Abstract
Since its introduction more than four and half decades ago, the science of cardiopulmonary resuscitation has been enriched with a significant amount of scientific evidence. This in turn has led to the birth of new evidence based guidelines for resuscitation published by the European Resuscitation Council and the American Heart Association in late 2005. This article aims to review the recent advances and controversies in the science of resuscitation.
Keywords: cardiopulmonary resuscitation, CPR, defibrillation
Cardiopulmonary resuscitation (CPR) is one of the key aspects of clinical practice. Delaying CPR after cardiac arrest often results in poor outcome. For every minute without CPR, survival from witnessed ventricular fibrillation (VF) cardiac arrest decreases by 7–10%.1 Ischaemic heart disease is the leading cause of death in the world.2,3,4,5,6 Sudden cardiac arrest (SCA) is responsible for more than 60% of adult deaths from coronary heart disease.7 Data from the Centers for Disease Control and Prevention in the USA estimates that approximately 330 000 people die annually from coronary heart disease. About 250 000 of these deaths occur in the out‐of‐hospital setting.7,8,9 The OPALS study in Canada (Ontario Prehospital Advanced Life Support Study) reported out‐of‐hospital cardiac arrest rates at 0.6 per 1000 population per year.10 Data from Scotland and five other European cities showed that the annual incidence of resuscitation for out‐of‐hospital cardiopulmonary arrest of cardiac aetiology is 50–66 per 100 000 population.11,12 VF is the predominant rhythm encountered in the first 3–5 min after sudden out‐of‐hospital cardiac arrest.13 In this rhythm, which is incompatible with life, the left ventricle develops a very rapid rhythm that prevents blood from pumping out to the body. Immediate therapy with defibrillation is the only effective treatment and resuscitation is most successful if defibrillation is performed in about the first 5 min after collapse.14,15,16 Immediate CPR with chest compressions and ventilation provides a small but critical amount of blood to the heart and brain while waiting for a defibrillator to arrive. CPR increases the likelihood that a shock will terminate VF. CPR is especially important if a shock is not delivered for 5 min or more after collapse.17,18,19 Many victims of SCA, therefore, can survive if bystanders act immediately while VF is still present, but successful resuscitation is unlikely once VF has deteriorated to asystole.1 Since its introduction more than four and half decades ago,20 the science of CPR has been enriched with a significant amount of scientific evidence. This in turn has led to the birth of new evidence based guidelines for resuscitation published by the European Resuscitation Council (ERC) and the American Heart Association (AHA) in late 2005.19,20,21,22 This article aims to review the recent advances in the science of resuscitation.
Bystander CPR
To improve the pre‐hospital care of victims of cardiac arrest, the AHA and ERC use four links in action called the chain of survival, wherein a sequence of interventions results in improved survival after cardiac arrest. These links are5,6,19:
Early recognition of the emergency and activation of the emergency medical services (EMS)
Early bystander CPR—immediate CPR can double or triple the victim's chance of survival from cardiac arrest
Early delivery of shock with a defibrillator—CPR plus defibrillation within 3–5 min of collapse can produce survival rates as high as 49–75%
Early advanced life support followed by post‐resuscitation care delivered by health care providers.
Bystanders can perform three of the four links in the chain of survival. When bystanders recognise the emergency and activate the EMS system, they ensure that basic and advanced life support providers are dispatched to the site of the emergency. In many communities, the time interval from EMS call to EMS arrival is 7–8 min. This means that in the first minutes after collapse the bystander will play the major role in CPR. Therefore, successful rescuer actions at the scene of cardiac arrest are of extreme importance and time critical. For every minute without CPR, survival from witnessed VF cardiac arrest decreases by 7–10%.1 When bystander CPR is provided, the decrease in survival is more gradual and averages 3–4% per minute from collapse to defibrillation. Bystander CPR has been shown to double or triple the chances of survival from witnessed cardiac arrest at many different intervals to defibrillation.1,23,24,25 Litwin et al26 looked at survival according to location of collapse. Patients who had a cardiac arrest in public were more likely to have had their arrest witnessed and were more likely to have received resuscitation from bystanders than patients who had a cardiac arrest at home (69% vs 49%). The survival rate among patients who had a cardiac arrest in public was much higher than that among patients who suffered an arrest at home (27% vs 13%). Taking into account time to defibrillation and whether the arrest was witnessed, much of this difference could be explained by the higher rate of resuscitation given by bystanders in public.
