Abstract
Unexplained pain after hip arthroplasty is frustrating for patients and surgeons. We describe the use of hip arthroscopy in management of the painful hip arthroplasty, critically evaluate the outcomes of these patients, and refine indications for hip arthroscopy in this setting. We retrospectively reviewed 14 patients (16 hips) who underwent hip arthroscopy after joint replacement. One patient had suspected septic arthritis despite negative aspiration and one had known septic arthritis but was not a candidate for open arthrotomy; two had intraarticular migration of hardware. The remaining 10 patients (11 hips) had persistent pain despite negative diagnostic studies. The two patients (two hips) with infection were successfully treated with arthroscopic lavage and débridement plus intravenous antibiotics. Intraarticular metal fragments and a loose acetabular screw were successfully removed in two patients (three hips). Findings in the remaining 11 hips included a loose acetabular component (one); corrosion at the head-neck junction of a metal-on-metal articulation (one); soft tissue-scar impingement at the head/cup interface (four); synovitis with associated scar tissue (four); and capsular scarring with adhesions (one). Arthroscopy represented a successful treatment or directly led to a successful treatment in 12 of 16 hips. We observed no complications as a result of the arthroscopy. Arthroscopy may be of value in selected patients undergoing hip arthroplasty with unexplained pain after an inconclusive standard workup.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Persistent pain after hip arthroplasty often presents a diagnostic and therapeutic challenge. In many cases, a standard workup, including plain radiographs, peripheral blood studies, joint aspiration, and bone scan, can lead to treatable diagnoses such as loosening or infection [2, 14]. However, there remains a subset of patients in whom these studies are nondiagnostic, often leading to frustration for both the patient and physician.
The advent of reproducible and safe techniques for hip arthroscopy has allowed minimally invasive access to the hip and the ability to inspect, diagnose, and treat various problems associated with hip abnormalities [12]. Naturally, as experience with hip arthroscopy has developed, indications have evolved over time. For patients who have previously undergone hip arthroplasty, reports have described arthroscopy for retrieval of third bodies [3, 10, 13, 16] and for débriding infection [4]. While a number of authors report the use of arthroscopy to evaluate and treat various painful conditions after knee arthroplasty [1, 5, 7, 11, 15, 17–20], its usefulness in evaluating and treating the chronically painful hip arthroplasty (after a negative standard workup) is not known.
The purpose of this study was (1) to review the results of hip arthroscopy after THA in a consecutive series of patients; and (2) to examine the indications for hip arthroscopy in patients with a painful hip arthroplasty and a negative workup for loosening and infection.
Materials and Methods
We retrospectively reviewed 14 patients (16 hips) who underwent arthroscopy after THA between September 1997 and December 2006 (Table 1). We did not exclude any patients who underwent arthroscopy following hip arthroplasty during this time period. Indications for arthroscopy were intractable pain despite negative radiographs and aspiration arthrogram. The laboratory findings (CBC with differential, C-reactive protein, and sedimentation rate) were within normal range in all except for one patient with known sepsis who was medically compromised and could not undergo open arthrotomy. All patients underwent hip aspiration (16 hips). This was nondiagnostic except in the aforementioned case of known sepsis. No patients had a bone scan. Two patients (two hips) received a diagnostic lidocaine injection but neither experienced substantial relief of symptoms. Two additional patients (two hips) received a Marcaine plus cortisone injection into the psoas sheath that failed to provide symptomatic relief. All of the patients in the diagnostic dilemma group were counseled and fully understood that the arthroscopic procedure might not be able to diagnose or solve the problem and that an open procedure still might be necessary. These patients all chose to proceed with arthroscopy given this information.
Table 1.
