Abstract
This Classic article is a reprint of the original work by R. Merle d’Aubigné and M. Postel, Functional Results of Hip Arthroplasty with Acrylic Prosthesis. An accompanying biographical sketch on R. Merle d’Aubigné, MD, is available at DOI 10.1007/s11999-008-0571-2. The Classic Article is ©1954 by the Journal of Bone and Joint Surgery, Inc. and is reprinted with permission from Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;35:451--475.
Six hundred and twenty-one arthroplasties of the hip have been performed since the beginning of 1948 in the Clinique chirurgicale orthopédique et réparatrice of the Hôpital Cochin and in our private practice (Table 1).
Table 1.
Hip arthroplasties
| Trauma | 131 |
| Osteo-arthritis | 264 |
| Congenital subluxation | 104 |
| Congenital luxation | 66 |
| Rheumatoid arthritis | 14 |
| Spondylitis ankylosans | 26 |
| Miscellaneous | 16 |
| Total | 621 |
Careful follow-up has enabled us to determine the functional result in the great majority of our patients (243): of the 340 patients operated upon for osteo-arthritis, trauma, or congenital subluxations of the hip from six months to five years previously, six died (three from postoperative embolisms and three from intercurrent disease later) and eleven were lost to follow-up. All of the other patients have been reviewed at four months, at six months, and at one year after the operation. Thereafter, the patients have been examined once a year.
Technique
From 1947 to 1948, the technique advised by Smith-Petersen was used as exactly as possible. In a certain number of patients, however, in whom extensive excision of the femoral head was necessary, we inserted the Judet acrylic prosthesis through the anterior approach.
As the early results in patients in whom acrylic femoral-head prostheses had been inserted were slightly better than the results in those in whom Vitallium cups had been used, we progressively came to prefer, during the year 1948, the use of the acrylic prosthesis. We used Hueter’s anterior approach, a conservative excision of the head, and reaming of the acetabulum in order to make it fit the acrylic head exactly. In patients with osteo-arthritis, we always resected the capsule.
The prosthesis used was a slightly modified Judet prosthesis. There was a longer and stronger sleeve at the base of the head. This was exactly fitted around the neck stump which had been shaped by means of a special instrument. It was hoped that this exact fitting would prevent fracture of the stem; this proved after some time to be unfounded, for in patients in whom bone absorption occurred at the end of the neck stump the sleeve became loose. Thus, after having observed several fractures of the stem, we began to use a Judet prosthesis with a steel re-enforcement.
At the beginning of 1949, a review of the results in our patients showed 25 to 30 percent. of the results to be fair or poor. A careful study of these suggested that most of the partial or complete failures were due to the inadequate mechanical conditions of the new joint.
The following points appeared to be particularly important:
The conservation or restoration by the prosthesis of the normal length of the femoral neck (Figs. 1A through 2C).
- The correction of anteversion, which was achieved in three ways:
- By the oblique insertion of the prosthesis. A moderate anteversion can be corrected by inserting the prosthesis in a plane more nearly frontal than that of the neck (Fig. 3).
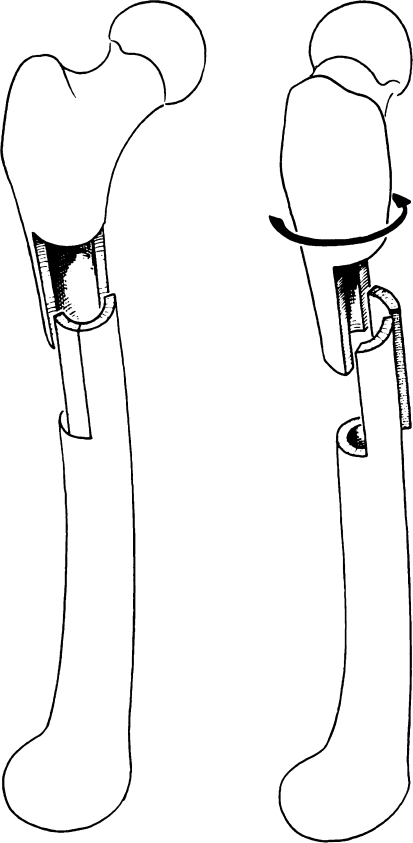
- By derotation osteotomy of the diaphysis. In six cases, strong anteversion was corrected by a step-shaped osteotomy performed around an intramedullary nail. This was done in the same stage as the arthroplasty. The crossing of the nail and of the prosthetic stem is a delicate step of the operation (Figs. 4, 5A–B).
- By the insertion of the cervico-capital prosthesis. We now prefer to correct strong anteversion by the insertion in the corrected direction of our cervico-capital prosthesis (Fig. 6A–B).
Proper fitting of the acetabulum to the prosthetic head: This was difficult to do in congenital conditions. The necessity of obtaining a good exposure of the posterior and inferior parts of the acetabulum, as well as of the anterior part, appeared evident.
