Abstract
Objective
To develop a core curriculum for orthopaedic surgery and to conduct a national survey to assess the importance of 281 items in the curriculum. Attention was focused specifically on 24 items pertaining to the curriculum that are pertinent to the spine.
Study design
A cross‐sectional survey of a random sample of orthopaedic surgeons whose primary affiliation was non‐academic, representing the provinces and territories of Canada
Methods
A questionnaire containing 281 items was developed. A random group of 131 (out of 156) orthopaedic surgeons whose primary affiliation is non‐academic completed the questionnaire. The data were analysed quantitatively using average mean scores, histograms, the modified Hotelling's T2 test and the Benjimini–Hochberg procedure.
Results
131 of 156 (84%) orthopaedic surgeons participated, in this study. 14 of 24 items were ranked at no less than 3 out of 4 thus suggesting that 58% of the items are important or probably important to know by the end of residency (SD⩽0.07). Residents need to learn the diagnosis and principles of managing patients with common conditions of the spine.
Conclusions
The study shows, with reliable statistical evidence, that orthopaedic residents are no longer expected to be able to perform spinal fusions with proficiency on completion of residency. Is the exposure to surgical spine problems and the ability to be comfortable with operating expectations specific to the fellowship level? If so, the focus during residency or increasing accredited spine fellowships needs to be addressed to ensure that enough spine surgeons are educated to meet the future healthcare demands projected for Canada.
Keywords: medical education, orthopaedic spine curriculum
This paper is part of a larger study regarding the development and validation of a core curriculum for orthopaedic surgery. One entire core curriculum was validated, and then 10 individual analyses were completed so as to clarify the content that residents should learn during residency in orthopaedic surgery. This paper is about items of the core curriculum related to the orthopaedic spine.
The World Health Organization (WHO) declared the years 2000–2010 as the Bone and Joint Decade. One of the main reasons for this declaration was the current and projected burden of illness brought to society by musculoskeletal (MSK) conditions.1,2,3 One aim of the decade is to improve medical education at all levels in the area of MSK health.
A previous study validating the core curriculum recommendations for MSK conditions that was outlined by the Bone and Joint Decade Undergraduate Curriculum Group indicated that emergent and common conditions pertaining to the spine accounted for four out of the top 10 items that residents should know by the end of residency.4 In the United States, orthopaedic spine surgeons have suggested educational guidelines for resident training in spine surgery,5,6 and educational leaders are currently debating whether or not to implement a certification process.5,7,8 Similarly, in the United Kingdom, concern for adequate educational opportunities in the area of spine surgery is being questioned,9 and ways to increase recruitment into the discipline of spine surgery are being investigated.10,11
In Canada, the discipline of orthopaedic surgery has become extremely sub‐specialised. It is the responsibility of every academically accredited orthopaedic residency training programme to produce orthopaedic surgeons who would be capable of starting a practice on completion of his or her training. It is the responsibility of the board of examiners to ensure effective evaluation of orthopaedic surgeons before they start their practices. A debate exists between those designing the training programmes and the Board of Examiners with respect to the content of the questions for the Orthopaedic Fellowship Examination. Does the fellowship examination reflect what an orthopaedic surgeon whose primary affiliation is non‐academic needs to know before starting a safe and competent practice? In order to answer this question, consensus needs to be obtained regarding the curriculum to be emphasised during the educational process of an orthopaedic resident.
The Royal College of Physicians and Surgeons of Canada (RCPSC) and Specialty Committee for Orthopaedic Surgery, the Board of Examiners for Orthopaedic Surgery, and the Canadian Orthopaedic Association along with Bone and Joint Decade Canada supported an educational initiative to develop and validate an orthopaedic curriculum targeted to meet the needs of residency education in Canada. One section of this curriculum was dedicated to the education domain of orthopaedic spine. The orthopaedic specialty committee for the RCPSC and the chief examiners of the Board of Examiners requested that the national survey that assesses the importance of curriculum items be determined by orthopaedic surgeons whose primary affiliation is non‐academic. The reasons for this are twofold.
First, the attrition rate into a full‐time academic practice in any of the 16 accredited academic orthopaedic programmes is low. Surgeons in non‐academic practices may be in a position to provide input to a curriculum that is targeted to meet the needs of community orthopaedic surgeons. Second, orthopaedic surgeons in academic centres in general are already very specialised and their opinions may not necessary reflect what is required to be practised in community hospitals. For these reasons, a nation‐wide randomisation of orthopaedic surgeons whose primary affiliation was non‐academic was requested and subsequently conducted.
