Abstract
Because of improvements in surgical technique, anesthesia, and rehabilitation, mortality after hip arthroplasty may be on the decline. The purpose of this study was to determine the 90-day mortality rate after uncemented total hip arthroplasty (THA) performed under regional anesthesia. We retrospectively reviewed 7478 consecutive patients undergoing cementless primary or revision THA between January 2000 and July 2006. Patient survivorship was established and causes of death were obtained by accessing the Social Security Death Index, Centers for Disease Control and Prevention National Death Index, and State Departments of Vital Statistics. There were two intraoperative deaths from cardiac arrest. The overall 30- and 90-day mortality rates were 0.24% (18 of 7478) and 0.55% (41 of 7478), respectively. Thirty-day mortality after primary THA was low at 0.13% (eight of 6272). The most common cause of death was cardiovascular-related. Mortality after modern THA seems to have remained very low despite the availability of this procedure to patients of all ages and comorbidities.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
For nearly 50 years, THA has been one of the most effective and economical interventions in orthopaedic surgery [5, 10, 19] having a perioperative mortality rate usually less than 1% [2, 3, 6, 8, 23, 26–29, 37]. Emerging demographic and epidemiologic studies are projecting large increases in the demand for primary and revision arthroplasty over the next two decades [14–16]. Furthermore, THA is being performed in patients who are older and infirm [1, 12, 13, 21, 22, 35, 38, 41].
Improvements in surgical and pain management techniques, such as the use of uncemented femoral components and multimodal anesthesia, improve outcome after THA [1, 7, 25, 30, 32]. Additionally, new rehabilitation regimens that are accelerated, aggressive, and continued in the outpatient setting have demonstrated improvement in patient outcome [17, 25, 39, 40]. The combination of improvements in surgical practices and advances in perioperative care has caused mortality from THA to decline.
The primary purpose of this study was to determine the overall early mortality rate within 90 days of surgery in a consecutive group of patients who underwent uncemented THA under regional anesthesia who were subjected to multimodal pain management and accelerated rehabilitation. Secondly, we wished to report differences in mortality rates between revision and primary surgeries. Lastly, we sought to report differences in mortality among different age groups undergoing THA.
Materials and Methods
From an institutional database we retrospectively identified and reviewed 7478 consecutive patients who underwent elective THA between January 2000 and July 2006. We excluded patients receiving partial joint replacements or nonarthroplasty procedures. Of the 7478 patients, 3589 were men with a mean age of 63 years (range, 13–93 years) and 3889 were women with a mean age of 63 years (range, 15–97 years). Primary arthroplasty was performed in 6272 patients, including 5749 unilateral and 523 bilateral procedures. Revision hip arthroplasty was performed in 1206 patients; of these, 1201 were unilateral and five were bilateral. We obtained prior Institutional Review Board approval.
All patients in this cohort were evaluated and cleared 3 to 6 weeks before surgery by an anesthesiologist and a cardiologist. We used hypotensive regional anesthesia for all patients unless contraindicated or unsuccessful to achieve. The conversion rate to general anesthesia at our institution is approximately 2%. Hip arthroplasty was carried out in a laminar flow room with all members of the surgical team wearing body exhaust suits during surgery. All operations were performed by or under the supervision of one fellowship-trained arthroplasty surgeon (JP, PFS, RHR). Hip arthroplasties were performed in a supine position through a modified anterolateral gluteus medius splitting approach using uncemented femoral and acetabular components. The latter was true for revision arthroplasty also.
All patients were subjected to early mobilization in the postoperative period. Multiple standardized protocols were closely followed for all patients. The prophylactic anticoagulation regimen was the same throughout the study period. This consisted of administration of warfarin on postoperative Day 1 and continuing for 6 weeks aiming for an international normalized ratio of 1.5 to 2. Unless contraindicated, patients also received 1000 units of intravenous heparin at the time of hip dislocation. Intravenous antibiotics, namely first-generation cephalosporin (or vancomycin for those with penicillin allergy), were administered preoperatively and for 24 hours after the surgery.
