The incidence in San Diego is increasing and is concentrated mostly in persons of Mexican origin.
Keywords: Mycobacterium bovis, tuberculosis, trends, incidence, epidemiology, immigration, Mexico, mortality, Hispanic, research
Abstract
The epidemiology of tuberculosis (TB) in the United States is changing as the incidence of disease becomes more concentrated in foreign-born persons. Mycobacterium bovis appears to be contributing substantially to the TB incidence in some binational communities with ties to Mexico. We conducted a retrospective analysis of TB case surveillance data from the San Diego, California, region from 1994 through 2005 to estimate incidence trends, identify correlates of M. bovis disease, and evaluate risk factors for deaths during treatment. M. bovis accounted for 45% (62/138) of all culture-positive TB cases in children (<15 years of age) and 6% (203/3,153) of adult cases. M. bovis incidence increased significantly (p = 0.002) while M. tuberculosis incidence declined (p<0.001). Almost all M. bovis cases from 2001 through 2005 were in persons of Hispanic ethnicity. Persons with M. bovis were 2.55× (p = 0.01) as likely to die during treatment than those with M. tuberculosis.
The pattern of tuberculosis (TB) in the United States is changing as the incidence of TB disease becomes more concentrated in foreign-born persons. Of the annual total US TB cases, >54% are now concentrated in persons born outside of the United States (1); in communities with high immigration, the proportion can exceed 70% (2). TB prevention and treatment strategies, particularly those in communities on the border with Mexico, will need to be adapted to accommodate the changing epidemiology of TB (3).
San Diego, California, together with its sister city Tijuana-Tecate, Mexico, is the largest binational metropolitan region in the United States, accounting for 34% of the southern border population (4). In San Diego County, the Hispanic population has grown from 20% to 29% in the past 15 years (5). Of the total annual TB cases in San Diego, >70% occurred among foreign-born persons, of whom nearly half originated from Mexico (2). A review of culture-positive TB cases in San Diego County in the late 1990s indicated that 6.6% of all adult TB cases and 39% of all pediatric (<15 years of age) TB cases from this region were not caused by Mycobacterium tuberculosis, the most common TB pathogen in the United States, but were instead caused by M. bovis, a pathogen more often associated with TB in cattle (6). This finding represented the highest reported proportional incidence of TB from M. bovis among industrialized countries (7).
M. bovis is a pathogen in the complex of bacteria that includes M. tuberculosis, which causes TB in humans and animals. TB from M. bovis has been generally considered rare in the United States after its successful eradication from cattle in the mid-1900s (8), but wider use of laboratory tools for species-level diagnosis of TB pathogens has started to shed light on an unexpected regional presence of M. bovis in communities with large Hispanic populations. While M. bovis TB has been most often documented in Hispanic communities with close proximity to Mexico (6,9), a recent review of M. bovis cases in New York City indicates that the problem is not limited to US regions that border Mexico (10).
The clinical and pathologic characteristics of M. bovis TB is indistinguishable from M. tuberculosis TB in most cases, but there are relevant considerations for prevention and treatment strategies in communities where M. bovis contributes to TB incidence. First, M. bovis is thought to be spread to humans primarily through consumption of raw dairy products and inhalation of infectious droplets from cattle (11,12), with only minimal human-to-human transmission (13). Second, M. bovis is almost universally resistant to the key antituberculous drug pyrazinamide (PZA), which necessitates a 9-month treatment duration instead of the standard 6-month, short-course therapy, which is possible with PZA in the treatment regime. Third, higher mortality rates during treatment may be associated with M. bovis (14).
Multidrug-resistant (MDR) strains of M. bovis (15–17), the high proportional incidence of M. bovis (9,18) in pediatric TB cases, and frequent HIV co-infection (19) are important additional considerations in developing effective treatment and prevention strategies for M. bovis. To document the trends and the effect of M. bovis on TB epidemiology, we examined TB case surveillance data from 1994 through 2005 in San Diego County and identified risk factors related to M. bovis disease and deaths during treatment in the last 5 years.
Methods
Data Sources
This study used routine TB surveillance data from 1994 through 2005. The study protocol was approved by the Institutional Review Boards of San Diego State University and the University of California, San Diego. Demographic and clinical data were obtained from the Tuberculosis Information Management System (TIMS) database maintained by the San Diego County TB Control Program. Since the early 1990s, a TB isolate has been submitted to the county public health laboratory for every reported TB case. All TB isolates from patient specimens were initially identified as M. tuberculosis complex on the basis of the AccuProbe hybridization protection assay (GenProbe, San Diego, CA, USA). Specimens were further identified as either M. bovis or M. tuberculosis on the basis of culture morphologic findings, the results of the niacin strip test, the nitrate reduction test, and the specimens’ susceptibility to PZA (20). Furthermore, all isolates identified as M. bovis from 2004 and 2005 were confirmed to have spoligotypes consistent with M. bovis (21). Population data for San Diego County were obtained from San Diego Association of Governments’ estimates based on census and calculated data.