The purpose of this study was to determine the importance of the core content that should be included in a core curriculum for orthopaedic surgery, with attention focused on topics specific to the spine.
The null hypothesis tested was that all items in the core curriculum for orthopaedic surgery pertaining to the spine are equally as important for a resident to demonstrate knowledge or perform with proficiency during residency.
Methods
Development of the outcome measure
A 281‐item outcome measure (questionnaire) consisting of three sections was created. The validated international core curriculum for MSK health made up the first section of items. This study was conducted in the campuses of the 16 accredited academic institutions in Canada. A cross‐sectional survey of programme directors and selected educators representing six disciplines and 77 accredited academic training programmes that manage patients with MSK conditions was completed. A copy of this questionnaire can be obtained from the corresponding author on request.4
Specialty objectives of the RCPSC specifically pertaining to orthopaedic surgery made up the second cluster of items. The third section included a complete procedure list based on code books from across Canada. The outcome measure was created and compared with the curricula of 16 accredited institutions in Canada to ensure the inclusion of items that the university programmes thought to be important.
This outcome measure underwent a full review for content by 10 orthopaedic‐surgery educators (Fellows of the Royal College of Surgeons of Canada) of both genders representing adult and paediatric orthopaedic surgery from within Canada and the USA, including two chief examiners representing the Anglophone and Francophone Boards of Examiners, Programme Directors representing The RCPSC Specialty Committee for Orthopaedic Surgery and educational leaders within the Canadian orthopaedic community. A modified outcome measure was developed on the basis of the feedback of this content review, and the final outcome measure consisted of 281 items. The outcome measure was translated into French for the purposes of data collection with the Francophone orthopaedists. In this particular paper, the focus was on 24 items pertaining to orthopaedic spine. This questionnaire is available on request from the corresponding author.
Sample question
Each of the 281 question items were structured in a fashion similar to the sample question below that pertains to a resident's ability to perform with proficiency a posterior decompression of the lumbar spine (fig 1). The choices for response for each question were 0—unable to assess, 1—not important, 2—probably not important, 3—probably important and 4—important.
Figure 1 Sample question.
Randomisation and cross‐sectional survey
Altogether, 156 orthopaedic surgeons with non‐academic primary affiliation were randomised via a random number table to this study, based on the 2004 active RCPSC list of practising orthopaedic surgeons in Canada. The randomisation was done in three separate processes to ensure representation from all regions in Canada.
A schedule for interviews was arranged and conducted in both official languages depending on the functional language of each respondent. This cross‐sectional survey was completed. The Anglophone interviews were completed either over the telephone or in person, and the Francophone interviews were completed through direct one‐on‐one interviews during a research tour through Quebec.
Statistical analysis
Data were analysed descriptively and quantitatively using histograms, a modified Hotelling's T2 statistic12 with p value determined by a permutation test, and the Benjamini–Hochberg/Yekutieli procedure.13,14,15,16 Our goal was to draw conclusions about the 24 questions pertaining to orthopaedic spine. Although on a superficial glance most questions seem to have been “important”, in fact, our data enabled us to group, or “cluster” questions so that those within a cluster were deemed roughly alike in importance, whereas those in different clusters were judged to be different in importance. Analyses were made by techniques developed for testing large numbers of hypotheses, which have become popular and crucial to understanding studies of gene expression by microarrays. The approach was pioneered initially by Benjamini and Hochberg14,15,16 and has been applied by them to behavioural and educational settings.15
Each of the 131 orthopaedic surgeons queried answered the larger set of 281 questions, and let alone the subset of 24 questions devoted to orthopaedic spine without knowing the answers given by any of the other surgeons. Therefore, our analyses assumed that each respondent answered questions independently of the answers of any other respondent, but that the answers to different questions by the same respondent might be dependent.16 Each surgeon's response regarding the spine was taken initially to be a 24‐dimensional list of integers, each between 0 and 4. The 131 respective environments were similar enough for our purposes that we took the answers to be drawn from a common sampling distribution. However, the coordinates of each surgeon's list (vector) of 24 answers were taken to be dependent. Procedures where such dependence might be judged are extensions and adaptations of the celebrated McNemar test for 2×2 tables.