Too often, patients who have a cardiac arrest at home do not receive CPR from family members.27 A report from the Seattle Heart Watch programme compared the outcomes of patients resuscitated at the scene by a bystander trained in CPR with those patients who initially received CPR from EMS personnel.28 While there was no significant difference in the percentage of patients resuscitated at the scene and admitted alive to the hospital (67% vs 61%), the percentage discharged alive was significantly higher among those with bystander initiated CPR (43% vs 22%). In the OPALS study,10 the out‐of‐hospital cardiac arrest survival was shown to be significantly improved by three modifiable factors: citizen (bystander) CPR; fire and police CPR; and response with automated defibrillator in 8 min or less.10,29 Furthermore, this study found that the single modifiable factor associated with very good quality of life was citizen initiated CPR. The study clearly identified citizen initiated bystander CPR as a strong and independent predictor of very good functional outcomes for survivors from out‐of‐hospital cardiac arrest.30
Therefore, we must rely on a trained and willing public to initiate CPR and to call for professional help and early defibrillation. Based on these facts, many countries have recently started public training programmes that include teaching CPR and first‐responder automated external defibrillator (AED) use. However, despite the recent emphasis on the importance of bystander initiated CPR and the expansion of public training programmes, CPR is performed in only a third or less of witnessed arrests in western societies.30,31,32 Why bystanders are reluctant to perform CPR is still not clear. Inadequate training methods, complicated guidelines or fear of transmitted diseases may be responsible.19 Frequent, shorter and more accessible CPR courses for the public may be an appropriate solution.33
Recognising cardiorespiratory arrest
In the latest 2005 AHA and ERC guidelines for resuscitation,19,21 an initial pulse check as a sign of cardiorespiratory arrest has been omitted for lay rescuers as it takes too long and has low accuracy. Time spent attempting to confirm the presence or absence of a carotid pulse by lay rescuers may significantly delay the initiation of cardiac compressions. Therefore, lay rescuers should start CPR once the victim is not responding and not breathing normally. Only trained rescuers or health care professionals should check for the carotid pulse and, if it is absent, should be ready to perform chest compressions immediately. In a study by Eberle et al,34 the diagnostic accuracy of checking the carotid pulse by lay persons was found to be only 65%. Bahr et al35 also found the skills of lay people in checking the carotid pulse to be inaccurate for confirming the presence or absence of circulation. Agonal gasps occur commonly in the first few minutes of SCA. Bystanders, when asked by ambulance dispatchers over the telephone if breathing is present, often misinterpret agonal gasps as normal breathing. Lay people, therefore, should be taught to begin CPR if the victim is unconscious and not breathing normally. It should be emphasised during training that agonal gasps occur commonly in the first few minutes after SCA and they are an indication for starting CPR immediately and should not be confused with normal breathing.21
Compression–ventilation ratio
Interruption of chest compressions during CPR has a detrimental impact on survival from cardiac arrest.36 On stopping chest compressions, the coronary and cerebral blood flow decreases substantially. On resuming chest compressions, several compressions are necessary before the coronary flow recovers to its previous level.37 In the first minutes of VF SCA, blood oxygen content remains high and myocardial and cerebral oxygen supply is limited more by the diminished cardiac output than a lack of oxygen in the lungs. Therefore, ventilation does not appear to be as important as chest compressions, but it does appear to contribute to survival from prolonged asphyxial arrest.38 Obviously, the ventilation rate needed to maintain a normal ventilation–perfusion ratio during CPR is much smaller than normal because pulmonary blood flow is low. Recent evidence indicates that unnecessary interruptions to chest compressions occur frequently during in‐hospital and out‐of‐hospital CPR.39,40,41,42
There are no human data available to date that have identified the optimal compression–ventilation ratio for CPR. Mathematical and animal models showed that matching of pulmonary blood flow and ventilation might be more appropriate at compression–ventilation ratios higher than 15:2.43,44 A recent porcine model comparing the clinical and haemodynamic parameters in VF cardiac arrest demonstrated that increasing the compression–ventilation ratio from 15:2 to 30:2 generated a 30% higher cardiac output and doubled common carotid artery blood flow.45 To achieve optimal compression rates and reduce the frequency of interruption in compressions, a universal compression–ventilation ratio of 30:2 was recommended by consensus.46
Defibrillation timing and CPR before defibrillation
Early defibrillation is critical for survival from SCA for several reasons. Firstly, the most frequent initial rhythm in witnessed SCA is VF. Secondly, the treatment for VF is electrical defibrillation. Thirdly, the probability of successful defibrillation diminishes rapidly over time. Finally, VF tends to deteriorate to asystole within a few minutes.1,19 Therefore, defibrillation as soon as possible is the standard care for VF. In a study of over 12 000 patients treated by EMS, 4546 had witnessed VF. For these patients a shorter defibrillation response interval was significantly correlated with an increased chance of survival to hospital discharge.47 In laboratory studies, defibrillation success for VF is practically 100% immediately after induction of this rhythm. The success decreases to about 80–90% after 60 s of sustained VF, and after 20 min of sustained VF restoration of a perfusing rhythm is rare.48,49 In a study of 148 patients with out‐of‐hospital cardiac arrest in US casinos, 105 had VF. The survival rate was 74% for victims who received their first defibrillation within the first 3 min after collapse. For those who received their first defibrillation after the first 3 min, the survival rate was only 49%.13
A study examining the long term outcomes of out‐of‐hospital VF cardiac arrest in patients who received successful early defibrillation (mean (SD) time 5.7 (1.6) min) reported no difference in the long term survival outcomes between these patients and patients who did not have cardiac arrest.50 Therefore, early defibrillation is useful and effective if applied within 4–5 min of onset of out‐of‐hospital cardiac arrest. In the 2005 International Consensus Conference on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science,51 an important question was raised based on some recent evidence: whether to defibrillate first or to perform CPR first followed by defibrillation, particularly when more than 4–5 min has elapsed from collapse to rescuer intervention in victims with VF cardiac arrest. In animal studies, prolonged VF of more than 7 min was more effectively treated when 5 min of CPR was performed before defibrillation.52,53 In two human studies of out‐of‐hospital VF arrest, when the interval between the call to the EMS and delivery of the initial shock was 4–5 min or longer, a period of CPR before attempted defibrillation improved survival rates.11,12
