Abstract
Objective
Patient satisfaction is important to payers, clinicians, and patients. The concept of satisfaction is multifactorial and measurement is challenging. Our objective was to explore use of a mixed-methods design to examine patient satisfaction with chiropractic care for low back pain.
Methods
Patients were treated 3 times per week for 3 weeks. Outcomes were collected at Week 3 and Week 4. Qualitative interviews were conducted by the treating clinician and a non-treating staff member. Outcome Measures were the Roland Morris Questionnaire (RMQ), the Visual Analog Scale (VAS), and the Patient Satisfaction Scale (PSS). Interviews were recorded and transcribed, and analyzed for themes and constructs of satisfaction. We compared qualitative interview data with quantitative outcomes, and qualitative data from 2 different interviewers.
Results
All patients reported high levels of satisfaction. Clinical outcomes were unremarkable with little change noted on VAS and RMQ scores. We categorized patient comments into the same constructs of satisfaction as those identified for the PSS: Quality of Care, Information, Effectiveness, and Caring. An additional construct (Quality of Care) and additional subcategories were identified. Satisfaction with care is not explained by outcome alone. The qualitative data collected from 2 different interviewers had few differences.
Conclusion
The results of this study suggest that it is feasible to use a mixed-method design to examine patient satisfaction. We were able to refine data collection and analysis procedures for the outcome measures and qualitative interview data. We identified limitations and offer recommendations for the next step: the implementation of a larger study.
Keywords: chiropractic; manipulation, spinal; back pain; patient satisfaction
INTRODUCTION
Patient satisfaction is increasingly important to stakeholders in the healthcare delivery system, including third party payers, health care providers, and patients, who are increasingly assuming the role of consumers with choices. More recently, satisfaction is being assessed as an outcome in clinical research. In chiropractic clinical research specifically, several studies have shown patients report higher satisfaction with chiropractic care than care received from medical doctors. The concept of satisfaction, however, is multifactorial and measurement is a challenge (1;2). In one study, for example, Breen and Breen reported that 57% of the variance in patient satisfaction was explained by improvement of their condition (3).
A number of instruments measuring patient satisfaction have been developed. Satisfaction measures are: global, measuring overall or general satisfaction: multidimensional, measuring satisfaction with different aspects of patient health and the care received; and disease-specific, such as for low back pain, or generic, appropriate for any patient (4). Satisfaction measures are also classified as direct, measuring the actual experience of a patient in a clinic or study, or indirect, measuring a patient's attitude about their health or care (2;5;6).
To assess satisfaction, Hudak et al (2) recommend supplementing a multidimensional measure with global questions, using a direct measure as opposed to indirect, and using both close- and open-ended questions. They also recommend that satisfaction with care be assessed separately from satisfaction with treatment outcome. Finally, Hudak et al suggest that combining interview data with survey questions may lead to a better understanding of patient satisfaction.
A mixed-methods approach uses both quantitative and qualitative methods . The quantitative approach is widely used in clinical trials, measuring factors such as pain and disability. Qualitative data is increasingly valued for its contributions that inform policy and practice (7). In qualitative research, data are collected in order to describe and explain the meanings people ascribe to specific phenomena (8, 9).
The purpose of the study was to explore the feasibility of using a mixed-method design to examine patient satisfaction with chiropractic care. Our second aim was to compare the qualitative data gathered by the treating clinician with data gathered by a non-treating staff member. Our third aim was to explore possible differences and similarities between patient satisfaction reported in qualitative data to that reported in quantitative measures.
METHODS
Enrollment
This project was approved by the institutional review board of Palmer College of Chiropractic. Patients for this pilot study were recruited by telephone from a database of willing potential participants maintained by the research department. We established a target enrollment of 4 patients, which allowed us to test the study design and procedures within the parameters of very limited resources. Volunteers were screened for preliminary eligibility (Table 1) over the phone. Those that met the inclusion requirements were invited to participate in a baseline visit. They completed baseline outcome and demographic measures and were examined by the study clinician to determine final eligibility status. Eligible patients were asked to return for a second visit where they signed the consent form before being enrolled in the trial.
Table.1.
