Abstract
Background
Fatty liver disease (FLD) is highly prevalent in Western countries, but recent data have shown that FLD is also emerging in China.
Aim
To investigate the prevalence and risk factors of FLD in the Shuiguohu district of Wuhan city, central China, during 1995–2004.
Methods
12247 individuals (7179 men and 5068 women) over 18 years of age who were living in the area were investigated for FLD in the Zhongnan Hospital of Wuhan University from 1995 to 2004. FLD was determined by the ultrasonographic method. Height, weight, blood pressure, fasting blood sugar, alanine aminotransferase, total cholesterol and triglyceride were determined by routine laboratory methods.
Results
The prevalence of FLD was 12.5% in 1995, and rose gradually to 24.5% by 2003–4. The prevalence was twice as high in men (28.1%) as in women (13.8%), and increased with age in females, and males <60 years of age. Multivariate analysis showed that several risk factors were profoundly associated with the prevalence of FLD, including male sex, old age, obesity, hyperlipidaemia (cholesterol or triglyceride), fasting hyperglycemia and hypertension.
Conclusion
The prevalence of FLD in the Shuiguohu district of Wuhan city, central China, was shown to have increased during the 10‐year period, 1995 to 2004. The FLD was found to be closely associated with sex, age, obesity and other metabolic syndrome features.
Fatty liver disease (FLD) is an increasingly recognised disease in the world. FLD can be either alcoholic or non‐alcoholic, and both conditions may progress to the end stage of liver disease. The mean prevalence of FLD in western countries, as measured by ultrasonography, ranges from 20% to 60%.1 Many potential risk factors for non‐alcoholic fatty liver disease (NAFLD) including obesity, insulin resistance, hyperlipidaemia and diabetes have been identified previously.2,3,4 Two reports from Shanghai5 and Shenzhen6 showed that the prevalence of FLD was 20.8% (17.9% after adjustment by age and sex) in East China and 20.7% in South China, respectively, lower than that in western countries.7 However, the incidence and prevalence of FLD in other area of China is unclear. The incidence of FLD is likely to rise steadily in the Chinese population owing to the increase in elderly population, changes in life style, alcohol and excessive food intake, westernisation of the diet style, a general lack of exercise and prevalence of viral hepatitis. To date, there is no report of a change in FLD prevalence during the recent 10 years in China. The current study aimed to investigate the prevalence and risk factors of FLD during 1995–2004 in the Shuiguohu district of Wuhan city, central China and to gain a better understanding of the changes in FLD prevalence and the aetiology of FLD.
Patients and methods
Subjects
In all, 12247 individuals aged >18 years, who were living in the Shuiguohu district and having physical examinations in the check‐up centre of Zhongnan Hospital of Wuhan University during 10‐year period from 1995 to 2004, were retrospectively studied. Each subject gave his/her written, informed consent, and the study was approved by the ethics committee of the Wuhan University Zhongnan Hospital.
Methods
Each patient's chart was reviewed independently by two authors (ZLW and XQC). Questionnaires were designed to include previous history of diseases and the details of drugs. Body weight, height and blood pressure were measured during physical examination. Liver, gallbladder and spleen were examined by ultrasonograph (LOGIQ400PROB, China, with a probe frequency of 3.5 MHz) between 08:00 h and 09:00 h after overnight fasting. Serum alanine aminotransferase (ALT), total cholesterol, triglyceride and plasma glucose levels were examined by routine laboratory tests. Individuals with chronic viral hepatitis (hepatitis B, C), cirrhosis of liver, malignancies, pregnancy, long‐term using of oestrogens, tamoxifen, corticosteroids and patients with incompleted data were excluded from the study.
Diagnosis criteria
Diagnosis of FLD was based on the presence of an ultrasonographic pattern,8,9 which meets the criteria of FLD designed by the Chinese Liver Disease Association 2002.10,11 Body mass index (BMI) was calculated as the weight in kilograms divided by the square of the height in meters, and BMI ⩾25 kg/m2 was defined as obesity in both men and women according to the redefined World Health Organization criterion in the Asia Pacific Region.12 Hypertension was diagnosed by systolic blood pressure ⩾140 mm Hg or diastolic blood pressure ⩾90 mm Hg according to the criterion of World Health Organization. Hyperlipidaemia was defined as total cholesterol ⩾5.2 mmol/l or triglyceride ⩾1.7 mmol/l. Fasting hyperglycemia was defined as fasting blood sugar ⩾6.1 mmol/l. Serum ALT abnormalities was defined as ALT⩾43 IU/l.
