Abstract
Background
The National Service Framework for coronary heart disease (CHD) defines standards for the secondary prevention of cardiovascular disease in at risk individuals, including those with peripheral arterial disease (PAD).
Aim
To assess current standards of secondary prevention and health monitoring in patients with PAD following a vascular procedure, and additionally compare care in patients with and without diagnosed CHD.
Methods
Indicators for this cross sectional survey were identified from national recommendations and evidence. A retrospective review was conducted of general practitioner records, for patients who were treated in hospital for PAD.
Results
Data were collected for 103 patients from 42 practices. Overall, prescribing was well achieved for antiplatelets but poor for statins. Standards of assessment of blood pressure, smoking status, and smoking cessation advice were high. However, approximately only half of the patients received advice about exercise or had their body mass index checked. Furthermore, for all indicators, standards of care for patients who additionally had a diagnosis of CHD were better than for patients without CHD.
Conclusion
The cross sectional survey suggested the treatment received by some patients with established PAD is substandard. There is considerable potential to increase secondary prevention of CHD in patients with PAD disease in primary care.
The National Service Framework for coronary heart disease (CHD)1 published in 2000 defines national standards for the application of appropriate secondary prevention measures to those at risk of cardiovascular disease, including those with peripheral arterial disease (PAD). Symptoms of coronary artery disease or electrocardiographic abnormality are found in half of patients presenting with PAD, and coronary angiography abnormalities and duplex evidence of carotid artery disease have been found in 90% and 40%, respectively.2 Furthermore, PAD has been found to be an independent predictor of increased risk of cardiovascular death. In patients with symptomatic PAD there is a 30% risk of death within 5 years and nearly 50% within 10 years, primarily due to myocardial infarction (MI) (60%) or stroke (12%).2 An aggressive approach is therefore required to modify risk factors to reduce the risk of fatal and non‐fatal MI and stroke in patients with PAD.2
Currently the management of patients with established CHD is substandard,3,4 and even when recommendations are implemented there is much variation in the care that patients receive.5 Secondary prevention strategies in patients with PAD are likely to be worse than for patients with CHD. For example, a recent study focusing on cholesterol management in general practice showed that patients with stroke or PAD achieved poorer cholesterol control than those with CHD. In this study approximately 50% of patients with PAD and 43% with a stroke had cholesterol values <5 mmol/l compared to 60% of patients with CHD.6
The objectives of this cross sectional survey were:
to assess current standards of secondary prevention measures and health monitoring in patients with PAD following a vascular procedure
to compare standards of secondary prevention in patients with PAD with and without diagnosed CHD.
Methods
Design
The survey was designed as a retrospective record review of general practitioner (GP) held medical records (paper and electronic). Evidence based indicators for the study were identified from national recommendations and evidence,1,2,7,8,9,10,11,12 (table 1). A structured data collection form was designed to collect data for each indicator and relevant supplementary information.
Table 1 Standards achieved for evidence based indicators.
| Evidence based indicator. The patient record shows that: | All patients | Patients with diagnosed CHD | Patients with no diagnosed CHD | |
|---|---|---|---|---|
| n = 103* | ||||
| (%; PCT % range) | n = 39* (%) | n = 64* (%) | ||
| 1: | Aspirin or clopidogrel is currently prescribed unless contraindicated | 81/92 (88.0; 84–94) | 35/35 (100) | 46/57 (80.7) |
| 2a: | Cholesterol has been checked in the past 12 months | 73† (70.9; 67–83) | 33†/39 (84.6) | 40/64 (62.5) |
| 2b: | Cholesterol value is ⩽5 mmol/l | 54/72‡ (75.0; 72–80) | 28/32‡ (87.5) | 26/40 (65.0) |
| 2c: | A statin is currently prescribed if cholesterol value was >5 mmol/l, unless contraindicated | 8/15§ (53.3; 25–100) | 4/4 (100) | 4/11 (36.4) |
| 3a: | Blood pressure has been checked in the past 12 months | 90 (87.4; 83–89) | 39/39 (100) | 51/64 (79.7) |
| 3b: | Blood pressure is <140/85 mm Hg | 43/90 (47.8; 41–53) | 19/39 (48.7) | 24/51 (47.1) |
| 4a: | Smoking status has been checked in the past 12 months | 85 (82.5; 78–88) | 38/39 (97.4) | 47/64 (73.4) |
| 4b: | Cessation advice/health education was given if patient was a smoker | 21/22 (95.5; 90–100) | 8/8 (100) | 13/14 (92.9) |
| 5: | Exercise advice re: walking given in the past 12 months, unless contraindicated | 47/84¶ (56.0; 46–75) | 27/35 (77.1) | 20/49 (40.8) |
| 6: | BMI has been checked in the past 12 months, unless contraindicated | 46/92** (50.0; 43–56) | 26/37 (70.3) | 20/55 (36.4) |
BMI, body mass index.
