Abstract
Background
Anaphylaxis is a life threatening reaction where prompt and appropriate management can save lives. Epinephrine (adrenaline) is the treatment of choice; however, the recommended dose and route of administration of epinephrine used in the management of anaphylaxis is different from that used in the management of cardiac arrest.
Objective
To investigate how junior doctors would administer epinephrine in a case of anaphylactic shock in an adult patient.
Methods
Junior medical staff in two district general hospitals were assessed with a short questionnaire.
Results
95 junior hospital doctors were assessed. The majority (94%) would administer epinephrine as the life saving drug of choice, but only 16.8% would administer it as recommended by the UK Resuscitation Council Guidelines.
Conclusion
Junior doctors may be called to make immediate management decisions in patients with anaphylaxis; however, widespread confusion exists regarding the dose and route of administration of epinephrine. Strategies to improve education and access to appropriate drugs are needed. A labelled “anaphylaxis box” on every resuscitation trolley, containing the dose of epinephrine with clear labelling for intramuscular use, may be one solution.
Anaphylactic shock is a life threatening condition, which requires immediate and appropriate medical treatment. Although its true incidence is unknown, it is estimated to range from 10–30 cases per 100 000 population per year.1 A UK survey of fatal anaphylaxis in individuals over 16 years of age reported 20 deaths per year.2
Epinephrine (adrenaline) is the life saving drug of choice in the acute management of severe anaphylactic shock and its use is recommended in guidelines issued by the UK Resuscitation Council.3 These guidelines advise that epinephrine 0.5 mg via the intramuscular route should be given by first medical responders. Intravenous epinephrine is potentially hazardous.4,5,6 It should only be used by experienced personnel when intravenous access can be obtained without delay and where there is continuous monitoring4 of the heart rate, rhythm, blood pressure and in the presence of a defibrillator. Slow intravenous injection at a rate of 100 μg/min is recommended, stopping when a response has been obtained (1:100 000 dilution is safer).3 Its use should probably be limited to the theatre and intensive care environment.
Deaths have been reported from the inappropriate use of epinephrine in the context of allergic reactions5 and case reports published highlighting the occurrence of adverse effects of intravenous epinephrine.4
The dose and route of administration of epinephrine used in the management of cardiac arrest is different from that used in anaphylaxis7 and it has been shown that confusion exists among junior doctors starting in the accident and emergency department regarding the administration of epinephrine.8
Method
A total of 95 doctors were assessed in two district general hospitals (one in North Wales and one in the east of England). On one day in each hospital, junior doctors were approached by one of the authors (RJ) and asked to complete a short questionnaire in his presence. The range of doctors approached in each of the two hospitals is shown in table 1.
Table 1 Grades of doctors asked to complete the questionnaire.
| Hospital 1 | Hospital 2 | |
|---|---|---|
| FY1 | 6 | 12 |
| FY2/SHO | 27 | 30 |
| SpR | 6 | 9 |
| TG | 5 | 0 |
| Total: | 44 | 51 |
FY1, Foundation year 1; FY2, Foundation year 2; SHO, senior house officer; SpR, specialist registrar; TG, Trust grade.
The assessment described the hypothetical case of anaphylactic shock in a non‐anaesthetised patient. Medical staff were asked to describe which drug they would administer, which dose and via which route. The questionnaire is shown in fig 1.
Figure 1 The questionnaire completed by the 95 doctors.
Results
Out of the 95 doctors questioned, 89 (94%) correctly said that they would administer epinephrine as their life saving drug of choice. However, only 16 (16.8%) were able to describe correctly the dose and route of administration as recommended in the UK Resuscitation Council guidelines.
