Abstract
Kaposi’s sarcoma (KS) is a multicentric tumor that most frequently involves the skin but can involve other tissues as well. Clinicians treating patients with KS or conducting clinical trials in this disease can benefit from imaging studies to document the extent of disease, to document changes with therapy, and to assess the extent of visceral and lymphatic involvement. A number of conventional techniques can be of use in meeting these needs, such as conventional light photography to assess skin or mucosal lesions, computerized tomography of the chest to assess pulmonary disease, and magnetic resonance imaging. In addition, a number of techniques are being developed with the goals of providing improved differentiation of KS from other diseases or providing information about the degree of angiogenesis in the lesions and other physiologic factors. We present here an overview of both established and experimental modalities of imaging in KS.
1. Introduction
Kaposi’s sarcoma (KS) differs from most other tumors in a number of important ways, and the needs and tools available for imaging differ as well. The goals of radiographic imaging for any tumor vary depending on whether imaging is performed to initially stage a malignant disease process or follow response to therapy. In the case of KS, precise staging and documenting every tumor site is often less important than in other malignancies because the disease is driven by a virus and is multifocal, and because the benefits of staging need to be balanced against the patient risks involved. Moreover, in KS perhaps more than other tumors, consideration is given to techniques that may provide a quantification of the disease burden on the skin and an assessment of functional angiogenic properties of the lesions.
The majority of KS patients present with skin disease alone. However certain KS subtypes, particularly endemic KS and AIDS-related KS, are associated with extra-cutaneous spread and visceral involvement. Detailed knowledge of the expected sites of involvement is imperative to accurately stage the patient. Patients presenting with skin disease alone may often have multiple irregularly shaped lesions with varying degrees of nodularity, making accurate quantitation of the extent of tumor involvement difficult. Thus, as will be described below, several techniques have been explored to enable clinicians to better measure the extent of disease. In this chapter, imaging techniques commonly used in patients with KS will be described. In addition, several novel imaging techniques under development will be discussed.
2. Staging in KS
2.1
There are a variety of different staging systems in use for KS, and these present a significant challenge in assessing new therapies and comparing them to the published literature. The system most frequently utilized today is the AIDS Clinical Trial Group (ACTG) staging system for AIDS-related KS (AIDS-KS) that was originally defined in 1988 (1). It was devised prior to the era of highly active anti-retroviral therapy (HAART) and classified patients into good- or poor-risk groups based on tumor extent (T), immune system status (I) as measured by CD4 T-lymphocyte count, and evidence of HIV-1–associated systemic illness (S).(1, 2) However reassessment of this staging system in the HAART era has revealed that the immune system is no longer a significant prognostic factor; thus, a refinement of the original ACTG staging system was developed that does not take the CD4 count into consideration.(3) A slightly different staging system has been proposed for transplant-related KS; there are three stages consisting of local skin disease, widespread skin disease, and disseminated disease involving viscera, lymph nodes and/or skin.(4) This staging system requires upper and lower gastrointestinal endoscopy and computerized tomography of the chest and abdomen as appropriate baseline imaging.
3. Imaging of the Skin and Mouth in KS
In general, when physicians consider imaging techniques, these techniques are thought of as a means to obtain information about parts of the body that are not easily visible on physical examination. However, in the case of KS, methodology to image skin lesions can be of considerable utility in creating a record of the extent of disease, quantifying the extent of disease, and obtaining physiologic information about such factors as blood flow or the state of oxygenation. To these ends, specialized photography, ultrasound, and thermal imaging are some of the techniques available.
3.1. Visible Light Photography
Clinicians treating patients with KS and conducting clinical trials of KS have for some time employed conventional light photography to create an objective record of the extent of disease at a specific timepoint that can facilitate later comparisons and create a record of the effects of therapeutic approaches.(5) Recent innovations in photographic techniques, such as digital imaging technology, have improved the ability to record images of skin and mucosal tissue in the mouth and can enhance the information that is derived from naked-eye inspection. In fact, visible light photography is probably the single most useful technique to image cutaneous and oral KS.
The majority of patients with KS present with skin disease alone and patient assessment begins with a thorough clinical examination that includes visual inspection of the skin and mucosa. The number, location, size, color and character of each lesion is described unless extensive skin disease (greater than 50 lesions) is present, in which case the lesions in a representative area are documented. Serial photography can be useful for monitoring disease progress or response to therapy. Whole body photographs should be taken, as well as photographs of sectors of the body and lesions of interest, ideally using standardized technique. Staging systems such as the ACTG system often call for several “marker” lesions to be followed during therapy, and this can be facilitated by photographing the lesions in a standardized manner with a small ruler placed near the lesions (Figure 1). Subsequent photography using the same technique can create an objective record of tumor responses. A drawback of this technique, however, is that it provides little information about tumor nodularity, which more frequently responds to therapy than does lesion size. Also, KS lesions that have completely responded to therapy sometimes remain as hyperpigmented areas, presumably from hemosiderin deposits. A skin biopsy can sometimes be useful in differentiating such hyperpigmented areas from residual KS.