All patients were seen on the day of surgery or the first postoperative day and encouraged to sit out of bed and ambulate if possible. All patients undergoing primary arthroplasty were allowed to weight bear as tolerated after surgery. A protected weight bearing protocol was in place for some patients undergoing revision arthroplasty. Patients were seen twice daily by the physical therapy team and assisted ambulation was performed. After discharge, patients were followed up at 3 weeks, 3 months, 6 months, and 1 year postoperatively.
We performed a detailed review of the clinical records for all patients. Protected information of the study subjects was submitted to the Social Security Death Index to investigate patient survivorship through July 2007. We submitted subjects not matched in the Social Security Death Index database to the Centers for Disease Control and Prevention’s National Death Index to complete information regarding patient survivorship. Once patient death was established, the National Death Index was hired to perform a cause of death retrieval report for underlying and associated causes of death. Causes of death were coded using the International Classification of Diseases (ICD-10). In addition to the data report from the National Death Index, we sent applications and the list of subjects to State Departments of Vital Statistics to obtain copies of death certificates. Official cause of death was recorded from each death certificate and entered into the database along with postmortem information when performed. We compared data from the ICD-10 codes and the certificates of death. Lastly, a detailed chart review of mortalities occurring within 90 days was conducted using electronic records. We placed special emphasis on in-hospital deaths and all deaths occurring within 90 days, and compared the differences in mortality per age group after THA.
Results
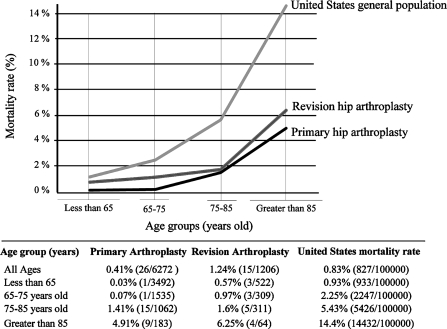
The overall mortality rate at 30 days after THA was 0.24% (18 of 7478). The vast majority of these deaths occurred in the hospital (13 of 18). The mortality rate at 90 days after index surgery was slightly higher at 0.55% (41 of 7478). When comparing primary and revision arthroplasty, primary hip arthroplasty was associated with the lowest 30-day mortality rate (0.13% [eight of 6272]) and 90-day mortality rate (0.41% [26 of 6272]). The perioperative mortality rate after revision arthroplasty was 0.83% (10 of 1206) and the 90-day mortality rate was 1.24% (15 of 1206). There were two intraoperative deaths from cardiac arrest, one during revision surgery and one during primary hip arthroplasty. The death rate after primary and revision THA was proportionally higher by age group (Fig. 1) [24]. Subjects less than 65 years old receiving primary elective THA had the lowest mortality of 0.03% (one of 3492), while those over 85 years old and receiving revision THA had the highest mortality of 6.25% (four of 64).
Fig. 1.
Age-matched death rates of the United States general population and patients undergoing total hip replacement are shown. The authors have not controlled for any other variables that influence mortality. All patients undergoing THA had preoperative screening prior to elective surgery.
Cardiovascular conditions were responsible for most deaths after THA. Cardiopulmonary arrest, acute coronary syndrome, stroke, pulmonary embolism, and arrhythmias were the listed causes of deaths (Table 1). Other causes of death included respiratory complications, malignancy, and sepsis.
Table 1.
Causes of death within 90 days after elective hip arthroplasty
| Etiology | Number of deaths |
|---|---|
| Cardiovascular | 23 |
| Acute coronary syndrome (8) | |
| Cardiopulmonary arrest (7*) | |
| Cerebrovascular accident (3) | |
| Pulmonary embolism (2) | |
| Ischemic colitis (2*) | |
| Ventricular tachyarrhythmia (1) | |
| Respiratory | 8 |
| Respiratory failure (5) | |
| Aspiration pneumonia (1) | |
| Pneumothorax (1) | |
| Pneumonia (1) | |
| Sepsis | 5 |
| Malignancy | 3 |
| Lung cancer (1) | |
| Cholangiocarcinoma (1) | |
| Malignant neoplasm unspecified (1) | |
| Other | 2 |
| Multiple organ failure (1) | |
| Unspecified (1) |
* Postmortem performed in one cardiopulmonary arrest case and one ischemic colitis case.