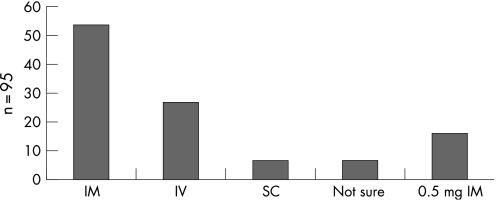
Only 57.9% of the doctors would give epinephrine intramuscularly (fig 2). Of these, 32.7% said they would have given 1 mg, 1.8% would have given a higher dose, 5.5% would have given a very low dose and 30.9% did not know what dose to give. Fewer doctors, 28.4%, said they would give epinephrine intravenously. Of these, 25.9% would have administered a dose of 0.5–1 ml of 1:10 000 solution, 29.6% would administer a higher dose and 44.4% did not know what dose to give. Only 6.3% of the doctors would administer epinephrine subcutaneously; 7.4% were not sure if they would administer it intravenously, intramuscularly or subcutaneously, and also would give the incorrect dose.
Figure 2 Number of doctors using the different routes of administration for epinephrine. IM, intramuscular; IV, intravenous; SC, subcutaneous.
Of the various grades of junior doctors questioned, 38.9% of the foundation year 1, 59.6% of the foundation year 2/senior house officers, and 73.3% of the specialist registrars said they would administer epinephrine via the intramuscular route.
Discussion
Junior medical staff may be called upon to make immediate decisions in the management of patients with anaphylaxis, and in our survey they were aware that epinephrine is the drug of choice. However, in both hospitals surveyed most medical staff did not know the correct dose and route of administration of epinephrine recommended to deal with this life‐threatening emergency. In particular, inappropriate choice of the intravenous route introduces a delay while an intravenous cannula is inserted and puts the patient at risk of arrhythmias (which may in themselves be fatal in a shocked patient).6
We have shown that not only the senior house officers in the study by Gompels et al8 are confused by the route and dose of epinephrine in anaphylaxis, but that this observation extends to most junior doctors throughout the various specialties in a hospital. It was also noted that doctors in a lower level of training were more likely to consider a route of administration other than the intramuscular route.
Strategies to improve education and access to appropriate drugs are needed. The ward or departmental resuscitation trolley is key to the management of medical emergencies in hospital and would normally be brought to the patient in anaphylaxis or cardiac arrest. At present these trolleys contain epinephrine syringes designed for use in patients with cardiac arrest. We would recommend a separate “anaphylaxis box” on the resuscitation trolley containing syringes containing the correct dose of epinephrine for anaphylaxis and clear labelling to direct intramuscular use.
Doctors of all grades who may be the first responders at a scene of anaphylactic shock should know how to manage the case according to the UK Resuscitation Council guidelines. Epinephrine is only part of the management of anaphylaxis but its early and correct use can be lifesaving.
Footnotes
Competing interests: None declared.
References
- 1.Peng M M, Jick H. A population‐based study of the incidence, cause and severity of anaphylaxis in the UK. Arch Intern Med 2004164317–319. [DOI] [PubMed] [Google Scholar]
- 2.Pumphrey R S, Roberts I S. Postmortem findings after fatal anaphylactic reactions. J Clin Pathol 200053273–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Project Team of the Resuscitation Council (UK) The emergency medical treatment of anaphylactic reactions for first medical responders and for community nurses (revised May 2005). www.resus.org.uk
- 4.Johnston S L, Unsworth J, Gompels M M. Lesson of the week: adrenaline given outside the context of life threatening allergic reactions. BMJ 2003326589–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pumphrey R S H. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy 2000301144–1150. [DOI] [PubMed] [Google Scholar]
- 6.American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: part 10. 6: anaphylaxis, Circulation 2005112IV143–IV145. [DOI] [PubMed] [Google Scholar]
- 7.Resuscitation Council (UK) Adult advanced life support algorithm of the Resuscitation Council (UK) (revised 2005). www.resus.org.uk
- 8.Gompels L L, Bethune C, Johnston S L.et al Proposed use of adrenaline (epinephrine) in anaphylaxis and related conditions: a study of senior house officers starting accident and emergency posts. Postgrad Med J 200278416–418. [DOI] [PMC free article] [PubMed] [Google Scholar]