Abstract
In order to compensate for the low partial pressure of oxygen at altitude, the human body undergoes a number of physiological changes. A vital component in this process is the increase in the concentration of circulating haemoglobin. The role of HIF‐1α, erythropoietin and red blood cells in this acclimatisation process is described, together with the fall in plasma volume that increases the concentration of haemoglobin in the early stages of hypoxic exposure.
Keywords: altitude, erythropoietin, haemoglobin, hypoxia inducible factor, polycythaemia
Although estimates vary, it is thought that approximately 140 million people live above 2500 m, with the majority being found in Central Asia, East Africa, Central and South America (table 1).1
Table 1 The five countries with the largest populations living above 2500 m1.
| Country | Estimated population living above 2500 m (millions) | Estimated percentage of the total population (%) |
|---|---|---|
| India | 26.82 | 3 |
| China | 22.09 | 2 |
| Mexico | 14.05 | 15 |
| Pakistan | 14.05 | 10 |
| Ethiopia | 13.76 | 25 |
The greatest challenge facing humans at altitude is the reduction in the partial pressure of oxygen that results from a fall in barometric pressure. When faced with this hypoxic challenge, the body responds in a number of different ways depending upon the rate and severity with which the stimulus is imposed. The acute hypoxia suffered by aviators in an unpressurised aircraft generates a very different set of physiological responses than the more chronic form experienced by mountaineers, who typically take several weeks to reach similar heights. It is striking to note that someone who ascends rapidly from sea level to the summit of Mt Everest (8850 m) will lose consciousness within seconds, while those who have spent several weeks ascending can often function relatively well. The physiological changes which allow this to occur are grouped together under the term “acclimatisation”, while change that occurs over many generations in high altitude populations is known as “adaptation”. In order to cope with hypoxia, the body attempts to maximise the delivery of oxygen to the tissues. Within minutes of arriving at altitude this is manifest by an increase in cardiac output and minute ventilation.2 Over time, additional improvements occur in both the circulation and tissues that enhance the acclimatisation process further. This review will focus upon perhaps the most widely known change seen on ascent to altitude, that is the increase in the concentration of haemoglobin.
Early historical developments
In 1674 Anthony Von Leeuwenhoeck announced to members of the Royal Society, “I have observed, taking some blood out of my hand, that it consists of small round globules driven through a crystalline humidity of water”.3
This, the first recorded description of a red blood cell (erythrocyte), would provide the starting point for a clear description of the constituents of the cell and finally, an understanding of its origins and function. At the University of Bologna in 1747, Vincenzo Menghini demonstrated the presence of iron in red cells by burning blood and showing that its ashes were attracted to a magnet.3 Later, Jons Jacob Berzelius distinguished between the protein “globulin” and the pigmented “haem” compound contained in the cell, before correctly identifying that the latter component carried the iron moiety.4 Subsequent experiments conducted by Johannes Mulder determined the composition of the “haem” component and demonstrated that the pigmented structure was responsible for carrying oxygen.5 By the middle of the nineteenth century, Felix Hoppe Seyler was able to crystallise the molecule and finally named it “haemoglobin”. Seyler would later go on to describe the formation of “oxyhaemoglobin” following the reaction of haemoglobin with oxygen.6 In 1865 Seyler presented his results to his colleague Paul Bert (fig 1). By exposing animals to a range of different barometric pressures, Bert was able to describe for the first time a rudimentary oxyhaemoglobin dissociation curve.7
Figure 1 Paul Bert, considered by many to be the father of high altitude physiology.
Bert is considered by many to be the father of high altitude physiology. With the publication of La Presson Bariometrique in 1878, Bert was the first to make the connection between the problems humans faced at high altitude and the fall in barometric pressure.8 This work had been prompted in large part by fellow Frenchman and physician Denis Jourdanet.9 Jourdanet had spent almost 20 years practising medicine at high altitudes in Mexico and had focused much of his attention on the effects of high altitude on humans. With Jourdanet's subsequent encouragement and financial support, Bert was able to build one of the earliest pressure chambers in his laboratory and was able to demonstrate that by breathing supplemental oxygen in hypoxic conditions, the symptoms of acute mountain sickness could be treated.
During his time in Mexico, Jourdanet observed a consistent increase in the viscosity of human blood at high altitude. This would lead Bert to correctly hypothesise that such a change was due to an increase in the concentration of red cells in the circulation. However, it would take another Frenchman, Francois‐Gilbert Viault to confirm this, when in 1890 he found that after 23 days at 4392 m, his own red cell count had risen from 5 to 8 million per cubic millimetre.10 In later studies on lowland Europeans and Peruvian high altitude residents, Viault was able to confirm what is now commonly known – haemoglobin concentrations rise on ascent to altitude.