Inclusion/Exclusion Criteria
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Age 18 and over | LBP from other than somatic tissues as determined by history and examination; |
| Mechanical LBP meeting classification 1, 2, 3, 4, or 6 of the Quebec Task Force (20). | Co-morbid pathology or poor health conditions that significantly complicate the prognosis of LBP; |
| Bone and joint pathology that are contraindications for manipulation; | |
| Retention of legal advice for a health-related claim; | |
| Inability to read or verbally comprehend English; | |
| Clear evidence of narcotic or other drug abuse; Use of manipulative care within the past 4 weeks; | |
| Unwillingness to postpone use of all types of manual treatment for low back pain, except those provided in the study for the duration of the study |
Interventions
Patients were treated 3 times per week for 3 weeks; then, 1 working day after the last treatment of the 3rd week they returned to the clinic to complete outcome measures including a satisfaction questionnaire and to participate in a satisfaction interview (Interview 1). Patients returned to complete a second round of outcome measures including a second satisfaction interview (Interview 2), 3-5 days after interview 1. They also received a final treatment at this time. Choice of patient treatment methods in this pragmatic trial were at the discretion of the study chiropractor and could be applied to the whole spine based on the needs of the patient. Manipulation consisted of Diversified technique and Flexion-Distraction technique (Cox Technic®). Therapeutic modality options included ice, hot packs, stretching, trigger point therapy, and ergonomic and lifestyle advice.
Outcome Measures
Primary outcomes measures were the Roland Morris Back Pain Disability Questionnaire (RMQ) and the visual analog scale for pain (VAS). The RMQ is a 24-item questionnaire specific to low back pain disability. It is reliable and valid (10) and sensitive to clinical change (11). The VAS is a 100-mm line on which patients make a mark corresponding to their level of pain. It is anchored at each end by the descriptors: “No Pain” and “The Worst Pain Possible”. It has been found to be reliable and valid (12-14). Satisfaction was measured using the Patient Satisfaction Scale (PSS), (4) with 2 additional questions modified from the work of Kalauokalani, et. al. (15):
“How satisfied are you with the overall results of your chiropractic care?” Patients mark a number from 0-10 with anchors of not at all satisfied (0) and extremely satisfied (10);
“Compared to my first visit, my low back pain is: entirely gone, much better, slightly better, slightly worse and much worse.”
Outcomes were assessed one working day following the last treatment of week 3 (week 3 outcomes) and again 3-5 days later at the beginning of week 4 (week 4 outcomes).
Qualitative satisfaction interviews were conducted on 2 separate visits by different clinic staff. The 1st interview was conducted 1 working day after the last treatment (week 3) by a non-treating clinical staff person. The 2nd interview was conducted 3-5 days later by the clinician who delivered all care during the study. The timing of interviews was an attempt to minimize the amount of time between the last treatment and the interviews while allowing a few days between interviews so that the previous interview was no longer fresh in the patient's mind. The clinician was blinded to the results of the first interview when conducting the second interview. All interviews were conducted face-to-face, and were guided by a list of semi-structured questions. (Table 2) The questions were based on the constructs of satisfaction identified by Cherkin et al for the PSS: information, caring, and effectiveness (4). Interviews were recorded and transcribed verbatim.
Table.2.
Semi-Structured Satisfaction Interview Questions
| 1. | In general, when you go to a doctor or chiropractor what kinds of things influence how satisfied you are with the overall experience? |
| 1a. | Of the things you just mentioned, which are the most important to you? |
| 2. | Let's shift gears now and talk specifically about the clinic here. Tell me about your satisfaction with the experience you had at this clinic. |
| 2a. | A couple of minutes ago, we talked about the things that are most important to you in terms of satisfaction, these were__________and__________. Tell me about your satisfaction with the clinic here in terms of__________and__________. |
Data Analysis
Quantitative Analysis
The RMQ is scored by counting the number of items selected by the patient. A maximum of 24 points is possible, with higher scores representing greater disability. The VAS is calculated by measuring the number of millimeters from the anchoring line to the patient's mark, resulting in a number from 0 to 100 that indicates level of pain. The PSS is scored on a 5-point Likert scale for each question where 1 = strongly agree, 2 = agree, 3 = neither agree nor disagree, 4 = disagree, 5 = strongly disagree. The values are recoded for analysis to a 1 to 5, most favorable (1) to least favorable (5) scale. This allows equivalent scoring of items where strongly disagree is a positive response (e.g. Question 2: The doctor did NOT give me a clear explanation of the cause of my pain). The recoded values are summed and means are reported for each of the 3 subscales as well as a total satisfaction score. Due to the small sample size in this pilot study, we did not aggregate the data.
Qualitative Analysis
The qualitative analysis began by a read-through of the narratives to get an overall sense of the data, (9;16) and to explore the fit between the narrative data and the constructs of satisfaction identified by Cherkin, et. al. for the PSS. We established a categorization scheme with the use of a conceptually clustered matrix (17) prior to the analysis (Table 3). We started with the preconceived notion that the categories of satisfaction would be those constructs identified by Cherkin, et al., thus, these constructs were the headings of the matrix. The categorical headings of the matrix were adaptive; meaning that new categories and new subcategories could be developed or existing categories deleted during the analysis.
Table 3.