Discussion
The growing demand for THA [16] coupled with age and increase in comorbidities of patients undergoing the procedure [12, 13] warrants investigation of its current perioperative mortality rate. The primary focus of this paper was to determine overall mortality and causes of death at 30 and 90 days for patients undergoing THA. Secondly, we chose to compare mortality rates of primary and revision arthroplasty. Lastly, we compared mortality rates among different age groups within our study. With these goals in mind, we recognize this study has some limitations. First, few autopsies were performed, thus limiting the validity of the listed causes of death on certificates. Furthermore, we had to rely on ICD-10 codes and death certificates for cause of death information and it is possible that this information was not always accurate. Despite these limitations, we provided the most objective available causes of death, and the reported causes of death were consistent and accurate with information and data collected from our hospital records. Further, this is a relatively large study reporting early mortality for consecutive patients undergoing uncemented THA under regional anesthesia and modern pain management and rehabilitation in a single institution. Every effort was made to determine the status of each patient in this study, which included contacting national and state registries. Finally, all patients were subjected to nearly the same surgical, anesthesia, and rehabilitation protocols. The latter minimized the influence of a confounding variable such as anticoagulation protocols and the type of anesthesia.
Previous studies have reported very low (0.24% to 1%) [3, 19, 29, 37, 41] perioperative mortality for elective primary THA (Table 2). Our study supports these findings with two intraoperative deaths and overall mortality rates of 0.24% (18 of 7478) and 0.55% (41 of 7478) at 30 and 90 days, respectively. Consistent with other reports [3, 27, 33, 37], we also found the most common cause of death to be cardiovascular-related.
Table 2.
Early mortality after primary and revision THA
| Author (year of publication) | Number of hip arthroplasties | Study period | 30-day | 90-day |
|---|---|---|---|---|
| Present study | 7478 | 2000–2006 | 0.24 | 0.55 |
| Lie et al. (2002) [18] | 67,548 | 1987–1999 | 0.41 | 0.93 |
| Blom et al. (2006) [3] | 1727 | 1993–1996 | 0.41* | 1.00* |
| Parvizi et al. (2001) [29] | 30,714 | 1969–1997 | 0.29 | |
| Whittle et al. (1993) [41] | 5078 | 1983–1985 | 0.95 | |
| Coventry et al. (1974) [6] | 2012 | 1969–1973 | 0.4* |
* Included only primary hip arthroplasty surgery.
In addition to reaffirming the effectiveness and safety of THA, our study results suggest that modern advances in surgery, anesthesia, and rehabilitation have helped keep mortality as low as previously reported despite early hospital discharges, more aggressive rehab protocols, and operations being performed in patients who are older and more infirm. Several improvements in orthopaedic practice are responsible for the low reported mortality rate in this study. First, procedures were completed in a high-volume hospital by experienced surgeons specializing in total joint arthroplasty. A high hospital case load and surgeon experience lower perioperative mortality and in-hospital deaths [9, 34]. Second, improvements in anesthesia and pain management have reduced mortality and improve outcome after THA. The use of hypotensive, neuroaxial anesthesia has reduced mortality from cardiorespiratory complications [11, 20, 33]. Finally, the use of multimodal anesthesia and analgesia for perioperative care and pain management has shown improvement in functional outcome and accelerated patient discharge [1, 25], which may indirectly help lower mortality. Changes in surgical practices and implantable devices have also helped reduce mortality after THA. A previous study reported the use of uncemented components decreases intraoperative death resulting from prevention of bone cement implantation syndrome [32]. Furthermore, studies have demonstrated increased implant survivorship for noncemented devices [4, 7, 30, 32, 36]. Increased implant lifetime will decrease the need for reoperation and reduce the increased risk of mortality which accompanies revision surgery. In addition, efforts made to decrease intraoperative time have helped limit blood loss, infection, and intraoperative complications [37]. The prophylactic uses of first-generation cephalosporin antibiotics and low-dose Coumadin (warfarin, Bristol-Myers Squibb Company, Princeton, NJ) anticoagulation have reduced infection and cardiovascular-related causes of death. Additionally, it is of importance to note the low incidence of thromboembolic events resulting in death (two of 7478). We found our data regarding death from thromboembolism to be comparable to previous studies [3, 18]. Of note, our study used a lower INR than the currently published ACCP guideline. We find these data interesting and believe they warrant a more controlled study in the future.