Twentieth century and beyond
The response of lowlanders to hypoxia
In 1906 Carnot and Deflandre, two scientists at the University of Paris, took the understanding of haemoglobin one step further. By injecting the serum of bleeding rabbits into otherwise healthy animals, they were able to demonstrate an increase in the red cell concentrations of the transfused animals. This, the authors felt, had shown “the presence of a substance haemopoietin [erythropoietin] capable of activating haemopoiesis and of rapidly provoking in normal animals, a high constant hyperglobulism”.11
Although it would take almost 50 years to demonstrate the effect of erythropoietin (EPO) on erythroid cell lines in humans, the structure and origins of the molecule would soon follow. However, it was not until the discovery of hypoxia inducible factor‐1α (HIF‐1α), largely as a result of Greg Semenza's work in the 1990s, that the agent responsible for EPO release was discovered.12,13 Under normoxic conditions, HIF‐1α has one of the shortest half lives of any normal protein, binding to the Von Hippel Lindau (VHL) protein inside healthy cells before rapidly degrading.14 However, under hypoxic conditions HIF‐1α resists VHL and instead binds to HIF‐1β to form HIF.15 This molecule subsequently binds to the EPO gene on chromosome 7 and stimulates red cell production. In Chuvash polycythaemia, a recessive condition common in parts of the former Soviet Union, abnormalities in the VHL protein prevent HIF‐1α from degrading under normoxic conditions.16 The consequences for those with this condition are the same as those seen in individuals ascending to altitude – an increase in HIF, EPO and red cell production.
As a protein that is being constantly being produced and degraded in cells, HIF‐1α responds to hypoxia rapidly. Within an hour of exposure to hypoxia, HIF‐1α concentrations peak and trigger an almost immediate rise in the concentration of circulating EPO.17 Increases in EPO are strongly related to the altitude reached, with a rise of 30% at 1900 m compared to 300% at 4500 m.18 Interestingly, absolute values can vary by as much as +400% to −40% among individuals exposed to 3000 m over a period of 24 h.19 The reasons for this variation are unclear, although it is thought that subtle polymorphisms in the EPO gene may make a significant contribution.20 During a prolonged stay at altitude, EPO levels continue to rise for up to 3 days before eventually returning to normal after 3 weeks.21 Recently, it has been suggested that this fall may be relative, with production of EPO remaining high throughout and the consumption of EPO gradually increasing over the first month of exposure. This would result in an apparent fall in EPO concentration, despite EPO production remaining high.22 Once bound to the erythroid cells in the bone marrow, EPO triggers an increase in iron turnover and a doubling of nucleated red cells within 7 days of exposure to moderate altitude.23 In a long term study conducted over a year, the increase in red cell production has been shown to continue for up to 8 months and result in an increase in red cell mass of 50%.24
Despite such an enormous change, the increase in haemoglobin concentration appears to be even more dramatic during the first few weeks spent at altitude. The reason for this was first identified in 1952 by Lawrence et al who measured changes in the circulation with autologous red cells labelled with radioactive phosphorous and found that plasma volume fell shortly after ascending to altitude.25 This was confirmed almost a decade later by Pugh, the physiologist assigned to the first successful expedition to Mt Everest in 1953 and the scientific leader of the landmark “Silver Hut” scientific expedition to the Khumbu region of Nepal in 1960–126 (fig 2).
Figure 2 The “Silver Hut” expedition, a landmark in high altitude research. Photograph courtesy of JB West.
Following 18 weeks above 4000 m, Pugh identified a 21% reduction in the plasma volume of four healthy expedition members. However over the following 3 months this deficit narrowed and resulted in just a 10% reduction by the end of the expedition.26 This transient fall in plasma volume has the potential to provide mountaineers with an important boost during the first few weeks at altitude. Although volumes of haemoglobin are only just starting to rise, a sudden reduction in plasma volume can rapidly increase the concentration of haemoglobin and therefore enhance the carriage of oxygen for any given volume of blood.