Study Design
We conducted a retrospective trend analysis of all culture-positive TB cases in the San Diego County TIMS database from 1994 through 2005 that were confirmed as either M. bovis or M. tuberculosis. We also conducted a detailed retrospective analysis of demographic and clinical variables associated with M. bovis case-patients and deaths during treatment from 2001 through 2005.
Demographic variables from the TIMS database used in the correlates and mortality analyses included sex, age, ethnicity, and country of birth. Clinical variables included: previous history of TB disease, presence or absence of pulmonary disease, presence or absence of multisite disease, presence or absence of acid-fast bacilli (AFB) in sputum smear, presence or absence of pulmonary lesions by chest radiograph, presence or absence of MDR TB, and HIV status.
Analysis
Trends
Trends in TB incidence were evaluated by using Poisson regression with time in years as the predictor variable, case number as the dependent variable, and population size as an additional exposure variable. Trend lines for M. bovis and M. tuberculosis were based on incidence predicted by Poisson regression fitted to the data. Trends in proportional incidence of M. bovis cases (relative to all TB cases) were assessed with a χ2 test for trend.
Correlates of M. bovis Disease
Demographic and clinical variables shown previously to be associated with TB diagnoses (6) were compared between M. bovis and M. tuberculosis. Variables significant at the 5% level by χ2 test in univariate analyses were entered into a multiple logistic regression model. The final model was derived by using the likelihood ratio method (22).
Analysis of Mortality Rates during Treatment
All deaths that occurred from the time that a TB case was reported until treatment was completed were documented with death certificates and recorded in TB case files. For the purposes of this study, causes of death in M. bovis and M. tuberculosis case files were transcribed from death certificates or California state death records and collated into 7 major causes of death based on the most common causes.
We investigated the apparently higher mortality rates during treatment among M. bovis cases relative to M. tuberculosis cases (14) by using a multiple logistic regression analysis with M. bovis as the exposure variable; death before treatment was completed as the outcome variable; and demographic and clinical variables as potential covariates. Univariate differences between causes of death in M. bovis and M. tuberculosis cases were analyzed with the Fisher exact test.
Results
Trends
Analysis of TB trends from 1994 through 2005 included 3,291 culture-positive cases of TB and excluded 806 cases (20%) that were based only on national and local clinical case definitions. Among all culture-positive cases, M. bovis was isolated in 8% (265/3,291) and M. tuberculosis in 92% (3,026/3,291). M. bovis accounted for 45% (62/138) of all culture-positive TB cases in children <15 years of age and 6% (203/3,153) of cases in adults (>15 years of age). No cases of M. bovis occurred in children <12 months of age.
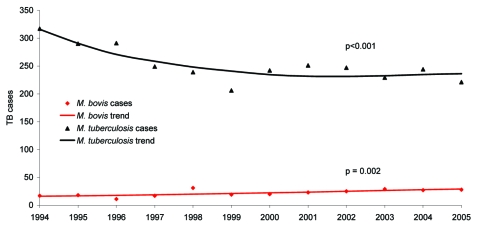
During the period under study, incident cases of M. bovis TB increased linearly (p = 0.002; Figure) at 4.1% per year from 17 cases (0.65/100,000 population) to 28 cases (0.93/100,000) per year. TB cases from M. tuberculosis declined in a nonlinear fashion (p<0.001) from 317 cases per year (12.1/100,000 population) to 221 cases (7.33/100,000). The annual proportion of TB cases attributed to M. bovis increased from 5% of all culture-positive cases in 1994 to 11% in 2005 (p<0.001, Table 1). The proportion of TB cases with culture-positive results remained relatively stable at ≈81% of annual reported TB cases.
Figure.
Trends in incidence of culture-positive tuberculosis (TB) cases from Mycobacterium bovis and M. tuberculosis in San Diego County, California, 1994–2005.
