
Postoperative: atrial fibrillation, mediastinitis and post‐operative bleeding.
Intraoperative or postoperative myocardial infarction, low‐output syndrome, stroke, gastrointestinal complications, wound infection and renal failure occur more frequently in elderly people after cardiac surgery and predict adverse outcomes.5
Survival benefits
CABG in octogenarians relieves angina effectively.1,28 The overall mortality after CABG in elderly patients has steadily declined over the years with improvements in surgical techniques. The crude survival rates after CABG in individuals aged >75 years in the UK has increased from 92.4% (n = 821) in 1998 to 94.1% (n = 1804) in 2001.3
A large study4 found a 34% reduction in risk‐adjusted operative mortality in elderly people (1982–96), apart from confirming a time‐related increase in the prevalence of older patients and an increase in the preoperative risk profile of these patients. But, when compared with patients of a younger age group, those aged >75 years continue to have poorer short‐term outcomes. In an analysis of 6057 patients who underwent isolated CABG between 1996 and 2002, the 30‐day mortality rate and the incidence of postoperative complications was found to largely escalate with age.27 In‐hospital outcomes and cost were examined among 2272 elderly people (⩾75 years) and 9745 younger patients (<75 years) who underwent CABG between 1997 and 2001 in another study.29 After controlling for clinical differences, age ⩾75 years was found to be associated with a longer length of hospital stay, higher mortality rates and higher in‐hospital cost.29 Other prospective studies30 found higher mortality and complication rates in the short term after CABG for octogenarians compared with subjects aged <75 years.
Although short‐term outcomes are poorer, the long‐term benefits seem to be good for most survivors of surgery. An analysis of nearly 25 000 patients aged >80 years who underwent CABG between 1987 and 1990 showed that, in those who survived, the long‐term survival rate was similar to that of the general population of octogenarians matched for age, sex and race.31 More recently, octogenarians (mean age 82 years) who underwent isolated elective CABG were found to have a satisfactory risk–benefit profile in the long term.32 The mortality was 7% and the 5‐year actuarial survival rate for the hospital survivors was 75% in this study, with a mean survival period of 76 months. However, for urgent or emergent cases, a marked increase in morbidity and mortality was noted.32
Indeed, the data in many of the above studies are several years old, but with technical and procedural advancement, we can only expect the outcomes to get better. This is in fact corroborated by recently published data from a prospective study in a UK tertiary centre, which shows excellent long‐term survival rates after CABG for individuals aged >80 years.33 A total of 12 461 consecutive patients (>80 years, n = 706) who underwent CABG between 1996 and 2003 were evaluated. Despite poorer short‐term outcomes, long‐term survival in the patients aged >80 years was significantly better compared with a general population with the same age–sex distribution (survival rate at 5 years 82.1% v 55.9%, p<0.001).33
In effect, CABG in patients >80 years effectively alleviates symptoms at the cost of poorer short‐term outcomes and higher costs of hospitalisation. But this can be offset by an excellent long‐term survival rate, which is comparable with that of the general population of octogenarians. There are concerns that the publication of surgeon‐specific mortality data may have an effect on selection of octogenarian patients for surgery. But, as the long‐term survival in this group of individuals is good, the effect on patient selection may actually be small.
Quality of life after CABG
As CABG effectively relieves angina and may prolong survival, improved quality of life could be expected after surgery. Equally important to determining the overall quality of life is the need to determine the effect that CABG has on physical and mental health. Data available to help clinicians identify those elderly patients who are likely to have an improvement in quality of life after CABG are limited. Although hospitalisation may be longer for elderly patients, physiological, psychological and social recovery patterns through the first 6 weeks postoperatively have been reported to be similar to those of a younger age group.34 In a study which used self‐reported health questionnaires in 1744 patients aged >65 years undergoing CABG, significant improvements were noted in quality of life after a 6‐month follow‐up.35 This benefit was present across all age groups and was found to be particularly magnified in patients who had a poorer preoperative health status. Hedeshian et al1 found that patients aged >70 years presented for CABG at a lower functional level than younger patients, but the marked improvement in functional capacity that occurred after surgery was comparable among all age groups. More recently, survivors among octogenarians who underwent isolated CABG were found to have an excellent quality of life for up to 5 years after surgery.28 Hence, excellent long‐term survival after CABG in elderly people may indeed be accompanied by an equally satisfactory quality of life in the majority.