One randomised study, however, showed equivalent survival rates when either CPR or defibrillation was performed first for any EMS call‐to‐shock interval.54 The consensus was that there were not sufficient data to recommend CPR before defibrillation for all victims of VF SCA. Lay rescuers should use the AED as soon as it is available. EMS rescuers may give five cycles (about 2 min) of CPR before attempting defibrillation for treatment of out‐of‐hospital cardiac arrest or pulseless ventricular tachycardia (VT), particularly when the EMS response (call to arrival) interval is longer than 4–5 min or EMS responders did not witness the cardiac arrest. EMS medical directors may create system protocols based on the average response interval of their system. When multiple rescuers are present, one rescuer can perform CPR while the other readies the defibrillator, thereby providing both immediate CPR and early defibrillation. The data were insufficient to determine whether this recommendation should be applied to in‐hospital cardiac arrest, what the ideal duration of CPR is before attempted defibrillation, and the duration of VF at which rescuers should switch from defibrillation first to CPR first.46
One‐shock rather than three‐shock scenario
There are no human studies so far to compare a one‐shock protocol with a three‐stacked shock protocol for treatment of VF cardiac arrest.19 Nevertheless, there are some plausible reasons to favour a one‐shock protocol over a three‐shock protocol.19 Firstly, animal studies have shown that frequent or long interruptions in chest compressions for rhythm analysis were associated with post‐resuscitation myocardial dysfunction and reduced survival rate.55 Interruption of chest compressions has also been shown to decrease the probability of converting VF to another rhythm.56,57 Secondly, the rhythm analysis for a three‐shock sequence performed by commercially available AEDs results in delays of up to 37 s between delivery of the first shock and delivery of the first post‐shock compressions.55 Thirdly, the first‐shock efficacy by current biphasic defibrillators was found to be more than 90%.58,59,60,61,62,63 If the first shock fails to eliminate VF, the incremental benefit of another shock is low and immediate resumption of CPR is likely to confer a greater value than another shock.19 Concerns that chest compressions might provoke recurrent VF in the presence of a post‐shock organised rhythm appear to be unfounded.63 For these reasons, a one‐shock protocol combined with immediate post‐shock CPR (without checking the rhythm or the pulse) seems reasonable and was included in the recent resuscitation guidelines as a substitute for the old three‐shock scenario.19
Public use of automated external defibrillators
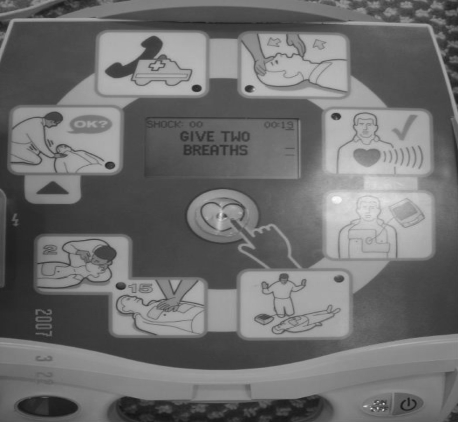
AEDs are lightweight, computerised devices containing a battery, capacitors and electronic circuitry to analyse the cardiac rhythm and inform the operator when a defibrillation shock is needed (fig 1). AEDs have been described as the “single greatest advance in the treatment of VF cardiac arrest since the development of CPR”.64 These devices have been shown to be extremely safe and highly accurate in detecting life threatening heart rhythms. The sensitivity and specificity for the detection of VF or rapid VT are 98% and 100%, respectively.65,66,67,68,69,70 The efficacy of AEDs in improving survival after out‐of‐hospital cardiac arrest has been shown in many studies. In a study by Valenzuela et al,13 AEDs were deployed in casinos and casino officers were trained in their use. By this intervention, the time from collapse to application of the first shock was shortened to a mean of 4.4 min and survival increased to 53%. In a recent randomised trial by Hallstrom et al,71 over 19 000 volunteers from shopping centres, recreational facilities, residential units and other community units were trained to perform CPR alone or CPR plus AED use. Patients treated by volunteers trained in CPR plus AED use were significantly more likely to receive a non‐EMS shock and significantly more likely to survive to discharge.
Figure 1 Automated external defibrillator used by the public.
Other similar studies have also shown significant improvement in survival of out‐of‐hospital cardiac arrest when AEDs were used by the public.72 Furthermore, in recent clinical trials,39,40 modified prototype AEDs recorded information about frequency and depth of chest compressions during CPR. If such devices become commercially available, AEDs may one day prompt rescuers to improve CPR performance.19 The AHA has recommended the development of special training programmes called public access defibrillation (PAD) programmes, which incorporate the training of AED use by bystanders at public places.73,74,75 The goal of these programmes is to shorten the time from onset of VF until CPR and shock delivery by ensuring that AEDs and trained lay rescuers are available in public areas where SCA is likely to occur. Public safety first responders (such as police, fire fighters, security personnel, ski patrol members and flight attendants), and family members of patients who have had a myocardial infarction should be trained and equipped to provide early defibrillation with AEDs.76
Monophasic versus biphasic waveforms and the shock dose
There are two types of defibrillators, based on the waveform they produce: monophasic and biphasic defibrillators. Monophasic defibrillators, which are no longer manufactured, deliver a unipolar current (one direction of current flow). Biphasic defibrillators, in contrast, deliver current that flows both in positive and negative directions. There are two types of biphasic waveforms, the biphasic truncated exponential (BTE) and rectilinear biphasic (RLB). Both types have been shown to be effective in terminating VF. First‐shock efficacy for long duration VF and VT has been shown to be greater with biphasic than monophasic waveforms and, therefore, use of biphasic defibrillators is recommended whenever possible.57,77 The ORBIT trial (Out‐of‐hospital Rectilinear Biphasic Investigational Trial)77 showed that rectilinear biphasic defibrillation waveforms at 120 J and 200 J were superior to monophasic waveforms at 200 J and 360 J, respectively, in converting VF to an organised rhythm. However, although a higher success rate in restoring electrical activity was noted, the survival rates to hospital admission and to hospital discharge were comparable to the monophasic waveforms. The optimal energy levels (shock doses) for both monophasic and biphasic defibrillators are unknown.