Summary of reported cases
| Case number* | Age (years) | Preoperative diagnosis | Postoperative diagnosis | Intervention | Followup (years after arthroscopy) | Clinical outcome |
|---|---|---|---|---|---|---|
| Diagnostic dilemmas | ||||||
| 1† | 58 | Suspected sepsis | Sepsis | Irrigation and débridement | 3 | No recurrence of infection |
| 5 | 71 | Intractable pain | Impingement of scar tissue | Débridement of scar tissue | 3 | Eventual acetabular revision |
| 6† | 67 | Intractable pain; fluid collection | Corrosion at the head-neck junction | Débridement of metal debris | 1 | Revision arthroplasty for metal hypersensitivity |
| 7 | 46 | Intractable pain | Loose acetabular component | None | 6.5 | Acetabular revision |
| 8 | 44 | Intractable pain | Anterior scar tissue with reactive synovitis | Débridement of scar tissue | 10 | Resolution of symptoms; no further intervention |
| 10 | 66 | Intractable pain | Adhesions; capsular scar | Débridement of adhesions and scar tissue | 1 | Acetabular revision at 1 year postoperatively |
| 11 | 50 | Intractable pain | Anterior scar tissue with reactive synovitis | Débridement of scar tissue | 1 | Open arthrotomy with psoas recession 1 year postoperatively |
| 12 | 45 | Intractable pain | Scar tissue; synovitis | Débridement of scar tissue | 1 | Continued pain but declined further intervention |
| 13 | 51 | Intractable pain | Anterior scar tissue with reactive synovitis | Débridement of scar tissue | 3 | Resolution of symptoms; no further intervention |
| 14 | 48 | Intractable pain | Anterior scar tissue impingement, small area corrosion with reactive synovitis | Débridement of scar tissue | 2 | Resolution of symptoms; no further intervention |
| 15 | 38 | Intractable pain | Anterior scar tissue impingement, small area corrosion with reactive synovitis | Débridement of scar tissue | 3 | Resolution of symptoms; no further intervention |
| 16 | 58 | Intractable pain | Dense anterior scar tissue impingement, reactive synovitis | Débridement of scar tissue | 1 | Resolution of symptoms; no further intervention |
| Therapeutic alternative | ||||||
| 2 | 83 | Sepsis | Sepsis | Irrigation and débridement | 3 | No recurrence of infection |
| 3 | 67 | Migrated wire | Migrated wire, loose metal beads | Removal of foreign bodies | 2 | Successful removal; second wire migrated at later date (see Case 9 subsequently) |
| 4 | 68 | Loose screw | Loose screw | Removal of screw | 9 | Successful removal; no further intervention |
| 9 | 72 | Migrated wire | Migrated wire | Removal of wire | 4 | Successful removal; no further intervention |
* Numbered chronologically; †see Results section for a more detailed description of these representative cases.
One patient underwent arthroscopy of bilateral painful THAs 7 years apart. One patient (one hip) underwent hip arthroscopy twice for recurrent migration of trochanteric wires into the articulation. We based outcomes on review of medical records from the patient’s most recent followup visit; no patients were specifically recalled for this study. The study group consisted of four men and 10 women with a mean age of 59 years (range, 38–83 years). All patients were available for followup at a minimum of 1 year (range, 1–9 years). This study was approved by our institutional review board.
All procedures were performed by the senior author (JCM). All patients received general anesthesia and were discharged on the day of surgery. The senior author prefers the lateral decubitus position because it provides reproducible bony landmarks for orientation and facilitates access for instrumentation. Patients were positioned in a specialized distraction device (Innomed, Savannah, GA) with appropriate padding to protect against neuropraxia. Two or three peritrochanteric portals were used.
After skin penetration, we used sheathed blunt trocars to pass through the intervening adipose, fascia, and muscle tissue until the hip capsule became palpable as a firm but not solid structure. This protects all interceding neurovascular structures and muscle from sharp equipment and repetitive trauma during the exchange of instruments and scopes. The entry point for the anterior superior trochanteric portal was placed at the junction of the anterior and mid 1/3 of the superior greater trochanteric ridge. We placed the posterosuperior trochanteric portal at the junction of the mid and posterior 1/3 of the superior greater trochanteric ridge. These portals can be switched between the camera and instrumentation as necessary. Cannulae were directed at the prosthetic neck under fluoroscopic control. We inserted the arthroscope after the capsule was distended with saline. After fluid was sent for culture, adhesions and periprosthetic granulation tissue were thoroughly débrided. If there were third-body particles within the hip (trochanteric wires, beads, and so on), we distracted the joint for removal. Finally, the joint was lavaged with at least 20,000 mL of sterile saline. There was typically less than 10 mL of blood loss. Total surgical time was typically less than 1 hour (mean, 45 minutes; range, 30–65 minutes).