*n is less when criterion is not applicable to all patients.
†Includes 1 patient who had cholesterol check carried out within 4 weeks of the survey but result (level) missing.
‡Cholesterol value not available for 1 patient who was checked.
§Statin contraindicated (3 patients).
¶Exercise advice (walking) contraindicated due to severe mobility problems (19 patients).
**BMI contraindicated due to leg amputation(s) (11 patients).
The six primary care trusts (PCTs) in Leicestershire were approached and asked if they were willing to participate in the multi‐practice survey. Three PCTs agreed to participate and a letter of invitation was then sent to all 87 general practices identified in the three PCTs at that time. Practices who failed to respond were sent a second letter. If no reply was received after the second letter a follow up telephone call was made to the practices.
Patients whose records were eligible for the survey were identified from Strategic Health Authority records as having undergone a vascular procedure in 2003 for PAD (amputation, arterial grafting, endarterectomy, or balloon angioplasty) in the year 1 January 2003 to 31 December 2003 inclusive. The study population included all patients admitted/discharged from two of the University Hospitals of Leicester (Leicester Royal Infirmary, Leicester General Hospital) with a diagnosis of PAD, and registered with a GP in the six PCTs in Leicestershire. Exceptions were: patients who had more than one procedure for PAD in the year reviewed (data were collected for the last admission only); patients who died at any time between date of procedure and date of survey; patients who had left their registered GP since the procedure.
A research associate collected data for patients in the recruited practices between September 2005 and March 2006. Data collected were entered into a database and basic statistical analysis undertaken using Excel and SPSS to measure standards of care.
This cross sectional survey was carried out as part of a local quality assurance programme between primary and secondary care. As such it constituted the first stage of a planned audit conducted to identify and compare levels of care; therefore, statistical significance was not sought in our analysis of the data collected. Additionally, the survey did not require ethics committee approval.
Results
Number of practices taking part and patient records reviewed
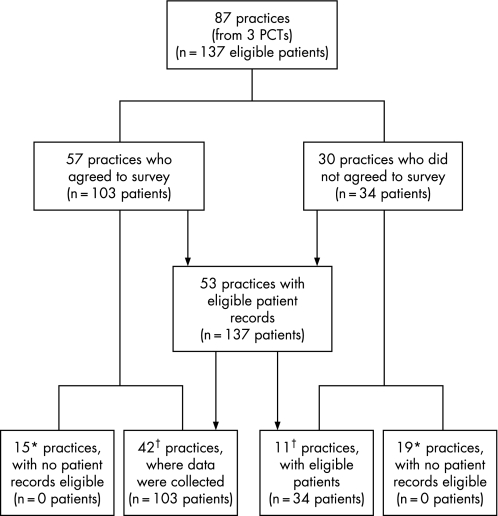
Three of the six PCTs agreed to participate and of the 87 practices in these three PCTs, 53 had eligible patients (fig 1). Of these, 42 (79%) agreed to take part in the survey. In total, 137 eligible patients were identified and data were collected for 103 (75%). The median number of patient records reviewed per practice was 2 (range 1–7).
Figure 1 Practices and patients included in the cross‐sectional survey. PCTs, primary care trusts. *No patients registered at practice at time of audit who had a procedure in 2003 for PAD. †Total number of eligible practices = 42+11 = 53.