The recommendation to use a one‐shock strategy created a new challenge of defining the optimal energy for the initial shock. In a study of out‐of‐hospital cardiac arrest, first‐shock efficacy using 360 J was not superior to that of 200 J and repeated shocks at the higher dose were associated with more atrioventricular block without evidence of long term harm.78,79 Therefore, energy levels are based on a consensus following careful review of the current literature.21 It is reasonable to use selected energies of 150–200 J for a biphasic truncated exponential waveform or 120 J for a rectilinear biphasic waveform and 360 J for monophasic defibrillators.
Box 1: Summary of the recent advances in CPR
Bystander CPR can significantly improve the chances of survival from witnessed cardiac arrest
Checking for circulation by palpating the carotid pulse should be discouraged among lay rescuers
Interruptions of chest compressions during CPR have a detrimental effect on survival and therefore, should be minimised
Early defibrillation is very important in determining survival from VF/VT cardiac arrest
In VF/VT cardiac arrest, a single defibrillatory shock followed by 2 min of uninterrupted CPR seems reasonable and more beneficial than three‐shock protocol
Biphasic defibrillators are superior to monophasic defibrillators in converting VF to an organised rhythm and their use is recommended whenever possible
Use of AEDs by the public has been shown to improve survival from out‐of‐hospital cardiac arrest
Patients who remain unconscious with spontaneous circulation after out‐of‐hospital VF cardiac arrest should receive therapeutic hypothermia management
Induction of post‐resuscitation hypothermia
The role of therapeutic hypothermia in post‐resuscitation care has been investigated extensively during the last decade. Two prospective randomised trials reported improved outcomes when deliberate hypothermia of 32–34°C was induced in comatose patients admitted to hospital after witnessed out‐of‐hospital VF cardiac arrest.80,81 In one of these two trials, 273 patients were randomised to be treated with either therapeutic hypothermia (32–34°C for 24 h) or normothermia; 75 of the 136 patients (55%) in the hypothermia group were discharged alive with good neurological outcome 6 months after discharge, compared with 54 of the 137 (39%) patients in the normothermia group.80 The second trial also reported a better survival rate in the hypothermia group (49%) compared with the normothermia group (26%).81 It is strongly recommended that patients remaining comatose after return of spontaneous circulation following a witnessed VF cardiac arrest receive therapeutic hypothermia management.82 The role of hypothermia treatment after in‐hospital cardiac arrest or arrest from other rhythms remains inconclusive and further studies are required to address these issues.
Box 2: Controversial issues in CPR
There are no human studies to determine the optimal compression–ventilation ratio during CPR; a ratio of 30:2 was recommended by consensus
There are no sufficient data to recommend CPR before defibrillation for all victims of VF cardiac arrest
The optimal energy levels (shock doses) for both monophasic and biphasic defibrillators are unknown
The role of therapeutic hypothermia after in‐hospital cardiac arrest is unknown
There is currently insufficient evidence to support or refute the use of vasopressin as alternative to, or in combination with, epinephrine in any cardiac arrest rhythm
High dose epinephrine and the use of vasopressin
Despite its use in cardiopulmonary arrest for more than four decades, the optimal dose of epinephrine (adrenaline) in this situation is still unknown. The evidence supporting the use of a dose of 1 mg every 3–5 min is derived from animal studies. Recently, some animal studies reported that the use of much higher doses of epinephrine (0.2 mg/kg) improves the rate of survival after cardiac arrest.83,84 However, three large randomised human trials found that, despite improvement in the rates of return of spontaneous circulation, there was no statistically significant difference in survival to hospitalisation or hospital discharge between standard and high dose epinephrine use.85,86,87 Therefore, high dose epinephrine cannot be recommended in cardiopulmonary arrest.
The use of vasopressin in cardiopulmonary arrest as an alternative to epinephrine has been a matter of much debate during recent years. Small human studies reported the use of vasopressin during cardiopulmonary arrest to be promising with regard to return of spontaneous circulation and rate of hospital discharge.88,89 Following the results of these small studies, the AHA recommended that vasopressin could be used as an alternative to epinephrine for the treatment of adult refractory VF.90 However, two recent randomised studies comparing vasopressin with epinephrine for in‐hospital and out‐of‐hospital cardiac arrest were unable to demonstrate an overall increase in the rates of return of spontaneous circulation or survival for vasopressin when compared to epinephrine.91,92
A recent meta‐analysis of five randomised trials showed no statistically significant difference between vasopressin and epinephrine for return of spontaneous circulation, death within 24 h or death before hospital discharge.93 It was agreed in the 2005 International Consensus Conference on CPR that there is currently insufficient evidence to support or refute the use of vasopressin as an alternative to, or in combination with, epinephrine in any cardiac arrest rhythm.51 Epinephrine is still considered the primary vasopressor in cardiac arrest. Individual resuscitation councils will need to determine the role of vasopressin in their resuscitation guidelines.
Conclusion
Bystander CPR is the most important determinant of survival following out‐of‐hospital cardiopulmonary arrest. The greatest challenge for successful out‐of‐hospital resuscitation is the improvement of lay rescuer CPR education. Increased efficiency of instruction, improved skill retention through frequent and short CPR courses, and reduced barriers to action for basic and advanced life support providers are crucial in achieving this goal. Lay rescuers should start CPR if the victim is not responding and not breathing normally. Checking the circulation by palpating a carotid pulse should be discouraged among lay rescuers. Minimising interruptions of chest compressions should be emphasised during CPR, and induction of post‐resuscitation hypothermia after return of spontaneous circulation following a witnessed VF cardiac arrest should be tried. There are insufficient data to recommend the use of vasopressin either as alternative to, or in combination with, epinephrine in CPR (boxes 1 and 2).