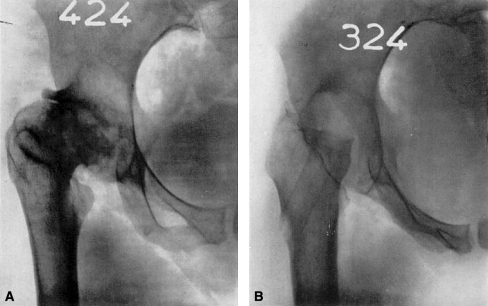
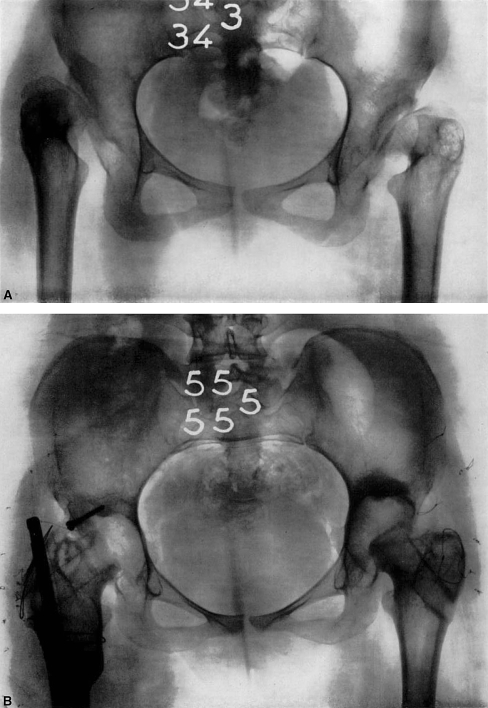
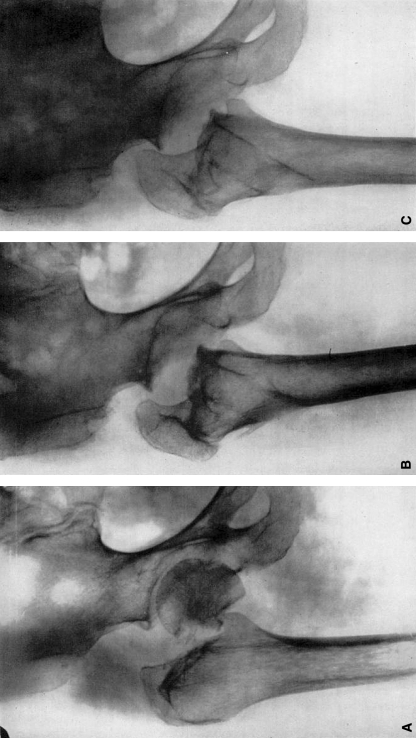
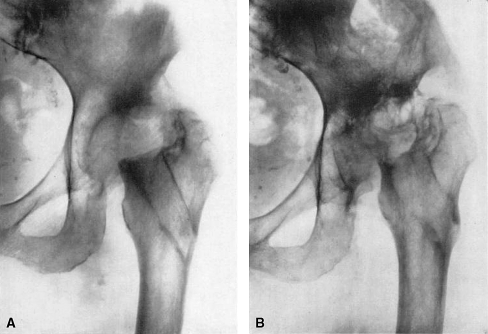
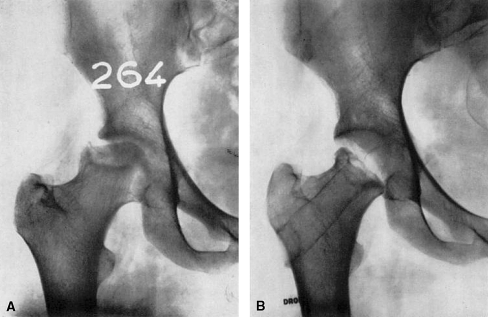
Fig. 1A–B .
(A) Congenital subluxation with osteo-arthritis. (B) Fourteen months after arthroplasty. Very bad result. The neck is too short, and anteversion has not been corrected. This patient was subjected to an arthrodesis.
Fig. 2A–C.
(A) Congenital subluxation with osteo-arthritis. (B) Arthroplasty with correction of anteversion by the oblique insertion of the prosthesis. The full length of the neck has been restored. Very good result at ten months. (C) Twenty-one months postoperatively. Slight recurrence of pain. Roentgenogram shows beginning bone resorption around the prosthesis.
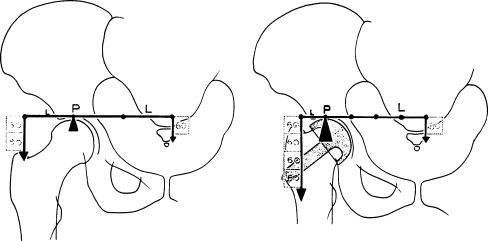
Fig. 3.
Correction of anteversion by the oblique insertion of the prosthesis.
Fig. 4.
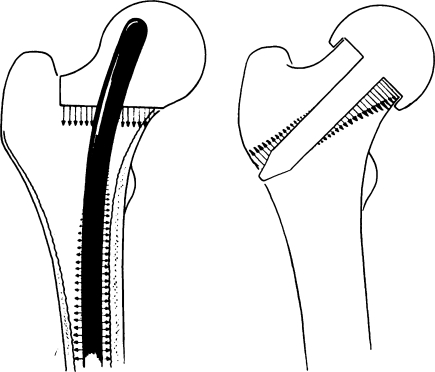
Correction of anteversion by osteotomy. An intramedullary nail is inserted. The femur is cut and is rotated around the nail. The crossing of the nail and of the stem of the prosthesis makes this technique difficult. Insertion of a cervico-capital prosthesis is preferable.
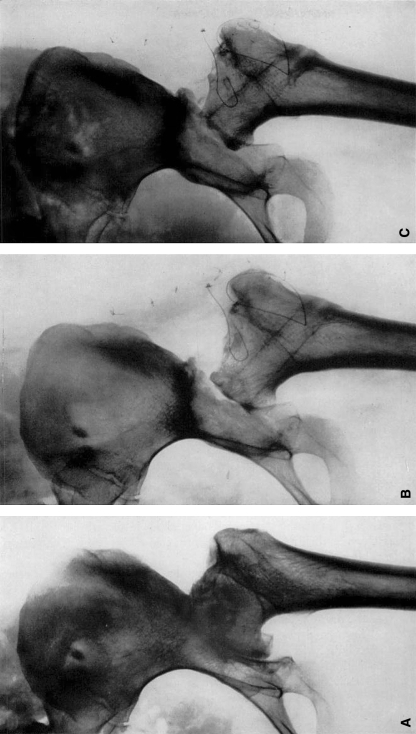
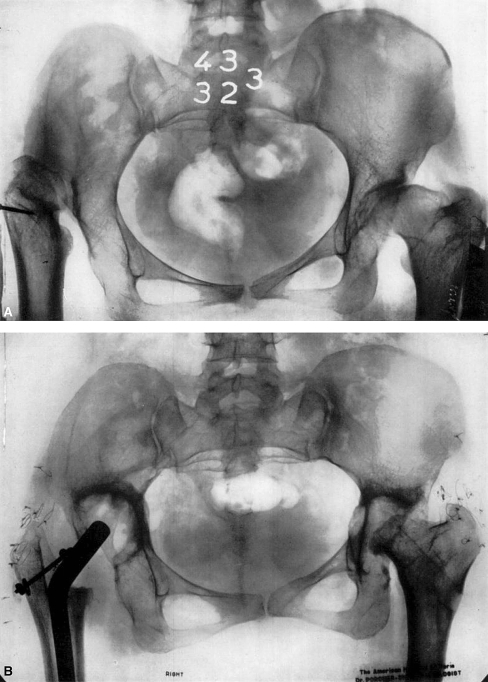
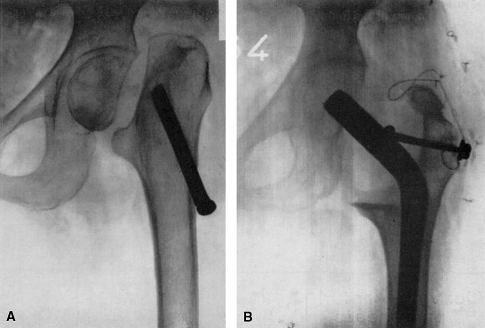
Fig. 5A–B.