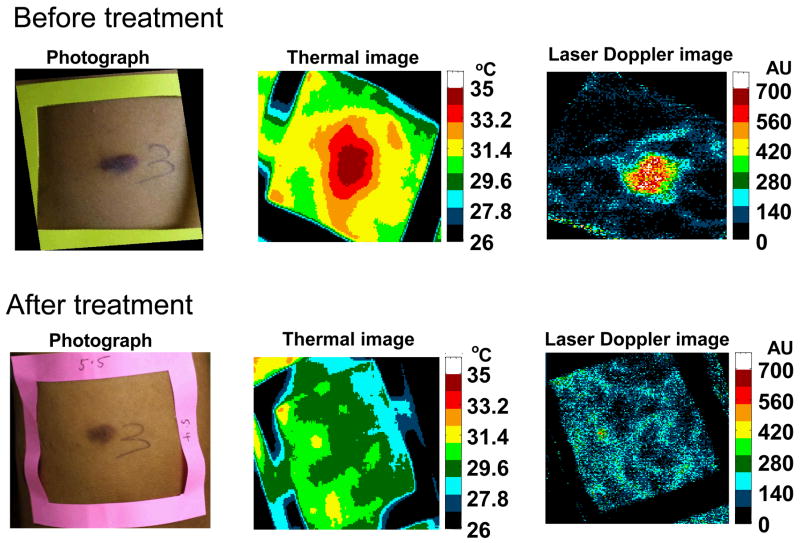
Figure 1.
Typical example of light photography, thermal imaging, and laser Doppler imaging of a KS lesion prior to therapy and after therapy. As can be seen, the thermal and laser Doppler images normalized after treatment, while the lesion was still evident by light photography. Reproduced with permission from Hassan et al., Technology in Cancer Research and Treatment, 3 (5), 451–7, 2004.
3.2. Ultrasound
The use of ultrasound for imaging skin was reported as early as 1979 when Alexander and Miller reported the ability of ultrasound to determine skin thickness.(6) Significant improvements in techniques have since been developed. Images of the skin can be displayed in one-dimensional A mode (capable of measuring skin thickness), two-dimensional B mode (produces a vertical cross-sectional image), or C mode (produces horizontal images of the skin).(7) In comparison to ultrasound frequencies used to image abdominal organs, much higher frequencies are required to generate images of sufficient resolution to identify the various layers of the skin. In general, frequencies in the 20–25 mHz range are used, which provide axial resolution of 50–80 μm and a lateral resolution of 200–300 μm. Ultrasongraphy has been reported to be useful to delineate deep margins of lesions and assess tumor size in response to therapy (8, 9). However, while the technique has potential advantages, it is not widely used by most researchers caring for patients with KS or conducting clinical trials in this disease.
3.3. Infrared Thermal Imaging
KS is a highly vascular tumor characterized by a hyperproliferation of spindle cells that are thought to be derived from vascular or other endothelial cells. The spindle cells form vascular slits that are filled with blood. Given the vascular nature of KS, it is an excellent model to investigate experimental techniques for assessing tumor vascularity and vascular changes in response to treatment. One approach that has recently been investigated is thermal imaging. Infrared thermal imaging has been used to study biological thermoregulatory abnormalities that directly or indirectly influence skin temperature.(10) The thermal signatures consist of both the superficial vascularity and deep tissue metabolic activity.(11) Thermal imaging uses a digital infrared camera to map the temperature on a given body surface area. An image can be created in which different shades of grey or different colors depict different temperatures. Highly vascular lesions are usually warmer than surrounding tissue.
A clinical study assessing the role of infrared thermal imaging demonstrated that KS lesions can be differentiated from surrounding uninvolved tissue by a temperature gradient; KS lesions demonstrating a median of 1.1°C higher temperatures than the surrounding skin (Figure 1).(12) In addition, this temperature gradient resolved in response to effective KS therapy, in many cases before the lesions resolved by visual inspection or palpation. The utility of this technique in monitoring trials of KS and other tumors in which angiogenesis is an important feature is currently under study. As described elsewhere in this chapter, infrared thermal imaging can complement other more experimental techniques such as laser Doppler imaging (LDI) and multi-spectral imaging to assess angiogenic features of KS lesions.
4. Imaging of Visceral and Lymphatic Disease in KS
4.1. Radiography
Conventional radiology can be used to visualize KS lesions, especially those in the lungs, and it continues to play a role in the assessment of KS. However, computerized tomography (CT) and magnetic resonance imaging (MRI) are generally more useful in the assessment of visceral and lymphatic KS.
4.1.1. Conventional radiographs of the chest
While pulmonary involvement has been reported in all KS subtypes, it occurs more commonly in endemic and AIDS-related KS and is associated with a poor prognosis. (13–18) While antiretroviral therapy has improved KS outcomes of all forms of KS, pulmonary KS should still be regarded as a serious disease manifestation; one study documented a median survival of just 1.6 years for patients with AIDS-related pulmonary disease even in the era of HAART.(19) Several chest radiograph findings of pulmonary KS have been described, including reticulonodular infiltrates, homogeneous infiltrates, pleural effusions and lymphadenopathy (Figure 2).(17, 20) KS has a tendency to proliferate in the interstitium, and the peribronchial and perivascular lymphatics resulting in bilateral reticulonodular infiltrates with a predilection for the peri-hilar area and lower lung fields. Autopsy confirmed KS in 14 of 16 patients presenting with pleural effusions.
Figure 2.
Chest radiograph demonstrating typical bilateral reticulonodular infiltrates of KS confirmed by biopsy
The presence of co-morbidities such as infection, particularly in patients with AIDS-related KS, may complicate the interpretation of imaging findings. While radiographic findings have a high positive predictive value for the presence of pulmonary KS, they are not specific and their presence does not reduce the likelihood of co-existent infection or other disease processes. In practice, pulmonary radiographs are perhaps most useful in excluding pulmonary KS involvement or providing a tool to follow the disease progress.