Abbreviations
AED - automated external defibrillator
AHA - American Heart Association
BTE - biphasic truncated exponential
CPR - cardiopulmonary resuscitation
EMS - emergency medical services
ERC - European Resuscitation Council
OPALS - Ontario Prehospital Advanced Life Support Study
ORBIT - Out‐of‐hospital Rectilinear Biphasic Investigational Trial
PAD - public access defibrillation
RLB - rectilinear biphasic
SCA - sudden cardiac arrest
VF - ventricular fibrillation
VT - ventricular tachycardia
Footnotes
Conflict of interest statement: The author does not have any financial or other conflict of interest
References
- 1.Larsen M P, Eisenberg M S, Cummins R O.et al Predicting survival from out‐of‐hospital cardiac arrest: a graphic model. Ann Emerg Med 1993221652–1658. [DOI] [PubMed] [Google Scholar]
- 2.Murray C J, Lopez A D. Mortality by cause for eight regions of the world: global burden of disease study. Lancet 19973491269–1276. [DOI] [PubMed] [Google Scholar]
- 3.Sans S, Kesteloot H, Kromhout D. The burden of cardiovascular diseases mortality in Europe. Task force of the European Society of Cardiology on Cardiovascular Mortality and Morbidity Statistics in Europe. Eur Heart J 1997181231–1248. [PubMed] [Google Scholar]
- 4.Kesteloot H, Sans S, Kromhout D. Evolution of all‐causes and cardiovascular mortality in the age group 75–85 years in Europe during the period 1970–1996: a comparison with worldwide changes. Eur Heart J 200223384–398. [DOI] [PubMed] [Google Scholar]
- 5.Fox R. Trends in cardiovascular mortality in Europe. Circulation 1997963817. [PubMed] [Google Scholar]
- 6.Levi F, Lucchini F, Negri E.et al Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world. Heart 200288119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng Z J, Groft J B, Giles W H.et al Sudden cardiac death in the United States, 1989 to 1998. Circulation 20011042158–2163. [DOI] [PubMed] [Google Scholar]
- 8.Chugh S S, Jui J, Gunson K.et al Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate‐based review in a large US community. J Am Coll Cardiol 2004441268–1275. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention Web‐based injury statistics Query and Reporting System (Wis QARS) (Online). Centres for Disease Control and Prevention. www.cdc.gov/ncipc/wisqars
- 10.Stiell I G, Wells G A, Field B J.et al Improved out of hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: OPALS study phase III. Ontario pre‐hospital advanced life support. JAMA 19992811175–1181. [DOI] [PubMed] [Google Scholar]
- 11.Pell J P, Sirel J M, Marsden A K.et al Presentation, management and outcome of out of hospital cardiac arrest: comparison by underlying aetiology. Heart 200389839–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herlitz J, Bahr J, Fischer M.et al Resuscitation in Europe: a tale of five European regions. Resuscitation 199941121–131. [DOI] [PubMed] [Google Scholar]
- 13.Valenzuela T D, Roe D J, Nichol G.et al Outcome of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med 20003431206–1209. [DOI] [PubMed] [Google Scholar]
- 14.Vaillancourt C, Stiell I G. Cardiac arrest care and emergency medical services in Canada. Can J Cardiol 2004201081–1090. [PubMed] [Google Scholar]
- 15.Rea T D, Eisenberg M S, Sinibaldi G.et al Incidence of EMS‐treated out‐of‐hospital cardiac arrest in the United States. Resuscitation 20046317–24. [DOI] [PubMed] [Google Scholar]
- 16.Cobb L A, Fahrenbruch C E, Olsufka M.et al Changing incidence of out‐of‐hospital ventricular fibrillation, 1980‐2000. JAMA 20022883008–3013. [DOI] [PubMed] [Google Scholar]
- 17.Cobb L A, Fahrenbruch C E, Walsh T R.et al Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out of hospital ventricular fibrillation. JAMA 19992811182–1188. [DOI] [PubMed] [Google Scholar]
- 18.Wik L, Hansen T B, Fylling F.et al Delayed defibrillation to give basic cardiopulmonary resuscitation to patients with out of hospital ventricular fibrillation: a randomized trial. JAMA 20032891389–1395. [DOI] [PubMed] [Google Scholar]
- 19.American Heart Association American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2005112 (suppl) [DOI] [PubMed] [Google Scholar]
- 20.Kouwenhoven W B, Jude J R, Knickerbocker G G. Closed‐chest cardiac message. JAMA 19601371064–1067. [DOI] [PubMed] [Google Scholar]
- 21.European Resuscitation Council European Resuscitation Council guidelines for resuscitation 2005. Resuscitation 2005
- 22.Ibrahim W H, Gehani A A. Insight into the new changes in European Resuscitation Council Guidelines for adult resuscitation (2005). Middle East J Emerg Med 2006621–24. [Google Scholar]
- 23.Valenzuela T D, Roe D J, Cretin S.et al Estimating effectiveness of cardiac arrest interventions, a logistic regression survival model. Circulation 1997963308–3313. [DOI] [PubMed] [Google Scholar]
- 24.Holmberg M, Holmberg S, Helitz J. Effects of bystander cardiopulmonary resuscitation in out of hospital cardiac arrest in Sweden. Resuscitation 20044759–70. [DOI] [PubMed] [Google Scholar]