Bilateral congenital dislocation. In the right hip, anteversion of 80 degrees has been corrected by derotation osteotomy during the arthroplasty. Very good result. In the left hip, anteversion has been corrected by the oblique insertion of the prosthesis. Very good result after two years.
Fig. 6A–B.
Congenital dislocation of the right hip had been previously operated upon with a poor result. Arthrop1asty with the cervico-capital prosthesis and correction of the anteversion brought about a good result. In the left hip residual subluxation was corrected by arthroplasty in which a Judet prosthesis was used. Very good result.
From 1949 to the end of 1952, our technique was modified as follows:
Gibson’s posterolateral approach was used in all patients in order to obtain a good exposure of all parts of the acetabulum and to enable a thorough evaluation and correction of anteversion.
The normal length of the femoral neck was conserved whenever possible. The normal length of the femoral neck was restored by the insertion of the cervico-capital prosthesis when the neck had been absorbed or was congenitally short or had had to be resected for a pathological condition.
The prosthetic head was exactly fitted to the acetabulum.
More recently, at the end of 1952, a review of late results showed that there was late functional deterioration among formerly good or fair results in 15 per cent.
Deterioration appeared to be caused by bone absorption around the prosthesis. Believing that absorption is due to a too great pressure of the stem of the Judet prosthesis on the wall of the cervical canal, we have been brought to use our cervico-capital prosthesis with a long intramedullary stem (Fig. 7) even in patients in whom the shortness of the neck did not make it necessary, at least in relatively young patients.
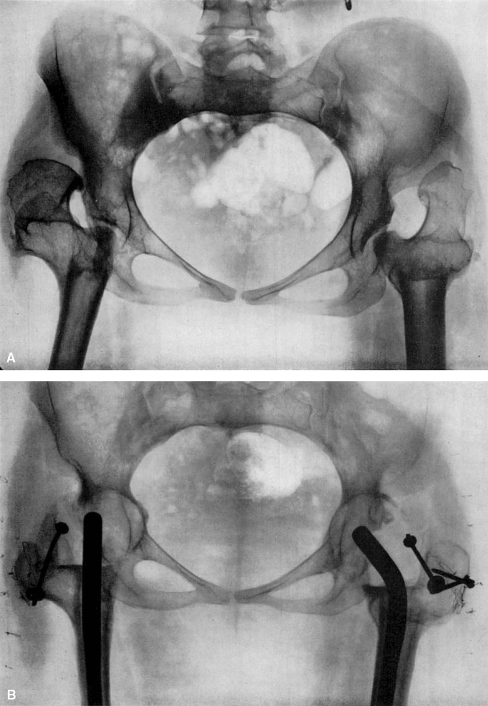
Fig. 8A–B.
Bilateral congenital dislocation previously treated by osteotomy. There was severe pain and a permanent abduction deformity. Arthroplasty was performed on both sides with the insertion of the cervico-capital prosthesis. Very good result after six months.
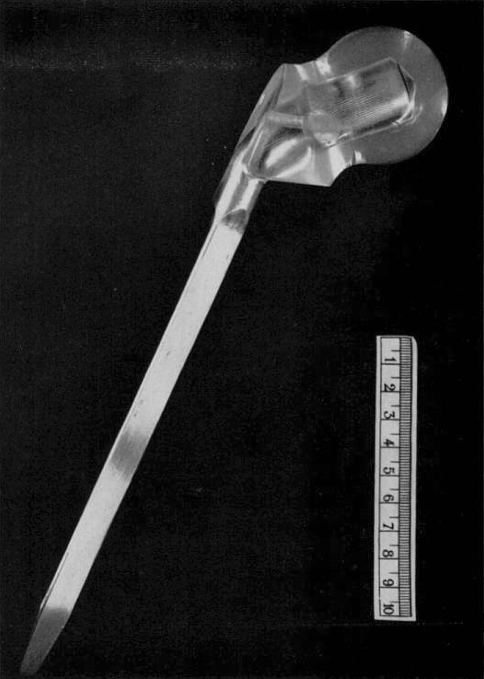
Fig. 7.
The cervico-capital prosthesis (modified from that of J. Gosset) with the long intramedullary stem and flat weight-bearing surface.
Present Technique
Approach: We use in all cases Gibson’s excellent posterolateral approach which consists in a slightly posteriorly curved incision, fifteen centimeters long, on the lateral aspect of the trochanter through the skin and fascia lata, together with the section of the glutaeus medius tendon around the trochanter and section of the glutaeus minimus tendon.
A T-shaped opening of the capsule is made along its iliac insertion in patients with trauma, while excision of the capsule is done in patients with osteo-arthritis.
The hip is dislocated.
Acetabulum: Nothing is done to the acetabulum when it is sound in patients with trauma to the hip. In patients with osteo-arthritis, conservative excision, with careful removal of bone formations at the inferior and posterior borders, is performed. The acetabulum is carefully reamed to make it spherical and to make it fit the prosthetic head exactly. In patients with congenital subluxations, a new acetabulum has to be created in the posterior and inferior part of the shallow cavity. In patients with high congenital disclocations, the acetabulum is made in the normal place or slightly higher.
Femoral head and neck: In old patients with a sound and normally anteverted femoral neck, we still use the Judet prosthesis (with steel re-enforcement) which has been modified by being made with a strong, long sleeve and which is exactly fitted by means of a special instrument. In all other patients, we use the cervico-capital prosthesis with an intramedullary stem. In these patients, the femoral neck may have been absorbed (non-union) or the neck may be strongly anteverted, congenitally short, or involved in a pathological condition. The cervico-capital prosthesis is used in all patients under sixty. The neck is resected in two planes: one vertical and sagittal between the trochanter and the base of the neck and the other horizontal just above the lesser trochanter. The medullary canal is opened, and, if necessary, it is widened to permit the insertion of the big steel stem of the prosthesis. The prosthesis is hammered in. The bone sections, however, are made to conform exactly to the prosthesis before it is hammered into place.
Finally reduction of the prosthesis into the acetabulum and suture of the tendons and fascia lata with steel wire are done.
Prosthesis
Our cervico-capital prosthesis is made of acrylic with the head and neck cut at its inferolateral end by two flat surfaces meeting at right angles. The vertical surface must be adjusted to the medial aspect of the trochanter, and the inferior surface must rest on the base of the neck immediately superior to the lesser trochanter. A strong steel stem, twenty-five centimeters long, which is inserted into the plastic material goes down into the medullary canal. It is cylindrical at its superior third, triangular in its medial part, and flat at its inferior third in order to conform to the posterior curve of the shaft.