Table 1. Proportional contribution of Mycobacterium bovis and M. tuberculosis to total culture-positive TB cases, San Diego County, California, 1994–2005*.
| Year | Total TB cases | Total no. (%) culture-positive TB cases† | No. (%)‡ M. bovis cases | No. (%)‡ M. tuberculosis cases |
|---|---|---|---|---|
| 1994 | 420 | 334 (80) | 17 (5) | 317 (95) |
| 1995 | 438 | 308 (70) | 18 (6) | 290 (94) |
| 1996 | 384 | 302 (79) | 11 (4) | 291 (96) |
| 1997 | 332 | 266 (80) | 17 (6) | 249 (94) |
| 1998 | 342 | 270 (79) | 31 (11) | 239 (89) |
| 1999 | 299 | 225 (75) | 19 (8) | 206 (92) |
| 2000 | 295 | 262 (89) | 20 (8) | 242 (92) |
| 2001 | 330 | 274 (83) | 23 (8) | 251 (92) |
| 2002 | 317 | 272 (86) | 25 (9) | 247 (91) |
| 2003 | 315 | 258 (82) | 29 (11) | 229 (89) |
| 2004 | 320 | 271 (85) | 27 (10) | 244 (90) |
| 2005 | 305 | 249 (82) | 28 (11) | 221 (89) |
*TB, tuberculosis. †Excludes 11 case-patients who had an isolate of M. tuberculosis complex resistant to pyrazinamide, but did not have species-level identification. Percent given is of all TB cases. ‡Percent given is of total culture-positive TB case-patients.
Correlates of M. bovis Disease
Of the 1,324 culture-positive TB cases reported from 2001 through 2005, M. bovis accounted for 10% (132/1,324), comprising 54% (29/54) of cases among children <15 years of age and 8% (103/1,270) among adults (>15 years of age). Of the M. bovis TB cases, >96% were found in persons of Hispanic ethnicity, and 60% were among those of known Mexican origin. Univariate analysis indicated that sex, previous TB episode, and sputum AFB smear results were not significantly different between M. bovis and M. tuberculosis case-patients (Table 2). No MDR TB cases were identified among the M. bovis cases, whereas 1.5% of the M. tuberculosis cases had initial isolates that were MDR (defined as resistant to at least both isoniazid and rifampin). All of the M. bovis isolates were resistant to PZA, whereas 0.8% of the M. tuberculosis cases were PZA resistant. Of the 1,316 TB cases included in the multiple logistic regression model, factors associated with M. bovis disease included Hispanic ethnicity, multisite disease, being 5–14 years of age, and having extrapulmonary disease with a normal chest radiograph. HIV co-infection was not significantly more associated with M. bovis disease compared with M. tuberculosis (p = 0.08; Table 3).
Table 2. Univariate comparison of Mycobacterium bovis cases relative to M. tuberculosis cases, San Diego County, California, 2001–2005*.
| Characteristic | No. (%)†M. bovis cases, n = 132 | No. (%)† M. tuberculosis cases, n = 1,192 | Univariate p value |
|---|---|---|---|
| Sex | 0.15 | ||
| M | 75 (56.8) | 754 (63.2) | |
| F |
57 (43.2) |
438 (36.7) |
|
| Age group, y | <0.001 | ||
| 0–4 | 15 (11.4) | 10 (0.8) | |
| 5–14 | 14 (10.6) | 15 (1.3) | |
| 15–24 | 21 (15.9) | 156 (13.1) | |
| 25–44 | 46 (34.8) | 409 (34.3) | |
| 45–64 | 20 (15.2) | 356 (29.9) | |
| >64 |
16 (12.1) |
246 (20.6) |
|
| Race/ethnicity | <0.001‡ | ||
| Hispanic | 128 (96.9) | 529 (44.3) | |
| White | 3 (2.27) | 151 (12.6) | |
| Asian | 1 (0.75) | 420 (35.2) | |
| Black | 0 | 86 (7.2) | |
| Other |
0 |
6 (1.0) |
|
| Country of birth | <0.001 | ||
| Mexico | 79 (59.8) | 382 (32.0) | |
| United States | 53 (40.2) | 302 (25.3) | |
| Philippines | 0 | 248 (20.8) | |
| Other |
0 |
260 (21.8) |
|
| Previous TB | 0.52 | ||
| Yes | 5 (3.8) | 60 (5.0) | |
| No | 127 (96.2) | 1128 (94.6) | |
| Unknown§ |
0 |
4 (0.3) |
|
| Sputum AFB smear result | 0.16 | ||
| Positive | 40 (30.3) | 590 (49.4) | |
| Negative | 43 (32.5) | 461 (38.6) | |
| Not done§ |
49 (37.1) |
141 (11.8) |
|
| Disease site | <0.001 | ||
| Pulmonary | 71 (53.7) | 1031 (86.4) | |
| Extrapulmonary |
61 (46.2) |
161 (13.5) |
|
| Clinical manifestations | <0.001 | ||
| Single site disease | 84 (63.6) | 1036 (86.9) | |
| Multisite disease |
48 (36.4) |
156 (13.1) |
|
| Chest radiograph lesions | <0.001 | ||
| No lesions | 55 (41.7) | 123 (10.3) | |
| Pulmonary lesions consistent with TB | 75 (56.8) | 1063 (89.2) | |
| Unknown§ |
2 (1.5) |
6 (0.5) |
|
| HIV status | <0.001 | ||
| Negative | 48 (36.4) | 611 (51.3) | |
| Positive | 33 (25.0) | 107 (9.0) | |
| Unknown |
51 (38.6) |
474 (39.8) |
|
| Treatment outcome | 0.02 | ||
| Died before treatment completed | 19 (14.3) | 91 (7.6) | |
| Alive at end of treatment | 102 (77.2) | 913 (76.5) | |
| Unknown | 11 (8.3) | 188 (15.7) |
*TB, tuberculosis; AFB, acid-fast bacillus. †Percentages do not always add up to 100% due to rounding. ‡Fisher exact p value. §Not included in χ2 calculation.