Matrix of Satisfaction Constructs*
| Caring | Quality of Care | Information | Effectiveness |
|---|---|---|---|
| Exchange of information | Proactive | Of Care (Outcome) | |
| Kind of treatment | Informative | Of Doctor | |
| Global treatment approach | Timely | Listening | |
| Understandable | Knowledgeable | ||
| Experienced | |||
| Uses an active management approach |
Original categories for satisfaction in the PSS included the headings information, caring, and effectiveness. Additional category and subcategories were identified from the narrative data.
A line-by-line categorical analysis was then conducted in which each line of the transcript was numbered, and every comment made by patients during the interview was added to the matrix under one of the column headings. Themes and patterns that emerged during the analysis were identified. When a comment was identified that did not fit with the pre-established headings, further modifications to the categorization scheme were made. As we coded the data, sub-categories emerged under the broader headings, and a new category was identified.
The narratives were blinded as to patient identity, interviewer, and whether it was the first or second interview. The co-investigators (RMR and JAP) coded the narratives separately and final coding decisions were reached by consensus. Results of both interviews (week 3 and week 4) are presented together in the results section.
We used the evaluative criteria described by Lincoln and Guba to ensure the integrity of the qualitative data. We:
included narrative quotations to capture the authentic voice of the patients;
mailed transcripts of the interviews to patients and asked them to review their transcripts to determine the accuracy of the data and provide additional feedback, (none provided additional feedback);
met on several occasions during the analysis phase to discuss coding, and if there were discrepancies, come to consensus (peer debriefing) (18;19).
RESULTS
Figure 1 is a flow chart of participant involvement in the trial. We enrolled 4 patients but 2 dropped out soon after entering the study, 1 due to a cardiac problem that required hospitalization and the other due to a family medical emergency. Two additional patients were enrolled to replace the drop-outs. All patients who completed the active care phase of the trial participated in both satisfaction interviews suggesting that the process was tolerable to patients.
Figure 1.
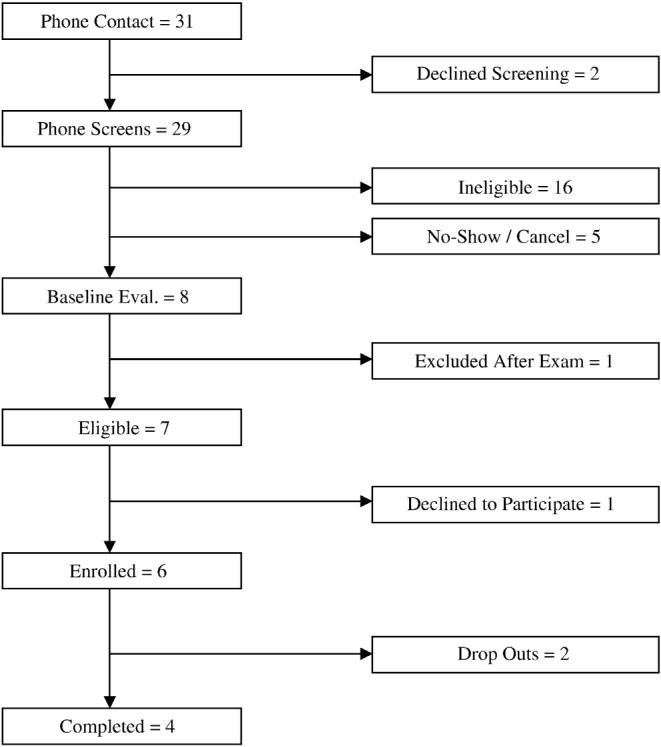
Recruitment and enrollment flow chart.
Baseline demographic data of the 6 patients who enrolled in the study are reported in Table 4. All patients were white, non-Hispanic, non-smokers, ranging in age from 24 to 73 years. Three of the patients were male and 3 female. Of the 4 patients who completed the study, interview and outcome data was obtained on all 4 with the exception of missing data on the week 4 PSS for 1 patient. Clinical outcomes are summarized in Table 5. Patients 2, 4, and 5 showed mild improvement in their low back pain VAS scores. Patient 3 had a mild improvement on VAS at week 3 but was essentially unchanged from baseline by week 4. Patients 2 and 4 had mild improvement in disability scores (RMQ). RMQ score for patient 3 changed from a score of 0 at baseline to 1 by the 4 week outcome and patient 5 changed from 4 at baseline to 3 at week 4, neither of which is considered a clinically important change.
Table 4.