4.1.2. Skeletal survey
KS involvement of bone and skeletal muscle is infrequently reported. A recent review identified only 66 published cases, the majority occurring in endemic and AIDS-related subtypes.(21) Several reports suggest that patients may present with asymptomatic osseous lesions, without skin or visceral disease. (22) However, in general most cases are associated with locally aggressive, chronic disease that penetrates underlying bone. The relative degree of pain does not appear to correlate with radiological appearances, as often extensive osteolysis may result in minimal symptoms. Bones involved may include skull, hard palate, mandible, vertebra, sternum, rib cage, long bones, and the small bones of hands and feet.(21, 23, 24) The majority of lesions are osteolytic in nature, with or without an associated periosteal reaction, but sclerotic appearances have also been reported (Figure 3).(25)
Figure 3.
MRI of the ankle demonstrating abnormal enhancement of calcaneus, talus and navicular bones, with an enhancing fluid collection anterior to the ankle mortis due to KS.
If patients with known KS have bony lesions, the physician must then assess whether the lesions are in fact due to the KS or to other causes. The differential diagnosis of osseous lesions is vast, but may be broadly classified into infectious and neoplastic causes. Bartonella infection causing bacillary angiomatosis, Mycobacterium tuberculosis, M. avium-intracellulare, Nocardia asteroides, and Neisseria gonorrhoea are a selection of the most frequently cultured organisms. In patients with HIV-associated KS, physicians must be particularly alert for the possibility of Mycobacterium infections. With regard to neoplastic causes, primary bone lymphoma, angiosarcoma, hemangioendothelioma, and spindle cell pseudotumors may appear similar to KS on radiographs.
4.1.3. Computerized tomography (CT)
After chest plain radiograph, CT of the thorax is the imaging modality of choice for assessment of pulmonary KS. The superiority of CT to conventional radiographs of the chest has been demonstrated by a number of studies. (17, 26, 27) Significant variation in the type and frequency of radiographic abnormalities has been reported, many of which may be non-specific. However, typical appearances includes nodules (76%), bronchovascular infiltrates (66%), tumoral masses (53%), pleural effusions (55%), and lymphadenopathy (43%) (Figure 4).(20, 28) Although none of these findings are specific, the combination of poorly defined nodules, fissural nodularity, and a bronchovascular distribution of perihilar opacities on CT is highly suggestive of pulmonary KS.(29) Lytic lesions of the sternum and thoracic spine and soft tissue masses are also well-recognized findings.(30) The role of CT is to document findings that are characteristic of KS and where appropriate, to facilitate definitive diagnostic procedures such as fiberoptic bronchoscopy, thoracoscopy or even open lung biopsy.
Figure 4.
Chest CT with characteristic KS peri-hilar bronchovascular infiltrates.
Classic KS generally has minimal if any abdominal involvement identified by CT.(31) In patients with AIDS-KS, KS involvement of the liver can occur and can be detected using contrast imaging. In spite of this, extensive contrast imaging studies are not routinely performed unless there is a particular suspicion of hepatic neoplasm. (32) Generally KS lesions tend to be multifocal, originating in the capsular, hilar and portal areas. Non-contrast CT scans may identify multiple hypoattenuated nodules. However due to the vascular nature of KS, delayed imaging (4–7 minutes) post contrast injection results in lesion enhancement or increased attenuation compared to surrounding parenchyma. (33) Splenomegaly or discrete splenic lesions may be seen occasionally, as can involvement of the peri-intestinal tissue (Figure 5).(31) Hyperattenuating lymphadenopathy may be seen with CT in approximately 80% of cases of disseminated KS (Figure 6).(34)
Figure 5.
CT of the abdomen showing an inflammatory matted mass from extensive gastrointestinal involvement with KS.
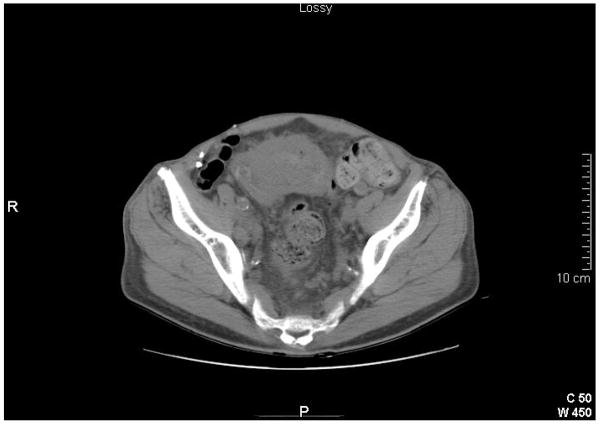
Figure 6.
CT of the pelvis showing femoral lymphadenopathy with an enhanced pattern from KS involvement.
More recently the CT imaging findings in two patients with transplant-related KS have been described, both cases involved KS in the transplanted organ.(35, 36) These cases highlight the importance of including KS in the differential diagnosis of enhancing lesions of the kidney or urinary tract, especially in settings where KS may be epidemiologically more likely.
4.2. Magnetic Resonance Imaging (MRI)
Transition from plain radiography to CT demonstrates a significant improvement in the quality of available imaging but also exposes patients to increased radiation. The development of MRI has provided a technique to ascertain soft-tissue lesions without radiation exposure. MRI provides excellent spatial resolution, however with better contrast resolution than computed tomography. In spite of the significant strides established with MRI, however, it has not yet become a standard imaging process for KS.
