Abstract
Our review of angiostrongyliasis in China found that the disease is emerging as a result of changes in food consumption habits and long-distance transportation of food. Enhanced understanding of angiostrongyliasis epidemiology, increased public awareness about the risks associated with eating raw food, and enhanced food safety measures are needed.
Keywords: angiostrongyliasis, Angiostrongylus cantonensis, epidemiology, outbreak, China, dispatch
Angiostrongylus cantonensis was first described as a parasite of the Norway rat (Rattus norvegicus) and the black rat (R. rattus) in Guangzhou (formerly Canton), People’s Republic of China, in 1933. The first human case was reported from Taiwan in 1945. Transmission to humans is primarily by consumption of raw snails. Contaminated vegetables and paratenic hosts such as freshwater prawns, crabs, and frogs may also play a role in transmission (1).
The first case of human angiostrongyliasis in mainland China was diagnosed in 1984 (2). During the past decade, the number of cases has sharply increased (3). A large outbreak occurred in Beijing during 2006. The outbreak peaked during August and involved 160 persons, 100 of whom were hospitalized. This number of patients is similar to the total number of infections recorded in China over the past decade. Our aim was to briefly review angiostrongyliasis outbreaks in mainland China, update angiostrongyliasis epidemiology, and recommend measures to prevent and control angiostrongyliasis.
The Study
The first reported outbreak of angiostrongyliasis in China occurred in 1997 in the city of Wenzhou in the eastern coastal Zhejiang province; it affected 65 persons (4). Since 2000, 6 more outbreaks have been reported, along with numerous individual cases. A literature review found 334 recorded cases; only 4 cases were reported between 1984 and the 1997 outbreak in Wenzhou city. The 7 outbreaks summarized in Table 1 accounted for 86.5% of the total cases.
Table 1. Reported angiostrongyliasis outbreaks in mainland China since 1997.
| Year | Location (city, province) | No. infections | Source of infection | Reference* |
|---|---|---|---|---|
| 1997 | Wenzhou, Zhejiang | 65 | Pomacea canaliculata† | Zheng RY et al., 2001 |
| 2002 | Changle, Fujian | 8 | P. canaliculata† | Lin JX et al., 2003 |
| 2002 | Fuzhou, Fujian | 9 | P. canaliculata† | Yang FZ et al., 2004 |
| 2002 | Fuzhou, Fujian | 13 | Achatina fulica‡ | Wu CH et al., 2004 |
| 2004 | Kunming, Yunnan | 25 | P. canaliculata† | Han JH et al., 2005 |
| 2005 | Kunming, Yunnan | 9 | P. canaliculata† | Wei LP et al., 2005 |
| 2006 | Beijing, Beijing | 160 | P. canaliculata† | Not available |
*Full reference details are available from the corresponding author upon request. †Common name, apple snail. ‡Common name, giant African land snail.
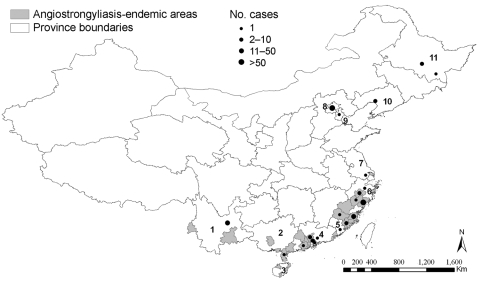
The Figure depicts the 9 provinces in China where angiostrongyliasis has been reported thus far. The youngest patient was 11 months of age, and the oldest was 70 years of age. In the recent Beijing outbreak, 99 of the 100 hospitalized patients were available for interview; 59 were male and 40 were female, age range was 13–57 years, median age was 36 years. The causative agent was confirmed for 16 (4.8%) of 334 cases. Four children died. Outbreak investigations found that 75.1% of all patients had eaten raw apple snails (Pomacea canaliculata) or raw giant African land snails (Achatina fulica).
Figure.
Provinces in People’s Republic of China where cases of angiostrongyliasis has been reported and locations where outbreaks occurred. Province names: 1, Yunnan; 2, Guangxi; 3, Hainan; 4, Guangdong; 5, Fujian; 6, Zhejiang; 7, Jiangsu; 8, Beijing; 9, Tianjing; 10, Liaoning; 11, Heilongjiang.