Table 3. Odds ratios from final logistic regression model of variables correlated with TB from Mycobacterium bovis versus M. tuberculosis, San Diego County, California, 2001–2005*.
| Risk factors |
M. bovis vs. M. tuberculosis
(n = 130 vs. n = 1,186) |
|
|---|---|---|
| OR (95% CI) | p value | |
| Age group, y (ref >65 y) | 0.002 | |
| 0–4 | 2.43 (0.81–7.28) | 0.11 |
| 5–14 | 4.38 (1.38–13.9) | 0.01 |
| 15–24 | 1.06 (0.45–2.49) | 0.90 |
| 25–44 | 0.68 (0.31–1.45) | 0.32 |
| 45–64 |
0.50 (0.21–1.15) |
0.10 |
| Race/ethnicity (ref = white) | <0.001 | |
| Hispanic | 7.97 (2.36–26.93) | <0.001 |
| Asian | 0.08 (0.01–0.76) | 0.03 |
| Black | 0 | 0.99 |
| Other |
0 |
0.99 |
| Extrapulmonary disease | 4.51 (2.36–8.62) | <0.001 |
| Normal chest radiograph results | 3.16 (1.63–6.11) | <0.001 |
| Multisite disease |
4.31 (2.54–7.3) |
<0.001 |
| HIV status† (ref = negative) | 0.13 | |
| Positive | 1.75 (0.93–3.29) | 0.08 |
| Unknown | 0.87 (0.48–1.58) | 0.65 |
*n = 1,316. TB, tuberculosis; OR, odds ratio; CI, confidence interval; ref, referent. †Variable not significant in multivariate analysis.
Analysis of Mortality Rates during Treatment
Of 1,324 culture-positive TB case-patients, 1,119 were evaluated in the analysis of mortality rates during treatment. Fifteen percent (205/1,324) were excluded because of missing data on case survival, including patients who were lost to follow-up or moved during treatment. Of the 1,119 cases, 110 (19 M. bovis and 91 M. tuberculosis) patients died during TB treatment (n = 81) or before treatment was begun (n = 29). M. bovis patients who died during treatment were treated for a similar duration (mean 61 days, standard deviation [SD] 93.9) as M. tuberculosis patients (mean 60 days, SD 101.3).
No deaths during treatment were recorded in the pediatric M. bovis TB case-patients; 1 pediatric death was recorded among the M. tuberculosis TB treatment cases. In a multivariate analysis (n = 1,119), M. bovis patients were 2.55× (p = 0.01) as likely to die before treatment completion than M. tuberculosis patients, after differences in age, race and ethnicity, country of birth, chest radiograph abnormalities, multisite disease, and HIV status were accounted for (Table 4). Univariate analyses of the causes of death in M. bovis and M. tuberculosis cases showed no significant differences (p>0.05) except for the category of “other noninfectious disease,” which was overrepresented in the M. tuberculosis group (Table 5).
Table 4. Factors associated with death before completion of TB treatment in TB patients, San Diego County, California, 2001–2005*.
| Risk factor | OR (95% CI) | p value |
|---|---|---|
|
Mycobacterium bovis disease |
2.55 (1.27–5.11) |
0.01 |
| HIV infection (ref = negative) | <0.001 | |
| Positive | 4.50 (2.19–9.24) | <0.001 |
| Unknown |
2.09 (1.19–3.67) |
0.01 |
| Age group, y (ref = 0–4 y) | <0.001 | |
| 5–14 | Not defined | 1.00 |
| 15–24 | 0.79 (0.06–9.88) | 0.86 |
| 25–44 | 1.54 (0.17–13.78) | 0.70 |
| 45–64 | 4.75 (0.55–41.12) | 0.16 |
|
>65 |
17.19 (2.04–145.01) |
0.01 |
| Country of birth (ref = United States) | <0.001 | |
| Mexico | 0.52 (0.30–0.90) | 0.02 |
| Philippines | 0.52 (0.28–0.97) | 0.04 |
| Other |
0.25 (0.12–0.53) |
<0.001 |
| Chest radiograph lesions | 2.21 (0.97–5.05) | 0.06 |
| Multisite disease | 1.86 (1.10–3.15) | 0.02 |
*n = 1,119. TB, tuberculosis; OR, odds ratio; CI, confidence interval; ref, referent.