Statistical analysis
Descriptive results of continuous variables were expressed as mean (standard deviation (SD)). The difference in numeric data was assessed using the Student's t test, and categorical data using the χ2 test. In the analysis of continuous variables, data were categorised according to cut‐off values and analysed using a χ2 test or Fisher's exact test. Logistic regression analysis was used to identify risk factors for FLD. Odds ratios (OR) and 95% confidence interval (CI) were estimated when appropriate. All statistical comparisons were two‐tailed, and p values<0.05 were considered significant. Statistical analyses were performed using SPSS V.12.0 software.
Results
The prevalence of FLD and gender difference
Table 1 shows the demographic and clinical data of the participants. Differences in age, BMI, sonographic fatty liver and other clinical characteristics between sexes were significant. Of the 12247 subjects, 2715 were diagnosed as FLD by ultrasonograph and the average prevalence of FLD was 22.2% (28.1% in men, 13.8% in women).
Table 1 Demographic and clinical data of the study population.
| Total (n = 12247) | Men (n = 7179) | Women (n = 5068) | |
|---|---|---|---|
| Age (years), mean (SD) | 43.08 (13.61) | 43.36 (13.67) | 42.68 (13.57)** |
| BMI (kg/m2), mean (SD) | 23.36 (3.31) | 24.13 (3.13) | 22.29 (3.24)** |
| Sonographic fatty liver, n (%) | 2715 (22.2) | 2016 (28.1) | 699 (13.8)** |
| BMI ⩾25 kg/m2, n (%) | 3733 (30.5) | 2821 (39.3) | 912 (18.0)** |
| High fasting glucose ⩾6.1 mmol/l, n (%) | 1327 (10.8) | 861 (12) | 466 (9.2)** |
| High systolic blood pressure ⩾140 mm Hg, n(%) | 1526 (12.5) | 1034 (14.4) | 492 (9.7)** |
| High diastolic blood pressure ⩾90 mm Hg, n (%) | 1796 (14.7) | 1335 (18.6) | 461 (9.1)** |
| Alanine aminotransferase ⩾43 IU/l, n (%) | 1745 (14.2) | 1400 (19.5) | 345 (6.8)** |
| High total cholesterol ⩾5.2 mmol/l, n (%) | 3325 (27.1) | 2017 (28.1) | 1308 (25.8)* |
| High triglyceride ⩾1.7 mmol/l, n (%) | 3048 (24.9) | 2247 (31.3) | 801 (15.8)* |
BMI, body mass index.
*p<0.05, indicating significant difference between sexes.
**p<0.001, indicating significant difference between sexes.
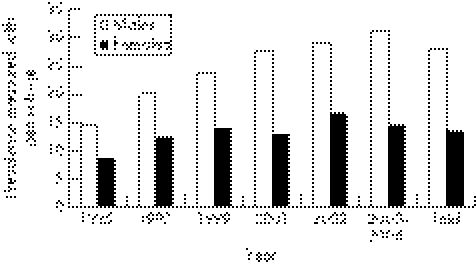
As shown in table 2 and fig 1, the prevalence of FLD during 1995–2004 increased from 12.5% in 1995 to 24.5% during April 2003 to March 2004 (in trend analysis, p<0.001). In males, the prevalence of FLD increased significantly; this was not seen in females. The average prevalence of FLD during the 10‐year period was twice as high in males as in females (28.1 vs 13.8%, p<0.001).
Table 2 The trend of prevalence of fatty liver in Shuiguohu district of Wuhan city, central China, during 1995–2004.