A. cantonensis–endemic foci have been discovered in the provinces of Fujian, Guangxi, Hainan, Yunnan, and Zhejiang (Figure). Jinhua city in Zhejiang province is the parasite-endemic setting furthest north. Infected A. fulica were found in a farm (used for temporary cultivation and selling of snails) in Liaoning province in northeast China; however, the infected snails might have been imported from provinces located further south.
Thirty-two species of wild mollusk in China have been screened for A. cantonensis; 22 of these species (68.8%) harbored the parasite (Table 2). The highest rate and intensity of infections were recorded in A. fulica, followed by slugs (Vaginulus spp.) and P. canaliculata. Terrestrial snails and slugs showed higher rates and intensities of infections than freshwater mollusks. However, at least 1 freshwater snail, P. canaliculata, plays an important role in the epidemiology of angiostrongyliasis.
Table 2. Known intermediate hosts of Angiostrongylus cantonensis in mainland China.
| Species | First investigation, y, place | First observation of positive specimens, y, place | Highest recorded prevalence, %, place | Reference* |
|---|---|---|---|---|
| Achatina fulica†‡ | 1979–1982, Guangzhou | 1979–1980, Guangzhou | 96.8, Zhongshan | Ding BL et al., 1982 Liang HK et al., 1984 Liang HK et al., 1992 Zhang HM et al., 1996 |
| Pomacea canaliculata§¶ | 1988, Hekou | 1997, Cangnan | 69.4, Cangnan | Li FH et al., 1989 Pan CW et al., 2002 Li YS et al., 2001 |
| Camaena cicatricosa‡ | 1979–1982, Guangzhou | 1979–1982, Guangzhou | 50.0, Zhongshan | Ding BL et al., 1982 Liang HK et al., 1984 Liang HK et al., 1992 |
| Vaginulus sp.# | 1980–1982, Guangzhou | 1980–1982, Guangzhou | 49.2, Guangzhou | Ding BL et al., 1982 |
| Phiolomycus bilineatus# | 1979–1982, Guangzhou | 1979–1982, Guangzhou | 100, Guangzhou | Ding BL et al., 1982 Liang HK et al., 1984 |
| Deroceras leave# | 2005, Lianjiang/Nan’an | 2005, Lianjiang/Nan’an | 23.8, Lianjiang/Nan’an | Li LS et al., 2006 |
| Vaginulus yuxjsjs sp. nov# | 1988, Hekou | 1988, Hekou | 21.0, Hekou | Li FH et al., 1989 |
| Ariophantidae spp.‡ | 1988, Hekou | 1988, Hekou | 12.0, Hekou | Li FH et al., 1989 |
| Macrochlamys loana# | 2005, Lianjiang/Nan’an | 2005, Lianjiang/Nan’an | 11.2, Lianjiang/Nan’an | Li LS et al., 2006 |
| Limax flavus# | 2005, Lianjiang/Nan’an | 2005, Lianjiang/Nan’an | 10.1, Lianjiang/Nan’an | Li LS et al., 2006 |
| Bradybaena brevispira‡ | 1979–1982, Guangzhou | 1979–1980, Guangzhou | 8.3, Nanhai | Liang HK et al., 1984 Liang HK et al., 1992 Pan CW et al., 2002 |
| Meghimatium bilinestum‡ | 2005, Lianjiang/Nan’an | 2005, Lianjiang/Nan’an | 5.9, Lianjiang/Nan’an | Li LS et al., 2006 |
| Trichochloritis rufopila‡ | 1986–1990, Zhuhai | 1986–1990, Zhuhai | 5.8, Zhuhai | Liang HK et al., 1992 |
| Trichochloritis hungerfordianus‡ | 1986–1990, Zhuhai | 1986–1991, Zhuhai | 5.7, Zhuhai | Liang HK et al., 1992 |
| Vaginulus alte# | 1988, Hekou | 1988, Hekou | 4.2, Hekou | Li FH et al., 1989 |
| Bellamya spp.¶ | 2005, Lianjiang/Nan’an | 2005, Lianjiang/Nan’an | 4.1, Lianjiang/Nan’an | Li LS et al., 2006 |
| Bellamya aeruginosa¶ | 2004, Minhou/Lianjiang | 2004, Minhou/Lianjiang | 3.8, Minhou | Lin JX et al., 2005 |
| Bradybaena similaris‡ | 1980–1982, Guangzhou | 1980–1982, Guangzhou | 3.2, Guangzhou | Ding BL et al., 1982 |
| Bradybaena ravida‡ | 2005, Lianjiang/Nan’an | 2005, Lianjiang/Nan’an | 3.1, Lianjiang/Nan’an | Li LS et al., 2006 |
| Plectotropis appanata‡ | 2005, Lianjiang/Nan’an | 2005, Lianjiang/Nan’an | 2.6, Lianjiang/Nan’an | Li LS et al., 2006 |
| Bellamya quadrata¶ | 1986–1990, Panyu | 1986–1990, Panyu | 2.5, Panyu | Liang HK et al., 1992 |
*Full reference details are available from the corresponding author upon request. †Common name, giant African land snail. ‡Land snail. §Common name, apple snail. ¶Freshwater snail. #Slug.