A prospective study of thoracic MRI identified a pattern of MRI signal abnormalities that are suggestive of pulmonary KS, namely irregular increased signal intensity in T1 weighted images with markedly reduced signal intensity on T2-weighted images and significant enhancement of KS lesion after gadolinium administration.(37) MRI has also been useful for detecting of both cardiac and bone involvement, with higher sensitivities than other imaging techniques. (38, 39)
4.3. 18F-Fluorodeoxyglucose (FDG)-Positron Emission Tomography (PET)
PET is an imaging technique most frequently that utilizes the radionuclide 18F-fluorodeoxyglucose (FDG), which is a glucose analog. Like glucose, FDG is transported into cells via the glucose channels and its uptake is increased in metabolically active malignant lesions.(40) FDG is known to accumulate avidly in certain malignancies and its role of PET in KS is currently being defined.(41) Published data consist of three case reports with conflicting findings. Two reports documented low FDG avidity with pulmonary and lymph node KS and suggested that PET may have a role differentiating HIV associated KS from other neoplastic processes.(42, 43) By contrast, a third report documented markedly increased FDG uptake in a patient with transplant-associated pulmonary KS.(44) Prospective and more extensive studies of this modality will be required in order to sort out the patterns found with KS and to determine what role if any it has in general clinical practice.
4.4. 99mTc-Tetrofosmin Scintigraphy
99mTc-Tetrofosmin is a cationic lipophilic radiotracer with tumor-seeking properties that is rapidly cleared from the lungs and liver, permitting early high quality images.(45) It has been employed in lung cancer patients in detecting primary and metastatic disease, in addition to determining response to therapy. (46–48) Spanu et al, investigated the benefit of 99mTc-Tetrofosmin in detecting both cutaneous and extra-cutaneous tumors. This study included planer, single photon emission computerized tomography (SPECT) and neck pinhole(P)-SPECT in selected patients with KS (classic KS, AIDS-KS, and transplantation-associated KS). With regard to the KS patients studied, 99mTc-Tetrofosmin uptake was observed in 88% of patients with clinically evident lesions. Scintigraphy, particularly SPECT, gave additional information regarding depth of invasion and identified subclinical lesions. It was less sensitive in the detection of small, isolated and scattered lesions. A small patient number limits interpretation of the data somewhat, but the sensitivity and specificity of SPECT 99mTc-Tetrofosmin was 82.6% and 100% respectively. Planer 99mTc-Tetrofosmin imaging showed a sensitivity of 69.6% and a specificity of 100%.
There is some evidence that the utility of 99mTc-Tetrofosmin scintigraphy is increased when it is combined with other imaging modalities. For example, in combination with ultrasound, it seems to reliably indentify KS lymph node involvement and differentiate such nodes from reactive hyperplastic nodes. In combination with 67Ga-citrate scintigraphy it may differentiate between KS and lymphomatous involvement.(49) Other radioisotopes have also been reported to be of benefit in detecting KS lesions such as 99mTc-pertechnetate, 201TI-chloride, 111In-DTPA-labeled pegylated liposomes, 99mTc-MIBI, 111In-DTPA octreotide and 18F fluorodeoxyglucose.(42, 50–54)
5. Novel Techniques
In the past several years, a number of new techniques have been explored for possible utility in KS. Some of these provide physiologic information about angiogenic features of KS lesions in addition to anatomical data.
5.1. Laser Doppler Imaging (LDI)
LDI utilizes a low-power laser beam to measure the doppler shift due to blood flow patterns in skin up to a depth of 1mm.(55) When monochromatic light from the laser interacts with a moving object, such as a red blood cell, a change in the frequency of the scattered light is induced in comparison to the light backscattered from background non-moving tissue. A photodetector is used to measure the degree of tissue perfusion which is expressed in arbitrary units termed ‘flux” values.
Angiogenesis results in increased blood flow that can be assessed by LDI.(56, 57) Flux values identified by LDI are generally higher in KS lesions than normal surrounding skin (Figure 1).(58) One study that assessed a series of cutaneous KS lesions using both LDI and infrared thermal imaging showed a strong correlation between these two techniques, suggesting that either can be used to detect functional vascular abnormalities in KS lesions.(12) However a combination of the two imaging techniques may be superior to either one alone, as they assess different physical properties and also gather information from different depths, with infrared thermal imaging being influenced by deeper vessels than LDI.
5.1.1. Multi-Spectral Imaging
Multispectral imaging is currently being explored as an experimental technique to gather information about cutaneous KS lesions. Spectral imaging collects reflectance images at several different wavelengths. In the case of KS, near-infrared wavelengths (700–1000 nm) are utilized because the absorptions of oxy- and/or deoxy-hemoglobin are relatively high compared to water and lipids at those wavelengths. Based on relative absorbencies, one can estimate the oxygenation of blood, estimate the total blood volume, and provide a spatial map of blood volume and oxygenated-hemoglobin in tissue. However interpretation of the data is complicated by certain confounders such as the effect of light scattering, the amount of melanin in the skin, and hemoglobin breakdown products. In a research setting this imaging system has been utilized to differentiate between malignant and benign skin lesions.(59) Studies of its use in KS showed that it could provide information on the status of the lesions as well as their response to therapy.(60, 61) However, the optimal algorithms to correct for the confounding factors noted above in assessing blood volume and status of oxygenation have not yet been established.