Who among the elderly are ideal candidates for CABG?
This, unfortunately, is not an easy question to answer. Risk–benefit profiles are individualised, and each elderly patient must be assessed on his or her own merit. There are no universally accepted standards for selection or rejection of patients for surgery. An elderly person with few background illnesses and a good expected quality and length of life would probably stand to benefit from CABG. On the other hand, an octogenarian with several comorbidities and an expected suboptimal quality of life after surgery would probably be best managed conservatively. The greatest risk, however, is in the critically ill elderly patient for whom the CABG operation may be the best of several high‐risk options.
Conclusion
Coronary artery surgery for the elderly is now safer than ever before, owing to modern surgical techniques and pharmacological breakthroughs. Despite magnified perioperative and postoperative dangers, symptom relief occurs in most patients. Long‐term survival and quality of life are also preserved or enhanced in the majority. Clinicians must understand the normal physiological changes associated with ageing in order to construct a risk–benefit analysis that is specifically tailored to each patient. This analysis should take into account a patient's life expectancy and quality of life both before and after a procedure, and not just age alone. Discrepancies between chronological age and biological age must be dealt with. Further, the physician is expected to anticipate end‐of‐life issues and the potential need for rehabilitation or nursing home placement in the early postoperative period. Most important among all is that these issues must be discussed with the patients and their families. Hence, it is up to the patient and the clinician to explore the potential benefits of an improved quality of living with the attendant risks of the procedure versus alternative treatment. Advanced age alone should not be a deterrent for coronary artery bypass surgery if it has been determined that these benefits outweigh the potential risk.
Multiple choice questions; answers at the end of references
-
Mark the statements which are true
-
-
A. There has been an increase in the number of elderly patients undergoing CABG
-
-
B. Therapeutic advancements have led to a decrease in the number of elderly individuals with cardiovascular problems.
-
-
C. Elderly patients generally present with an excellent functional level with few background problems.
-
-
D. Age alone is an independent risk factor for poor outcomes after CABG
-
-
E. The single most important thing clinicians must consider prior to choosing CABG over conservative therapy is, age
-
-
-
Mark the statements which are true
-
-
A. Chronological age goes hand in hand with biological age
-
-
B. Diastolic dysfunction can occur with increasing age
-
-
C. Arterial grafts have better patency rates than venous grafts
-
-
D. Radial grafts are better than internal mammary artery grafts
-
-
E. Vein grafts should never be used
-
-
-
Mark the statements which are false
-
-
A. OPCAB should replace conventional on‐pump surgery in elderly people
-
-
B. OPCAB can be of benefit in high‐risk groups
-
-
C. Stroke and SIRS are less frequent with OPCAB compared to on‐pump CABG
-
-
D. LVEF is an important marker of prognosis in elderly individuals
-
-
E. Number of vessels involved has no influence on the outcome of CABG
-
-
-
Mark the statements which are true
-
-
A. CABG in octogenarians compared to that in younger persons results in higher in‐hospital mortality
-
-
B. CABG has poor long‐term prognosis in the majority of people aged over 75
-
-
C. Octogenarians undergoing CABG in the UK have lower rates of long‐term survival compared to the general population of octogenarians
-
-
D. Quality of life is preserved or enhanced in the majority of elderly individuals after CABG
-
-
E. The decision to operate must always be left to the surgeon
-
-
Abbreviations
CABG - coronary artery bypass grafting
LAD - left anterior descending
LMS - left main stem
LVEF - left ventricular ejection fraction
OPCAB - off‐pump coronary artery bypass surgery
SIRS - systemic inflammatory response syndrome
Answers
A, D
B, C
A, E
A, D
Footnotes
Funding: None.
Competing interests: None.
Ethical approval: Not required.