Our analysis also included the comparisons of questions to each other. Every respondent answered every question as 1, 2, 3 or 4. No missing data was reported. For a specific question, a respondent's answer was regarded as a four‐dimensional vector, with coordinate i = 1 when the answer given was i (where i is 1, 2, 3, or 4), and 0 for the other three coordinates. Estimating covariance is invariably a difficult statistical task.17 This particular study involved a covariance that was singular and not a full rank. The reason for singularity is that the coordinate differences for two questions sum to 0; thus, once three of the differences are known, the fourth can also be known. We compared two questions by comparing the difference between the two cited four‐dimensional vectors of responses to the questions by adapting the celebrated Hotelling's T2 to the scenario where the covariance matrix of the difference is singular. Because in our application the resulting sampling distribution is unknown, we resorted to a computer‐intensive permutation test18 to compare each pair of questions.
The Benjamini–Hochberg procedure was then used to help us interpret the large number of tests carried out for differences between pairs of questions. This section of the study consisted of 24 questions, representing not only 24 values of the average response to the question but also 276 pairs of questions to be compared, which is far too many for Bonferroni's celebrated method of comparison. This is the ingenious Benjamini–Hochberg approach. First, a test for equality of 24 pairs of questions at the 0.05 level is completed. However, a simultaneous 0.05 p value is not required. Instead, we decide for each pair whether we “accept” or “reject”, but take the less stringent view that we allow ourselves a pre‐assigned (expected) fraction of “type 1 errors”, not just the single error allowed by the Bonferroni method.13,14,15 The expected fraction (the false discovery rate) used for this study was 5%.
Clusters were formed from examination of the empirical average scores of questions. We examined this empirical distribution for obvious “break points” and justified the breaks by the results of cited Benjamini–Hochberg testing.
Results
Demographics
131 of 156 orthopaedic surgeons whose primary affiliation is non‐academic participated in this study, for an overall response rate of 84%. There was a 90% response rate from the Atlantic and Quebec provinces, 80% from Ontario and the territories, and 80% from the western provinces of Manitoba, Saskatchewan, Alberta and British Columbia.
In all 85% percent of the respondents classified themselves as generalists and 15% as specialists. The average age of each respondent was 48.7 years. Each respondent was in practice for an average of 16.8 years. Males made up 90% of the respondents and females 10%.
No fellowship training (46/131)
Out of the 131 respondents 46 did not complete fellowship training after residency.
Combined fellowship training (26/131)
Twenty three respondents completed combined fellowship training in total joint arthroplasty and either trauma, sports medicine, spine, paediatrics, oncology or upper extremity reconstruction. Two respondents completed fellowship training in paediatrics combined with either trauma or rehabilitative orthopaedic surgery. One respondent combined fellowship training in the spine and hand.
Individual fellowship training (59/131)
Ten individuals completed separate fellowship training in adult hip and knee reconstruction, nine in sports medicine, eight in spine, seven in hand and wrist reconstruction, four in hand and microvascular surgery, five in upper extremity, two in foot and ankle, four in trauma, four in paediatric orthopaedics and six in general orthopaedics.
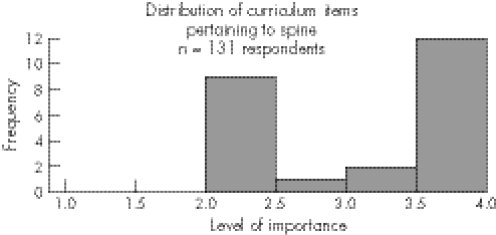
Orthopaedic spine curriculum content
Out of 24 items 14 (58%) items pertaining to spine curriculum content received an average mean score of >3.2 out of a scale of 4 by all 131 respondents, suggesting that 58% of the items are either probably important or important to know by the end of residency. In addition, the Benjamini–Hochberg procedure demonstrates that for 77% of the 24×23/2 = 276 possible pairs of questions pertaining to the spine, the distribution of the responses to one of the items was different from that of the responses to the other. Using the false discovery rate of the 0.05 criterion applied to the Hoteling T test summary of the responses to the questionnaire, the topics associated with the comparison of one question to another were found to be of unequal importance to the respondents (see histogram, fig 2).
Figure 2 Distribution of spine curriculum: items in order of importance.