Once the patients were awake and transferred to the day surgery center, they were taught to walk with crutches. We used no formal physical therapy. Patients were discharged home the same day and seen in the office at 1 week for an initial wound check and suture removal. Patients were then seen for routine clinical checks at 6 weeks, 3 months, and annually thereafter.
The surgeon must pay close attention to various technical aspects of the procedure to avoid known complications. Traction should be applied for as short a duration as possible and the groin and foot must be well-padded to avoid postoperative nerve palsies, skin abrasions, and ankle pain. Meticulous sterile technique is of utmost importance given the underlying prosthesis. Attention must also be paid to ensuring that the metal arthroscopy cannulae do not scratch the articulating surface. We had available multiple arthroscopy sets and arthroscopes so all the arthroscopy kits and arthroscopes were fully sterilized between cases.
Results
There were no perioperative complications in this series of 15 patients (16 hip arthroscopies). Patients were full weight bearing and used crutches for an average of 5 days (range, 2–7 days).
Twelve cases were performed for diagnostic purposes (Table 1). One patient (Case 1) had suspected sepsis that could not be confirmed by standard testing (Table 1). Eleven cases had hip arthroscopy for persistent pain despite negative radiographs and aspiration arthrogram. Findings included a loose acetabular component (one); corrosion at the head-neck junction of a metal-on-metal articulation (one); soft tissue-scar impingement at the head/cup interface (four); synovitis with associated scar tissue (four); and capsular scarring with adhesions (one).
In four cases, arthroscopy was used as an alternative to open arthrotomy for selected clinical scenarios. One case (Case 2) of joint sepsis in a patient who was not a candidate for open arthrotomy was lavaged and débrided arthroscopically and treated with intravenous antibiotics without recurrent sepsis at minimum 3-year followup. Intraarticular metal fragments (Fig. 1A–B) and a loose acetabular screw (Fig. 2A–C) were successfully removed through arthroscopic means in three cases.
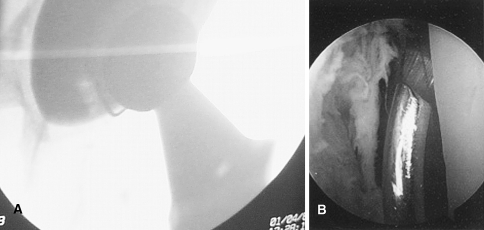
Fig. 1A–B.
Case 3. (A) A fluoroscopic image shows a migrated trochanteric wire noted 3 years after revision left hip arthroplasty. (B) An intraoperative photograph shows the same hip during arthroscopic wire removal.
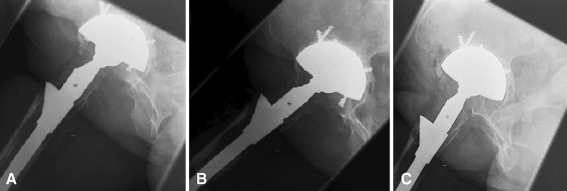
Fig. 2A–C.
Case 4. (A) Serial radiographs demonstrate progressive loosening and migration of a peripheral acetabular screw after THA. (B) Shows progression of screw backing out. (C) Shows plain radiograph after screw was removed arthroscopically.
Overall, arthroscopy represented a successful treatment (six patients, six hips) or directly led to a successful treatment (revision of components in two patients, two hips) in eight of 12 cases considered diagnostic dilemmas at the time of surgery. Four of the nine patients with isolated abnormal soft tissue findings had persistent symptoms after débridement. Arthroscopy was a successful therapeutic alternative in all four patients with known problems.
Selected Case Reports
Case 1
A morbidly obese 58-year old woman underwent bilateral THA and, 5 years later, had revision on the left hip for aseptic loosening. She presented 2 years after revision with recurrent and intractable hip pain. Hip aspiration was difficult because of her obesity. Two aspirations were nondiagnostic; one produced no joint fluid and the other grew Staphylococcus aureus on broth only. Her erythrocyte sedimentation rate and C-reactive protein levels were mildly elevated. Because of this inconclusive evidence, hip arthroscopy was performed to obtain joint fluid and a synovial biopsy. Concurrent joint lavage and débridement were planned. At the time of arthroscopy, a sample of joint fluid was obtained and sent for culture. Hypertrophic and hyperemic synovial lining was encountered and aggressively débrided. The joint fluid sample grew S. aureus on solid media. Parenteral antibiotics were administered for 6 weeks. She did not undergo any subsequent procedures on the left hip. At 3 years postoperatively, there has been no recurrence of infection and her hip pain has resolved.