When comparing rates of primary and revision arthroplasty and respective age groups, our data show that subjects less than 65 years old receiving primary elective THA had the lowest mortality of 0.03% (one of 3492), while those over 85 years old and receiving revision THA had the highest mortality of 6.25% (four of 64). These mortality rates are as low as those previously published [3, 19, 29, 37, 41]. In addition to aforementioned advances in surgical, anesthesia, and rehabilitation techniques, rigorous preoperative screening and identification of high-risk patients for complications, especially cardiovascular complications and near-fatal arrhythmias, are extremely important and have been fundamental in reducing mortality after THA at our institution [31]. Advances in rehabilitation strategies have recently received more attention and may help to reduce complications and perioperative mortality after THA. Aggressive postoperative rehabilitation strategies and home exercise rehabilitation improve short-term outcome after surgery by improving the patient’s functional status and preventing complications such as dislocation [17, 39, 40]. Although decreases in mortality have not been directly attributed to rehabilitation strategies, it is certain they help improve patient outcome and function and thus influence outcome after THA. More studies are needed to establish their relationship and benefit.
Our data support the fact that hip arthroplasty performed using modern techniques appears extremely safe; yet, despite rigorous screening methods, deaths still occur. Shorter lengths of hospital stay make prevention of postoperative complications increasingly difficult to prevent. Also, the preponderance of cardiovascular-related deaths is reason to place more emphasis on preoperative screening and postoperative monitoring of high-risk patients to prevent cardiovascular complications and related deaths in the future. Further reductions in mortality will be attributed to our ability to identify, manage, and treat patients with risk factors for cardiovascular complications. As THA is performed more frequently in older and sicker patients, it is important we continue to monitor its associated mortality.
Acknowledgments
We thank the Pennsylvania Department of Health & Vital Statistics and National Death Index.
Footnotes
One or more of the authors (JP, PFS, and RHR) are consultants for Stryker Orthopedics. No funding was used for this research.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was not required for the study.