The first cluster of items considered to be the most important emphasised the importance of knowing and understanding the content rather than the specific operative procedures that pertain to the spine. The second cluster of items considered important pertained to two procedures. The third cluster of items considered probably not important were procedures associated with arthrodesis of the cervical, thoracic and lumbar spine (table 1).
Table 1 Spine content.
| Item number | |
|---|---|
| <2.94 | Probably not important items to learn how to do with proficiency during a residency training program |
| 206 | Procedure—anterior decompression of the thoracic spine |
| 207 | Procedure—anterior decompression of the cervical spine |
| 200 | Procedure—discectomy in the thoracic spine |
| 209 | Procedure—arthrodesis of the thoracic spine |
| 210 | Procedure—arthrodesis of the cervical spine |
| 205 | Procedure—anterior decompression of the lumbar spine |
| 204 | Procedure—posterior decompression of the cervical spine |
| 203 | Procedure—posterior decompression of the thoracic spine |
| 201 | Procedure—discectomy in the cervical spine |
| 208 | Procedure—arthrodesis in the lumbar spine |
| 2.95 to 3.54 | Items that are probably important (nice to know) and perform with proficiency during a residency training programme |
| 202 | Procedure—posterior decompression of the lumbar spine |
| 199 | Procedure—discectomy of the lumbar spine |
| 3.56 to 3.74 | Items that are important (should know) and can be performed with proficiency during a residency training programme |
| 32 | Content—take a relevant history, identify and characterise inflammatory back pain such as ankylosing spondylitis |
| 3.76 to 4.0 | Items that are important (must know) and can be performed with proficiency during a residency training programme |
| 36 | Content—specify the signs and symptoms, outline the assessment and investigations, propose a differential diagnosis, outline the principles of management of a patient with neck pain |
| 33 | Content—take a relevant history, identify and characterise spinal deformity such as scoliosis |
| 7 | Content—the ability to construct an appropriate differential diagnosis and plan of patient enquiry, examination, limited investigation and assessment for a patient presenting with back pain. |
| 31 | Content—take a relevant history, identify and characterise vertebral fractures of osteoporotic origin |
| 28 | Content—take a relevant history, identify and characterise mechanical neck and back pain relating to non‐specific low back pain, spondylolysthesis, spondylolysis and lumbago |
| 35 | Content—specify the signs and symptoms, outline the assessment and investigations, propose a differential diagnosis and outline the principles of management of a patient with low back pain and sciatica |
| 29 | Content—take a relevant history, identify and characterise spinal cord or root entrapment (ie, herniated disc) |
| 30 | Content—take a relevant history, identify and characterise vertebral fractures of traumatic origin |
| 34 | Content—Take a relevant history, identify and characterise destructive lesions of the spine presenting as back pain which may be of infectious or tumour origin such as TB, metastasis and/or malignancy |
| 40 | Content—specify signs and symptoms, immediate complications, outline the assessment and investigations, outline the immediate and long‐term management of a patient with an acute spinal injury |
| 16 | Content—demonstrate knowledge, diagnose, initially manage and refer (if necessary) a patient with cauda equina compression |
Discussion
The increased burden of illness caused by MSK conditions has made an impact on the world and on society. Arthritis is one major condition afflicting Canadians. Conditions of the spine are major contributors to long‐term pain and disability.2,19 It is important for all healthcare professionals who manage patients with MSK conditions to become knowledgeable in the assessment and diagnosis of conditions pertaining to the spine. The importance of implementing strategies to understand why individuals are not choosing orthopaedic spine surgery as a discipline of choice has also been questioned.7,8,10
Historically, orthopaedic surgeons performed arthrodesis of the cervical, thoracic and lumbar spine, and neurosurgeons performed the decompressions. Presently, orthopaedic surgeons and neurosurgeons are performing “spine surgery” as members of the same “service or team” and for various indications.20 The reasons for the increase in instrumental spinal fusions may be multifactorial. The first reason is that the population demographics and the increase in incidence and prevalence of arthritis of the spine may lead to an increase in spinal fusions. The second, reason involves the considerable advances in technology.21,22 The third reason may be the presence of financial incentives.20 Irrespective of these reasons, the fact remains that the demand for spinal fusions has increased, more fusions are being performed,21,22 with the numbers approaching similar numbers as the amount of hip and knee replacements .20
Currently, this study suggests that graduating residents from orthopaedic surgery residency training programmes in Canada should not be expected to be able to perform with proficiency arthrodesis of the spine at any level by the end of his or her training. Why the major shift in practice from the past? Are spinal fusions too difficult for residents to learn during their training or are the residents simply lacking the educational opportunity or exposure in the form of “direct” hands on experience? The reasons for this shift may be explained by the fact that instrumented spinal fusions are technically more demanding and may lead to more complications.23,24,25,26 New graduates may be reluctant to perform procedures without additional fellowship training.