Baseline demographic data
| Variable | n |
|---|---|
| Number of patients | 6 |
| Sex | |
| Female | 3 |
| Ethnicity | |
| Hispanic or Latino | 0 |
| Not Hispanic or Latino | 6 |
| Race | |
| White | 6 |
| Other | 0 |
| Education Level | |
| High School or less | |
| Trade or Tech. School | 1 |
| Some College | 1 |
| College Degree | 3 |
| Professional or Graduate Degree | 1 |
| Employment | |
| Student | 0 |
| Part-time | 1 |
| Full-time | 1 |
| Self-employed (full-time) | 1 |
| Retired | 3 |
| Marital Status | |
| Single (never married) | 2 |
| Married | 4 |
| Living with partner | 0 |
| Separated / Divorced | 0 |
| Widowed | 0 |
| Have health insurance? | |
| Yes | 5 |
| Insurance covers chiropractic? | |
| No | 1 |
| Yes | 3 |
| Don't Know | 1 |
| Tobacco Use (No) | 6 |
Table 5.
Baseline and follow-up outcome scores
| Variable / Patient | Baseline | 3 weeks | 4 weeks |
|---|---|---|---|
| VAS (0-100mm) | |||
| Patient 1 | 64 | -* | - |
| Patient 2 | 15 | 7 | 5 |
| Patient 3 | 33 | 26 | 36 |
| Patient 4 | 34 | 15 | 15 |
| Patient 5 | 34 | 28 | 26 |
| Patient 6 | 32 | - | - |
| Roland Morris (0=no disability) | |||
| Patient 1 | 13 | - | - |
| Patient 2 | 3 | 0 | 1 |
| Patient 3 | 0 | 0 | 1 |
| Patient 4 | 5 | 3 | 1 |
| Patient 5 | 4 | 3 | 3 |
| Patient 6 | 10 | - | - |
| Overall satisfaction (0=not at all satisfied, 10=extremely satisfied) | |||
| Patient 1 | - | - | |
| Patient 2 | 8 | 9 | |
| Patient 3 | 10 | 8 | |
| Patient 4 | 9 | 2 | |
| Patient 5 | 10 | 10 | |
| Patient 6 | - | - | |
| Compared to first visit LBP is (1-6) †: | |||
| Patient 1 | - | - | |
| Patient 2 | 2 | 2 | |
| Patient 3 | 3 | 3 | |
| Patient 4 | 2 | 2 | |
| Patient 5 | 3 | 3 | |
| Patient 6 | - | - | |
| PSS total score (mean)†† | |||
| Patient 1 | - | - | |
| Patient 2 | 1.8 | 1.8 | |
| Patient 3 | 2.2 | - | |
| Patient 4 | 1.3 | 1.2 | |
| Patient 5 | 1.6 | 1.6 | |
| Patient 6 | - | - | |
| PSS Information subscale (mean) | |||
| Patient 1 | - | - | |
| Patient 2 | 2.0 | 2.0 | |
| Patient 3 | 2.0 | - | |
| Patient 4 | 1.3 | 1.0 | |
| Patient 5 | 1.0 | 2.0 | |
| Patient 6 | - | - | |
| PSS Caring subscale (mean) | |||
| Patient 1 | - | - | |
| Patient 2 | 1.3 | 1.8 | |
| Patient 3 | 2.0 | - | |
| Patient 4 | 1.0 | 1.0 | |
| Patient 5 | 1.0 | 1.0 | |
| Patient 6 | - | - | |
| PSS Effectiveness subscale (mean) | |||
| Patient 1 | - | - | |
| Patient 2 | 2.0 | 2.0 | |
| Patient 3 | 2.3 | - | |
| Patient 4 | 1.7 | 1.7 | |
| Patient 5 | 2.3 | 2.0 | |
| Patient 6 | - |
- Indicates missing data
1-Entirely gone, 2-Much better, 3-Slightly better, 4-Unchanged, 5-Slightly worse, 6-Much worse
1 = Most satisfied, 5 = Least satisfied.
Results for the PSS and the two additional satisfaction questions are listed in Table 5. Patient total and subscale scores all indicated high levels of satisfaction, ranging from 1.0 to 2.3 where 5.0 is the least satisfaction. Figure 2 lists the questions and subscales of satisfaction in the PSS. We concentrated on the subscales of satisfaction from the PSS when analyzing the interview data. The first question of the satisfaction outcome (How satisfied are you with the overall results of your chiropractic care?) is scored from 0 to 10 with 10 representing highest satisfaction. All showed high overall satisfaction at the end of week 3 and 3-5 days later at the beginning of week 4 except patient 4, whose values changed from 9 to 2.
Figure 2.