References
- 1.Hedeshian M H, Namour N, Dziadik E.et al Does increasing age have a negative impact on six‐month functional outcome after coronary artery bypass? Surgery 2002132239–244. [DOI] [PubMed] [Google Scholar]
- 2.Ricci M, Karamanoukian H L, Abraham R.et al Stroke in octogenarians undergoing coronary artery surgery with and without cardiopulmonary bypass. Ann Thorac Surg 2000691471–1475. [DOI] [PubMed] [Google Scholar]
- 3. National Adult Cardiac Surgical Database Report 2000–2001. http://www.ctsnet.org/file/SCTS2000pages72‐81Age.pdf (accessed 22 Nov 2006)
- 4.Ivanov J, Weisel R D, David T E.et al Fifteen‐year trends in risk severity and operative mortality in elderly patients undergoing coronary artery bypass graft surgery. Circulation 199897673–680. [DOI] [PubMed] [Google Scholar]
- 5.Moshkovitz Y, Paz Y, Shabtai E.et al Predictors of early and overall outcome in coronary artery bypass without cardiopulmonary bypass. Eur J Cardiothorac Surg 19971231–39. [DOI] [PubMed] [Google Scholar]
- 6.Loop F D, Lytle B W, Cosgrove D M.et al Coronary artery bypass graft surgery in the elderly. Indications and outcome. Cleve Clin J Med 19885523–34. [DOI] [PubMed] [Google Scholar]
- 7.Loran D B, Zwischenberger J B. Thoracic surgery in the elderly. J Am Coll Surg 2004199773–784. [DOI] [PubMed] [Google Scholar]
- 8.Lakatta E G. Changes in cardiovascular function with aging. Eur Heart J 199011(Suppl C)22–29. [DOI] [PubMed] [Google Scholar]
- 9.Eagle KA Guyton R A, Davidoff R.et al ACC/AHA 2004 guideline update for coronary artery bypass graft surgery. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to update the 1999 guidelines for coronary artery bypass graft surgery). American College of Cardiology Website http://www.acc.org/clinical/guidelines/cabg/cabg.pdf 2004 (accessed 22 Nov 2006)
- 10.Lytle B W, Loop F D, Cosgrove D M.et al Long‐term (5 to 12 years) serial studies of internal mammary artery and saphenous vein coronary bypass grafts. J Thorac Cardiovasc Surg 198589248–258. [PubMed] [Google Scholar]
- 11.Gardner T J, Greene P S, Rykiel M F.et al Routine use of the left internal mammary artery graft in the elderly. Ann Thorac Surg 199049188–194. [DOI] [PubMed] [Google Scholar]
- 12.Kurlansky P A, Williams D B, Traad E A.et al Arterial grafting results in reduced operative mortality and enhanced long‐term quality of life in octogenarians. Ann Thorac Surg 200376418–427. [DOI] [PubMed] [Google Scholar]
- 13.Taggart D P, D'Amico R, Altman D G. Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet 2001358870–875. [DOI] [PubMed] [Google Scholar]
- 14.Mussa S, Choudhary B P, Taggart D P. Radial artery conduits for coronary artery bypass grafting: current perspective. J Thorac Cardiovasc Surg 2005129250–253. [DOI] [PubMed] [Google Scholar]
- 15.Possati G, Gaudino M, Prati F.et al Long‐term results of the radial artery used for myocardial revascularization. Circulation 20031081350–1354. [DOI] [PubMed] [Google Scholar]
- 16.Murphy G J, Ascione R, Angelini G D. Coronary artery bypass grafting on the beating heart: surgical revascularization for the next decade? Eur Heart J 2004252077–2085. [DOI] [PubMed] [Google Scholar]
- 17.Deng M C, Dasch B, Erren M.et al Impact of left ventricular dysfunction on cytokines, hemodynamics, and outcome in bypass grafting. Ann Thorac Surg 199662184–190. [DOI] [PubMed] [Google Scholar]
- 18.van Dijk D, Nierich A P, Jansen E W.et al Early outcome after off‐pump versus on‐pump coronary bypass surgery: results from a randomized study. Circulation 20011041761–1766. [DOI] [PubMed] [Google Scholar]