5.1.2. 2′-deoxy-2′flouro-5iodo-1-beta-D-arabinofuransyluracil (FIAU)
Kaposi’s sarcoma-associated herpesvirus (KSHV), the causative agent for KS, encodes kinases that phosphorylate certain nucleoside analogs such as 2′-deoxy-2′flouro-5iodo-1-beta-D-arabinofuransyluracil (FIAU). This knowledge has been harnessed to investigate the possibility of using the viral enzyme to specifically concentrate 125I -FIAU or 131I-FIAU in KSHV associated tumor cells harboring virus to both image and deliver therapeutic radiation.(62, 63) Using a KSHV-infected primary effusion lymphoma (PEL) tumor cell line (BCBL1), cell uptake assays with 14C-FIAU and ex vivo bio-distribution studies with 125I -FIAU showed that uptake and retention of 125I -FIAU is highly specific for KSHV-infected cells when the virus is in a lytic phase. Bortezomib, a potent stimulator of KSHV lytic genes including a viral-encoded kinase, was found to induce selective concentration of radiolabeled FIAU. Thus, it may provide a simple means to localize KSHV-associated malignancies and may be found to have utility in the clinical setting after additional research is conducted.
5.1.3. Imaging probes targeting matrix metalloproteinases
Matrix metalloproteinases (MMP) are a group of enzymes responsible for extracellular membrane (ECM) and basement membrane (BM) proteolysis, and thus are the most relevant group of proteinases for tumor invasion.(64) The accessibility of MMPs in the ECM or on the cell wall and the relative over-production in cancer compared to the normal surrounding tissues, make MMPs an attractive target for in vivo imaging. MMPs are regulated by a number of endogenous inhibitors that prevent matrix degradation; the most specific of these are tissue inhibitors of metalloproteinases (TIMPs). To date, the only imaging probe to reach clinical investigation is 111In-DTPA-N-TIMP-2. Unfortunately the tracer distributed predominantly to the kidneys and did not localize in other tissues.(65) Suggested explanations for lack of efficacy included possible down-regulation of MMP activity in response to prior therapy or perhaps interference of anti-HIV protease inhibitors.
6. Summary
As described in this chapter, a variety of imaging techniques are useful in the clinical assessment of KS or in the conduct of clinical trials involving this tumor, and several additional imaging techniques are now under development. Because KS is a multifocal disease and lesions are often irregular or confluent, a major challenge in the conduct of clinical trials is the documentation of the extent of disease and changes with therapy. Visible light photography, especially if done with a standard methodology, can be extremely valuable for this purpose. Other available techniques that can have utility in the assessment of visceral disease include radiography, computerized tomography, and MRI. A number of other techniques are now under study that may have better specificity for KS lesions, provide assessments of tumor depth, or may provide information about the physiologic characteristics of the lesions such as temperature or blood flow. It is possible that as these are further developed and standardized, they will become part of the armamentarium of the practicing physician facing patients with this disease.
Acknowledgments
This work was supported by the Intramural Research Program of the NIH, NCI and NICHD.
References
- 1.Krown SE, Metroka C, Wernz JC. Kaposi’s sarcoma in the acquired immunodeficiency syndrome: a proposal for uniform evaluation, response, and staging criteria. J Clin Oncol. 1989;7:1201–7. doi: 10.1200/JCO.1989.7.9.1201. [DOI] [PubMed] [Google Scholar]
- 2.Krown SE, Testa MA, Huang J. AIDS-related Kaposi’s sarcoma: prospective validation of the AIDS Clinical Trials Group staging classification. AIDS Clinical Trials Group Oncology Committee. J Clin Oncol. 1997;15(9):3085–92. doi: 10.1200/JCO.1997.15.9.3085. [DOI] [PubMed] [Google Scholar]
- 3.Nasti G, Talamini R, Antinori A, et al. AIDS-related Kaposi’s Sarcoma: evaluation of potential new prognostic factors and assessment of the AIDS Clinical Trial Group Staging System in the Haart Era--the Italian Cooperative Group on AIDS and Tumors and the Italian Cohort of Patients Naive From Antiretrovirals. J Clin Oncol. 2003;21(15):2876–82. doi: 10.1200/JCO.2003.10.162. [DOI] [PubMed] [Google Scholar]
- 4.Al-Khader AA, Suleiman M, Al-Hasani M, Haleem A. Posttransplant Kaposi sarcoma: staging as a guide to therapy and prognosis. Nephron. 1988;48(2):165. doi: 10.1159/000184900. [DOI] [PubMed] [Google Scholar]
