Abstract
Objective
To assess the experience gained in digital rectal examination (DRE) by medical students in the Republic of Ireland by the completion of undergraduate training.
Methods
A national survey was conducted targeting all 582 final year students from the five medical schools completing their undergraduate studies in the summer of 2005. Format was anonymous questionnaire. Experience of DRE was defined as the student having performed at least one examination on either patient or teaching mannequin.
Results
In total, 396 (68%) of 582 students responded. No experience of DRE was reported in 97 (24%), with mannequin‐only experience in a further 78 (20%). Of the remaining 221 (56%) who performed DRE on at least one patient, one third (74) reported no confidence in their ability to interpret their findings properly.
Conclusion
Undergraduate training in DRE is limited. Training in DRE can no longer be reasonably considered part of the core curriculum taught in Irish medical schools.
Digital rectal examination (DRE) has been considered an essential skill for the trained medical doctor, with traditional undergraduate training always emphasising the need for familiarity with this simple diagnostic examination.1 DRE is required in all patients where a possible diagnosis may be facilitated.2 Traditionally a cornerstone of prostate cancer diagnosis, recent reports suggest the positive predictive value and sensitivity of DRE in the screening for prostate cancer is strongly dependent on serum prostate specific antigen (PSA) value. Indeed, DRE alone performs poorly as a screening modality at low PSA values.3 Despite this limitation, few dispute the need for DRE to remain in the diagnostic armamentarium of specialists in urology and coloproctology. Up to a third of rectal cancers are palpable and failure to perform DRE in these instances may clearly delay diagnosis.4 General physicians, however, acquire far less experience of DRE in routine practice. Outside the specialised areas already described, increasing numbers may no longer view this intrusive examination as part of a routine general physical examination.
The balance between the patient's right to be examined by competent trained personnel and the student's need to practise DRE before being considered trained is a difficult one. The General Medical Council has stated that medical students during training should acquire and become proficient in comprehensive physical examination, but no clear guidance is provided on how this is to be achieved.5 The Irish Medical Council's Guide to ethical conduct makes no direct reference to undergraduate training in DRE despite the intimate and intrusive nature of this examination.6 With an increasing medico‐legal awareness, proper procedures for medical students must be constructed and failure to comply may be considered criminal.7
In studies based in general practice within the UK, it has been found that confidence in performing and interpreting DRE was associated with the perception of having been well taught to do rectal examination while at medical school.8 This study has analysed the current practices in relation to undergraduate training of DRE on a national level within the Republic of Ireland. It involved the cooperation of all medical schools within the state.
METHODS
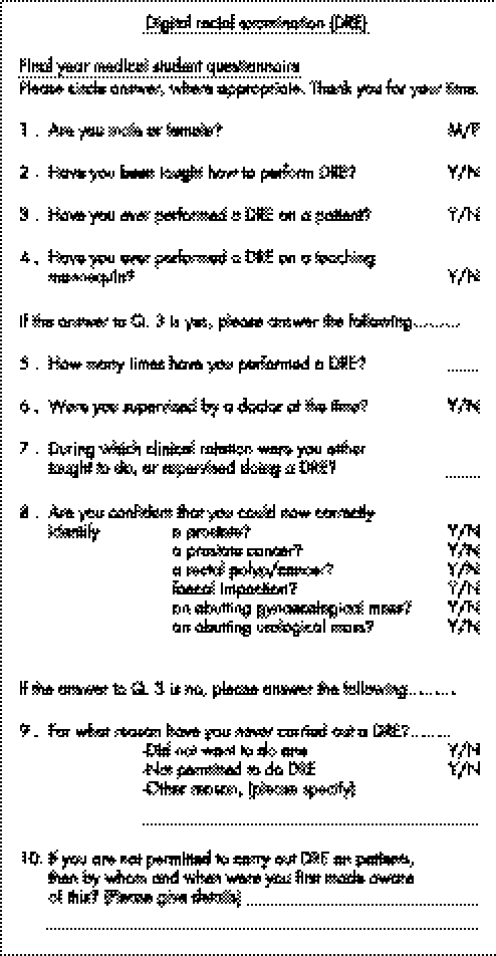
All 582 final year medical students within the Republic of Ireland during the summer of 2005 (Royal College of Surgeons in Ireland, Trinity College Dublin, University College Cork, University College Dublin, and University College Galway) were invited to participate in this study within one week of completion of their undergraduate training. With the agreement of each college, the survey was conducted in the format of a questionnaire. To our best knowledge no externally validated DRE questionnaire exists and therefore this questionnaire was designed specifically for this study (fig 1). With the belief that anonymity would encourage honesty, all surveys were accepted after completion in an anonymous fashion. Demographic information such as student age, race, nationality or background was not requested.
Figure 1 Study questionnaire. The questionnaire was anonymous and excluded data such as age, race and background.