We began to use this prosthesis at the beginning of 1951, and we have used it in sixty-five cases. The results to the present have been satisfactory. Three criticisms of its use can be made:
As with all acrylic prostheses the wearing-out of the material is to be feared;
Its insertion demands the complete excision of the femoral neck;
It is necessary to fit the individual patient with the proper sized prosthesis, and in some cases the prosthesis has had to be especially made after accurate measurements on the roentgenograms had been taken.
For these reasons, we are now working on a prosthesis of the same shape but made of stainless steel. This prosthesis will allow its length to be adjusted.
Results
In this paper only the results of arthroplasty with the insertion of an acrylic prosthesis in traumatic and degenerative conditions, as well as subluxatious, will be reviewed.
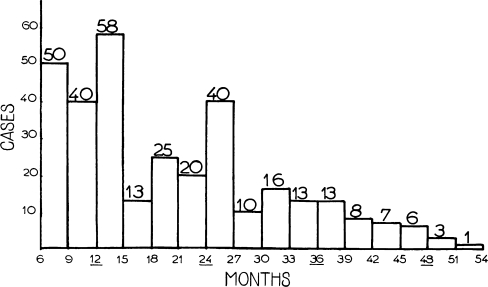
Four hundred and five patients have been subjected to arthroplasty. Six died within the first year and eleven were lost to follow-up. The duration of follow-up for 323 patients is shown in Table 2 and Chart 1.
Table 2.
Hip arthroplasties with acrylic prosthesis follow-up (Trauma to hip. Osteo-arthritis, and subluxations)
| Total no. of patients | 405 | |
| No. of patients operated upon Jan. 1948 to Nov. 1952 | 340 | |
| No. of patients operated upon in subsequent six months | 65 | |
| Deaths | 6 | |
| Postoperative | 3 | |
| From intercurrent disease in first year | 3 | |
| Lost to follow-up | 11 | |
| Followed-up (not including patients operated upon in last six months) | 323 | |
| Less than one year | 90 | |
| One to two years | 116 | |
| Two to three years | 79 | |
| Three to four years | 34 | |
| Four years or more | 4 |
Chart 1.
Follow-up. (Reproduced by permission from Mémoires de l’Académie de Chirurgie, 79: 461, 1953.)
Early results at the end of the first postoperative year are available in 225 cases.
Late results from one and a half years to four and a half years after the operation are available in 153 patients. The shortest period of follow-up for these patients is eighteen months and the longest is fifty-four months, the average being twenty-nine months.
To ensure an objective appreciation of the results, we have used the method of grading shown in Table 3.
Table 3.
Method of grading functional value of hip*
| Pain | Mobility | Ability to walk | |
|---|---|---|---|
| 0 | Pain is intense and permanent. | Ankylosis with bad position of the hip. | None. |
| 1 | Pain is severe even at night. | No movement: pain or slight deformity. | Only with crutches. |
| 2 | Pain is severe when walking; prevents any activity. | Flexion under 40 degrees. | Only with canes. |
| 3 | Pain is tolerable with limited activity. | Flexion between 40 and (60) degrees. | With one cane, less than one hour; very difficult without a cane. |
| 4 | Pain is mild when walking: it disappears with rest. | Flexion between 60 and 80 degrees; patient can reach his foot. | A long time with a cane; short time without cane and with limp. |
| 5 | Pain is mild and inconstant: normal activity. | Flexion between 80 and 90 degrees: abduction of at least 15 degrees. | Without cane but with slight limp. |
| 6 | No pain. | Flexion of more than 90 degrees; abduction to 30 degrees. | Normal. |
* Adapted from Tableau 1, Revue d’Orthopédie, 35: 542, 1949.
The results are classified in two ways: absolute results (the evaluation of the functional value of the hip after the operation) (Table 4) and relative results (the appreciation of the difference between the preoperative and the postoperative functional states, in other words, the functional benefit brought to the patient by the operation) (Table 5).
Table 4.
Functional grading of the hip
| Pain | Ability to walk | Mobility normal or nearly normal | |
|---|---|---|---|
| Very good | P + W = 11 or 12 | ||
| 6 | 6 | Walk without cane, with no pain and no limp. | |
| 6 | 5 | Walk without cane, with no pain but with slight limp. | |
| 5 | 6 | Walk without cane, with no limp but with slight pain when starting. | |
| Good | P + W = 10 | ||
| 5 | 5 | Walk without cane, with slight pain and slight limp. | |
| 4 | 6 | Walk without cane, with pain but no limp. | |
| 6 | 4 | Walk without cane, without pain: a cane used to go outdoors. | |
| Medium | P + W = 9 | ||
| 5 | 4 | Slight pain: a cane is used outdoors. | |
| 4 | 5 | Pain after walking some minutes; no cane is used but there is a slight limp. | |
| 6 | 3 | No pain: a cane is used all the time. | |
| Fair | P + W = 8 | ||
| 5 | 3 | Slight pain; a cane is used all the time. | |
| 4 | 4 | Pain after walking: a cane is used outdoors. | |
| Poor | P + W = 7 or less | ||
| Mobility Reduced | |||
| If the mobility is reduced to 4, the result is classed one grade lower. | |||
| If the mobility is reduced to 3 or less, the result is classed two grades lower. | |||
Table 5.
Method of the evaluation of improvement brought about by operation in affections of the hip (relative result)
| Preoperative grading | Postoperative grading | Difference | Improvement | |
|---|---|---|---|---|
| Pain | 3 | 5 | 2 × 2 = 4 | =9 |
| Mobility | 2 | 5 | 3 = 3 | |
| Ability to walk | 3 | 4 | 1 × 2 = 2 | |
| Very great improvement = 12 or more | ||||
| Great improvement = 7 to 11 | ||||
| Fair improvement = 3 to 7 | ||||
| Failure = less than 3 | ||||
For function of the hip, painlessness and ability to walk are much more important than mobility. For this reason, the first and last numbers are multiplied by two. In this way the grading may be used to compare the results of arthroplasty with those of arthrodesis. For example, a successful arthrodesis in a patient who had a painful congenital dislocation will give:
| Preoperatire | Postoperatire | Difference | ||
|---|---|---|---|---|
| Pain | 2 | 6 | 4 × 2 = 8 | = 8 good result |
| Mobility | 5 | 1 | −4 | |
| Ability to walk | 3 | 5 | 2 × 2 = 4 | |
In a similar case, partial success of the arthroplasty would give:
| Preoperative | Postoperative | Difference | ||
|---|---|---|---|---|
| Pain | 2 | 4 | 2 × 2 = 4 | = 7 fair result |
| Mobility | 6 | 5 | −1 | |
| Ability to walk | 3 | 5 | 2 × 2 = 4 | |
Early Results
Traumatic Cases
Early results of arthroplasty in patients with trauma to the hip best teach us the mechanical conditions which must be fulfilled by the prosthesis in order to provide good balance of the hip.