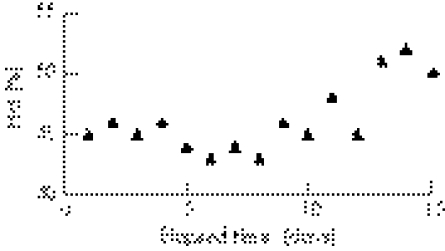
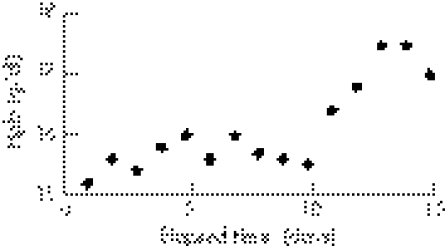
Previously unpublished data from the 2005 Xtreme Everest Expedition to Cho Oyu (8201 m) demonstrate that large increases in haematocrit and haemoglobin concentration occurred during the 15 day journey from Kathmandu (∼1530 m) to advanced base camp (∼5700 m) (figs 3 and 4).
Figure 3 The mean values of haematocrit (Hct) seen in four mountaineers ascending from 1530 m to advanced base camp (5700 m) on Cho Oyu (8201 m).
Figure 4 The mean values of haemoglobin (Hgb) concentration seen in four mountaineers ascending from 1530 m to advanced base camp (5700 m) on Cho Oyu (8201 m).
A rapid increase in the concentration of haemoglobin provides mountaineers with a means to compensate for the dramatic fall in arterial oxygen saturation seen at altitude (table 2).
Table 2 Content of oxygen in the blood at 1530 m and at Cho Oyu advanced base camp (5700 m).
| Day 1: 1530 m | Day 14: 5700 m | |
|---|---|---|
| Arterial oxygen saturation (Sao2) | 95 | 82 |
| Haemoglobin concentration (g/dl) | 15.2 | 17.5 |
| Oxygen delivered by haemoglobin | 19.3 | 19.2 |
| to the tissues (ml/100 ml blood) |
Despite a fall in arterial oxygen saturation, the content of oxygen in the blood remains unchanged at Cho Oyu advanced base camp (5700 m) due to a significant increase in haemoglobin concentration.
Although a small increase in haemoglobin would normally be expected over the first few weeks at altitude, the increase in concentration seen here (approximately 2 g/dl) is largely due to a redistribution of total body water, with fluid being shifted from the circulation and deposited into the interstitial space. Unfortunately, the factors responsible for this shift are unclear and despite a number of different studies that have examined the behaviour of the sympathetic nervous system and a range of different hormones at altitude, we are still no closer to explaining this phenomenon.
The response of high altitude residents to hypoxia
As Viault demonstrated more than a century ago, sea level and high altitude residents both experience an increase in haemoglobin on ascending to higher altitudes. Although the final concentration can vary, the increase is largely dependent upon the altitude reached and the individual's arterial oxygen saturation.27 Underlying this similarity is the knowledge that the structure and function of haemoglobin molecules vary little between different ethnic groups. Although the incidence of haemoglobinopathies (such as sickle cell disease and β‐thalassaemia) may vary between populations, the behaviour of HIF, EPO and red cells when exposed to hypoxia is broadly similar.1 Despite this, considerable variation exists in the final concentration of haemoglobin between different ethnic groups resident at moderate altitude. Over the last two decades Cynthia Beall and her colleagues have conducted a number of meticulous studies comparing the haemoglobin concentrations of residents in Bolivia, Tibet and Ethiopia living at altitudes of 3500–4000 m29,30,31,32 (table 3).
Table 3 Haemoglobin concentrations in residents living at 3500–4000 m and at sea level.
| Haemoglobin in males (g/dl) | Haemoglobin in females (g/dl) | |
|---|---|---|
| Sea level | 15.3 | 13.4 |
| Bolivia | 17.9 | 16.8 |
| Tibet | 16.7 | 15.0 |
| Ethiopia | 15.9 | 15.0 |
In a comparison between Bolivian and Tibetan residents, Beale and her colleagues were able to control for a range of potential conflicting factors including concurrent medical illnesses, dietary deficiencies, occupation, cigarette smoking and exposure to fossil fuel smoke. This subsequently allowed the authors to demonstrate that genetic factors accounted for more than 85% of the difference between the two groups and led them to conclude that the difference was due to Tibetans undergoing a much longer period of adaptation. Although high altitude residents have been present in the Altiplano regions of the Andes for approximately 9000–12 000 years, the Himalayan plateau has been populated by humans for more than 50 000 years and it is this difference that has provided Tibetans with a longer period to adapt to hypoxia and subsequently develop a lower concentration of haemoglobin.