Case 6
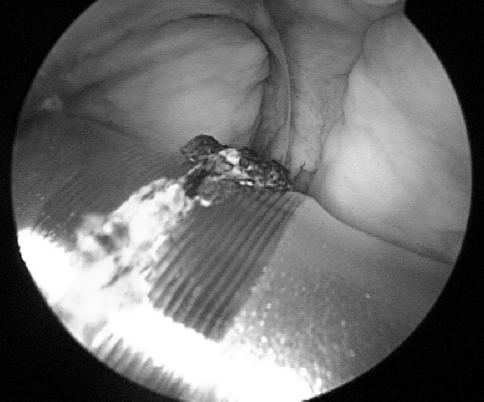
A 67-year-old man presented 16 months after THA with a metal-on-metal articulation with persistent groin and thigh pain of 6 months’ duration. The pain was worse with weight bearing and he required a cane for support. Physical examination revealed large, prominent soft tissue swelling in the left proximal thigh. Radiographs and ultrasound were negative. Hip aspiration was negative for signs of infection. Hip arthroscopy revealed diffuse metal synovitis, corrosion at the femoral head-neck junction (Fig. 3), and numerous porous beads within the joint and at the articulation. There was abundant reactive granulation tissue throughout the joint. The patient was referred back to his operating surgeon for further workup and was subsequently diagnosed with metal hypersensitivity. The patient was eventually treated with revision to a metal-on-polyethylene articulation 1 year after arthroscopy.
Fig. 3.
Case 6. An intraoperative photograph shows corrosion at the femoral head-neck junction in a patient with diffuse metal synovitis.
Discussion
Improvements in instrumentation, safe joint distraction techniques, and surgical expertise have overcome the technical challenges that previously limited hip joint access through arthroscopy. The ability to directly diagnose and treat hip abnormalities with minimally invasive techniques continues to evolve. Indications for hip arthroscopy in the native hip have included management of labral tears and chondral lesions, removal of loose or foreign bodies, subtotal synovectomy, and synovial biopsy and pyarthrosis [12]. The role of arthroscopy in the workup and treatment of problems related to previous hip arthroplasty is less clear. Specifically, the value of arthroscopy in evaluating the persistently painful hip arthroplasty remains unknown.
Limitations of this study include the absence of standardized preoperative and postoperative outcomes scores. However, in this group of patients with somewhat unusual clinical problems, it would be difficult to determine what outcome instrument would best capture their hip status. Furthermore, although this series represents an inclusive group of patients who underwent arthroscopy postarthroplasty, we did not define strict inclusion criteria in advance.
A number of case reports [9, 10, 13] and small case series [4, 6] have described hip arthroscopy after previous arthroplasty. Hyman et al. [4] reported eight patients treated with arthroscopic irrigation and débridement for confirmed late periprosthetic infection. They noted no recurrence of infection and no progressive radiographic loosening at a mean followup of 70 months [4]. Open arthrotomy and débridement has remained our standard treatment for the acutely infected hip arthroplasty. However, we successfully treated one patient who was not a candidate for open arthrotomy using arthroscopy. In a second patient with suspected joint infection, the diagnosis was confirmed and treated through arthroscopy.
The removal of foreign bodies and entrapped cement using arthroscopic techniques has been previously reported after hip arthroplasty [9, 10, 13, 16]. In these cases, dislocations of hip implants in either the perioperative period or later resulted in entrapment of the implanted drain or fragmented cement debris, preventing successful closed reduction. Hip arthroscopy was used to clear the interposed material and enable closed reduction of the hip prosthesis. None of the patients in this series were treated for entrapped debris postdislocation; however, we were able to successfully remove migrated hardware using arthroscopic techniques in three cases.