| 1995 | 1997 | 1999 | 2001 | 2002 | 2003–4 | Total | |
|---|---|---|---|---|---|---|---|
| Total number (men/women) | 1000 (664/336) | 1000 (525/475) | 1000 (584/416) | 1000 (558/442) | 1000 (595/405) | 7247 (4253/2994) | 12247 (7179/5068) |
| Age (years) | 41.93 (13.62) | 41.62 (14.8) | 41.28 (12.28) | 41.41 (13.46) | 41.42 (12.57) | 43.25 (13.62) | 43.08 (13.61) |
| BMI (kg/m2) | 22.07 (3.12) | 22.96 (3.21) | 22.89 (3.04) | 22.72 (3.29) | 23.01 (3.34) | 23.57 (3.38) | 23.36 (3.31) |
| ALT (⩾43 IU/l), n (%) | 68 (6.8) | 111 (11.1) | 142 (14.2) | 149 (14.9) | 169 (16.9) | 1106 (15.3) | 1745 (14.3) |
| FLD, n (%) | 125 (12.5) | 163 (16.3) | 197 (19.7) | 210 (21) | 241 (24.1) | 1779 (24.5) | 2715 (22.2) |
| Men, n (%)/women, n (%) | 97 (14.6)/28 (8.3) | 105 (20)/58 (12.2) | 139 (23.8)/58 (13.9) | 154 (27.6)/56 (12.7) | 174 (29.2)/67 (16.5) | 1347 (31.2)/432 (14.4) | 2016 (28.1)/699 (13.8) |
ALT, alanine aminotransferase; BMI, body mass index; FLD, fatty liver disease.
Figure 1 Prevalence of fatty liver disease among 12247 Chinese adults during 1995 to 2004.
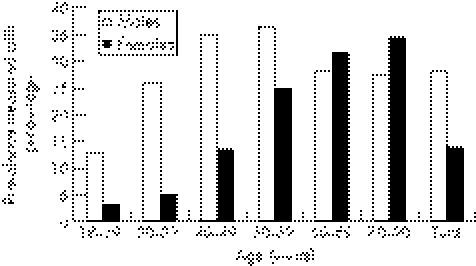
The prevalence of FLD was 12.8% in men aged 18–29 years and increased gradually to 36.5% in men aged 50–59 years and slowed down after 60 years. In women, the prevalence of FLD increased gradually from 3% in those aged 18–29 years to 24.9% in 50–59 years and peaked in ⩾70 years (fig 2). The prevalence of FLD in men <60 years was significantly higher than that in women with similar age (28.2 vs 11.1%, p<0.001), whereas in those >60 years the prevalence of FLD between men and women was similar (27.9 vs 32.3%, p = 0.051).
Figure 2 Age‐specific prevalence of fatty liver disease among 12247 Chinese adults.
Risk factors or predictors of FLD
Table 3 shows variations in the prevalence of FLD according to the metabolic status. Increasing of FLD prevalence was closely associated with increasing of body mass index (BMI), fasting hyperglycemia, hypertension, hyperlipidaemia and raised ALT levels.
Table 3 Association of fatty liver with various metabolic status among 12247 Chinese adults.
| Variables | FL/total | Total (n = 12247) | Men (n = 7179) | Women (n = 5068) |
|---|---|---|---|---|
| n | (95% CI) | (95% CI) | (95% CI) | |
| Body mass index (kg/m2) | ||||
| <25 | 809/8514 | 9.5 (8.9 to 10.1) | 12.3 (11.3 to 13.3) | 6.6 (5.8 to 7.3) |
| 25–30 | 1653/3391 | 48.7 (47.1 to 50.4)* | 50.5 (48.6 to 52.4)* | 42.1 (38.7 to 45.5)* |
| ⩾30 | 253/342 | 73.9 (69.2 to 78.5)* | 73.4 (67.6 to 79.1)* | 80.2 (72.7 to 87.7)* |
| High fasting glucose (mmol/l) | ||||
| <6.1 | 2110/10920 | 19.3 (18.6 to 20.1) | 25.3 (24.2 to 26.3) | 11.2 (10.3 to 12.1) |
| ⩾6.1 | 605/1327 | 45.6 (43 to 48.4)* | 48.9 (45.6 to 52.2)* | 39.3 (34.8 to 43.7)* |
| High systolic blood pressure (mm Hg) | ||||
| <140 | 2175/10721 | 20.3 (19.5 to 21.1) | 26.9 (25.8 to 28) | 11.3 (10.4 to 12.3) |
| ⩾140 | 540/1526 | 35.4 (32.9 to 37.7)* | 34.9 (32 to 37.8)* | 36.6 (32.3 to 40.9)* |
| High diastolic blood pressure (mm Hg) | ||||
| <90 | 2023/10451 | 19.4 (18.6 to 20.1) | 25.2 (24.1 to 26.3) | 11.9 (11 to 12.9) |
| ⩾90 | 692/1796 | 38.5 (36.2 to 40.7)* | 40.6 (38 to 43.2)* | 32.5 (28.3 to 36.8)* |
| Alanine aminotransferase (IU/l) | ||||
| <43 | 1792/10502 | 17.1 (16.4 to 17.3) | 21.5 (20.4 to 22.5) | 11.8 (10.8 to 12.7) |
| ⩾43 | 923/1745 | 52.9 (50.5 to 55.2)* | 57.9 (55.3 to 60.6)* | 41.7 (36.5 to 47)* |
| High total cholesterol (mmol/l) | ||||
| <5.2 | 1629/8922 | 18.3 (17.4 to 19.1) | 24.6 (23.4 to 25.7) | 9.6 (8.6 to 10.5) |
| ⩾5.2 | 1086/3325 | 32.7 (31.1 to 34.3)* | 37.1 (35 to 39.2)* | 26 (23.6 to 28.4)* |
| High triglyceride (mmol/l) | ||||
| <1.7 | 1222/9199 | 13.3 (12.6 to 14) | 17.5 (16.5 to 18.6) | 8.4 (7.6 to 9.2) |
| ⩾1.7 | 1493/3048 | 49 (47.2 to 50.7)* | 51.2 (49.2 to 53.3)* | 42.6 (39.1 to 46)* |
*p<0.001, when compare with normal group.