Since the end of 1948, we have used Judet’s acrylic prosthetic head in the treatment of non-union of the femoral neck and of necrosis of the femoral head after fracture or traumatic dislocation. During the first two years, we used an anterior approach (either Smith-Petersen’s or Hueter’s). In the last two years, we used Gibson’s posterolateral approach.
Of seventy-six cases, sixty-four have been followed for one year or more. The results are as follows: in 43 per cent. the results were good or very good, in 22 per cent. they were fair, and in 34 per cent. they were poor.
A study of the poor results revealed that these were brought about by the operation, postoperative accidents, or shortness of the stump of the femoral neck.
Accidents were of three types:
Fracture: Three cases of fracture of the femoral shaft or of the upper extremity occurred during the operation when the anterior approach was used; none occurred during operation when the posterior approach was used.
Fracture of the prosthesis: Three cases of fracture of the prosthesis occurred with the first type; none have occurred with the use of the new type.
Dislocation: Ten postoperative dislocations occurred in sixty operations during the first two years. Six of these were reduced by manipulation and four required open operation. The femoral head remained stable in only two, and dislocation recurred in all others. In the majority, the results were poor; some, however, were fair.
Dislocation is evidently due to the shortness of the femoral neck and not to the removal of the capsule, for:
We always preserve the capsule in cases of trauma;
Since 1951, thanks to preservation or restoration of the normal length of the neck, dislocation has occurred in only two cases of sixty-seven (both of these were satisfactorily reduced by manipulation and the reduction was maintained);
Four cases of dislocation have been re-operated upon and a cervico-capital prosthesis has been inserted with very good results.
Shortness of the femoral neck is also responsible for the persistence of pain or for bad balance when no dislocation is present. If the head presses on the lateral part of the roof of the acetabulum and not on the surface, pain is always observed (Fig. 9A–C).
Fig. 9A–C.
(A) Non-union of the femoral neck with absorption of the neck stump. (B) Arthroplasty was done with a Judet head. (C) Three years postoperatively, the prosthesis became loose. The head pressed on the lateral part of the roof of the acetabulum. Roentgenogram shows sclerosis and the formation of a cyst. Very bad result.
Even when the head is in the center of the cavity, the shortness of the neck lever may cause pain or bad balance because, according to Pauwels, of the extra weight imposed on the joint (Fig. 10).
Fig. 10.
As shown by Pauwels, pressure on the femoral head is equal to the sum of the weight of the superior part of the body and of the force of the abductor muscles necessary to stabilize the pelvis. If the length of the femoral head is normal, the pressure is three times the weight of the body; if the neck is short, the pressure may be five or six times that weight. (Reproduced by permission from Revue de Chirurgie, 71: 284, 1952.)
Comparison of postoperative results in the patients with normal femoral necks with those in patients with absorbed neck stumps makes quite evident the necessity for the restoration of normal length of the neck.
When the neck is short, 78 per cent. of the results are fair or poor and 22 per cent. are good (Fig. 11A–B). When the neck is long, 28 per cent. of the results are fair or poor and 72 per cent. are good (Chart 2).
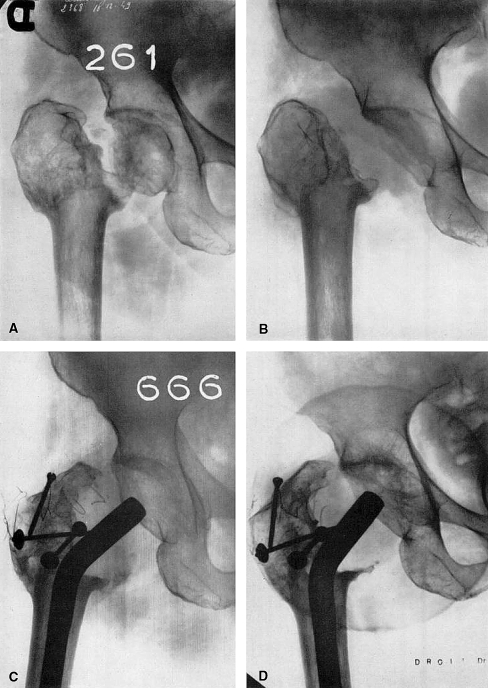
Fig. 11A–D.
(A) Ununited fracture of the neck of the femur previously treated by osteotomy. There was absorption of the neck. (B) An unsuccessful attempt at arthroplasty with the use of a Judet prosthesis. (C) One year after the insertion of the cervico-capital prosthesis. (D) Three years postoperatively. Roentgenogram shows slight absorption of bone under the prosthesis, but there is no looseness. The good result has been maintained.
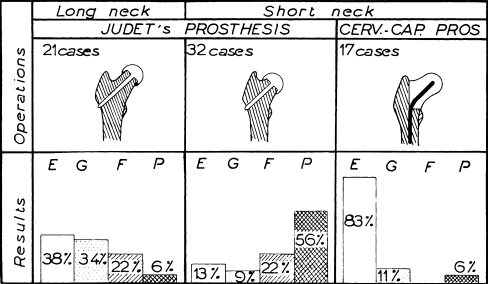
Chart 2.
Early results from the use of hip prostheses in treatment of non-union of the femoral neck and aseptic necrosis are compared. E, excellent; G, good: F, fair: and P, poor.
Since 1951, we have always used our cervico-capital prosthesis in patients with short neck stumps (Fig. 12A–B). The results are shown in Chart 2.
Fig. 12A–B.
(A) Ununited fracture of the femoral neck in a patient seventy-five years old. Roentgenogram shows absorption of the neck stump. (B) Two years after the insertion of the cervico-capital prosthesis. Roentgenogram shows no bone absorption. Good result maintained. Patient uses one cane.
In patients in whom the neck is nearly normal, about two thirds of the results are good with the use of the Judet head; however, when the neck has been absorbed, the proportion of good results is reversed. In the patients with an absorbed neck stump, the insertion of a cervico-capital prosthesis gave a high proportion of excellent results.
We think our figures undoubtedly show the superiority of the results gained from the use of a prosthesis which restores the normal mechanics of the hip.