We identified previously unrecognized component-related problems in two patients (metal corrosion in one patient and acetabular loosening in another). Both patients were subsequently treated with revision arthroplasty. In a previous report [3], arthroscopy was used to assess acetabular cup loosening in a patient with clinical and radiographic signs of massive polyethylene wear 3 years after THA. The polyethylene was broken into three pieces. Khanduja and Villar [6] recently described the use of hip arthroscopy to diagnose a loose acetabular component in a patient who presented with persistent pain after resurfacing hip arthroplasty and had a negative preoperative workup for infection and loosening.
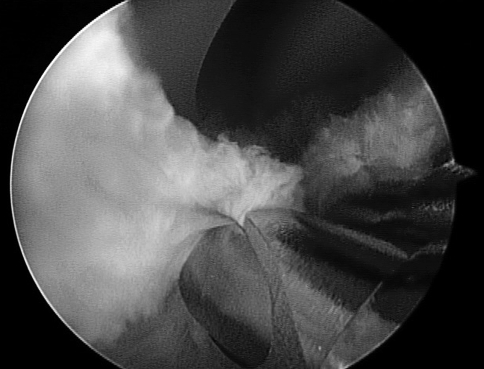
Three of the four patients in this study with impinging scar tissue experienced complete pain relief after débridement; an additional two patients out of four with nonimpinging scar tissue plus synovitis had complete resolution of their symptoms. One patient with adhesions and capsular scarring without impingement or synovitis had complete resolution of symptoms after arthroscopic débridement (Fig. 4). Although this has not been previously documented in arthroscopy post-THA, the literature supports arthroscopy after TKA for débridement of fibrous scar tissue causing painful, limited motion, patella clunk, and tethered patella syndrome [1, 5, 8, 11, 15, 17–19]. It is important to note, however, arthroscopy was least successful in this subgroup of patients with only five of nine patients achieving complete pain relief.
Fig. 4.
Case 15. Impinging soft tissue is visible during arthroscopic débridement.
Most problems after hip arthroplasty can be diagnosed by clinical examination (leg-length discrepancy, abductor weakness, etc.), plain radiography (component loosening, malposition, trochanteric nonunion, etc.), or special studies such as bone scan or aspiration arthrogram (subtle loosening or sepsis). Often, newer imaging modalities such as CT or MRI are of limited utility in these cases due to metal artifact that limits the ability to visualize peri- and intraarticular structures. In cases in which unexplained symptoms persist despite negative diagnostic evaluation, surgeons have been cautious to proceed to diagnostic open arthrotomy as a result of the prolonged recovery and associated risks of infection, instability, deep venous thrombosis, pulmonary embolism, muscle weakness, and nerve injury. In this situation, arthroscopy may be a useful diagnostic, and sometimes therapeutic, tool. The work up for patients in this series consisted of plain radiographs, aspiration arthrogram, and blood work consisting of complete blood count with differential, C-reactive protein, and sedimentation rate. Metal-reduction CT and MRI were not available for most of the patients in this study. One of the most recent patients did have a negative aspiration arthrogram spiral CT. Two of the patients with persistent groin pain had no relief from injecting the psoas sheath under ultrasound guidance with a cortisone derivative and long-lasting analgesic. Two patients had intraarticular analgesic injections without relief and four patients were referred for spine evaluation that failed to indicate lumbar pathology as a source of pain. In this series, arthroscopy effectively treated or directly led to effective treatment in eight of 12 cases presenting as diagnostic dilemmas. Arthroscopy also served as an effective therapeutic alternative in four cases with known postarthroplasty problems. Arthroscopy allowed for direct inspection of the joint and implants without the morbidity and risks associated with open arthrotomy. All cases were performed on an outpatient basis and the recovery period was substantially shorter than after open arthrotomy. Our indications for arthroscopy after THA continue to evolve. We are more inclined to perform arthroscopy in patients with identifiable loose bodies or signs and symptoms of impingement. Further prospective, controlled studies are needed to further define the role of arthroscopy in evaluating the painful hip arthroplasty.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bocell JR, Thorpe CD, Tullos HS. Arthroscopic treatment of symptomatic total knee arthroplasty. Clin Orthop Relat Res. 1991;271:125–134. [PubMed]