Logistic regression analysis revealed that FLD was significantly associated with male sex, age, elevated BMI, abnormality ALT, fasting glucose, total cholesterol, triglyceride and hypertension (table 4).
Table 4 The logistic regression model for the multivariate analysis among 12247 Chinese adults.
| Variables | OR (95% CI) | ||
|---|---|---|---|
| Total (n = 12247) | Men (n = 7179) | Women (n = 5068) | |
| Sex | 1.588 (1.391 to 1.814)** | ||
| Age (per 10 years) | 1.206 (1.152 to 1.262)** | 1.143 (1.084 to 1.205)** | 1.315 (1.197 to 1.444)** |
| Body mass index (⩾25 kg/m2) | 5.418 (4.857 to 6.044)** | 6.162 (5.357 to 7.088)** | 6.802 (5.389 to 8.584)** |
| Alanine aminotransferase (⩾43 IU/l) | 2.837 (2.449 to 3.287)** | 2.75 (2.339 to 3.233)** | 3.374 (2.411 to 4.722)** |
| High fasting glucose | 1.574 (1.332 to 1.86)** | 1.368 (1.125 to 1.665)* | 2.248 (1.663 to 3.039)** |
| High systolic blood pressure (⩾140 mm Hg) | 0.979 (0.786 to 1.22) | 0.874 (0.675 to 1.132) | 1.561 (1.117 to 2.182)* |
| High diastolic blood pressure (⩾90 mm Hg) | 1.45 (1.23 to 1.71)** | 1.585 (1.318 to 1.906)** | 1.124 (0.753 to 1.679) |
| High total cholesterol (⩾5.2 mmol/l) | 1.369 (1.196 to 1.568)** | 1.285 (1.094 to 1.51)** | 1.374 (1.07 to 1.763)* |
| High triglyceride (⩾1.7 mmol/l) | 3.549 (3.121 to 4.035)** | 3.044 (2.626 to 3.529)** | 4.965 (3.84 to 6.42)** |
*p<0.05.
**p<0.001.
Discussion
The present study indicated that the prevalence of FLD was 14.6% in men and 8.3% in women in 1995, increasing gradually to 31.2% in men and 14.4% in women during the period 2003–4. The average prevalence of FLD during the 10‐year period was twice as high in men (28.1%) as in women (13.8%), which is similar to a Japanese report.13 The current study estimated that the prevalence of FLD from 2003 to 2004 was 24.5% (31.2% in men and 14.4% in women) in Wuhan residents, which was similar to 24.3% in Korean population in the year 2003,14 and higher than that of 21.8% in Japanese adults in the year 2000.15 One recent study in Shanghai from October 2002 to April 2003 showed the prevalence of FLD was 20.8% (17.9% after adjustment by age and sex).5 These studies have shown that the prevalence of FLD is truly increasing in urban areas in China. Wuhan is a modern city in central China with >8 million inhabitants and has developed very fast during these 10 years. In the Shuiguohu district, most residents are cadres or white‐collar workers who are well educated and have a high income. Improved living conditions, excessive eating and drinking, fast‐pace lifestyle, overweight and obesity are all supposed to be related to the increase of the prevalence of FLD in this area.