Table 5. Primary causes of death before treatment completion in Mycobacterium bovis and M. tuberculosis TB case-patients (n = 110), San Diego County, California, 2001–2005*.
| Cause of death | No. (%) Mycobacterium bovis case-patients | No. (%) M. tuberculosis case-patients | p value† |
|---|---|---|---|
| Pulmonary TB | 2 (11) | 20 (22) | 0.42 |
| Extrapulmonary TB | 3 (16) | 8 (9) | 0.58 |
| Pulmonary NOS | 0 | 8 (9) | 0.41 |
| HIV related | 6 (32) | 12 (13) | 0.11 |
| Cardiovascular | 7(37) | 18 (20) | 0.19 |
| Infectious (not TB) | 1(5) | 2 (2) | 0.84 |
| Other noninfectious disease |
0 |
23 (25) |
0.01 |
| Total | 19 | 91 |
*TB, tuberculosis; NOS, not otherwise specified. †Fisher exact test.
Discussion
From 1994 through 2005, incidence of M. bovis TB cases in San Diego County increased in absolute number, as a proportion of total TB cases, and relative to the population. In contrast, TB incidence caused by M. tuberculosis declined during the same period. M. bovis cases were concentrated in persons of Hispanic descent, especially those of Mexican origin, and among those <15 years of age, in whom M. bovis accounted for 45% of the culture-positive cases. Deaths during treatment were largely confined to adults and were twice as high in M. bovis TB case-patients when compared with M. tuberculosis patients.
Our findings indicate that the incidence of TB caused by M. bovis in southern California is substantially higher than the national rate of 1.5% estimated from TB surveillance data (23) but is similar to the proportional incidence (13%) among Mexican-born case-patients in New York, New York. It was previously hypothesized that TB attributed to M. bovis in San Diego is most likely being driven by recent infections in children and largely reactivated latent infections in adults, secondary to HIV co-infection (6). Our findings confirm the continued high incidence of M. bovis in children >12 months of age, but the role of HIV co-infection in M. bovis case-patients relative to M. tuberculosis cases is less clear.
Almost half of the culture-positive pediatric TB cases in this binational region of >3 million persons were caused by M. bovis, which has clinical implications. Since M. bovis is intrinsically resistant to PZA, a critical component of the standard 6-month, short-course treatment for M. tuberculosis, M. bovis treatment is usually extended to 9 months of isoniazid and rifampin (14). In southern California, and perhaps other Hispanic communities with close ties to Mexico, empiric extended TB treatment for children without culture-positive disease, particularly those with a history of consuming unpasteurized dairy products, should be considered.
Although one quarter of the M. bovis TB case-patients were co-infected with HIV, HIV was not significantly more associated with M. bovis TB compared with M. tuberculosis in our study or in the previous M. bovis study in this community (6). Confidence in this finding is somewhat limited because 40% of the TB case-patients did not have their HIV status reported. However, because most of the case-patients with an unknown HIV status were <15 or >55 years of age, the age groups at lowest risk for HIV, these missing data likely did not mask an association if one exists.
HIV co-infection plays a role in the epidemiology of adult M. bovis TB, but likely the growing Hispanic population with close ties to Mexico, and not HIV, is the major driving force behind the increasing number of M. bovis cases we observed. Given the long latency of this disease, the unclear role of airborne transmission in M. bovis TB (13), and the fluid population dynamics of the San Diego region, however, the true population at risk and what might be behind the trends observed are difficult to describe. The relative contributions of reactivated latent M. bovis infection compared with recent infection could not be discerned in our study, but prudent prevention strategies would include a focus on eliminating consumption of unpasteurized dairy products in both adults and children in the United States and Mexico.
Our study confirms earlier preliminary findings (14) that M. bovis case-patients appear to be more than twice as likely to die before TB treatment completion compared with M. tuberculosis patients, despite being treated for the same mean number of days. The association of higher mortality rates during M. bovis treatment persisted after HIV, multisite disease, age, and ethnicity were accounted for. Causes of death related to noninfectious disease, such as malignancy and noninfectious gastrointestinal pathologies, were underrepresented in the M. bovis cases (0 vs. 25%), but, overall, the M. bovis and M. tuberculosis cases were not significantly different with regard to all causes of death.