A normal haemoglobin concentration is vital for longevity and is well demonstrated by the huge variance in life expectancy (42 v 70 years) between those with Chuvash polycythaemia and matched controls.16 This enormous difference is largely due to the increase in viscosity caused by the high concentration of red cells in the circulation that results in an increased incidence of heart failure and thrombo‐embolic disease. Over the course of 50 000 years, Tibetan residents have undergone considerable natural selection that has discouraged the survival and reproductive success of those with high haemoglobin concentrations. By comparison, the Andean natives, whose ancestors moved to high altitude relatively recently, have not yet achieved an equivalent level of adaptation. This is compounded by the widespread colonisation of Andean communities which has led to out‐breeding with low altitude residents.
In order to maintain low levels of haemoglobin and still deliver adequate amounts of oxygen to the tissues, Tibetan residents have made a unique adaptation. Following exposure to low partial pressures of oxygen, humans respond by increasing the rate and depth of their breathing in order to ensure adequate oxygenation. Although this hypoxic ventilatory response (HVR) varies considerably between humans, a pattern has emerged. In a comparison between Tibetan and Andean high altitude residents, Tibetans have been found to have a higher HVR and as a consequence an increase in resting minute ventilation.32 This would suggest that the blunted HVR of Andean residents might limit the delivery of oxygen to the tissues and therefore promote an increase in red cell production with potentially detrimental effects. A low HVR also contributes to the development of chronic mountain sickness (CMS), a condition found in some high altitude residents which is characterised by abnormally high concentrations of haemoglobin. The resulting clinical problems faced by those with CMS are similar to those seen in Chuvash polycythaemia.33 Interestingly, current evidence seems to infer that CMS is much more common in the Andean population, suggesting that without sufficient “time” for adaptation, populations at altitude can face considerable difficulties.34
Unlike the genetic changes made by Tibetan high altitude residents, little is known about how Ethiopians have adapted to their environment. However, unlike Tibetans, Ethiopians have consistently high arterial oxygen saturations despite the hypoxic environment, suggesting that natural selection may have led to improved oxygen delivery to the circulation and an increase in oxygen affinity of red blood cells.30
Conclusion
Since Von Leeuwenhoeck's discovery of “small round globules” almost 400 years ago, scientists have been able to identify, in detail, the structure and function of haemoglobin. More recently, the discovery of HIF‐1α has identified the trigger for increases in EPO and red cell production under hypoxic conditions. These developments will continue to provide the basis for future research that explores the process of acclimatisation at both the cellular and molecular level. This will focus not only on red blood cells but also on the tissues they supply. Fascinating research opportunities surely beckon!
Abbreviations
CMS - chronic mountain sickness
EPO - erythropoietin
HIF‐1α - hypoxia inducible factor‐1α
HVR - hypoxic ventilatory response
VHL protein - Von Hippel Lindau protein
Footnotes
Competing interests: None.
References
- 1.Niermeyer S, Zamudio S, Moore L G. The people. In: Hornbein TF, Schoene RB, eds. High altitude – an exploration of human adaptation. New York: Marcel Dekker, 200143–100.
- 2.Ward M P, Milledge J S, West J B.High altitude medicine and physiology. London: Arnold, 200044–49.
- 3.Houston C.Going higher. Seattle: The Mountaineers, 199857–58.
- 4.Berzelius J J.Förelãsninger över djurkemien. Stockholm: Marquad, 1806–08, vol 1–2,
- 5.Severinghaus J W, Astrup P, Murray J F. Blood gas analysis and critical care medicine. Am J Respir Crit Care Med 1998157114–122. [DOI] [PubMed] [Google Scholar]
- 6.Hoppe‐Seyler F. ?ber das verhalten des blutfarbstoffes im spectrum des sonnenlichtes. Arch Pathol Anat Physiol 186223446 [Google Scholar]
- 7.West J B.High life: a history of high altitude physiology and medicine. New York: Oxford University Press, 199840–73.
- 8.Bert P.La pression barométrique: recherches de physiologie expérimentale. Paris: Masson, 1878
- 9.Bert P.Barometric pressure: researches in experimental physiology. Columbus, OH: College Book Company, 1943
- 10.Viault F. On the large increase in the number of red cells in the blood of the inhabitants of the high plateaus of South America. In: West JB, ed. High altitude physiology. Stroudsburg, PA: Hutchinson Ross, 1981333–334.