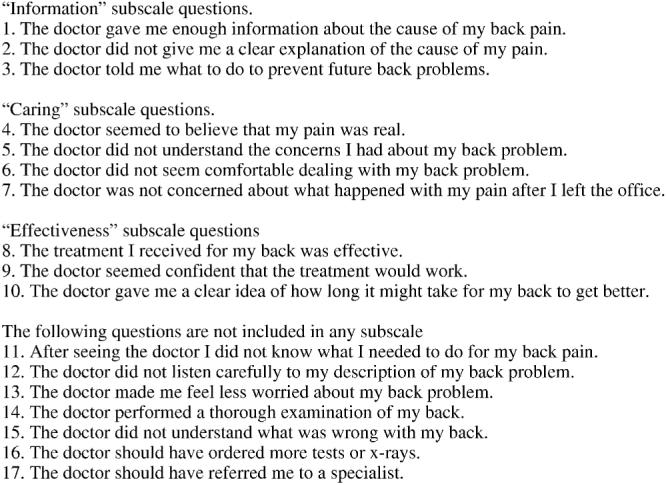
PSS questions and subscales of satisfaction.
The qualitative interviews also revealed that patients were highly satisfied. One patient (Patient 3) expressed dissatisfaction with the number of treatments and that the length of the treatment sessions was too short. In general, more in-depth information about patient satisfaction was gathered in the second interviews (Table 6).
Table 6.
Constructs of satisfaction and subcategories coded in interviews for all patients
| Patient 2 | Patient 5 | Patient 3 | Patient 4 | |
|---|---|---|---|---|
| Interview 1 | 1. Effectiveness of Doctor - Active management approach | 1. Effectiveness of Doctor - Listening | 1. Effectiveness of Care | 1. Quality of Care - Exchange of information |
| 2. Effectiveness of Doctor - Listening | 2. Quality of Care - Exchange of information | 2. Quality of Care - Kind of treatment | 2. Effectiveness of Care | |
| 3. Effectiveness of Care | 3. Information Timely | 3. Effectiveness of Doctor - Knowledgeable | ||
| 4. Quality of Care - Kind of treatment | 4. Information Proactive | 4. Effectiveness of Doctor - Experienced | ||
| 5. Quality of Care - Exchange of Information | 5. Information Informative | 5. Information - Proactive | ||
| 6. Effectiveness of Care | 6. Quality of Care - Kind of treatment | |||
| 7. Information Understandable | 7. Effectiveness of Doctor - Active management | |||
| 8. Caring | ||||
| 9. Quality of Care - Global approach | ||||
| Interview 2 | 1. Effectiveness of Care | 1. Quality of Care - Exchange of information | 1. Effectiveness of Care | 1. Quality of Care - Exchange of information |
| 2. Effectiveness of Doctor - Listening | 2. Information Timely | 2. Information Informative | 2. Effectiveness of Doctor - Listening | |
| 3. Effectiveness of Doctor - Knowledgeable | 3. Effectiveness of Care | 3. Quality of Care - Exchange of information | 3. Caring | |
| 4. Quality of Care - Exchange of Information | 4. Effectiveness of Doctor - Knowledgeable | 4. Caring | 4. Effectiveness of Doctor - Knowledgeable | |
| 5. Information - Understandable | 5. Information Informative | 5. Effectiveness of Doctor - Active management | ||
| 6. Information - Proactive | 6. Information Proactive | 6. Information - Proactive | ||
| 7. Quality of Care - Kind of treatment | 7. Quality of Care - Global approach | 7. Effectiveness of Care | ||
| 8. Quality of Care - Global approach | 8. Quality of Care - Kind of treatment | |||
| 9. Information - Informative | 9. Quality of Care - Global approach |
The contrast of interview vs. PSS subscales follows:
The first subscale of the PSS is Information, which is made up of 3 questions. These questions focus on informing the patient about the cause of their pain and what to do to prevent future back pain. Based on our interview data, we divided the information subscale into further subcategories. For example, Patient 5 says “I want to stay informed on what's going on… keeping me informed about what's causing it; what I can do better.” Patients' comments showed a desire for what we termed proactive information. That is information about what they could do not only to prevent future pain but to speed their recovery. They also wanted information to keep them informed in a timely or up-to-date fashion, which we termed timely information. Patient 5 states “I tend to want to stay informed on really (unintelligible word) important about my health so when they're doing tests or doing anything I want to know why they're doing what they're doing. I want to know the cause of it. I want to know how it can be prevented. I want to know what… like… I can do. I like information to be given to me.” Patients want information that is understandable and informative. Patient 2 noted that s/he wants information explained “in layman's terms,” and felt pleased with participation in the study because s/he “learned something.”
The next subscale of satisfaction in the PSS is Caring. The 4 questions of this subscale ask if the doctor believes the patient, understands the patient's concerns, was comfortable dealing with the patient's pain and was concerned about the patient after they left the office. The patients we interviewed de-emphasized caring as a subscale compared to the emphasis placed on it in the PSS. Patient 4 gave this example of caring: “if they… seem like they believe what you say about your pain or whatever.” Patient 4 noted a negative example of caring from recent experiences outside of our study. In his/her interview Patient 4 noted: “I felt kind of brushed off by the medical community here lately.” This was a sentiment that he/she repeated in the second interview: “this one doctor treated me like I was making it up.” None of the patients placed examples of caring in their top indicators for judging satisfaction.