The debate regarding the type of educational exposure that both residents and fellows should experience is ongoing.5,6,8,9,10,11,27,28,29,30 Orthopaedic programmes may dedicate less time to spinal surgery than the neurosurgery programmes.31 In addition, orthopaedic residents may perceive themselves to be less competent in complex and basic procedures of the spine compared with neurosurgery residents.31
The strengths of the study included: (1) a previously validated international core curriculum for MSK health; (2) randomisation of orthopaedic surgeons in three different regions of Canada; (3) a full review of content before conducting the study; (4) direct one‐on‐one interviews that may explain the 84% response rate; (5) the use of a translated outcome measure and direct interviews with the Francophone orthopaedists that may explain the 90% response rate from the Quebec/Atlantic provinces; and (6) full endorsement of the RCPSC, the 16 academically accredited orthopaedic surgery training programmes; the Canadian Orthopaedic Association, and the Bone and Joint Decade Canada, demonstrating an unprecedented collaboration for the sole purpose of improving the education of orthopaedic surgeons across Canada.
The limitations of the study include (1) a positive response bias that existed within the questionnaire; (2) limited scale grading the level of importance and (3) in the present study, the wording of the questions asking each respondent to indicate the importance of either content or procedures. This implies that we are asking opinions rather than what they are actually doing.
Conclusions
Educating an orthopaedic resident begins with the core curriculum. This study has identified a core body of knowledge pertaining to the spine that residents need to know, understand and be able to perform with proficiency on completion of residency. Terminal and enabling objectives for orthopaedic spine curricula should focus on emergent and common problems of the spine, with fellowship examination questions focusing on this content.
Our study identifies a major difference in expectation from past graduates who historically have performed spine fusions but now are only expected to perform with proficiency a lumbar discectomy and posterior decompressions by completion of residency. If this is true, then how will the future healthcare needs of Canadians requiring spine procedures be addressed?
Canadians' residency training programmes will need to continue to provide suggestions and solutions to ensure that adequate surgical exposure and educational experiences in spine occur in Canada. In addition, programmes will need to facilitate a shift back to the basic procedures considered essential for orthopaedic surgeons. If this goal is not achieved, then a strategic plan including the possibility of referral centres may need to be developed and implemented to ensure that enough “spine” surgeons exist to meet the present and future demands of Canadians with spine problems.
Abbreviations
MSK - musculoskeletal
RCPSC - Royal College of Physicians and Surgeons of Canada
Footnotes
Funding: This study was made possible through the generous contribution of The Royal College of Physicians and Surgeons of Canada 2004 Medical Education Travelling Fellowship.
Competing interests: None.