Non-Traumatic Cases
The early results of arthroplasty in osteo-arthritis, either essential or secondary to congenital subluxation, show the important influence of technique. In these cases, however, the influence of good technique is limited by the pathological process.
Our experience is discussed for the two periods:
From 1947 to 1950, we used the Smith-Petersen technique which consisted in a wide anterior approach, the interposition of a Vitallium cup, and the creation of a wide acetabulum which allowed mobility both in the acetabulum and at the neck stump. At the beginning of our experience with the use of the Judet acrylic head, we were under the influence of these principles and our attention was focused on mobility rather than on the stability of the hip joint.
From 1950 to the present time, our approach to the problem has been slightly different. Our aim is to obtain a mechanically stable joint, the parts of which are fitted to each other with precision, and to accept the risk of a limitation of mobility.
In this last period our technique is characterized by points which have already been emphasized:
Good exposure of the entire joint anteriorly and posteriorly by means of Gibson’s posterolateral approach;
Preservation or reconstruction of the normal length of the femoral neck;
Correction of anteversion in patients with congenital conditions;
The exact fitting of the prosthetic head to the acetabulum (such an exact fitting allows only two or three millimeters of joint space).
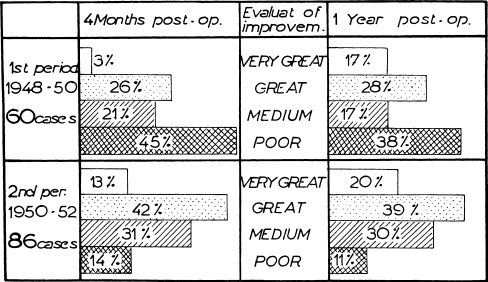
The comparison of the early functional results from the use of the two techniques may teach us whether or not the later modifications in technique are improvements (Chart 3).
Chart 3.
Chart shows early results (at four months) and the improvement brought about by the operation (evaluated at one year after the operation). (Adapted from Tableau 2. Mémoires de l’Académie de Chirurgie,79: 463, 1953.)
During the period 1947 to 1950, 45 per cent. of the patients showed really good results after one year, but 17 per cent. showed fair results and 38 per cent. showed unsatisfactory results. During the period 1950 to the present, good results were seen in 55 per cent. of the patients after four months, and good results were seen in 59 per cent. after one year. Only 11 per cent. showed unsatisfactory results (Chart 3).
It may he concluded from these figures that, with the creation of a mechanically well adjusted hip, good function is more quickly and more frequently obtained.
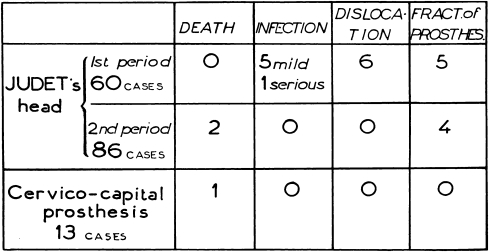
If we consider the postoperative accidents and complications (Chart 4), we find that there were fewer accidents with the use of the later technique, with the exception of fractures of the prosthesis which should be completely overcome in the future through the use of our new device.
Chart 4.
Chart shows the incidence of early complications and the causes of failure. (Adapted from Tableau 3, Mémoires de l’ Académie de Chirurgie,79: 464. I953.)
Postoperative dislocations have not occurred because of the preservation or restoration of the normal length of the femoral neck.
Study of early results of arthroplasty enables us to say that, during the first postoperative year, the functional result depends mainly upon the mechanical conditions. If the trouble is essentially mechanical, as in cases of trauma and in a certain number of cases of congenital or acquired deformity, good technique gives a high percentage of excellent functional results.
The prospects are less favorable in the presence of progressive degenerative conditions.
All of this leads one to ask the question: How do the good results stand the test of time?
Late Results
Follow-up of patients after one year may show three things:
Improvement by adaptation of the muscles and the joint to the new conditions created by the operation.
Stability: A patient, now aged seventy, whose hips are shown in Figure 13A–B, who had been subjected to one of our first arthroplasties showed a consistently maintained result fifty-four months after operation.
Deterioration: The function of the hip after the operation may grow worse because of (a) deterioration of the prosthesis itself by fracture or by wearing, (b) resorption of the bone caused by the mechanical action of the foreign body, and (c) the persistence of the degenerative process which, of course, had not been suppressed by the operation.
Fig. 13A–B.
(A) Ununited fracture of the neck with a long neck stump. (B) Three and one-half years after the insertion of a Judet prosthesis. Roentgenogram shows no looseness of the prosthesis. Good result was maintained. (The superior part of the femoral-neck stump was broken during the operation; this united.)
From this point of view, we have reviewed all of the patients with trauma, osteoarthritis, or congenital subluxations followed for more than eighteen months, and we have compared the functional state at the end of the first postoperative year with that at the last examination. This comparison was possible in 146 of our patients.
This comparison was done separately on cases of trauma, on cases of osteo-arthritis. and on cases of congenital subluxation; but, as we found that the postoperative course was practically the same in the three groups, all of the cases have been grouped in one chart (Chart 5). In this chart, the patients have been divided into three groups, according to the duration of the follow-up: one and one-half to two years, two to three years, and three years or more.
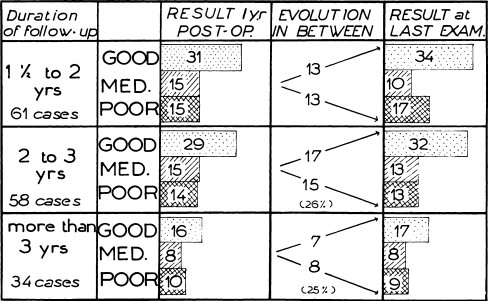
Chart 5.
Evolution of functional result.
The left-hand column shows the number of good, medium (fair), and poor results one year after the operation. The central column gives the number of patients in whom the result has improved or has worsened between the examination at the end of the first postoperative year and the last examination. In the right-hand column are shown the proportion of good, medium (fair), and poor results seen when the patients were last examined.
It must, be pointed out that the percentage of deterioration is about the same (20 to 25 per cent.) in the cases reviewed after two years, three years, or four years. This may suggest that deterioration generally occurs during the second year and that the number will not rise very much with the passing of time (Chart 6).