The final subscale of the PSS is Effectiveness. This subscale contains 3 questions, 1 about treatment effectiveness, 1 about doctor confidence, and 1 about the patient gaining a “clear idea of how long it might take” to get better. The comments of patients we interviewed led us to break this subcategory into 2 areas: effectiveness of treatment, and effectiveness of doctor.
We asked all patients to identify their top indicators for judging satisfaction. Effectiveness of treatment or treatment outcome was identified for all the patients (Table 7). Patient 3: “Well, I am looking for relief of my lower back pain. That's the reason I came here.” Patient 2: “Well, primarily the outcome. I mean if I go away feeling better that's the most important thing.” Patient 3, when asked “what would you say is the most important to you?” replied “the results.”
Table 7.
Top indicators of satisfaction for each patient
| Patient | General | Specifically in this study |
|---|---|---|
| Patient 2 | Effectiveness of Care (outcome) | Effectiveness of Care (outcome) |
| Effectiveness of Doctor | Information | |
| Listening | Proactive | |
| Knowledgeable | ||
| Patient 3 | Effectiveness of Care (outcome) | Effectiveness of Care (outcome) |
| Caring | ||
| Patient 4 | Effectiveness of Care (outcome) | Effectiveness of Care (outcome) |
| Effectiveness of Doctor | Quality of Care | |
| Listening | Kind of care | |
| Knowledgeable | ||
| Patient 5 | Information | Effectiveness of Care (outcome) |
| Timely | Information | |
| Informative | Understandable | |
| Proactive | Informative |
Interview data led us to further subdivide effectiveness of doctor into 4 additional subcategories: listening, knowledgeable, experienced, and used an active management approach. An important aspect of satisfaction for Patient 2 was “how well I think they are listening to me.” The importance of an active management approach was also stressed by several patients. Patient 4 noted that his/her problem had been “addressed… more than it's been addressed in the past with any other chiropractor… and he was interested in coming up with different paths of investigation.” S/he said other doctors “did the cat scan and stuff and they didn't see anything and left it at that… none of them actually said well lets do some more tests,” despite his/her ongoing complaint.
Another category of satisfaction that emerged as we conducted the qualitative interviews and analysis was quality of care. This was further divided into 3 subcategories: exchange of information, kind of treatment, and global approach to treatment. Exchange of information is a category beyond just listening or providing information. This is a 2 way interactive flow of information. Patient 2 gave this example: “I remember one incident a long time ago and I was going in to see the doctor pretty discouraged about what was happening to me, and I just said that I think it's this and this and this; and he said well, you're probably right. It's your body.” Kind of treatment was an aspect of satisfaction expressed by several patients. When asked what was important for satisfaction Patient 2 said “primarily the kind of treatment… I think it was something that was especially workable for me.” Patient 4 also noted that kind of care was important s/he related an experience where the s/he felt the kind of treatment was inappropriate: “The chiropractor that I've been working with in the past, just, I'm not really satisfied with… because there was, you know, there was very little what I would consider appropriate work done on my lower back. I felt her approach was insignificant… and had no effect, ineffective.” Global treatment approach was important to Patient 2 who said “it's a low back study, and you were dealing with my arm and that problem, and, you know, working on healing that also. So it went beyond… I guess, because I feel like everything is connected anyway. So it goes anything goes beyond the lower back.” Patient 4 also noted that “I was happy to get involved… because I felt that my biggest problem is with my neck… and that has improved greatly.”
In addition to the subscales of information, caring, and effectiveness, the PSS also includes 7 questions that are not grouped in a subscale of satisfaction. The first question asked if after seeing the doctor the patient would know what to do for the back pain. Patients in our study expressed the importance of proactive information which is how we categorized this sort of comment. Whether the doctor listened carefully to the patient's description of the back problem was the second of the non-categorized questions. We categorized patient comments as effectiveness of doctor - listening that matched this question. The question asking if the doctor made the patient feel less worried about their back problem was a theme not expressed by our patients. Our patients did talk about the importance of the doctor's knowledge, experience, and an active approach to management which fits with the next questions paraphrased here as: the doctor performed a thorough examination, understood what was wrong with my back, should have ordered more tests, or referred me to a back specialist.