Our study also showed that the prevalence of FLD in males was higher than that in females before the age of 60 years, but was similar between men and women after the age of 60 years. Reduced adiponectin concentrations caused by androsterone in males and the deficiency of oestrogen and relatively increased androsterone after climacteric in women >60 years may have contributed to the differences in age and sex.14,16 This implies that before the age of 60 years, men may experience more prolonged exposure to FLD, steatohepatitis and cirrhosis, as well as proatherosclerotic risk factors associated with NAFLD.17,18
Our findings showed that the risk factors of FLD are high BMI, male sex, old age, high levels of total cholesterol or triglyceride, or fasting blood sugar, high diastolic blood pressure for men and high systolic blood pressure for women as assessed by logistic regression analysis, in agreement with the report in Shanghai.5 Our data showed that FLD was mainly associated with obesity, hyperglycemia, dyslipidaemia and hypertension. These are the main features of the recently characterised metabolic syndrome, and people with the metabolic syndrome are at increased risk of diabetes mellitus and cardiovascular disease.17,18,19,20,21,22 FLD is believed to be an additional feature of metabolic syndrome and a common “burden of disease” in the Chinese population.
Concern is growing about FLD, not only because it is a common liver disorder but also because it is one of the leading causes of aminotransferase abnormalities. Unexplained elevation in aminotransferase concentrations is strongly associated with adiposity and thus may represent FLD or NAFLD. The current study showed the prevalence of elevated ALT increased during the past 10 years and reached to15.3% in 2003–2004, which was more than that of the available estimates in the US (8.9%) between 1999 and 2002.23 The trend of the prevalence of serum ALT was well paralleled with FLD in our data. FLD is significantly associated with raised ALT levels: of those with abnormal serum ALT levels in our study, more than half (52.9%) had FLD. The increasing in ALT may be a consequence of FLD.
Our study could not separate alcoholic fatty liver disease (AFLD) from NAFLD as it was a retrospective study, and the patient charts did not record the accurate intake of alcohol. Two studies from the southeast of China showed that the prevalence of AFLD was low, only 0.79% and 0.94% in Shanghai5 and Zhejiang Provinces,24 respectively, but one study from North China showed that the prevalence of AFLD was 6.1% in heavy drinkers since more prevalent heavy drinkers were found there.25 Wuhan is located in the central China, where there are less habitual and heavy drinkers than in the north China,25 and it can be supposed that FLD is mainly composed of NAFLD in this area. In addition, this investigation was restricted to the Shuiguohu district where the provincial government was located. The results may reflect the higher standards of education and living conditions in this district. It would be interesting to investigate FLD with additional factors such as alcohol, education and economic income in future studies. The diagnosis of FLD was based on abdominal ultrasonography instead of liver biopsy/histological examination. For practical reasons this ultrasonographic method is however widely used in the detection of FL. The sensitivity of abdominal ultrasonography to detect FLD is as high as 89% and the specificity is 93%.8
In conclusion, FLD has increased during recent 10 years in the Shuiguohu district in Wuhan city, central China and is closely associated with male sex, old age, obesity and other metabolic syndrome features. The strategies for the prevention of this emerging disease in central China need to be further pursued.
Acknowledgements
We thank Prof Guanmin Chen, Dr Qin Liu for their valuable advice on statistical analysis and Prof Changjie Song for his assistance with critical revision of the manuscript in English language.
Abbreviations
ALT - alanine aminotransferase
BMI - body mass index
FLD - fatty liver disease
NAFLD - non‐alcoholic fatty liver disease
Footnotes
Funding: This work was supported by a grant from the Natural Science Foundation of Hubei province, China (2006ABA240).
Competing interests: None declared.