Practice characteristics
A higher proportion of practices who participated were teaching practices and group practices compared to those who declined to take part (table 2). Teaching practices represented 18% of eligible practices who did not agree, compared to 43% of practices where data were collected. Group practices represented 64% of eligible practices who did not agree, compared to 83% of practices where data were collected.
Table 2 Characteristics of practices in three participating primary care trusts.
| Characteristics of practices: | All practices | Practices with eligible patient records | Practices with eligible patient records who did not agree | Practices where audit data were collected |
|---|---|---|---|---|
| n = 87 | n = 53 | n = 11 | n = 42 | |
| Training status: n (%) | ||||
| Teaching practice | 21 (24.1) | 20 (37.7) | 2 (18.2) | 18 (42.9) |
| Non‐teaching practice | 66 (75.9) | 33 (62.3) | 9 (81.8) | 24 (57.1) |
| Number of GPs: n (%) | ||||
| Group practice | 62 (71.3) | 42 (79.2) | 7 (63.6) | 35 (83.3) |
| Single‐handed | 25 (28.7) | 11 (20.8) | 4 (36.4) | 7 (16.7) |
GPs, general practitioners.
Patient characteristics
Characteristics of patients in our sample are shown in table 3. A higher proportion of patients whose records were reviewed was male (62%) than female (38%). The mean (SD) age for all patients was 73 (11.0) years, although females were on average older than males (77 (11.0) years for females, and 70 (10.0) years for males). The mean (SD) number of months since the procedure was carried out for PAD was 29 (3.6).
Table 3 Characteristics of patients whose records were reviewed.
| Variables | All patients n = 103* |
|---|---|
| Age in years: | |
| All patients, mean (SD) | 73 (11.0) |
| Female, mean (SD) | 77 (11.0) |
| Male, mean (SD) | 70 (10.0) |
| Gender: | |
| Female, n (%) | 39 (37.9) |
| Male, n (%) | 64 (62.1) |
| Co‐morbidity, past medical history of, n (%): | |
| Hypertension | 71 (68.9) |
| Atrial fibrillation | 12 (11.7) |
| Angina | 32 (31.1) |
| MI | 19 (18.4) |
| Stroke/CVA/TIA | 23 (22.3) |
| Cardiovascular disease (stroke, angina or MI) | 51 (49.5) |
| Diabetes, type 1 | 3 (2.9) |
| Diabetes, type 2 | 27 (26.2) |
| History of smoking, ever* | 70/89* (78.7) |
| Vascular symptoms before procedure, n (%): | |
| Intermittent claudication | 75 (72.8) |
| Ischaemic rest pain | 38 (36.9) |
| Arterial ulceration | 34 (33.0) |
| Arterial gangrene | 9 (8.7) |
| Ischaemic rest pain, or arterial ulceration or gangrene | 54 (52.4) |
| Months since vascular procedure, mean (SD) | 29 (3.6) |
| Previous vascular procedure†, n (%) | 48/101† (47.5) |
CVA, cerebrovascular accident; MI, myocardial infarction; TIA, transient ischaemic attack.
*Data available for 89 patients only.
†Data available for 101 patients only.
Overall 69% of patients had a history of hypertension, and 50% of patients had cardiovascular disease (diagnosed with one or more of stroke, angina, or MI). In addition, although only 26% of patients were current smokers, 79% of patients had a history of smoking ever (current smoker or ex‐smoker).
Current standards of practice
Table 1 shows current standards of practice for our survey sample.
Secondary prevention: prescribing
Prescription rates of medication for secondary prevention measures were well achieved for aspirin or clopidogrel (88%) but much lower for statins (68% for all patients, and 53% currently for patients with cholesterol value >5 mmol/l).
Health monitoring and prevention in the preceding 12 months
Annual blood pressure monitoring (87%), smoking status check (83%), and cessation advice to current smokers (96%) were all well achieved. The proportion of patients who had a cholesterol check was less well achieved (71%) and the percentages of patients who had their body mass index (BMI) checked (50%) or whose records indicated that they had received exercise (walking) advice (56%) were even lower.