References
- 1.Public Health Agency of Canada (PHAC) Economic burden of illness in Canada, 1993. Ottawa 1993
- 2. Health Canada, Economic burden of illness in Canada, 1998 (EBIC). Ottawa Health Canada 1998
- 3.Goetzel R Z, Long S R, Ozminkowski R J.et al Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting US employers. J Occup Environ Med 200446398–412. [DOI] [PubMed] [Google Scholar]
- 4.Wadey V M R, Tang E‐T, Abelseth G.et al Canadian interdisciplinary core curriculum for musculoskeletal health—a rheumatologist's perspective. J Rheumatol. In press [PubMed]
- 5.Herkowitz H N, Connolly P J, Gundry C R.et al Resident and fellowship guidelines: educational guidelines for resident training in spinal surgery. Spine 2000252703–2704. [DOI] [PubMed] [Google Scholar]
- 6.Garfin S R. Editorial on residencies and fellowships. Spine 2000252700–2702. [DOI] [PubMed] [Google Scholar]
- 7.Herkowitz H N, Benzel E C. Controversies in spine: subspecialty certification should not be a requirement for spine surgery. Spine 2002271478–1483. [PubMed] [Google Scholar]
- 8.Dwyer A P, Herkowitz H N, Benzel E C. Controversies in spine: Should there be subspecialty certification in spine surgery? Spine 200227148–183. [PubMed] [Google Scholar]
- 9.Clark S. Training in orthopaedic spine surgery. Lancet 20043511224. [DOI] [PubMed] [Google Scholar]
- 10.Conn K S, Sharp D J, Gardner A D H. Orthopaedic specialist registrar training and attitudes to spine surgery in the United Kingdom: reasons for poor recruitment and suggestions for improvement. Eur Spine J 200211515–518. [DOI] [PubMed] [Google Scholar]
- 11.Crockard H A. Training spinal surgeons. J Bone Joint Surg Br 199274‐B174–175. [DOI] [PubMed] [Google Scholar]
- 12.Behseta S, Kass R E. Testing equality of two functions using BARS. Stat Med 2005243523–3534. [DOI] [PubMed] [Google Scholar]
- 13.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Serv 1995B57289–300. [Google Scholar]
- 14.Benjamini Y, Hochberg Y. Multiple hypotheses testing with weights. Scand J Stat 199724407–418. [Google Scholar]
- 15.Benjamini Y, Hochberg Y. The adaptive control of the false discovery rate in multiple hypotheses testing. J Behav Educ Stat 20002560–83. [Google Scholar]
- 16.Benjamini Y, Yoav, Yekutieli D The control of the false discovery rate in multiple testing under dependency. Ann Stat 2001291165–1188. [Google Scholar]
- 17.Qu A, Lindsay B. Bulding adaptive estimating equations when inverse of covariance estimation is difficult. J Roy Stat Soc Serv B 200365127–142. [Google Scholar]
- 18.Efron B, Tibshirani R J.An Introduction to the Bootstrap. New York: Chapman & Hall, 1993202–218.
- 19.Badley E, DesMeules M. eds. Arthritis in Canada—an ongoing challenge. Chapter 1—Introduction. Ottawa: Health Canada, 2003
- 20.Deyo R A, Nachemson A, Mirza S K. Spinal‐fusion surgery—the case for restaint. N Engl J Med 2004350722–726. [DOI] [PubMed] [Google Scholar]
- 21.Schnee C L, Freese A, Ansell L V. Outcome analysis for adults with spondylolisthesis treated with posterolateral fusion and transpedicular screw fixation. J Neurosurg 19978656–63. [DOI] [PubMed] [Google Scholar]
- 22. Agency for Healthcare Research and Quality Healthcare cost and utilization project 2004 http://www.ahrq.gov (accessed 25 January 2007)
- 23.Richardson W J. Complications in spinal surgery. Curr Opin Orthoped 1993221325–1329. [Google Scholar]
- 24.Turner J A, Ersek M, Herron L, atient outcomes after lumbar spinal fusions et alJAMA 1992268907–911. [PubMed] [Google Scholar]
- 25.Deyo R A, Ciol M A, Cherkin D C.et al Lumbar spinal fusion: a cohort study of complications, reoperations, and resource use in the Medicare population. Spine 199319931463–1470. [PubMed] [Google Scholar]
- 26. Myers MA, Hamilton SR, Bogosian AJ et al Visual loss as a complication of spine surgery: a review of 37 cases. Spine 1997221325–1329. [DOI] [PubMed] [Google Scholar]
- 27.Matheny J M, Brinker M R, Elliot M N.et al Confidence of graduating family practice residents in their management of musculoskeletal conditions. Am J Orthop 200029945–952. [PubMed] [Google Scholar]
- 28.Grauer J N, Vaccaro A R, Beiner J M.et al Similarities and differences in the treatment of spine trauma between surgical specialties and location of practice. Spine 200429685–696. [DOI] [PubMed] [Google Scholar]
- 29.Eismont F J. The education, training, and evaluation of a spine surgeon (presidential address). Spine 1996212059–2063. [DOI] [PubMed] [Google Scholar]
- 30.Dailey S W, Brinker M R, Elliott M N. Orthopaedic residents' perceptions of the content and adequacy of their residency training. Am J Orthop 199827563–570. [PubMed] [Google Scholar]
- 31.Dvorak M F, Collins J B, Murnaghan L.et al Confidence in spine training among senior neurosurgical and orthopedic residents. Spine 200631831–837. [DOI] [PubMed] [Google Scholar]