Of 15 wild rodent species captured in mainland China, 11 harbored A. cantonensis. The prevalence and intensity of infection were generally higher in R. norvegicus than in other rodents. Infections were also found among nonhuman primate, equine, and canine species (5,6). However, the prevalence in domestic animals and nonrodent wildlife remains to be fully investigated.
During surveys of 12 potential paratenic host species in China, A. cantonensis larvae were recovered from frogs (Hylarana guentheri, Rana limnocharis, and R. plancyi) and toads (Bufo melanostictus). In contrast to the situation on different Pacific islands (7,8), A. cantonensis has not yet been found in freshwater shrimp, fish, crabs, and planariae in mainland China.
The A. cantonensis–endemic area in China is rapidly expanding, and causes are multifactorial. First, A. fulica and P. canaliculata have invaded the southern part of China after being imported from East Africa in the 1930s and South America (through Taiwan) in the 1980s, respectively. While both snail species were imported as food, they also became established in the wild fauna and are now common in southern China. Second, vast habitats with suitable environmental conditions can be found in many parts of the country. Recent studies indicate suitable habitats not yet colonized; hence, further expansion of A. cantonensis–endemic settings is cause for concern (9). Finally, the low host specificity of A. cantonensis further supports the expansion of this parasite into new areas.
The predominant freshwater and land snail species found in Chinese markets are P. canaliculata, A. fulica, Cipangopaludina chinensis, and Bellamya aeruginosa. The first 2 account for most A. cantonensis infections in mainland China. In Taiwan, C. chinensis plays an important role in the epidemiology of angiostrongyliasis (10). Recently, B. aeruginosa was found to harbor natural infections with A. cantonensis; several infections have been linked to this species (11,12). Consumption of freshwater shrimp and crabs has increased over consumption of snails. Although only few A. cantonensis infections could be traced to shrimp and crabs and none yet in China, their infection potential merits attention.
Conclusions
The booming economy and rapid infrastructure development in China have affected food production and trade. For example, these developments enabled the countrywide marketing of aquaculture products and snails produced in the southern provinces, which might also be responsible for the emergence of foodborne trematodiasis (13). After the recent angiostrongyliasis outbreak in Beijing, the source of infection was traced to P. canaliculata originating from Guangxi province in southwest China. Socioeconomic changes have also increased the popularity of specific consumption habits across China. Although the residents of the southeastern coastal areas have a long history of eating raw food, including snails and seafood, similar dishes have recently become popular among the urban middle and upper classes in inland China.
After the 2006 outbreak in Beijing, different measures have been proposed for preventing and controlling angiostrongyliasis. First, food safety and transportation must be improved to avoid human infections and the further spread of intermediate host snails to areas in which the disease is not endemic. In snail farms, rigorous control of rats should be implemented. Collection and marketing of wild snails should be limited. Second, hygiene and food preparation techniques in restaurants should be improved to prevent cross-contamination of other food items. Third, these efforts should be accompanied by sound information in communication and education campaigns to raise public awareness. The basic message, that consumption of raw or undercooked snails is a key risk factor for the transmission of a serious disease, can be easily conveyed and is readily understood by the public. After the first outbreak in Wenzhou city in 1997, a comprehensive health education campaign about safe food consumption habits and the most prominent symptoms associated with angiostrongyliasis was launched in Zhejiang province. Few cases were reported thereafter.
Awareness of angiostrongyliasis needs to be improved for consumers and health professionals. Education campaigns should inform consumers about the risk of contracting angiostrongyliasis, e.g., by eating raw snails, and professional knowledge among healthcare providers should be improved to ensure timely detection of infections and adequate medical response.