- 11.Carnot P, Deflandre C. Sur l'activite haemopoietique du serum. Compt Rend Acad D Sc 1906143432–435. [Google Scholar]
- 12.Semenza G L. Regulation of erythropoietin production. New insights into molecular mechanisms of oxygen homeostasis. Hematol Oncol Clin North Am 19948863–884. [PubMed] [Google Scholar]
- 13.Semenza G L, Roth P H, Fang H M.et al Transcription regulation of genes encoding glycolytic enzymes by hypoxia‐inducible factor 1. J Biol Chem 199426923757–23763. [PubMed] [Google Scholar]
- 14.Wang G L, Jiang B H, Rue E A.et al Hypoxia‐inducible factor 1 is a basic‐helix‐loop‐helix‐PAS heterodimer regulated by cellular oxygen tension. Proc Natl Acad Sci U S A 1995925510–5514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang G L, Semenza G L. Molecular basis of hypoxia‐induced erythropoietin expression. Curr Opin Haematol 19963156–162. [DOI] [PubMed] [Google Scholar]
- 16.Gordeuk V R, Sergueeva A I, Masnikova G Y.et al Congenital disorder of oxygen sensing: association of the homozygous Chuvash polycythaemia VHL mutation with thrombosis and vascular abnormalities but not tumours. Blood 2004103(10)3924–3932. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt W. Effects of intermittent exposure to high altitude on blood volume and erythropoietic activity. High Alt Med Biol 20023(2)167–176. [DOI] [PubMed] [Google Scholar]
- 18.Mottram D R.Drugs in sport. 4th edn. London: Routledge, 2005229
- 19.Ri‐Li G, Witkowski S, Zhang Y.et al Determinants of erythropoietin release in response to short term, hypobaric hypoxia. J Appl Physiol 2002922361–2367. [DOI] [PubMed] [Google Scholar]
- 20.Witkowski S, Karlsen T, Resaland G.et al Optimal altitude for “living high‐training low” [abstract]. Med Sci Sports Exerc 200133S292 [Google Scholar]
- 21.Abbrecht P H, Littell J K. Plasma erythropoietin in men and mice during acclimatization to different altitudes. J Appl Physiol 19723254–58. [DOI] [PubMed] [Google Scholar]
- 22.Grover R F, Bärtsch P. Blood. In: Hornbein TF, Schoene RB, eds. High altitude – an exploration of human adaptation. New York: Marcel Dekker, 2001493–523.
- 23.Huff R L, Lawrence J H, Siri W E.et al Effects of changes in altitude on haemopoietic activity. Medicine 195130197–217. [DOI] [PubMed] [Google Scholar]
- 24.Refnaforje C, Lozano R, Valdivieso S. The polycythaemia of high altitude: iron metabolism and related aspects. Blood 195914433–455. [PubMed] [Google Scholar]
- 25.Lawrence J F, Huff R L, Siri W.et al A physiological study in the Peruvian Andes. Acta Med Scand 1952142117–131. [DOI] [PubMed] [Google Scholar]
- 26.Pugh L G C E. Blood volume and haemoglobin concentration at altitudes above 18000 feet (5500 m). J Physiol 1964170344–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levine B D. Intermittent hypoxic training: fact and fantasy. High Alt Med Biol 20023(2)177–193. [DOI] [PubMed] [Google Scholar]
- 28.Vasquez R, Villena M. Normal haematological values for healthy persons living at 4000 meters in Bolivia. High Alt Med Biol 20012(2)361–367. [DOI] [PubMed] [Google Scholar]
- 29.Beall C M, Brittenham G M, Macuaga F.et al Variation in haemoglobin concentration among samples of high‐altitude natives in the Andes and the Himalayas. Am J Hum Biol 19902639–651. [DOI] [PubMed] [Google Scholar]
- 30.Beall C M, Decker M J, Brittenham G M.et al An Ethiopian pattern of human adaptation to high altitude hypoxia. Proc Natl Acad Sci U S A 200299(26)17215–17218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beall C M, Brittenham G M, Strohl K P.et al Hemoglobin concentration of high‐altitude Tibetans and Bolivian Aymara. Am J Phys Anthropol 1998106385–400. [DOI] [PubMed] [Google Scholar]
- 32.Beall C M, Strohl K P, Blangero J.et al Ventilation and hypoxic ventilatory response of Tibetan and Aymara high altitude natives. Am J Phys Anthrop 1997104427–447. [DOI] [PubMed] [Google Scholar]
- 33.Severinghaus J W, Bainton C K, Carcelen C. Respiratory insensitivity to hypoxia in chronically hypoxic man. Respir Physiol 19661308–334. [DOI] [PubMed] [Google Scholar]
- 34.Moore L G, Asmus I, Curran L. Chronic mountain sickness: gender and geographical variation. In: Ohno H, Kobayashi , Masuyama S , et al eds. Progress in mountain medicine and high altitude. Matsumoto, Japan: Press Committee on Mountain Medicine and High Altitude Physiology, 1998114–119.