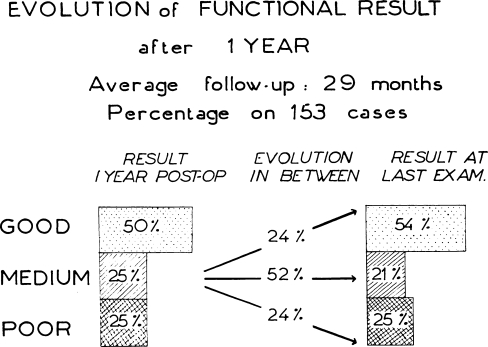
Chart 6.
In Chart 6, all of the cases are grouped without consideration of the duration of the follow-up. It is clearly shown that the proportion of more or less improved results is approximately the same at the last examination as that at the end of the first year. This is due to the fact that the impaired results are balanced by an equal number of improved results. The late improvements are due to the wonderful adaptability of nature. These must not, however, cause us to forget deterioration for which, even if we do not hold ourselves responsible, the patient may.
The fact is that 20 per cent. of our results do not last. One of five patients, happy one year after operation, will have a partial (sometimes total) recurrence of his condition (Table 6).
Table 6.
Late: Deterioration of results (after one year)
| No. of cases | |||
|---|---|---|---|
| Frequency | |||
| Osteo-arthritis and subluxations | 21 to 100 | ||
| Trauma | 8 to 53 | ||
| Total 29 of 153 | |||
| Symptoms | |||
| Impaired mobility (No. of cases) | Increased pain (No. of cases) | Increased pain and impaired ability to walk (No. of cases) | Increased pain and impaired ability to walk and impaired mobility (No. of cases) |
| 3 | 8 | 14 | 4 |
| Degree of deterioration slight (No. of cases) | Medium (No. of cases) | Serious (No. of cases) | |
| 8 | 18 | 3 | |
| Postoperative functional state compared with that before operation | |||
| Much better(No. of cases) | Better(No. of cases) | Same(No. of cases) | Worse(No. of cases) |
| 7 | 12 | 5 | 5 |
The degree of impairment of the result varies. When we compared the functional state of the patient at the last examination with that before the operation, we found that five patients were as badly off as they had been before the operation and that five were worse. However, seven of these had shown poor results from the beginning.
The causes of late deterioration are not always easy to find. Information may be obtained by clinical examination, roentgenograms, and operative findings (Table 7).
Table 7.
Late deteriorations (roentgenographic and operative findings)
| No. of cases | |
|---|---|
| Periarticular bone production | 4 |
| Joint stiffness without bone formation | 2 |
| Bone absorption around prosthesis: | |
| with fracture of prosthesis | 5 |
| with prosthesis unchanged | 6 |
| with wearing | 8 |
| No particular findings | 4 |
| Total | 29 |
In nineteen of twenty-nine cases, impairment of the result was possibly due to fracture of the prosthesis, wearing of the prosthesis, or bone absorption around the prosthesis.
We believe that these complications can probably be eliminated by a better designed prosthesis:
Fracture of the acrylic prosthesis may be avoided by the central steel stem of the Judet device; most of those which broke had not been equipped with this stem. However, we have seen three fractured stems with the steel re-enforcement.
Wearing of the prosthesis was found in more than half of the acrylic prosthetic heads removed one year or more after the operation. This is reason enough to prefer a steel or Vitallium prosthesis to one made of acrylic.
Bone absorption is a more serious matter. It occurs chiefly on the neck stump, with sclerosis, sharpening of the end of the stump, and widening of the canal (Figs. 14A–B). The acetabulum may also show absorption, although in fewer cases (Fig. 15A–C). Bone absorption is sometimes seen in the roentgenograms of patients in whom a good result has been maintained (Table 8).
Fig. 14A–B.
(A) Arthroplasty with interposition of the Judet prosthesis for osteo-arthritis of the hip. (B) Three years and ten months postoperatively. Roentgenogram shows very great bone absorption around the prosthesis, loosening of the prosthesis, and absorption of the acetabulum. Functional result, which was good, has deteriorated after one year.
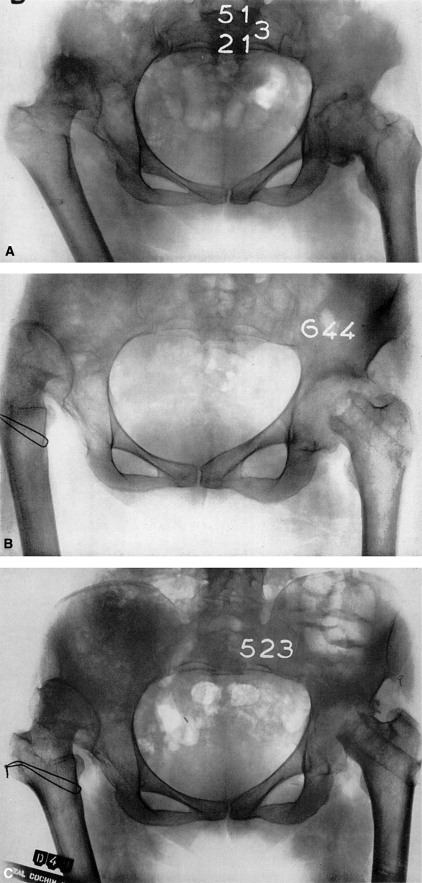
Fig. 15A–C.
(A) Osteo-arthritis of the left hip. Congenital dislocation of the right hip. (B) Osteotomy of the right hip. Arthroplasty of the left hip. Good result one year postoperatively. (C) Two and a half years postoperatively, roentgenogram showed bone absorption in the neck and acetabulum. Functional result deteriorated.
Table 8.
Bone absorption around the prosthesis
| Functional Status | Appearance normal as seen by X-ray (No. of cases) | Bone absorption(No. of cases) |
|---|---|---|
| Maintained | 116 | 8 |
| Deteriorated | 23 | 19 |
In our experience, bone absorption was found in eight patients of 124 in whom results were maintained, while it was present in nineteen patients of twenty-three with impaired results. This fundamental difference in incidence suggests that bone absorption and the consequent loosening of the prosthesis are the chief causes of late recurrence of pain.