Acknowledgments
We thank Li-Ying Wang for her support with data collection; Xian-Hong Wang, Kun Yang, Shi-Zhu Li, and He-Xiang Liu for assistance with data analysis; and Jürg Utzinger for revising this manuscript. We are also grateful to the anonymous referees for a set of useful comments on an earlier version of this manuscript.
This work was supported by grants from the National Natural Science Foundation of China (No. 30590373), the Ministry of Science and Technology of China (No. 2005DKA21104), and the Ministry of Health (No. 2006-133).
Biography
Mr Lv works at the National Institute of Parasitic Diseases, Chinese Center for Disease Control and Prevention, in Shanghai. He is engaged in research on the epidemiology of angiostrongyliasis in China and the compatibility of A. cantonensis with different host snails.
Footnotes
Suggested citation for this article: Lv S, Zhang Y, Steinmann P, Zhou X-N. Emerging angiostrongyliasis in mainland China. Emerg Infect Dis [serial on the Internet]. 2008 Jan [date cited]. Available from http://www.cdc.gov/EID/content/14/1/161.htm
References
- 1.Alicata JE. The discovery of Angiostrongylus cantonensis as a cause of human eosinophilic meningitis. Parasitol Today. 1991;7:151–3. 10.1016/0169-4758(91)90285-V [DOI] [PubMed] [Google Scholar]
- 2.He JZ, Zhu SH, Yang SQ, Yu BW, Chen YS, Hu QX, et al. First discovery and evidence of Angiostrongylus cantonensis in the cerebrospinal fluid from a case of the population of mainland China. J Guangzhou Med Coll. 1984;12:1–4. [Google Scholar]
- 3.Chen XG, Li H, Lun ZR. Angiostrongyliasis, mainland China. Emerg Infect Dis. 2005;11:1645–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng RY, Jin R, Lin BC, Pan CW, Xue DY. Probing and demonstrating etiological factors for the outbreak of angiostrongyliasis cantonensis in Wenzhou. Sh J Prev Med. 2001;13:105–7. [Google Scholar]
- 5.Duffy MS, Miller CL, Kinsella JM, Lahunta AD. Parastrongylus cantonensis in a nonhuman primate, Florida. Emerg Infect Dis. 2004;10:2207–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mason KV. Canine neural angiostrongylosis: the clinical and therapeutic features of 55 natural cases. Aust Vet J. 1987;64:201–3. 10.1111/j.1751-0813.1987.tb15181.x [DOI] [PubMed] [Google Scholar]
- 7.Alto W. Human infections with Angiostrongylus cantonensis. Pac Health Dialog. 2001;8:176–82. [PubMed] [Google Scholar]
- 8.Yoshimura K, Sugaya H, Ishida K. The role of eosinophils in Angiostrongylus cantonensis infection. Parasitol Today. 1994;10:231–3. 10.1016/0169-4758(94)90124-4 [DOI] [PubMed] [Google Scholar]
- 9.Lv S, Zhou XN, Zhang Y, Liu HX, Zhu D, Yin WG, et al. The effect of temperature on the development of Angiostrongylus cantonensis (Chen, 1935) in Pomacea canaliculata (Lamarck, 1822). Parasitol Res. 2006;99:583–7. 10.1007/s00436-006-0198-8 [DOI] [PubMed] [Google Scholar]
- 10.Chen ER. Current status of food-borne parasitic zoonoses in Taiwan. Southeast Asian J Trop Med Public Health. 1991;22(Suppl):62–4. [PubMed] [Google Scholar]
- 11.Lin JX, Zhou XN, Li LS, Zhang Y, Cheng YZ, Zhang RY, et al. Bellamya aeruginosa acts as the intermediate host for Angiostrongylus cantonensis. Chin J Zoonoses. 2005;21:24–6. [Google Scholar]
- 12.Li LS, Zhou XN, Lin JX, Zhang Y, Chen YZ, Zhang RY, et al. Discovery of six new host species of Angiostrongylus cantonensis and investigation of the epidemic foci in Fujian province. Chin J Zoonoses. 2006;22:533–7. [Google Scholar]
- 13.Keiser J, Utzinger J. Emerging foodborne trematodiasis. Emerg Infect Dis. 2005;11:1507–14. [DOI] [PMC free article] [PubMed] [Google Scholar]