- 2.Bozic KJ, Rubash HE. The painful total hip replacement. Clin Orthop Relat Res. 2004;420:18–25. [DOI] [PubMed]
- 3.Fontana A, Zecca M, Sala C. Arthroscopic assessment of total hip replacement and polyethylene wear: a case report. Knee Surg Sports Traumatol Arthrosc. 2000;8:244–245. [DOI] [PubMed]
- 4.Hyman JL, Salvati EA, Laurencin CT, Rogers DE, Maynard M, Brause DB. The arthroscopic drainage, irrigation, and debridement of late, acute total hip arthroplasty infections: average 6-year follow-up. J Arthroplasty. 1999;14:903–910. [DOI] [PubMed]
- 5.Johnson DR, Friedman RJ, McGinty JB, Mason JL, St Mary EW. The role of arthroscopy in the problem total knee replacement. Arthroscopy. 1990;6:30–32. [DOI] [PubMed]
- 6.Khanduja V, Villar RN. The role of arthroscopy in resurfacing arthroplasty of the hip. Arthroscopy. 2008;24:122. [DOI] [PubMed]
- 7.Lawrence SJ, Kan RO. Arthroscopic lysis of adhesions after New Jersey LCS total knee arthroplasty. Orthopedics. 1992;15:943–944. [DOI] [PubMed]
- 8.Lucas TS, DeLuca PF, Nazarian DG, Bartolozzi AR, Booth RE Jr. Arthroscopic treatment of patellar clunk. Clin Orthop Relat Res. 1999;367:226–229. [DOI] [PubMed]
- 9.Luchetti WT, Copley LA, Vresilovic EJ, Black J, Steinberg ME. Drain entrapment and titanium to ceramic head deposition: two unique complications following closed reduction of a dislocated total hip arthroplasty. J Arthroplasty. 1998;13:713–717. [DOI] [PubMed]
- 10.Mah ET, Bradley CM. Arthroscopic removal of acrylic cement from unreduced hip prosthesis. Aust N Z J Surg. 1992;62:508–510. [DOI] [PubMed]
- 11.Markel DC, Luessenhop CP, Windsor RE, Sculco TA. Arthroscopic treatment of peripatellar fibrosis after total knee arthroplasty. J Arthroplasty. 1996;11:293–297. [DOI] [PubMed]
- 12.McCarthy JC, Busconi B. The role of hip arthroscopy in the diagnosis and treatment of hip disease. Orthopedics. 1995;18:753–756. [DOI] [PubMed]
- 13.Nordt W, Giangarra CE, Levy IM, Habermann ET. Arthroscopic removal of entrapped debris following dislocation of a total hip arthroplasty. Arthroscopy. 1987;3:196–198. [DOI] [PubMed]
- 14.Robbins GM, Masri BA, Garbuz DS, Duncan CP. Evaluation of pain in patients with apparently solidly fixed total hip arthroplasty components. J Am Acad Orthop Surg. 2002;10:86–94. [DOI] [PubMed]
- 15.Scranton PE Jr. Management of knee pain and stiffness after total knee arthroplasty. J Arthroplasty. 2001;16:428–435. [DOI] [PubMed]
- 16.Shifrin LZ, Reis ND. Arthroscopy of a dislocated hip replacement: a case report. Clin Orthop Relat Res. 1980;146:213–214. [PubMed]
- 17.Tzagarakis GP, Papagelopoulos PJ, Kaseta MA, Vlamis JA, Makestas MA, Nikolopoulos KE. The role of arthroscopic intervention for symptomatic total knee arthroplasty. Orthopedics. 2001;24:1090–1095; quiz 1096–1097. [DOI] [PubMed]
- 18.Vernace JV, Rothman RH, Booth RE Jr, Balderston RA. Arthroscopic management of the patellar clunk syndrome following posterior stabilized total knee arthroplasty. J Arthroplasty. 1989;4:179–182. [DOI] [PubMed]
- 19.Wasilewski SA, Frankl U. Arthroscopy of the painful dysfunctional total knee replacement. Arthroscopy. 1989;5:294–297. [DOI] [PubMed]
- 20.Wasilewski SA, Frankl U. Fracture of polyethylene of patellar component in total knee arthroplasty, diagnosed by arthroscopy. J Arthroplasty. 1989;4(Suppl):S19–S22. [DOI] [PubMed]