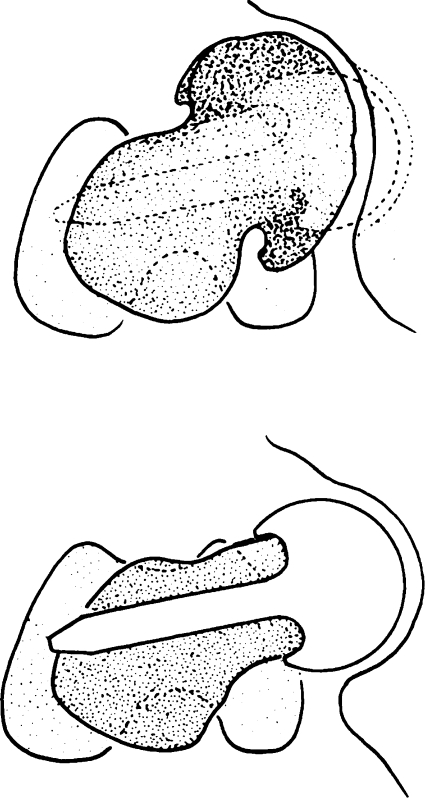
The cause of bone absorption is probably the very strong pressure put on a small surface of bone, perhaps less resistant on account of poor vascularization. If this is true, absorption must be greater laterally on the upper border of the canal and medially on the inferior border; the prosthesis will tilt and tend to come to a horizontal position (Figs. 16 through 18B). This is quite obvious in the roentgenograms of some patients.
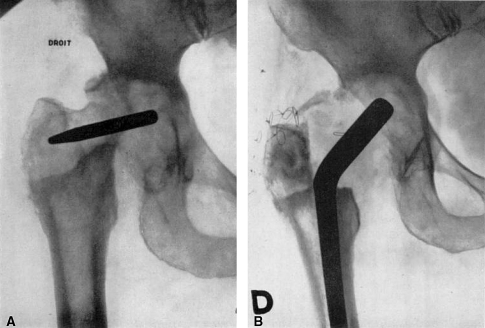
Fig. 17A–B.
(A) Roentgenogram shows necrosis of the femoral head after traumatic dislocation in a girl, twenty-one years old. (B) Two years after the operation. The functional result was excellent for one and a half years. The patient, at the time this roentgenogram was made, was pregnant : some pain had recurred. Roentgenogram shows slight absorption of the neck around the prosthesis.
Fig. 16.
Diagram shows the influence of pressure on bone absorption. With the use of the Judet prosthesis (right), absorption widens the cervical canal: the prosthesis becomes loose and absorption is aggravated. When the cervico-capital prosthesis is used (left), the device presses on a more vascularized part of the femur. Even with slight absorption, the prosthesis will not tilt nor will it become loose.
Fig. 18A–B.
(A) Osteo-arthritis of the hip. Patient was operated upon in another hospital; two years after the operation there was great absorption and tilting of the prosthesis. A very bad result. (B) Six months after the insertion of the cervico-capital prosthesis, there was a good functional result.
Progressive mobility of the prosthesis makes absorption more and more inevitable.
Bone absorption in the acetabulum is difficult to prevent, but loosening of the prosthesis in the femur can he sharply reduced, and perhaps even suppressed, by a better design of the prosthesis which should meet two specifications:
Distribution of pressure on as large a surface of bone as possible;
A design which, if some absorption occurs, will not allow progressive mobility of the prosthesis.
Our C prosthesis with the long intramedullary nail and flat weight-bearing surface seems to be the answer to these conditions. If absorption occurs on the weight-bearing surface, the piece will go slightly further down into the femur, but it will not tilt.
So far, in seventeen patients followed for more than two years, we have seen neither any clinical impairment nor roentgenographic evidence of loosening.
Conclusion
Results in hip arthroplasty with an inert prosthesis are very encouraging in the treatment of non-union of the femoral neck, traumatic necrosis of the femoral head, and osteo-arthritis. Unfortunately, a certain number of patients are not improved (20 per cent.) or, after one or two years’ improvement, suffer a partial or total recurrence of pain. Some of these failures are due to the persistence or the recurrence of the degenerative condition and cannot be avoided by technical improvements.
However, a fair number of failures are caused by mechanical disorders. Wearing or fracture of the prosthesis can certainly be eliminated by the use of a prosthesis made of inert metal rather than of acrylic. The ill effects of the absorption of bone in the upper end of the femur can probably be avoided by the better design of a prosthesis which will distribute pressure over a wide surface and prevent loosening of the prosthesis.
Summary
Late results in 243 arthroplasties with an acrylic prosthesis for traumatic or osteoarthritic conditions are reported.
Early results (after one year) show the importance of the restoration of the normal mechanics of the hip joint by the preservation or the restoration of normal length of the femoral neck, the exact correction of anteversion, and the precise fit of the prosthetic head to the acetabulum. A good exposure of the joint through the posterolateral approach appears necessary in order to fulfill these conditions.
Late results (from two to five years) show deterioration of the functional results in 20 per cent. These deteriorations appear to be caused by bone absorption around the Judet prosthesis and the consequent loosening of the prosthesis.
A new type of cervico-capital prosthesis is proposed which makes possible:
Restoration of the normal length of the femoral neck when it is congenitally or pathologically short;
Correction of anteversion, even when very marked;
A weight-bearing surface on a more vascularised part of the femur;
The distribution of pressure on hone so as to lessen bone absorption, to prevent its ill effects, and, particularly, to decrease mobility of the prosthesis.
Footnotes
Read at the Annual Meeting of The American Orthopaedic Association, Hot Springs, Virginia, July 1, 1953.
Richard A. Brand MD ✉ Clinical Orthopaedics and Related Research, 1600 Spruce Street, Philadelphia, PA 19103, USA e-mail: dick.brand@clinorthop.org
References
- d’Aubigné R. M., et Postel, M.: Traitement des accidents de la consolidation des fractures cervicales vraies du fémur. Rev. Chir., 71: 265–292, 1952. [PubMed]
- d’Aubigné, R. M., et Postel, M.: Résultats de l’arthroplastie dans les coxarthries et subluxations de la hanche avec un recul de quatre ans. Mém. de l’Acad. Chir., 79: 460–468, 1953. [PubMed]
- Gibson, Alexander: Posterior Exposure of the Hip Joint. J. Bone and Joint Surg., 32-B: 183–186, May 1950. [DOI] [PubMed]
- Gosset, J.: Arthroplastie de la hanche par plastie acrylique cervico-capitale (technique personnelle). Seim Hôp. de Paris, 26: 4494–4497, 1950. [PubMed]
- Judet, Jean, and Judet, Robert: The Use of an Artificial Femoral Head for Arthroplasty of the Hip Joint. J. Bone and Joint Surg. 32-B: 166–173, May 1950. [DOI] [PubMed]
- Pauwels: Des affections de la hanche d’origine mécanique et de leur traitement par 1’ostéotomie d’adduction. Rev. Chir. Orthop., 37: 22–30, 1951. [PubMed]
- Smith-Petersen, M. N.: Evolution of Mould Arthroplasty of the Hip Joint. J. Bone and Joint Surg., 30-B: 59–75, Feb. 1948. [PubMed]