- 25.Swor R A, Jackson R E, Cynar M.et al Bystander CPR, ventricular fibrillation, and survival in witnessed, unmonitored out of hospital cardiac arrest. Ann Emerg Med 199525780–784. [DOI] [PubMed] [Google Scholar]
- 26.Litwin P E, Eisenberg M S, Hallstrom A P.et al The location of collapse and its effect on survival from cardiac arrest. Ann Emerg Med 198716787–791. [DOI] [PubMed] [Google Scholar]
- 27.Ballew K A. Recent advances in cardiopulmonary resuscitation. BMJ 19973141462–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson R G, Hallstrom A P, Cobb L A. Bystander‐initiated cardiopulmonary resuscitation in the management of ventricular fibrillation. Ann Intern Med 197990737. [DOI] [PubMed] [Google Scholar]
- 29.Steill I G, Wells G A, De Maio V J.et al Modifiable factors associated with improved cardiac arrest in a multicenter basic life support/defibrillation system. OPLAS study phase I results. Ann Emerg Med 19993344–50. [DOI] [PubMed] [Google Scholar]
- 30.Steill I, Nichol G, Wells G.et al Health‐related quality of life is better for cardiac arrest survivors who received citizen cardiopulmonary resuscitation. Circulation 20031081939–1944. [DOI] [PubMed] [Google Scholar]
- 31.Cummins R O, Ornato J P, Thies W H.et al Improving survival from sudden cardiac arrest: “The chain of survival” concept: a statement for health professional from ACLS subcommittee and the ECC committee. AHA. Circulation 1991831832–1847. [DOI] [PubMed] [Google Scholar]
- 32.Herlitz J, Ekstorm L, Wennerblom B.et al Effects of bystander initiated CPR on ventricular fibrillation and survival after witnessed cardiac arrest outside hospital. Br Heart J 199472408–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Idris A, Roppolol L. Barriers to dispatcher‐assisted telephone cardiopulmonary resuscitation. Ann Emeg Med 200342738–740. [DOI] [PubMed] [Google Scholar]
- 34.Eberle B, Dick W F, Schneider T.et al Checking the carotid pulse: diagnostic accuracy of first responders in patients with and without a pulse. Resuscitation 199633107–116. [DOI] [PubMed] [Google Scholar]
- 35.Bahr J, Kingler H, Panzer W.et al Skills of lay people in checking the carotid pulse. Resuscitation 19973523–26. [DOI] [PubMed] [Google Scholar]
- 36.Kern K B, Hilwig R W, Berg R A.et al Importance of chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay‐rescuer scenario. Circulation 2002105745–749. [DOI] [PubMed] [Google Scholar]
- 37.Kern K B, Hilwig R W, Berg R A.et al Efficacy of chest compression‐only BLS CPR in the presence of occluded airway. Resuscitation 199839179–188. [DOI] [PubMed] [Google Scholar]
- 38.Berg R A. Role of mouth‐to‐mouth rescue breathing in bystander CPR for asphyxial cardiac arrest. Crit Care Med 200028(suppl)N193–N195. [DOI] [PubMed] [Google Scholar]
- 39.Wik L, Kramer‐Johansen J, Myklebust H.et al Quality of cardiopulmonary resuscitation during out of hospital cardiac arrest. JAMA 2005293299–304. [DOI] [PubMed] [Google Scholar]
- 40.Abella B S, Alvarado J P, Myklebust H.et al Quality of cardiopulmonary resuscitation during in hospital cardiac arrest. JAMA 2005293305–310. [DOI] [PubMed] [Google Scholar]
- 41.Abella B S, Sandbo N, Vassilatos P.et al Chest compression rates during CPR are suboptimal: a prospective study during in‐hospital cardiac arrest. Circulation 2005111428–434. [DOI] [PubMed] [Google Scholar]
- 42.Valenzuela T D, Kern K B, Clark L L.et al Interruptions of chest compressions during emergency medical systems resuscitation. Circulation 20051121259–1265. [DOI] [PubMed] [Google Scholar]
- 43.Babbs C F, Kern K B. Optimum compression to ventilation ratios during CPR under realistic, practical conditions: a physiological and mathematical analysis. Resuscitation 200254147–157. [DOI] [PubMed] [Google Scholar]
- 44.Sanders A B, Kern K B, Berg R A.et al Survival and neurological outcome after cardiopulmonary resuscitation with four different chest compression‐ventilation ratios. Ann Emerg Med 200240553–562. [DOI] [PubMed] [Google Scholar]
- 45.Yannopoulos D, Aufderheide T, Gabrielle A.et al Clinical and hemodynamic comparison of 15:2 and 30:2 compression‐to‐ventilation ratio for cardiopulmonary resuscitation. Crit Care Med 2006341444–1449. [DOI] [PubMed] [Google Scholar]
- 46.Haziniski M F, Nadkarni V M, Hickey R W.et al Major changes in the 2005 AHA guidelines for CPR and ECC. Reaching the tipping point for change. Circulation 2005112206–211. [DOI] [PubMed] [Google Scholar]
- 47.Rea T D, Eisenberg M S, Becker J.et al Temporal trends in sudden cardiac arrest: A 25‐year Emergency medical services perspective. Circulation 20031072780–2785. [DOI] [PubMed] [Google Scholar]
- 48.Holmberg M, Holmberg S, Herlitz J. incidence, duration and survival of ventricular fibrillation in out‐of‐hospital cardiac arrest patients in Sweden. Resuscitation 2000447–17. [DOI] [PubMed] [Google Scholar]