- 5.Pluda JM, Shay LE, Foli A, et al. Administration of pentosan polysulfate to patients with human immunodeficiency virus-associated Kaposi’s sarcoma. J Natl Cancer Inst. 1993;85(19):1585–92. doi: 10.1093/jnci/85.19.1585. [DOI] [PubMed] [Google Scholar]
- 6.Alexander H, Miller DL. Determining skin thickness with pulsed ultra sound. J Invest Dermatol. 1979;72(1):17–9. doi: 10.1111/1523-1747.ep12530104. [DOI] [PubMed] [Google Scholar]
- 7.Serup J. Ten years experience with high frequency ultrasound examination of the skin: Development and refinement of technique and equipment. In: Altmeyer PE-GS, Hoffman K, editors. Ultrasound in Dermatology. Berlin: Springer-Verlag; 1992. pp. 41–54. [Google Scholar]
- 8.Fornage BD, McGavran MH, Duvic M, Waldron CA. Imaging of the skin with 20-MHz US. Radiology. 1993;189(1):69–76. doi: 10.1148/radiology.189.1.8372222. [DOI] [PubMed] [Google Scholar]
- 9.Wortsman XC, Holm EA, Wulf HC, Jemec GB. Real-time spatial compound ultrasound imaging of skin. Skin Res Technol. 2004;10(1):23–31. doi: 10.1111/j.1600-0846.2004.00048.x. [DOI] [PubMed] [Google Scholar]
- 10.Maxwell-Cade C. Principles and practice of clinical thermography. Radiography. 1968;34(398):23–34. [PubMed] [Google Scholar]
- 11.Draper JW, Boag JW. Skin temperature distributions over veins and tumours. Phys Med Biol. 1971;16(4):645–54. doi: 10.1088/0031-9155/16/4/008. [DOI] [PubMed] [Google Scholar]
- 12.Hassan M, Little RF, Vogel A, et al. Quantitative assessment of tumor vasculature and response to therapy in kaposi’s sarcoma using functional noninvasive imaging. Technol Cancer Res Treat. 2004;3(5):451–7. doi: 10.1177/153303460400300506. [DOI] [PubMed] [Google Scholar]
- 13.Coll J, Pedro-Botet J, Pallas JO, Gimenez-Arnau AM, Barranco C. Classic Kaposi’s sarcoma with pulmonary involvement in an HIV-negative woman. Clin Exp Dermatol. 1995;20(5):410–2. doi: 10.1111/j.1365-2230.1995.tb01359.x. [DOI] [PubMed] [Google Scholar]
- 14.Lim TW, Lee MH, Park JG, Cho BK. Classic Kaposi sarcoma presenting as rapidly growing nodules. Cutis. 2001;68(1):50–2. [PubMed] [Google Scholar]
- 15.Buchbinder A, Friedman-Kien AE. Clinical aspects of epidemic Kaposi’s sarcoma. Cancer Surv. 1991;10:39–52. [PubMed] [Google Scholar]
- 16.Hill CA, Harle TS, Mansell PW. The prodrome, Kaposi sarcoma, and infections associated with acquired immunodeficiency syndrome: radiologic findings in 39 patients. Radiology. 1983;149(2):393–9. doi: 10.1148/radiology.149.2.6604929. [DOI] [PubMed] [Google Scholar]
- 17.Davis SD, Henschke CI, Chamides BK, Westcott JL. Intrathoracic Kaposi sarcoma in AIDS patients: radiographic-pathologic correlation. Radiology. 1987;163(2):495–500. doi: 10.1148/radiology.163.2.3562832. [DOI] [PubMed] [Google Scholar]
- 18.Penn I. Neoplastic complications of transplantation. Semin Respir Infect. 1993;8(3):233–9. [PubMed] [Google Scholar]
- 19.Palmieri C, Dhillon T, Thirlwell C, et al. Pulmonary Kaposi sarcoma in the era of highly active antiretroviral therapy. HIV Med. 2006;7(5):291–3. doi: 10.1111/j.1468-1293.2006.00378.x. [DOI] [PubMed] [Google Scholar]
- 20.Restrepo CS, Martinez S, Lemos JA, et al. Imaging manifestations of Kaposi sarcoma. Radiographics. 2006;26(4):1169–85. doi: 10.1148/rg.264055129. [DOI] [PubMed] [Google Scholar]
- 21.Caponetti G, Dezube BJ, Restrepo CS, Pantanowitz L. Kaposi sarcoma of the musculoskeletal system: a review of 66 patients. Cancer. 2007;109(6):1040–52. doi: 10.1002/cncr.22500. [DOI] [PubMed] [Google Scholar]
- 22.Noel KE, Mardirossian G, Schneider L. Primary intraosseous Kaposi’s sarcoma presenting as an asymptomatic periapical radiolucency: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(5):e65–70. doi: 10.1016/j.tripleo.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen C, Lander P, Begin LR, Jarzem P, Grad R. AIDS-related Kaposi sarcoma involving the tarsal bones. Skeletal Radiol. 1996;25(1):100–2. doi: 10.1007/s002560050044. [DOI] [PubMed] [Google Scholar]
- 24.Pitson GA, Aw TJ, Rodger A. Classical Kaposi’s sarcoma involving bone. Australas Radiol. 1999;43(3):391–3. doi: 10.1046/j.1440-1673.1999.433677.x. [DOI] [PubMed] [Google Scholar]
- 25.Shetty RR. Unusual bone manifestation of Kaposi’s sarcoma. Int J STD AIDS. 2004;15(8):566–7. doi: 10.1258/0956462041558276. [DOI] [PubMed] [Google Scholar]