Intermediate outcomes of care
Cholesterol value ⩽5 mmol/l was achieved for 75% of patients but blood pressure <140/85 mm Hg was achieved for only 48%. However, 85% of patients with a blood pressure ⩾140/85 mm Hg were currently prescribed antihypertensive medication.
Standards of secondary prevention in patients with PAD and diagnosed CHD compared to PAD patients with no diagnosed CHD
Standards of care for patients who had undergone a recent procedure for PAD and additionally had a diagnosis of CHD were better than for patients who had PAD without diagnosed CHD, for all indicators (table 1). Blood pressure control showed only a very marginal difference (49% in patients with CHD and 47% in patients with no CHD). However, statin prescribing, exercise advice and assessment of BMI showed very noticeable differences between patients with PAD with and without diagnosed CHD (statin if total cholesterol >5 mmol/l, 100% vs 36%; exercise advice, 77% vs 41%; BMI check, 73% vs 40%).
Discussion
Summary of main findings
This cross sectional survey suggests that standards of secondary prevention measures in patients with symptomatic PAD recently discharged from secondary care following a vascular procedure are suboptimal. Additionally, in our sample, standards of secondary prevention in patients with PAD without a diagnosis of CHD were much poorer than for patients with both diagnoses. This is in spite of PAD being an independent risk factor for fatal and non‐fatal MI.
Strengths and limitations
It is acknowledged that our results may not be a true reflection of secondary prevention in all practices as only 53 (61%) of the 87 practices in the three participating PCTs were eligible to take part in the survey. However, the other 34 practices did not have any patients who were discharged following a vascular procedure for PAD in 2003, and overall we collected data for 75% of eligible patients. There were some differences in the characteristics of eligible practices who did not agree to the survey compared to those that participated, in terms of teaching status and the proportion of practices that were single handed (table 2). However, these differences are unlikely to have had a substantial impact as the differences were not statistically significant.
The small number of patient records reviewed at some practices may limit the representativeness of the findings. As patient records were reviewed approximately 2 years following admission there was some loss of cases due to deaths or patients having left the practice where they were registered at the time of their vascular procedure.
Comparison with other studies
Our sample was small compared to a recent audit of cholesterol management in cardiovascular disease in English general practices,6 which included a subset of 3617 patients with PAD. In the latter study 50% of patients with PAD had a cholesterol value ⩽5 mmol/l compared to 75% of patients in our survey. However, our survey considered only PAD patients who had undergone a recent vascular procedure and were therefore of higher risk, whereas the cholesterol management audit collected data on all patients with a diagnosis of PAD. A study conducted in secondary care in the USA,13 which looked at a similar group of patients to our survey, also found that patients received suboptimal treatment following discharge after undergoing a vascular procedure.
Compared to aggregated 2005/2006 CHD Quality and Outcomes Framework (QoF) data for smoking, blood pressure and cholesterol indicators in patients with established CHD,14 care for patients with PAD whose records we reviewed was substandard. The proportion of patients who had blood pressure, cholesterol and smoking status checks when records were reviewed were 87% for blood pressure, 71% for cholesterol and 83% for smoking status compared to 98%, 93% and 96%, respectively, for the QoF CHD data. However, our survey considered care in the previous 12 months whereas QoF data looks at a 15 month period. Although the proportions achieving total cholesterol values ⩽5 mmol/l were very similar (75% in this study vs 79% for QoF data), blood pressure targets were very poorly achieved (48% for patients with PAD vs 87% QoF). However, blood pressure targets in our study were lower than the QoF targets (<140/85 mm Hg and ⩽150/90 mm Hg, respectively). Standards of care for patients with PAD who additionally had a diagnosis of CHD were similar to the QoF CHD data, with the exception of blood pressure control.
The recently published Scottish Intercollegiate Guidelines Network (SIGN) guidelines on the diagnosis and management of peripheral arterial disease15 include guidance on secondary prevention of cardiovascular events. Indicators that were utilised in this survey are similar to the SIGN recommendations (smoking cessation, cholesterol lowering, blood pressure control, antiplatelet treatment). However, tighter control of cholesterol is recommended by SIGN, ⩽3.5 mmol/l compared to ⩽5.0 mmol/l in this survey.