- 49.Hong M F, Dorian P. Update on advanced life support and resuscitation techniques. Curr Opin Cardiol 2004201–6. [PubMed] [Google Scholar]
- 50.Bunch T J, White R D, Gresh B J.et al Long‐term outcomes of out‐of‐hospital cardiac arrest after successful early defibrillation. N Engl J Med 20033482626–2633. [DOI] [PubMed] [Google Scholar]
- 51.Anon International Consensus Conference on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with treatment recommendations. January 23–30, 2005, Dallas [DOI] [PubMed]
- 52.Yakaitis R W, Ewy G A, Otto C W.et al Influence of time and therapy on ventricular fibrillation in dogs. Crit Care Med 19808157–163. [DOI] [PubMed] [Google Scholar]
- 53.Niemann J T, Cruz B, Garner D.et al Immediate counter shock versus CPR before counter shock in a 5‐minute swine model of ventricular fibrillation arrest. Ann Emerg Med 200036543–546. [DOI] [PubMed] [Google Scholar]
- 54.Jacobs I G, Finn J C, Oxer H F.et al CPR before defibrillation in out‐of‐hospital cardiac arrest: a randomized trial. Emerg Med Australas 20051739–45. [DOI] [PubMed] [Google Scholar]
- 55.Yu T, Weil M H, Tang W.et al Adverse outcomes of interrupted precordial compression during automated defibrillation. Circulation 2002106368–372. [DOI] [PubMed] [Google Scholar]
- 56.Eftestol T, Sunde K, Steen P A. Effects of interrupting precordial compressions on the calculated probability of defibrillation success during out‐of‐hospital cardiac arrest. Circulation 20021052270–2273. [DOI] [PubMed] [Google Scholar]
- 57.van Alem A P, Chapman F W, Lank W.et al A prospective, randomized and blinded comparison of first shock success of monophasic and biphasic waveforms in out‐of‐hospital cardiac arrest. Resuscitation 20035827–34. [DOI] [PubMed] [Google Scholar]
- 58.Bain A C, Swerdlow C D, Love C J.et al Multicenter study of principles‐based waveforms for external defibrillation. Ann Emerg Med 2001375–12. [DOI] [PubMed] [Google Scholar]
- 59.Poole J E, White R D, Kanz K G.et al Low‐energy impedance‐compensating biphasic waveforms terminate ventricular fibrillation at high rates in victims of out‐of‐hospital cardiac arrest. LIFE investigators. J Cardiovasc Electrophysiol 199781373–1385. [DOI] [PubMed] [Google Scholar]
- 60.White R D, Blackwell T H, Russell J K.et al Transthoracic impedance doesn't affect defibrillation, resuscitation, or survival in patients with out‐of‐hospital cardiac arrest treated with non‐escalating biphasic waveform defibrillator. Resuscitation 20056463–69. [DOI] [PubMed] [Google Scholar]
- 61.Mittal S, Ayati S, Stein K M.et al Comparison of a novel rectilinear biphasic waveform with a damped sine monophasic waveform for transthoracic ventricular defibrillation. ZOLL investigators. J Am Coll Cardiol 1999341595–1601. [DOI] [PubMed] [Google Scholar]
- 62.Scneider T, Martens P R, Paschen H.et al Multicenter, randomized, controlled trial of 150‐J biphasic shocks compared with 200 to 360‐J monophasic socks in the resuscitation of out‐of‐hospital cardiac arrest victims. Circulation 20001021780–1787. [DOI] [PubMed] [Google Scholar]
- 63.Hess E P, White R D. Ventricular fibrillation is not provoked by chest compression during post‐shock organized rhythms in out‐of‐hospital cardiac arrest. Resuscitation 2005667–11. [DOI] [PubMed] [Google Scholar]
- 64.Monsieurs K G, Handley A J, Bossaert L L. ERC Guidelines for Automated External Defibrillation. A statement from the Basic Life Support and Automated External defibrillation working Group (1) and approved by the Executive Committee of the European Resuscitation Council. Resuscitation 200148207–209. [DOI] [PubMed] [Google Scholar]
- 65.Dickey W, Dalzell G W, Anderson J M.et al The accuracy of decision‐making of semi‐automatic defibrillator during cardiac arrest. Eur Heart J 199213608–615. [DOI] [PubMed] [Google Scholar]
- 66.Weaver W D, Hill D, Fahrenbrunch C E.et al Use of the automatic external defibrillator in the management of out‐of‐hospital cardiac arrest. N Engl J Med 1988319661–666. [DOI] [PubMed] [Google Scholar]
- 67.Cecchin F, Jorgensen D B, Berul C I.et al Is arrhythmia detection by automatic external defibrillator accurate for children? Sensitivity and specificity of an automatic external defibrillator in 696 pediatric arrhythmias. Circulation 20011032483. [DOI] [PubMed] [Google Scholar]
- 68.Mattioni T A, Nadermanee K, Brodsky M.et al Initial clinical experience with fully automatic in‐hospital external cardioverter defibrillator. Pacing Clin Electrophysiol 1999221648. [DOI] [PubMed] [Google Scholar]
- 69.Martinez‐Rubio A, Kanaan N, Borggrefe M.et al Advances for treating in‐hospital cardiac arrest: safety and effectiveness of a new automatic external cardioverter‐defibrillator. J Am Coll Cardiol 200341627. [DOI] [PubMed] [Google Scholar]
- 70.Atkinson E, Mikysa B, Conway J A.et al Specificity and sensitivity of automated external defibrillator rhythm analysis in infants and children. Ann Emerg Med 200342185. [DOI] [PubMed] [Google Scholar]