DISCUSSION
The purpose of the study was to explore the feasibility of using a mixed-method design to examine patient satisfaction with chiropractic care. We successfully enrolled, treated, and evaluated the data for 4 patients who finished the study. Patient compliance with protocols was good: One patient inadvertently skipped the page of the satisfaction outcome containing the PSS. The patients who finished the active care phase were compliant with the 2 outcome visits with 2 recorded satisfaction interviews. We determined that gathering and analyzing both quantitative and qualitative data was feasible in this pilot study.
Our second aim was to compare the qualitative data gathered by the treating clinician and data gathered by a non-treating staff member. We conducted 2 separate qualitative interviews for each patient using different interviewers. While we successfully conducted 2 interviews on each patient, we had theorized that patients might not be as candid with the treating clinician as with another interviewer. Prior to implementing the study we believed that patients who were dissatisfied with their experience in our study would be less forthcoming about their dissatisfaction with the clinician who treated them, hence the 2 interview design. We were not fully able to test this theory since all patients scored high levels of satisfaction on the quantitative measures and described high levels of satisfaction in the interviews. One patient (patient 3) said that more treatments or longer treatment sessions would have been more satisfying possibly providing more relief. The patient expressed this to both interviewers.
The transcripts of the second interviews were all longer than the first interviews and contained as much or more information. This indicates more probing by the second interviewer (the treating clinician). This may be due to the clinician having more experience at interviewing patients than either of the other interviewers who did the first interviews. The 2 interview format was not productive although because of the small number of patients in this study, this conclusion might not hold true in a larger study.
Our third aim was to explore possible differences and similarities between satisfaction of patients reported in qualitative data to that reported in quantitative measures. 3 of the 4 patients reported high satisfaction. At the Week 3 data collection point, Patient 4 reported an overall satisfaction level of 9 (10 being highest satisfaction), and this level dropped to a 2 reported at Week 4. It is possible that this patient misinterpreted the scale the second time completing the outcome or that his or her satisfaction could have been reversed. The former theory is borne out by noting that all other satisfaction measures of patient 4 are essentially unchanged from week 3 to week 4 and the interview data indicated no great change in satisfaction between week 3 and week 4.
All patients had similarly good satisfaction scores on the Information subscale of the PSS. Information was also a top indicator of satisfaction for patients 2 and 5. Patient 3 was the only patient who reported that Caring was a top indicator of satisfaction. All patients had good scores on the Caring subscale of the PSS. The remaining top indicators were not represented in the PSS subscales.
We identified similar constructs of patient satisfaction to those described by Cherkin, et. al.; however, additional subcategories and a distinct category was developed to accommodate the narrative data. As mentioned previously, the PSS instrument includes the constructs of Caring, Effectiveness, and Information, and these were foundational to our initial categorization scheme. We found, however, that adding a category (Quality of Care), and subdividing Effectiveness into Effectiveness of Doctor and Effectiveness of Care (outcome) accommodated the rich descriptions of satisfaction that the patients shared.
When asked to give the top indicator for assessing satisfaction, all 4 patients reported that Effectiveness of Care (outcome) was one of the top priorities for assessing satisfaction. This is of interest because patients have been reported to have high satisfaction with chiropractic care, but satisfaction is not entirely explained by outcome. Our findings suggest that additional constructs of satisfaction are important, and may help explain the incomplete correlation of outcome to satisfaction in low back trials.
Another area contributing to satisfaction that was identified in our findings was the kind of treatment. There are many techniques currently being used in chiropractic, and while there are similarities, there are also vast differences. In chiropractic clinical research, patients are often treated with a single type of intervention. Our findings suggest the importance of chiropractic research incorporating different techniques.
Limitations
The sample size in the study is small (4 patients), which does not allow for generalization to a larger population or inferential statistics. However, we believe that this small n study was useful to „test run” the study design and procedures, and make modifications accordingly before committing resources on a larger study. Another limitation to this study was that the interviewers who conducted the first qualitative interviews had minimal training in interviewing. We plan to implement more training in this area in the next study.
CONCLUSION
The results of this study suggest that it is feasible to use a mixed-method approach to examine patient satisfaction. Moreover, additional satisfaction data may be obtained by including a qualitative component along with standard outcome measures in a clinical trial. We plan to conduct a larger pilot study to compare the satisfaction of patients reported in qualitative data to that reported in quantitative measures in order to possibly modify an existing instrument that is more applicable for chiropractic clinical research.
PRACTICAL APPLICATIONS.