- 26.Naidich DP, Garay SM, Leitman BS, McCauley DI. Radiographic manifestations of pulmonary disease in the acquired immunodeficiency syndrome (AIDS) Semin Roentgenol. 1987;22(1):14–30. doi: 10.1016/0037-198x(87)90019-8. [DOI] [PubMed] [Google Scholar]
- 27.Wolff SD, Kuhlman JE, Fishman EK. Thoracic Kaposi sarcoma in AIDS: CT findings. J Comput Assist Tomogr. 1993;17(1):60–2. doi: 10.1097/00004728-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Khalil AM, Carette MF, Cadranel JL, Mayaud CM, Bigot JM. Intrathoracic Kaposi’s sarcoma. CT findings Chest. 1995;108(6):1622–6. doi: 10.1378/chest.108.6.1622. [DOI] [PubMed] [Google Scholar]
- 29.Kuhlman JE. Imaging pulmonary disease in AIDS: state of the art. Eur Radiol. 1999;9(3):395–408. doi: 10.1007/s003300050682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Traill ZC, Miller RF, Shaw PJ. CT appearances of intrathoracic Kaposi’s sarcoma in patients with AIDS. Br J Radiol. 1996;69(828):1104–7. doi: 10.1259/0007-1285-69-828-1104. [DOI] [PubMed] [Google Scholar]
- 31.Moon KL, Jr, Federle MP, Abrams DI, Volberding P, Lewis BJ. Kaposi sarcoma and lymphadenopathy syndrome: limitations of abdominal CT in acquired immunodeficiency syndrome. Radiology. 1984;150(2):479–83. doi: 10.1148/radiology.150.2.6691105. [DOI] [PubMed] [Google Scholar]
- 32.Niedt GW, Schinella RA. Acquired immunodeficiency syndrome. Clinicopathologic study of 56 autopsies. Arch Pathol Lab Med. 1985;109(8):727–34. [PubMed] [Google Scholar]
- 33.Luburich P, Bru C, Ayuso MC, Azon A, Condom E. Hepatic Kaposi sarcoma in AIDS: US and CT findings. Radiology. 1990;175(1):172–4. doi: 10.1148/radiology.175.1.2179988. [DOI] [PubMed] [Google Scholar]
- 34.Herts BR, Megibow AJ, Birnbaum BA, Kanzer GK, Noz ME. High-attenuation lymphadenopathy in AIDS patients: significance of findings at CT. Radiology. 1992;185(3):777–81. doi: 10.1148/radiology.185.3.1438762. [DOI] [PubMed] [Google Scholar]
- 35.Rha SE, Byun JY, Kim HH, Baek JH, Hwang TK, Kang SJ. Kaposi’s sarcoma involving a transplanted kidney, ureter and urinary bladder: ultrasound and CT findings. Br J Radiol. 2000;73(875):1221–3. doi: 10.1259/bjr.73.875.11144804. [DOI] [PubMed] [Google Scholar]
- 36.Diaz-Candamio MJ, Pombo F, Lorenzo MJ, Alonso A. Kaposi’s sarcoma involving a transplanted kidney: CT findings. AJR Am J Roentgenol. 1998;171(4):1073–4. doi: 10.2214/ajr.171.4.9762999. [DOI] [PubMed] [Google Scholar]
- 37.Khalil AM, Carette MF, Cadranel JL, Mayaud CM, Akoun GM, Bigot JM. Magnetic resonance imaging findings in pulmonary Kaposi’s sarcoma: a series of 10 cases. Eur Respir J. 1994;7(7):1285–9. doi: 10.1183/09031936.94.07071285. [DOI] [PubMed] [Google Scholar]
- 38.Burgert SJ, Strickman NE, Carrol CL, Falcone M. Cardiac Kaposi’s sarcoma following heart transplantation. Catheter Cardiovasc Interv. 2000;49(2):208–12. doi: 10.1002/(sici)1522-726x(200002)49:2<208::aid-ccd21>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen S, Giurca C, Melliez H, et al. Kaposi’s sarcoma in HIV-infected patients: when and how should we evaluate bone involvement? AIDS. 2007;21(16):2251–2. doi: 10.1097/QAD.0b013e3282f006d7. [DOI] [PubMed] [Google Scholar]
- 40.Di Chiro G. Positron emission tomography using [18F] fluorodeoxyglucose in brain tumors. A powerful diagnostic and prognostic tool. Invest Radiol. 1987;22(5):360–71. doi: 10.1097/00004424-198705000-00002. [DOI] [PubMed] [Google Scholar]
- 41.Cheson BD, Pfistner B, Juweid ME, et al. Revised response criteria for malignant lymphoma. J Clin Oncol. 2007;25(5):579–86. doi: 10.1200/JCO.2006.09.2403. [DOI] [PubMed] [Google Scholar]
- 42.O’Doherty MJ, Barrington SF, Campbell M, Lowe J, Bradbeer CS. PET scanning and the human immunodeficiency virus-positive patient. J Nucl Med. 1997;38(10):1575–83. [PubMed] [Google Scholar]
- 43.Kulasegaram R, Saunders K, Bradbeer CS, O’Doherty M. Is there a role for positron emission tomography scanning in HIV-positive patients with Kaposi’s sarcoma and lymphadenopathy: two case reports. Int J STD AIDS. 1997;8(11):709–12. doi: 10.1258/0956462971918940. [DOI] [PubMed] [Google Scholar]
- 44.Martinez S, McAdams HP, Youens KE. Kaposi sarcoma after bilateral lung transplantation. J Thorac Imaging. 2008;23(1):50–3. doi: 10.1097/RTI.0b013e3181585bc4. [DOI] [PubMed] [Google Scholar]
- 45.Higley B, Smith FW, Smith T, et al. Technetium-99m-1, 2-bis[bis(2-ethoxyethyl) phosphino]ethane: human biodistribution, dosimetry and safety of a new myocardial perfusion imaging agent. J Nucl Med. 1993;34(1):30–8. [PubMed] [Google Scholar]