- 19.Czerny M, Baumer H, Kilo J.et al Inflammatory response and myocardial injury following coronary artery bypass grafting with or without cardiopulmonary bypass. Eur J Cardiothorac Surg 200017737–742. [DOI] [PubMed] [Google Scholar]
- 20.Penttila H J, Lepojarvi M V, Kiviluoma K T.et al Myocardial preservation during coronary surgery with and without cardiopulmonary bypass. Ann Thorac Surg 200171565–571. [DOI] [PubMed] [Google Scholar]
- 21.Loef B G, Epema A H, Navis G.et al Off‐pump coronary revascularization attenuates transient renal damage compared with on‐pump coronary revascularization. Chest 20021211190–1194. [DOI] [PubMed] [Google Scholar]
- 22.Ascione R, Lloyd C T, Underwood M J.et al On‐pump versus off‐pump coronary revascularization: evaluation of renal function. Ann Thorac Surg 199968493–498. [DOI] [PubMed] [Google Scholar]
- 23.Angelini G D, Taylor F C, Reeves B C.et al Early and midterm outcome after off‐pump and on‐pump surgery in Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. Lancet 20023591194–1199. [DOI] [PubMed] [Google Scholar]
- 24.Al‐Ruzzeh S, Nakamura K, Athanasiou T.et al Does off‐pump coronary artery bypass (OPCAB) surgery improve the outcome in high‐risk patients? : a comparative study of 1398 high‐risk patients, Eur J Cardiothorac Surg 20032350–55. [DOI] [PubMed] [Google Scholar]
- 25.Tashiro T, Todo K, Haruta Y.et al Coronary artery bypass grafting without cardiopulmonary bypass for high‐risk patients. Cardiovasc Surg 19964207–211. [DOI] [PubMed] [Google Scholar]
- 26.He G W, Acuff T E, Ryan W H.et al Determinants of operative mortality in elderly patients undergoing coronary artery bypass grafting. Emphasis on the influence of internal mammary artery grafting on mortality and morbidity. J Thorac Cardiovasc Surg 199410873–81. [PubMed] [Google Scholar]
- 27.Mortasawi A, Arnrich B, Walter J.et al Impact of age on the results of coronary artery bypass grafting. Asian Cardiovasc Thorac Ann 200412324–329. [DOI] [PubMed] [Google Scholar]
- 28.Wilson M F, Baig M K, Ashraf H. Quality of life in octagenarians after coronary artery bypass grafting. Am J Cardiol 200595761–764. [DOI] [PubMed] [Google Scholar]
- 29.Chee J H, Filion K B, Haider S.et al Impact of age on hospital course and cost of coronary artery bypass grafting. Am J Cardiol 200493768–771. [DOI] [PubMed] [Google Scholar]
- 30.Avery GJ I I, Ley S J, Hill J D.et al Cardiac surgery in the octogenarian: evaluation of risk, cost, and outcome. Ann Thorac Surg 200171591–596. [DOI] [PubMed] [Google Scholar]
- 31.Peterson E D, Cowper P A, Jollis J G.et al Outcomes of coronary artery bypass graft surgery in 24,461 patients aged 80 years or older. Circulation 199592II85–II91. [DOI] [PubMed] [Google Scholar]
- 32.Ishikawa S, Buxton B F, Manson N.et al Cardiac surgery in octogenarians. ANZ J Surg 200474983–985. [DOI] [PubMed] [Google Scholar]
- 33.Stoica S C, Cafferty F, Kitcat J.et al Octogenarians undergoing cardiac surgery outlive their peers: a case for early referral. Heart 200692503–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Artinian N T, Duggan C, Miller P. Age differences in patient recovery patterns following coronary artery bypass surgery. Am J Crit Care 19932453–461. [PubMed] [Google Scholar]
- 35.Rumsfeld J S, Magid D J, O'Brien M.et al Changes in health‐related quality of life following coronary artery bypass graft surgery. Ann Thorac Surg 2001722026–2032. [DOI] [PubMed] [Google Scholar]