In mouse models, evidence indicates that certain strains of M. bovis are more virulent than M. tuberculosis strains (24), but those findings are not generally supported in the literature on human M. bovis TB (7). Although our mortality analysis partially controlled for extent of disease, it did not include information on coexisting conditions, stage of HIV disease, diagnostic delays, and prior access to medical care. Therefore, M. bovis deaths might be accounted for by other factors, such as health disparities or treatment differences, which warrant further investigation.
Public health measures to control TB are currently focused on interrupting person-to-person transmission by promptly identifying and treating infectious patients and ensuring that they do not expose new contacts until treatment has rendered them noninfectious. Based on our data, these strategies, which have proven to be effective at reducing M. tuberculosis cases in San Diego and most regions of the United States, appear to be less effective in controlling M. bovis, suggesting that human-to-human transmission of M. bovis is less likely an important mode of transmission in this community. The consumption of contaminated dairy products has been proposed to be the primary source of human TB from M. bovis (25). This hypothese is supported by the findings of an investigation of M. bovis cases in New York that indicated the likely source of infection was unpasteurized cheese from Mexico (10). Additionally, San Diego pediatric M. bovis cases occur only after the age of weaning, when children are typically first exposed to dairy products (6), and M. bovis was also recently cultured from unpasteurized cheese seized at the San Diego–Mexico border (26,27).
Because of the widespread adoption of pasteurization of all commercially available dairy products in the United States, as well as the aggressive US state agricultural health programs designed to keep dairy cattle free from M. bovis disease, the threat of M. bovis in US dairy products was largely eliminated in the mid-20th century (8). The San Diego–Tijuana binational region, however, shares one of the busiest border crossings in the United States with Baja, Mexico (28), where M. bovis is prevalent in cattle and consumption of unpasteurized dairy products is a common cultural practice (29–32). Mexican dairy products, including the popular queso fresco (soft, unpasteurized cheese), may be brought into the United States for personal use and are sometimes distributed illegally (27). Given our finding that >90% of M. bovis cases in San Diego occurred in Hispanics, most of whom were born in Mexico, consumption of unpasteurized dairy products from Mexico is likely a major risk factor for M. bovis TB in San Diego. Collaboration with Mexico on prevention strategies, from education to regulation of the production of unpasteurized dairy products, and elimination of M. bovis from dairy cattle will be required in the long term to ensure that this mode of transmission is eliminated.
Limitations
A growing awareness of M. bovis as a cause of TB in San Diego since 1980 could have introduced a sampling bias into our trend estimates, but this possible bias is unlikely to have had a considerable effect in the years 1994 through 2005 as reported here. All suspected TB cases in San Diego County are reportable to the health department, and the county laboratory has consistently conducted testing to distinguish all M. tuberculosis complex isolates as either M. bovis or M. tuberculosis since 1994. The proportion of TB cases based only on clinical diagnosis and not species level culture has remained relatively level, at ≈20% of all reported TB cases. Increased efforts to obtain specimens for culture in pediatric TB cases in the years under study did not appear to change the proportion of culture-positive cases during the study period.
The cohort of TB case-patients who were not culture-positive and thus excluded from this analysis was significantly different from the study group. The <15-year age group (36% vs. 4%, respectively) and Hispanic ethnicity (57% vs. 45%) were both overrepresented in the excluded cases. Given that these are the groups most likely to have M. bovis TB, the total incidence of M. bovis, particularly in children, may be underestimated in our study.
Conclusions
San Diego, California, while unique in many respects because of its close proximity to Mexico, is possibly representative of other communities in the United States with large and growing Hispanic populations with ties to Mexico. The considerable and growing incidence of TB from M. bovis, especially in children, and the observed number of deaths during treatment in these cases is of serious concern. It raises the question of the importance of incorporating routine species-level identification into US TB surveillance as the national TB incidence shifts to persons born outside the United States. This surveillance will be greatly facilitated by the national genotyping project implemented by the US Centers for Disease Control and Prevention in 2004 (33), and its use will be particularly important for communities with strong ties to Mexico.
Acknowledgments
The authors thank Benjamin Sanchez for his assistance with dataset preparation and Richard Shaffer and Bohan Kolody for comments on early drafts of the manuscript.
Dr Rodwell received financial support from National Institutes of Health: HRSA and T32 #DA023356 as well as fellowship no. CF07-SD-302 from the California HIV/AIDS Research Program at the University of California and internal funds from the endowment of the Harold Simon Chair, Division of International Health and Cross-Cultural Medicine, University of California, San Diego.
Biography
Dr Rodwell is currently a clinical instructor and International Health Fellow at UCSD, specializing in international health and development, with an emphasis on TB monitoring, control, and treatment in resource-poor settings. His research interests include HIV/TB co-infection in San Diego and TB diagnosis and drug resistance in Mexico.