The questionnaire aimed to assess the student's experience of DRE acquired during undergraduate training. “Experience of DRE” was defined as the student having performed a DRE on either a patient or a teaching mannequin (plastic model male pelvis) on at least one occasion. Record was made whether experience was derived from patient or teaching mannequin. Students who had gained experience of DRE by the examination of a patient were asked to state the number of examinations performed. The students who had performed DRE on a patient were given the opportunity to rate their confidence in detecting routine pathology, as the assumption was made that students having never performed the examination on a patient could not reasonably be expected to have any confidence. The results were analysed in a standard manner for population surveys.
RESULTS
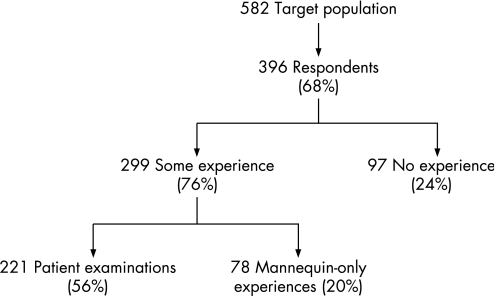
The questionnaires were completed by 396 (68%) of 582 students; 220 (71%) of 312 females and 176 (65%) of 270 males, with a total of 277 students (70%) positively reporting they had been taught how to perform DRE. Experience of DRE is presented in fig 2, and shows 175 respondents (44%) not having performed DRE on a patient by the time of completion of their undergraduate training.
Figure 2 Results flow chart illustrating the level of undergraduate‐acquired experience of digital rectal examination. Experience was defined as the student having performed at least one examination.
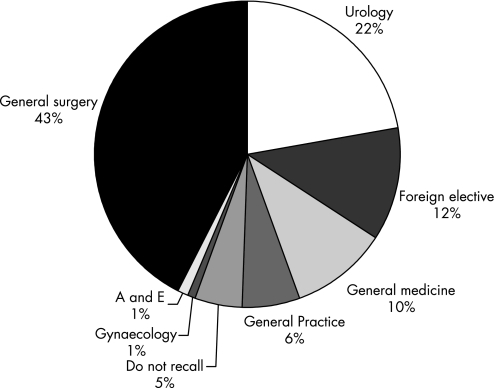
Of those students having examined a patient, the mean DRE number was 1.24 (range 1–100), with the median 2. DRE had been performed more than 10 times in 12 respondents (3%). All eight students who had performed more than 20 examinations did so while on clinical electives abroad. Supervision of patient examination was reported by 200 respondents (90%) with no clear reason elucidated for the lack of supervision of the remaining students. The clinical service offering most DRE training is presented in fig 3, with general surgery (43%) and urology (22%) offering greatest opportunity.
Figure 3 Source of undergraduate training in digital rectal examination.
Variable confidence was obtained from DRE training. Of 221 students with experience of DRE (by patient examination), confidence in identifying normal prostate, clinically overt prostate cancer or rectal polyp/tumour was reported in 134 (61%), 68 (31%) and 61 (28%), respectively. Despite having some experience of patient examination, one third of this group reported no confidence in their ability to interpret DRE findings.
No experience of patient DRE was reported by 175 (44%) respondents. The most common reported reason for this was a misunderstanding that students were not permitted to perform DRE on patients in 89 cases (51%).
DISCUSSION
It has been clearly stated previously that abdominal examination is not complete without the performance of rectal examination, and some authors have gone on to jest that it should be performed in all patients admitted to hospital “unless the examiner has no fingers”.1 Today, DRE may be increasingly confined to the domain of subspecialities such as urology and general surgery, and general training in DRE may have to be considered a thing of the past.
This report is the largest survey of undergraduate training in DRE and the only national study ever reported. The results are perhaps the most worrying yet. Turner et al surveyed students just before the final medical exams in Oxford in 1999; while seemingly reporting all students having performed at least one DRE, 42% had performed five or less DREs during a 3‐year clinical training period and 41% were “not at all confident” in giving an opinion based on findings at DRE.9 In a similar study conducted during the final weeks of undergraduate training in Melbourne in 2004, 17% of students had never done a DRE.10 In answer to the question we phrased “Have you been taught how to perform DRE?”, 70% of students in this study responded positively in comparison to 88% in the Oxford study and 92% in the Melbourne study. Of serious concern is the finding in this study that 44% of respondents in Irish medical schools reported never having performed a DRE on a patient, and, of these, 24% had never even performed simulated examination on a mannequin or plastic teaching model. Our results show that 88% of Irish graduating students had performed fewer than five DREs before finishing medical school versus 42% in the Oxford study. One reason may be temporal, with the time interval between the Oxford study and the latter studies suggesting that the numbers of DRE performed by medical students may be decreasing.