Patient satisfaction is multifactorial and difficult to measure
Quantitative and qualitative measures may be used to assess patient satisfaction
Factors that influence patient satisfaction can be categorized
Patients in this study described more factors influencing satisfaction than are measured by a standard satisfaction outcome measure
ACKNOWLEGEMENTS
The authors wish to thank Lori Byrd-Spencer and Therese Devlin for calling potential patients, Ilke Schwarz, DC, MS, and Therese Devlin for conducting satisfaction interviews, Leah Cafer for transcribing recorded interviews, Lance Corber for assistance with data management and Edward F. Owens, Jr., MS, DC, Dana J. Lawrence, DC, MMedEd, and Cynthia R. Long, PhD, for design guidance and editorial help with the manuscript. This investigation was conducted in a facility constructed with support from Research Facilities Improvement Grant Number C06 RR15433 from the National Center for Research Resources, National Institute of Health. This project was made possible by Grant Number K01-AT000977 from the National Center for Complementary and Alternative Medicine (NCCAM). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCCAM, or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- (1).Coulter ID, Hays RD, Danielson CD. The chiropractic satisfaction questionnaire. Top Clin Chiropr. 1994;1:40–43. [Google Scholar]
- (2).Hudak PL, Wright JG. The characteristics of patient satisfaction measures. Spine. 2000;25:3167–3177. doi: 10.1097/00007632-200012150-00012. [DOI] [PubMed] [Google Scholar]
- (3).Breen A, Breen R. Back pain and satisfaction with chiropractic treatment: what role does the physical outcome play? Clin J Pain. 2003;19:263–268. doi: 10.1097/00002508-200307000-00010. [DOI] [PubMed] [Google Scholar]
- (4).Cherkin D, Deyo RA, Berg AO. Evaluation of a physician education intervention to improve primary care for low-back pain. II. Impact on patients. Spine. 1991;16:1173–1178. doi: 10.1097/00007632-199110000-00008. [DOI] [PubMed] [Google Scholar]
- (5).George SZ, Hirsh AT. Distinguishing patient satisfaction with treatment delivery from treatment effect: a preliminary investigation of patient satisfaction with symptoms after physical therapy treatment of low back pain. Arch Phys Med Rehabil. 2005;86:1338–1344. doi: 10.1016/j.apmr.2004.11.037. [DOI] [PubMed] [Google Scholar]
- (6).Hudak PL, Hogg-Johnson S, Bombardier C, McKeever PD, Wright JG. Testing a new theory of patient satisfaction with treatment outcome. Med Care. 2004;42:726–739. doi: 10.1097/01.mlr.0000132394.09032.81. [DOI] [PubMed] [Google Scholar]
- (7).Dixon-Woods M, Sutton A, Shaw R, Miller T, Smith J, Young B, et al. Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Policy. 2007;12:42–47. doi: 10.1258/135581907779497486. [DOI] [PubMed] [Google Scholar]
- (8).Greenhalgh T, Taylor R. Papers that go beyond numbers (qualitative research) BMJ. 1997;315:740–743. doi: 10.1136/bmj.315.7110.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Creswell JW. Qualitative inquiry and research design: Choosing among five traditions. Sage Publications; Thousand Oaks, CA: 1998. [Google Scholar]
- (10).Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine. 2000;25(24):3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- (11).Stratford PW, Binkley JM, Riddle DL. Health status measures: Strategies and analytic methods for assessing change scores. Phys Ther. 1996;76:1109–1123. doi: 10.1093/ptj/76.10.1109. [DOI] [PubMed] [Google Scholar]
- (12).Mantha S, Thisted R, Foss J, Ellis JE, Roizen MF. A proposal to use confidence intervals for visual analog scale data for pain measurement to determine clinical significance. Anesth Analg. 1993;77:1041–1047. doi: 10.1213/00000539-199311000-00029. [DOI] [PubMed] [Google Scholar]
- (13).Miller MD, Ferris DG. Measurement of subjective phenomena in primary care research: the Visual Analogue Scale. Fam Pract Res J. 1993;13:15–24. [PubMed] [Google Scholar]
- (14).Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- (15).Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine. 2001;26:1418–1424. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- (16).Holloway I. Basic concepts for qualitative research. Blackwell Science; Oxford: 1997. [Google Scholar]
- (17).Miles MB, Huberman AM. Qualitative data analysis. 2nd ed. Sage Publications; Thousand Oaks, CA: 1994. [Google Scholar]
- (18).Lincoln YS, Guba EG. Paradigmatic controversies, contradictions, and emerging confluences. In: Denzin N, Lincoln YS, editors. Handbook of Qualitative Research. Sage; Thousand Oaks, CA: 2000. pp. 163–188. [Google Scholar]
- (19).Lincoln YS, Guba EG. Naturalistic inquiry. Sage; Beverly Hills, CA: 1985. [Google Scholar]
- (20).Spitzer WO, LeBlanc FE, Dupuis M. Scientific Approach to the assessment and management of activity-related spinal disorders: A monograph for clinicians; Report of the Quebec Task Force on Spinal Disorders. Spine. 1987;12:1S–59S. [PubMed] [Google Scholar]