References
- 1.Bellentani S, Bedogni G, Miglioli L.et al The epidemiology of fatty liver. Eur J Gastroenterol Hepatol 2004161087–1093. [DOI] [PubMed] [Google Scholar]
- 2.Park S H, Kim B I, Yun J W.et al Insulin resistance and C‐reactive protein as independent risk factors for nonalcoholic fatty liver disease in non‐obese Asian men. J Gastroenterol Hepatol 200419694–698. [DOI] [PubMed] [Google Scholar]
- 3.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med 20023461221–1231. [DOI] [PubMed] [Google Scholar]
- 4.Angelico F, Del Ben M, Conti R.et al Non‐alcoholic fatty liver syndrome: a hepatic consequence of commonmetabolic diseases. J Gastroenterol Hepatol 200318588–594. [DOI] [PubMed] [Google Scholar]
- 5.Fan J G, Zhu J, Li J X.et al Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatol 200543508–514. [DOI] [PubMed] [Google Scholar]
- 6.Shao G X, Zhang X G, Huang Z P.et al The association between BMI and the distribution of fatty liver in 28348 people with physical examination in Shenzhen. Zhonghua ganzangbing zazhi 200311372–373. [PubMed] [Google Scholar]
- 7.Fan J G. Steatohepatitis studies in China. Shijie Huaren Xiaohua Zazhi 200196–10. [Google Scholar]
- 8.Lonardo A, Bellini M, Tartoni P.et al The bright liver syndrome. Prevalence and determinants of a ‘bright' liver echopattern. Ital J Gastroenterol Hepatol 199729351–356. [PubMed] [Google Scholar]
- 9.Joseph A E, Saverymuttu S H, al‐Sam S.et al Comparison of liver histology with ultrasonography in assessing diffuse parenchymal liver disease. Clin Radiol 19914326–31. [DOI] [PubMed] [Google Scholar]
- 10.Fatty Liver and Alcoholic Liver Disease Study Group of Chinese Liver Disease Association Diagnostic criteria of nonalcoholic fatty liver disease. Zhonghua Gan Zang Bing Za Zhi 20031171. [PubMed] [Google Scholar]
- 11.Fatty Liver and Alcoholic Liver Disease Study Group, Chinese Liver Disease Association Diagnostic criteria of alcoholic liver disease. Zhonghua Gan Zang Bing Za Zhi 20031172. [PubMed] [Google Scholar]
- 12.Anuurad E, Shiwaku K, Nogi A.et al The new BMI criteria for Asians by the regional office for the western Pacific region of WHO are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health 200345335–343. [DOI] [PubMed] [Google Scholar]
- 13.Kojima S, Watanabe N, Numata M.et al Increase in the prevalence of fatty liver in Japan over the past 12 years: analysis of clinical background. J Gastroenterol 200338954–961. [DOI] [PubMed] [Google Scholar]
- 14.Park S H, Jeon W K, Kim S H.et al Prevalence and risk factors of non‐alcoholic fatty liver disease among Korean adults. J Gastroenterol epatol 200621138–143. [DOI] [PubMed] [Google Scholar]
- 15.Omagari K, Kadokawa Y, Masuda J.et al Fatty Liver in non‐alcoholic non‐overweight Japanese adults: incidence and clinical characteristics. J Gastroenterol hepatol 2002171098–1105. [DOI] [PubMed] [Google Scholar]
- 16.Nishizawa H, Shimomura I, Kishida K.et al Androgens decrease plasma adiponectin, an insulin‐sensitising adipocyte‐derived protein. Diabetes 2002512734–2741. [DOI] [PubMed] [Google Scholar]
- 17.James O F, Day C P. Non‐alcoholic steatohepatitis (NASH): a disease of emerging identity and importance. J. Hepatol 199829495–501. [DOI] [PubMed] [Google Scholar]
- 18.Marchesini G, Brizi M, Bianchi G.et al Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 2001501844–1850. [DOI] [PubMed] [Google Scholar]
- 19.Sanyal A J. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology 20021231705–1725. [DOI] [PubMed] [Google Scholar]
- 20.Marceau P, Biron S, Hould F S.et al Liver pathology and the metabolic syndrome X in severe obesity. J Clin Endocrinol Metab 1999841513–1517. [DOI] [PubMed] [Google Scholar]
- 21.Marchesini G, Bugianesi E, Forlani G.et al Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 200337917–923. [DOI] [PubMed] [Google Scholar]
- 22.Ford E S, Giles W H, Dietz W H. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA 2002287356–359. [DOI] [PubMed] [Google Scholar]
- 23.Ruhl C E, Everhart J E. Determinants of the association of overweight with elevated serum alanine aminotransferases activity in the United States. Gastroenterology 200312471–79. [DOI] [PubMed] [Google Scholar]
- 24.Li Y M, Chen W X, Yu C H.et al An epidemiological survey of alcoholic liver disease in Zhejiang province. Zhonghua Gan Zang Bing Za Zhi 200311647–649. [PubMed] [Google Scholar]
- 25.Lu X L, Luo J Y, Tao M.et al Analysis of dangerous factors for alcoholic liver disease. Zhonghua Gan Zang Bing Za Zhi 200412442–443. [PubMed] [Google Scholar]