DRE remains a consistent component of the practice of general surgeons and urologists. In an audit of 19 UK medical schools reported in 2002, Shah and colleagues found that only seven (37%) included urology as part of the core curriculum, with no formal urology lectures provided in six, and two schools stated it was possible for medical students to graduate with no exposure to urology.11 This highlights a worrying trend within UK medical schools away from mandatory undergraduate training in surgical subspecialities, and perhaps lays some foundation for declining exposure to DRE training. Shah further rationalises that urologic illness comprises 5% of all illness and therefore each student doing a 2 to 3 year clinical programme should receive at least 2–3 weeks focused urology training. Furthermore, DRE is a skill rarely examined in final examinations, perhaps encouraging neglect by students. Turner et al proposed that six supervised DREs should be viewed as an absolute minimum requirement for medical students.9 The wide range of DRE examinations reported in this study must not mislead the reader. The mean and median values for those with experience of patient examination in this report were 1.24 and 2, respectively. All eight students reporting more than 20 DREs did so while on student electives abroad, and one student claimed to have done 100 DREs during a 2 month elective clerking in‐patients for a tertiary referral surgical centre in the United States.
The response rate of 68% to this survey is very satisfactory and is in keeping with the necessary response rate from similar valid questionnaire studies.12 Unknown limitations may, however, exist in the assessment tools used in this and other comparable studies. The questionnaire used in our study has not been externally validated and, to our best knowledge, no externally validated DRE questionnaire exists. Similarly, only limited knowledge exists regarding the technique of teaching DRE. In our system, a plastic male pelvis model (mannequin) has provided the only substitute for the direct involvement of patients. Alternatively, in addition to standard teaching techniques, rectal teaching associates (RTA) have been critically assessed.13 These are trainers who use their own bodies as part of the teaching process, and the teaching method takes its origin from gynaecologic teaching associates.14 Popaduik reported medical students rating RTA‐assisted teaching as the most effective teaching tool in relation to DRE, in terms of enhancing confidence in ability to determine when to conduct DRE, improving the understanding of DRE, improving skill and technique in the DRE procedure, and practising patient interaction skills.13 In our centre the teaching mannequin remains the preferred mode of teaching DRE, but supervised patient examination is still perceived as the gold standard teaching experience.
Conclusions
The optimum teaching method of DRE for medical undergraduates is undefined but may employ a patient, mannequin, or RTA. The choice of training technique is a sensitive issue and clarification of ethical issues may be required from professional bodies. Universal undergraduate training in DRE is not currently being achieved in Irish medical schools. If DRE is to remain an essential part of the general physical examination this topic must be the subject of further investigation and discussion.
ACKNOWLEDGEMENTS
The authors wish to thank the deans and participants from all five medical schools within the Republic of Ireland.
Abbreviations
DRE - digital rectal examination
PSA - prostate specific antigen
RTA - rectal teaching associates
Footnotes
Conflict of interest: None declared.
References
- 1.Talley N J, O'Connor S. Clinical examination. A systematic guide to physical diagnosis. Blackwell Science 20003E178–179. [Google Scholar]
- 2.Ng D P, Mayberry J F, McIntyre A S.et al The practice of rectal examination. Postgrad Med J 199167904–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schroder F H, van der Maas P, Beemsterboer P.et al Evaluation of the digital rectal examination as a screening test for prostate cancer. Rotterdam section of the European Randomized Study of Screening for Prostate Cancer. J Natl Cancer Inst 1998901817–1823. [DOI] [PubMed] [Google Scholar]
- 4.Dixon A R, Thornton‐Holmes J, Cheetham N M. General practitioners' awareness of colorectal cancer: a 10‐year review. BMJ 1990301152–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.General Medical Council Tomorrow's doctors. 1993. http://www.gmc.org.uk
- 6.The Medical Council, Ireland A guide to ethical conduct and behaviour, 6th ed. Dublin, The Medical Council, Ireland 2004
- 7.Bewley S. The law, medical students, and assaults. BMJ 19923041551–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hennigan T W, Franks P J, Hocken D B.et al Rectal examination in general practice. BMJ 1990301667–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner K J, Brewster F. Rectal examination and urethral catheterisation by medical students and house officers: taught but not used. BJU International 200086422–426. [DOI] [PubMed] [Google Scholar]
- 10.Lawrentschuk N, Bolton D M. Experience and attitudes of final‐year medical students to digital rectal examination. MJA 2004181323–325. [DOI] [PubMed] [Google Scholar]
- 11.Shah J, Billington R, Manson J.et al Undergraduate urology: a survey of current provisions and guidelines for a core curriculum. BJUI 200289327–330. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong D, Ashworth D. When questionnaire response rates do matter: a survey of general practitioners and their views of NHS changes. Br J Gen Pract 200050479–480. [PMC free article] [PubMed] [Google Scholar]
- 13.Popadiuk C, Pottle M, Curran V. Teaching rectal examinations to medical students: an evaluation study of teaching methods. Acad Med 2002771140–1146. [DOI] [PubMed] [Google Scholar]
- 14.Kretzschmar R M. Evolution of the gynaecology teaching associate: an education specialist. Am J Obstet Gynecol 1978131367–373. [DOI] [PubMed] [Google Scholar]