References
- 1.Andersen LJ, Poulsen T, Krogh B, Nielsen T. Postoperative analgesia in total hip arthroplasty: a randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop. 2007;78:187–192. [DOI] [PubMed]
- 2.Barrett J, Losina E, Baron JA, Mahomed NN, Wright J, Katz JN. Survival following total hip replacement. J Bone Joint Surg Am. 2005;87:1965–1971. [DOI] [PubMed]
- 3.Blom A, Pattison G, Whitehouse S, Taylor A, Bannister G. Early death following primary total hip arthroplasty: 1727 procedures with mechanical thrombo-prophylaxis. Acta Orthop. 2006;77:347–350. [DOI] [PubMed]
- 4.Burke WV, Orishimo KF, McAuley JP, Engh CA. Midterm radiographic comparison of cementless acetabular shells containing lateralized and nonlateralized liners. J Arthroplasty. 2006;21:1099–1104. [DOI] [PubMed]
- 5.Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275:858–865. [DOI] [PubMed]
- 6.Coventry MB, Beckenbaugh RD, Nolan DR, Ilstrup DM. 2,012 total hip arthroplasties. A study of postoperative course and early complications. J Bone Joint Surg Am. 1974;56:273–284. [PubMed]
- 7.Danesh-Clough T, Bourne RB, Rorabeck CH, McCalden R. The mid-term results of a dual offset uncemented stem for total hip arthroplasty. J Arthroplasty. 2007;22:195–203. [DOI] [PubMed]
- 8.Dearborn JT, Harris WH. Postoperative mortality after total hip arthroplasty. An analysis of deaths after two thousand seven hundred and thirty-six procedures. J Bone Joint Surg Am. 1998;80:1291–1294. [DOI] [PubMed]
- 9.Doro C, Dimick J, Wainess R, Upchurch G, Urquhart A. Hospital volume and inpatient mortality outcomes of total hip arthroplasty in the United States. J Arthroplasty. 2006;21:10–16. [DOI] [PubMed]
- 10.Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand. 2000;71:337–353. [DOI] [PubMed]
- 11.Keith I. Anaesthesia and blood loss in total hip replacement. Anaesthesia. 1977;32:444–450. [DOI] [PubMed]
- 12.Kreder HJ, Berry GK, McMurtry IA, Halman SI. Arthroplasty in the octogenarian: quantifying the risks. J Arthroplasty. 2005;20:289–293. [DOI] [PubMed]
- 13.Krishnan E, Fries JF, Kwoh CK. Primary knee and hip arthroplasty among nonagenarians and centenarians in the United States. Arthritis Rheum. 2007;57:1038–1042. [DOI] [PubMed]
- 14.Kurtz S, Lau E, Halpern M, Ong K. Trend shows growing orthopedic surgery case load. Will surgeons be able to keep up? Mater Manag Health Care. 2006;15:61–62. [PubMed]
- 15.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. [DOI] [PubMed]
- 16.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. [DOI] [PubMed]
- 17.Levine B, Kaplanek B, Scafura D, Jaffe WL. Rehabilitation after total hip and knee arthroplasty: a new regimen using Pilates training. Bull NYU Hosp Jt Dis. 2007;65:120–125. [PubMed]
- 18.Lie SA, Engesaeter LB, Havelin LI, Furnes O, Vollset SE. Early postoperative mortality after 67,548 total hip replacements: causes of death and thromboprophylaxis in 68 hospitals in Norway from 1987 to 1999. Acta Orthop Scand. 2002;73:392–399. [DOI] [PubMed]
- 19.Lie SA, Engesaeter LB, Havelin LI, Gjessing HK, Vollset SE. Mortality after total hip replacement: 0–10-year follow-up of 39,543 patients in the Norwegian Arthroplasty Register. Acta Orthop Scand. 2000;71:19–27. [DOI] [PubMed]
- 20.Lieberman JR, Huo MM, Hanway J, Salvati EA, Sculco TP, Sharrock NE. The prevalence of deep venous thrombosis after total hip arthroplasty with hypotensive epidural anesthesia. J Bone Joint Surg Am. 1994;76:341–348. [DOI] [PubMed]
- 21.Lubbeke A, Katz JN, Perneger TV, Hoffmeyer P. Primary and revision hip arthroplasty: 5-year outcomes and influence of age and comorbidity. J Rheumatol. 2007;34:394–400. [PubMed]
- 22.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85:27–32. [DOI] [PubMed]