Conclusion
In spite of national and international recommendations and strong evidence of an increased risk of death due to cardiovascular disease, currently the treatment received by some patients with established PAD is substandard. There is considerable potential to increase secondary prevention of CHD in patients with PAD, using appropriate evidence based management. More attention needs to be given to this group of patients in primary care in order to improve secondary prevention.
Acknowledgements
We would like to thank all the general practices who participated in this survey, and the Clinical Governance Leads. We wish to thank all staff at the Leicestershire PCAG for their assistance and acknowledge the contribution made by Champa Patel at the planning stage and in assisting with recruitment of PCTs. We would also like to acknowledge the contribution made by Hanna Blackledge in helping identify patient records to be reviewed.
Abbreviations
BMI - body mass index
CHD - coronary heart disease
GP - general practitioner
MI - myocardial infarction
PAD - peripheral arterial disease
PCTs - primary care trusts
SIGN - Scottish Intercollegiate Guidelines Network
QoF - Quality and Outcomes Framework
Footnotes
Funding: The Leicestershire Interface Audit Group provided the funding for this cross‐sectional survey.
Competing interests: None declared.
References
- 1.Department of Health National Service Framework: coronary heart disease. London: Department of Health, 2000
- 2.Tierney S, Fennessy F, Hayes D B. ABC of arterial and vascular disease. Secondary prevention of peripheral vascular disease. BMJ 20003201262–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khunti K, Sorrie R, Jennings S.et al Improving aspirin prophylaxis in post myocardial infarction patients in primary care: collaboration between a primary care audit group and a health authority in a multi‐practice audit. BMJ 1999319297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campbell N C, Thain J, Deans H G.et al Secondary prevention in coronary heart disease: baseline survey of provision in general practice. BMJ 19983161430–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunkley A, Stone M, Squire I.et al An audit of secondary prevention of coronary heart disease in post acute myocardial infarction patients in primary care. Quality in Primary Care 20061415–20. [Google Scholar]
- 6.De Lusignan S, Hague N, Belsey J.et al The ‘rule of halves' still applies to the management of cholesterol in cardiovascular disease. Br J Cardiol 200613145–152. [Google Scholar]
- 7.Antithrombotic Trialists' Collaboration Collaborative meta‐analysis of randomised trials of antiplatelet therapy for prevention of death myocardial infarction, and stroke in high risk patients. BMJ 200232471–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huyen T, Anand S. Oral antiplatelet therapy in cerebrovascular disease, coronary artery disease, and peripheral arterial disease. JAMA 20042921867–1874. [DOI] [PubMed] [Google Scholar]
- 9.Heart Protection Study Collaborative Group MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high risk individuals: a randomised placebo controlled trial. Lancet 20023607–22.12114036 [Google Scholar]
- 10.Mehler P, Coll J, Estacio R.et al Intensive blood pressure control reduces the risk of cardiovascular events in patients with peripheral arterial disease and type 2 diabetes. Circulation 2003107753–756. [DOI] [PubMed] [Google Scholar]
- 11.Heart Outcomes Prevention Evaluation Study Investigators Effects of an angiotensin converting enzyme inhibitor, ramipril, on cardiovascular events in high risk patients. N Engl J Med 2000342145–153. [DOI] [PubMed] [Google Scholar]
- 12.Leng G C, Fowler B, Ernst E. Exercise for intermittent claudication. Cochrane Database Systematic Reviews 2005(1)CD000990. [DOI] [PubMed]
- 13.Mukherjee D, Lingam P, Chetcuti S.et al Missed opportunities to treat atherosclerosis in patients undergoing peripheral vascular interventions. Circulation 20021061909–1912. [DOI] [PubMed] [Google Scholar]
- 14.Anon Quality and Outcomes Framework CHD indicator data. 2005–6. http://www.ic.nhs.uk/services/qof
- 15.Scottish Intercollegiate Guidelines Network Diagnosis and management of peripheral arterial disease. Edinburgh: SIGN; 2006, (SIGN publication no. 89). http://www.sign.ac.uk (accessed 20 November 2006)