Footnotes
Suggested citation for this article: Rodwell TC, Moore M, Moser KS, Brodine SK, Strathdee SA. Mycobacterium bovis tuberculosis in binational communities. Emerg Infect Dis [serial on the Internet] 2008 Jun [date cited]. Available from http://www.cdc.gov/eid/content/14/6/909.htm
References
- 1.Cain KP, Haley CA, Armstrong LR, Garman KN, Wells CD, Iademarco MF, et al. Tuberculosis among foreign-born persons in the United States–achieving tuberculosis elimination. Am J Respir Crit Care Med. 2006;175:75–9. 10.1164/rccm.200608-1178OC [DOI] [PubMed] [Google Scholar]
- 2.San Diego Health and Human Services Agency. Comparative data: County of San Diego tuberculosis statistics, 1999−2006. 2007. [cited 2007 Sep 12]. Available from http://www2.sdcounty.ca.gov/hhsa/documents/Fctshttables2006FINAL.pdf
- 3.Voelker R. Pattern of US tuberculosis cases shifting. JAMA. 2007;297:685. 10.1001/jama.297.7.685 [DOI] [PubMed] [Google Scholar]
- 4.San Diego Association of Governments. San Diego–Baja California, land ports of entry: fact sheet. 2003. [cited 2007 Sep 12]. Available from http://www.sandag.cog.ca.us/uploads/publicationid/publicationid_1184_5148.pdf
- 5.San Diego Association of Governments. 2030 regional growth forecast. 2004. [cited 2007 Sep 2]. Available from http://www.sandag.org/uploads/publicationid/publicationid_1077_3212.pdf
- 6.LoBue PA, Betacourt W, Peter C, Moser KS. Epidemiology of Mycobacterium bovis disease in San Diego County, 1994–2000. Int J Tuberc Lung Dis. 2003;7:180–5. [PubMed] [Google Scholar]
- 7.Cosivi O, Grange JM, Daborn CJ, Raviglione MC, Fujikura T, Cousins D, et al. Zoonotic tuberculosis due to Mycobacterium bovis in developing countries. Emerg Infect Dis. 1998;4:59–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaneene JB, Miller R, Meyer RM. Abattoir surveillance: the US experience. Vet Microbiol. 2006;112:273–82. 10.1016/j.vetmic.2005.11.018 [DOI] [PubMed] [Google Scholar]
- 9.Dankner WM, Davis CE. Mycobacterium bovis as a significant cause of tuberculosis in children residing along the United States-Mexico border in the Baja California region. Pediatrics. 2000;105:E79. 10.1542/peds.105.6.e79 [DOI] [PubMed] [Google Scholar]
- 10.Center for Disease Control and Prevention. Human tuberculosis caused by Mycobacterium bovis—New York City, 2001–2004. MMWR Morb Mortal Wkly Rep. 2005;54:605–8. [PubMed] [Google Scholar]
- 11.Thoen C, Lobue P, de Kantor I. The importance of Mycobacterium bovis as a zoonosis. Vet Microbiol. 2006;112:339–45. 10.1016/j.vetmic.2005.11.047 [DOI] [PubMed] [Google Scholar]
- 12.Jalava K, Jones JA, Goodchild T, Clifton-Hadley R, Mitchell A, Story A, et al. No increase in human cases of Mycobacterium bovis disease despite resurgence of infections in cattle in the United Kingdom. Epidemiol Infect. 2007;135:40–5. 10.1017/S0950268806006509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LoBue PA, Betancourt W, Cowan L, Seli L, Peter C, Moser KS. Identification of a familial cluster of pulmonary Mycobacterium bovis disease. Int J Tuberc Lung Dis. 2004;8:1142–6. [PubMed] [Google Scholar]
- 14.LoBue PA, Moser KS. Treatment of Mycobacterium bovis infected tuberculosis patients: San Diego County, California, United States, 1994–2003. Int J Tuberc Lung Dis. 2005;9:333–8. [PubMed] [Google Scholar]
- 15.Ramarokoto H, Andrianasolo D, Rasolonavalona T, Ramaroson F, Razafitsiarovana I, Vincent V, et al. A case of pulmonary multiresistant tuberculosis (Mycobacterium bovis) in Madagascar. Arch Inst Pasteur Madagascar. 2003;69:37–40. [PubMed] [Google Scholar]
- 16.Hughes VM, Skuce R, Doig C, Stevenson K, Sharp JM, Watt B. Analysis of multidrug-resistant Mycobacterium bovis from three clinical samples from Scotland. Int J Tuberc Lung Dis. 2003;7:1191–8. [PubMed] [Google Scholar]