- 23.Miller KA, Callaghan JJ, Goetz DD, Johnston RC. Early postoperative mortality following total hip arthroplasty in a community setting: a single surgeon experience. Iowa Orthop J. 2003;23:36–42. [PMC free article] [PubMed]
- 24.Miniño AM, Heron MP, Murphy SL, Kochankek KD. Deaths: Final Data for 2004. Natl Vital Stat Rep. 2007;55:1–119. [PubMed]
- 25.Nuelle DG, Mann K. Minimal incision protocols for anesthesia, pain management, and physical therapy with standard incisions in hip and knee arthroplasties: the effect on early outcomes. J Arthroplasty. 2007;22:20–25. [DOI] [PubMed]
- 26.Nunley RM, Lachiewicz PF. Mortality after total hip and knee arthroplasty in a medium-volume university practice. J Arthroplasty. 2003;18:278–285. [DOI] [PubMed]
- 27.Paavolainen P, Pukkala E, Pulkkinen P, Visuri T. Causes of death after total hip arthroplasty: a nationwide cohort study with 24,638 patients. J Arthroplasty. 2002;17:274–281. [DOI] [PubMed]
- 28.Parvizi J, Ereth MH, Lewallen DG. Thirty-day mortality following hip arthroplasty for acute fracture. J Bone Joint Surg Am. 2004;86:1983–1988. [DOI] [PubMed]
- 29.Parvizi J, Johnson BG, Rowland C, Ereth MH, Lewallen DG. Thirty-day mortality after elective total hip arthroplasty. J Bone Joint Surg Am. 2001;83:1524–1528. [DOI] [PubMed]
- 30.Parvizi J, Keisu KS, Hozack WJ, Sharkey PF, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component: a long-term study of the Taperloc stem. J Arthroplasty. 2004;19:151–156. [DOI] [PubMed]
- 31.Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: When do fatal or near-fatal complications occur? J Bone Joint Surg Am. 2007;89:27–32. [DOI] [PubMed]
- 32.Parvizi J, Sullivan T, Duffy G, Cabanela ME. Fifteen-year clinical survivorship of Harris-Galante total hip arthroplasty. J Arthroplasty. 2004;19:672–677. [DOI] [PubMed]
- 33.Sharrock NE, Cazan MG, Hargett MJ, Williams-Russo P, Wilson PD Jr. Changes in mortality after total hip and knee arthroplasty over a ten-year period. Anesth Analg. 1995;80:242–248. [DOI] [PubMed]
- 34.Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res. 2007;457:35–41. [DOI] [PubMed]
- 35.Sturmer T, Gunther KP, Brenner H. Obesity, overweight and patterns of osteoarthritis: the Ulm Osteoarthritis Study. J Clin Epidemiol. 2000;53:307–313. [DOI] [PubMed]
- 36.Surdam JW, Archibeck MJ, Schultz SC Jr, Junick DW, White RE Jr. A second-generation cementless total hip arthroplasty mean 9-year results. J Arthroplasty. 2007;22:204–209. [DOI] [PubMed]
- 37.Tarity TD, Herz AL, Parvizi J, Rothman RH. Ninety-day mortality after hip arthroplasty: a comparison between unilateral and simultaneous bilateral procedures. J Arthroplasty. 2006;21:60–64. [DOI] [PubMed]
- 38.Tuominen U, Blom M, Hirvonen J, Seitsalo S, Lehto M, Paavolainen P, Hietanieni K, Rissanen P, Sintonen H. The effect of co-morbidities on health-related quality of life in patients placed on the waiting list for total joint replacement. Health Qual Life Outcomes. 2007;5:16. [DOI] [PMC free article] [PubMed]
- 39.Unlu E, Eksioglu E, Aydog E, Aydog ST, Atay G. The effect of exercise on hip muscle strength, gait speed and cadence in patients with total hip arthroplasty: a randomized controlled study. Clin Rehabil. 2007;21:706–711. [DOI] [PubMed]
- 40.Walker WC, Keyser-Marcus LA, Cifu DX, Chaudhri M. Inpatient interdisciplinary rehabilitation after total hip arthroplasty surgery: a comparison of revision and primary total hip arthroplasty. Arch Phys Med Rehabil. 2001;82:129–133. [DOI] [PubMed]
- 41.Whittle J, Steinberg EP, Anderson GF, Herbert R, Hochberg MC. Mortality after elective total hip arthroplasty in elderly Americans. Age, gender, and indication for surgery predict survival. Clin Orthop Relat Res. 1993;295:119–126. [PubMed]