- 71.Hallstrom A P, Ornato J P, Weisfeldt M.et al The Public Access Defibrillator Trial Investigators. Public access defibrillation and survival after out‐of‐hospital cardiac arrest. N Engl J Med 2004351637–646. [DOI] [PubMed] [Google Scholar]
- 72.Caffery S L, Willoughby P J, Pepe P E.et al Public use of automated external defibrillators. N Engl J Med 20023471242–1247. [DOI] [PubMed] [Google Scholar]
- 73.Weisfeldt M L, Kerber R E, McGoldrick R P.et al American Heart Association Report on Public Access Defibrillation Conference. December 8–10, 1994. Automatic External Defibrillator Task Force. Circulation 1995922740–2747. [DOI] [PubMed] [Google Scholar]
- 74.Weisfeldt M L, Kerber R E, McGoldrick R P.et al Public access defibrillation: a statement for health care professionals from the American Heart Association Task Force on Automatic External Defibrillation. Circulation 1995922763. [DOI] [PubMed] [Google Scholar]
- 75.Nichol G, Hallstrom A P, Ornato J P.et al Potential cost‐effectiveness of public access defibrillation in the United States. Circulation 1998971315–1320. [DOI] [PubMed] [Google Scholar]
- 76.Antman E M, Anbe D T, Armstrong P E.et al ACC/AHA guidelines for management of patients with ST‐elevation myocardial infarction. Circulation 2004110588. [DOI] [PubMed] [Google Scholar]
- 77.Morrison L J, Dorian P, Long J.et al Out‐of‐hospital cardiac arrest rectilinear biphasic to monophasic damped sine defibrillation waveforms with advanced life support intervention trial (ORBIT). Resuscitation 200566149–157. [DOI] [PubMed] [Google Scholar]
- 78.Weaver W D, Cobb L A, Copass M K.et al Ventricular defibrillation: a comparative trial using 175‐J and 320‐J socks. N Engl J Med 19823071101–1106. [DOI] [PubMed] [Google Scholar]
- 79.Haziniski M F, Nolan P, Becker L B.et al Controversial topics from the 2005 International Consensus Conference on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with treatment recommendations. Circulation 2005112133–136. [DOI] [PubMed] [Google Scholar]
- 80.The Hypothermia After Cardiac Arrest Study Group Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002346549–556. [DOI] [PubMed] [Google Scholar]
- 81.Bernard S A, Gray T W, Buist M D.et al Treatment of comatose survivors of out‐of‐hospital cardiac arrest with induced hypothermia. N Engl J Med 2002346557–563. [DOI] [PubMed] [Google Scholar]
- 82.Herlitz J, Castren M, Friberg H.et al Postresuscitation care: what are the therapeutic alternatives and what do we know? Resuscitation 20066915–22. [DOI] [PubMed] [Google Scholar]
- 83.Otto C W, Yakaitis R W, Ewy G A. Effects of epinephrine on defibrillation in ischemic ventricular fibrillation. Am Emerg Med 19853285. [DOI] [PubMed] [Google Scholar]
- 84.Brunette D D, Jameson S J. Comparison of standard versus high‐dose epinephrine in the resuscitation of cardiac arrest in dogs. Ann Emeg Med 1990198. [DOI] [PubMed] [Google Scholar]
- 85.Steill I G, Hebert M D, Weitzman B N.et al High dose epinephrine in the adult cardiac arrest. N Engl J Med 19923271045. [DOI] [PubMed] [Google Scholar]
- 86.Brown C G, Martin D R, Pepe P E.et al A comparison of standard‐dose epinephrine and high‐dose epinephrine in cardiac arrest outside the hospital. The multicenter high dose epinephrine study group. N Engl J Med 19923271051. [DOI] [PubMed] [Google Scholar]
- 87.Callaham M, Madsen C D, Barton C W.et al A randomized clinical trial of high‐dose epinephrine and nor‐epinephrine versus standard‐dose epinephrine in prehospital cardiac arrest. JAMA 19922682667. [PubMed] [Google Scholar]
- 88.Lindner K H, Prengel A W, Brinkmann A.et al Vasopressin administration in refractory cardiac arrest. Ann Intern Med 19661241061–1064. [DOI] [PubMed] [Google Scholar]
- 89.Lindner K H, Dirks B, Strohmenger H U.et al Randomized comparison of epinephrine and vasopressin in patients with out‐of‐hospital ventricular fibrillation. Lancet 1997349535–537. [DOI] [PubMed] [Google Scholar]
- 90.American Heart Association in collaboration with International Liaison Committee on Resuscitation. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. Part 6: advanted cardiovascular life support: section 6: pharmacology II: agents to optimize cardiac output and blood pressure. Circulation 2000102(suppl 8)I129–I135. [PubMed] [Google Scholar]
- 91.Steill I G, Herbert P C, Wells G A.et al Vasopressin versus epinephrine for in‐hospital cardiac arrest: a randomized controlled trial. Lancet 2001358105–109. [DOI] [PubMed] [Google Scholar]
- 92.Wenzel V, Krismer A C, Arntz H R.et al A comparison of vasopressin and epinephrine for out‐of‐hospital cardiopulmonary resuscitation. N Engl J Med 2004350105–113. [DOI] [PubMed] [Google Scholar]
- 93.Aung K, Haty T. Vasopressin for cardiac arrest: a systematic review and meta‐analysis. Arch Intern Med 200516517–24. [DOI] [PubMed] [Google Scholar]