- 46.Schillaci O, Monteleone F, D’Andrea N, et al. Technetium-99m tetrofosmin single photon emission computed tomography in the evaluation of suspected lung cancer. Cancer Biother Radiopharm. 1999;14(2):129–34. doi: 10.1089/cbr.1999.14.129. [DOI] [PubMed] [Google Scholar]
- 47.Schillaci O, Spanu A, Scopinaro F, et al. Mediastinal lymph node involvement in non-small cell lung cancer: evaluation with 99mTc-tetrofosmin SPECT and comparison with CT. J Nucl Med. 2003;44(8):1219–24. [PubMed] [Google Scholar]
- 48.Spanu A, Ginesu F, Pirina P, et al. The usefulness of 99mTc-tetrofosmin SPECT in the detection of intrathoracic malignant lesions. Int J Oncol. 2003;22(3):639–49. [PubMed] [Google Scholar]
- 49.Yang CC, Sun SS, Lin CC, Kao CH, Lee CC. Comparison of technetium-99m tetrofosmin and gallium-67 citrate scintigraphy for detecting malignant lymphoma. Anticancer Res. 2001;21(5):3695–8. [PubMed] [Google Scholar]
- 50.Gunnoe R, Kalivas J. Technetium scanning in Kaposi’s sarcoma and its simulators. J Am Acad Dermatol. 1982;6(4 Pt 1):463–9. doi: 10.1016/s0190-9622(82)70038-6. [DOI] [PubMed] [Google Scholar]
- 51.Lee VW, Chen H, Panageas E, O’Keane JC, Liebman HA. Subcutaneous Kaposi’s sarcoma. Thallium scan demonstration. Clin Nucl Med. 1990;15(8):569–71. doi: 10.1097/00003072-199008000-00011. [DOI] [PubMed] [Google Scholar]
- 52.Presant CA, Blayney D, Proffitt RT, et al. Preliminary report: imaging of Kaposi sarcoma and lymphoma in AIDS with indium-111-labelled liposomes. Lancet. 1990;335(8701):1307–9. doi: 10.1016/0140-6736(90)91188-g. [DOI] [PubMed] [Google Scholar]
- 53.Harrington KJ, Mohammadtaghi S, Uster PS, et al. Effective targeting of solid tumors in patients with locally advanced cancers by radiolabeled pegylated liposomes. Clin Cancer Res. 2001;7(2):243–54. [PubMed] [Google Scholar]
- 54.Peer FI, Pui MH, Mosam A, Rae WI. 99mTc-MIBI imaging of cutaneous AIDS-associated Kaposi’s sarcoma. Int J Dermatol. 2007;46(2):166–71. doi: 10.1111/j.1365-4632.2006.03001.x. [DOI] [PubMed] [Google Scholar]
- 55.Wardell K, Jakobsson A, Nilsson GE. Laser Doppler perfusion imaging by dynamic light scattering. IEEE Trans Biomed Eng. 1993;40(4):309–16. doi: 10.1109/10.222322. [DOI] [PubMed] [Google Scholar]
- 56.Rivard A, Fabre JE, Silver M, et al. Age-dependent impairment of angiogenesis. Circulation. 1999;99(1):111–20. doi: 10.1161/01.cir.99.1.111. [DOI] [PubMed] [Google Scholar]
- 57.Sorensen J, Bengtsson M, Malmqvist EL, Nilsson G, Sjoberg F. Laser Doppler perfusion imager (LDPI)--for the assessment of skin blood flow changes following sympathetic blocks. Acta Anaesthesiol Scand. 1996;40(9):1145–8. doi: 10.1111/j.1399-6576.1996.tb05578.x. [DOI] [PubMed] [Google Scholar]
- 58.Leu AJ, Yanar A, Jost J, Hoffmann U, Franzeck UK, Bollinger A. Microvascular dynamics in normal skin versus skin overlying Kaposi’s sarcoma. Microvasc Res. 1994;47(1):140–4. doi: 10.1006/mvre.1994.1009. [DOI] [PubMed] [Google Scholar]
- 59.Farina B, Bartoli C, Bono A, et al. Multispectral imaging approach in the diagnosis of cutaneous melanoma: potentiality and limits. Phys Med Biol. 2000;45(5):1243–54. doi: 10.1088/0031-9155/45/5/312. [DOI] [PubMed] [Google Scholar]
- 60.Vogel A, Dasgeb B, Hassan M, et al. Using quantitative imaging techniques to assess vascularity in AIDS-related Kaposi’s sarcoma. Conf Proc IEEE Eng Med Biol Soc. 2006;1:232–5. doi: 10.1109/IEMBS.2006.259462. [DOI] [PubMed] [Google Scholar]
- 61.Vogel A, Chernomordik VV, Riley JD, et al. Using noninvasive multispectral imaging to quantitatively assess tissue vasculature. J Biomed Opt. 2007;12(5):051604. doi: 10.1117/1.2801718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dexue Fu VL, Catherine Foss, James Fox, Martin Pomper, Richard Ambinder. Enzymatically-targeted 131-I therapy for herpesvirus-associated malignancies; ASCO Annual Meeting proceedings; 2006. Journal of Clinical Oncology; 2006. [Google Scholar]
- 63.Fu D, Tanhehco Y, Chen J, et al. Bortezomib-induced enzyme-targeted radiation therapy in herpesvirus-associated tumors. Nat Med. 2008 Sept 7; doi: 10.1038/nm.1864. [Epub ahead of print] PMID 18776891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Van de Wiele C, Oltenfreiter R. Imaging probes targeting matrix metalloproteinases. Cancer Biother Radiopharm. 2006;21(5):409–17. doi: 10.1089/cbr.2006.21.409. [DOI] [PubMed] [Google Scholar]
- 65.Kulasegaram R, Giersing B, Page CJ, et al. In vivo evaluation of 111In-DTPA-N-TIMP-2 in Kaposi sarcoma associated with HIV infection. Eur J Nucl Med. 2001;28(6):756–61. [PubMed] [Google Scholar]