- 17.Robles Ruiz P, Esteban J, Guerrero MLF. Pulmonary tuberculosis due to multidrug-resistant Mycobacterium bovis in a healthy host. Clin Infect Dis. 2002;35:212–3. 10.1086/341313 [DOI] [PubMed] [Google Scholar]
- 18.Dankner WM. Mycobacterium bovis: a significant cause of childhood tuberculous disease in San Diego, California. In: Program and Abstracts of the Interscience Conference on Antimicrobial Agents and Chemotherapy 33rd Interscience Conference on Antimicrobial Agents and Chemotherapy; 1993 Oct 17–20; New Orleans, Louisiana, USA. 1993;33:367. [Google Scholar]
- 19.Grange JM. Mycobacterium bovis infection in human beings. Tuberculosis (Edinb). 2001;81:71–7. 10.1054/tube.2000.0263 [DOI] [PubMed] [Google Scholar]
- 20.Grange JM, Yates MD, de Kantor IN. Guidelines for speciation within the Mycobacterium tuberculosis complex: WHO/EMC/ZOO/96.4. Geneva, Switzerland: World Health Organization: Emerging and other Communicable Diseases, Surveillance and Control; 1996. [Google Scholar]
- 21.Streicher EM, Victor TC, van der Spuy G, Sola C, Rastogi N, van Helden PD, et al. Spoligotype signatures in the Mycobacterium tuberculosis complex. J Clin Microbiol. 2007;45:237–40. 10.1128/JCM.01429-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York: Wiley; 2000. [Google Scholar]
- 23.Hlavsa MC, Moonan P, Cowan L, Navin T, Kammerer S, Pratt R, et al. Human Mycobacterium bovis tuberculosis—United States, 1995–2005. In: 56th Annual EIS Conference; 2007. Apr 16–20; Atlanta, Georgia, USA. p. 118. [Google Scholar]
- 24.Dunn PL, North RJ. Virulence ranking of some Mycobacterium tuberculosis and Mycobacterium bovis strains according to their ability to multiply in the lungs, induce lung pathology, and cause mortality in mice. Infect Immun. 1995;63:3428–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thoen C, Steele J. Mycobacterium bovis infection in animals and humans. Ames: Iowa State University Press; 1995. [Google Scholar]
- 26.Harris NB, Payeur J, Bravo D, Osorio R, Stuber T, Farrell D, et al. Recovery of Mycobacterium bovis from soft fresh cheese originating in Mexico. [Epub 2006 Dec]. Appl Environ Microbiol. 2006;73:1025–8. 10.1128/AEM.01956-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kinde H, Mikolon A, Rodriguez-Lainz A, Adams C, Walker RL, Cernek-Hoskins S, et al. Recovery of Salmonella, Listeria monocytogenes, and Mycobacterium bovis from cheese entering the United States through a noncommercial land port of entry. J Food Prot. 2007;70:47–52. [DOI] [PubMed] [Google Scholar]
- 28.Lange JE, Lauer EM, Voas RB. A survey of the San Diego-Tijuana cross-border binging: methods and analysis. Eval Rev. 1999;23:378–98. [DOI] [PubMed] [Google Scholar]
- 29.Cobos-Marin L, Montes-Vargas J, Zumarraga M, Cataldi A, Romano MI, Estrada-Garcia I, et al. Spoligotype analysis of Mycobacterium bovis isolates from northern Mexico. Can J Microbiol. 2005;51:996–1000. 10.1139/w05-083 [DOI] [PubMed] [Google Scholar]
- 30.Milian-Suazo F, Banda-Ruiz V, Ramirez-Casillas C, Arriaga-Diaz C. Genotyping of Mycobacterium bovis by geographic location within Mexico. Prev Vet Med. 2002;55:255–64. 10.1016/S0167-5877(02)00015-6 [DOI] [PubMed] [Google Scholar]
- 31.Milian-Suazo F, Salman MD, Black WC IV, Triantis JM, Ramirez C, Payeur JB, et al. Molecular epidemiologic analysis of Mycobacterium bovis isolates from Mexico. Am J Vet Res. 2000;61:90–5. 10.2460/ajvr.2000.61.90 [DOI] [PubMed] [Google Scholar]
- 32.Milian-Suazo F, Salman MD, Ramirez C, Payeur JB, Rhyan JC, Santillan M. Identification of tuberculosis in cattle slaughtered in Mexico. Am J Vet Res. 2000;61:86–9. 10.2460/ajvr.2000.61.86 [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. New CDC program for rapid genotyping of Mycobacterium tuberculosis isolates. MMWR Morb Mortal Wkly Rep. 2005. Jan [cited 2008 Mar 6]. Available from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5402a6.htm