Abstract
There are six different definitions of acetabular position based on observed inclination and anteversion made in either the (1) anterior pelvic plane or (2) coronal planes and based on whether each of the observations made in one of these two planes is (1) anatomic, (2) operative, or (3) radiographic. Anteroposterior pelvic tilt is the angle between the anterior pelvic plane and the coronal plane of the body. The coronal plane is a functional plane and the anterior pelvic plane is an anatomic pelvic plane. A cup may be in the “safe zone” by one definition but may be out of the “safe zone” by another definition. We reviewed published studies, analyzed the difference in varying definitions, evaluated the influence of the anterior pelvic tilt, and provided methods to convert from one definition to another. We recommend all inclination and anteversion measurements be converted to the radiographic inclination and anteversion based on the coronal plane, which is equivalent to the inclination and anteversion on the anteroposterior pelvic radiograph.
Introduction
With the advent of computer navigation for quantitative knowledge of acetabular component position, there has been an increasing number of studies measuring the cup position [2, 3, 5, 11, 18, 22, 23, 26, 36, 38]. Unfortunately, different imaging techniques have been used to report the outcome data for cup inclination and anteversion [9–11, 18, 23, 25, 27, 36, 38]. Murray’s definitions of the anatomic, operative, and radiographic planes of the acetabulum were based on the coronal plane [34]. Computer navigation has translated these to the anterior pelvic plane [34]. Some studies have included pelvic tilt [13, 14] and some have not [4, 17, 20, 22, 28, 31, 32, 42].
Computer navigation measurements based on the anterior pelvic plane cannot be directly compared with conventional radiographs measured on the coronal plane. Conventional radiographs have themselves been measured in error using the safe zones of Lewinnek et al. [30]. Lewinnek et al. [30] determined their safe zone based on a radiographic technique using a jig that positions the patient parallel to the anterior pelvic plane. Thus, this safe zone is not comparable to the coronal plane of radiographs. Furthermore, the variability of measurements on plain radiographs may introduce substantial errors [3, 17, 43]. To reduce errors associated with conventional radiographs, computed tomography (CT) scans and three-dimensional reconstructions have been used as imaging techniques to measure the true value of implant positions.
It is important to have a common measurement technique so the results of studies can be scientifically compared. We provide a comprehensive overview of the different methods used for measuring the inclination and anteversion of the acetabular component. We discuss the use of these measurement methods in the literature and in our own study results and propose a standardized method for reporting the orientation of the acetabular component.
Measurement Terminology
Anterior Pelvic Plane
The anterior pelvic plane is determined by three reference points: the two anterosuperior iliac spines and the anterior surface of the pubic symphysis. In 1922, Robinson et al. [42] first described the anterior pelvic plane as the pelvic frontal plane. In 1978, Lewinnek et al. [30] used a special positional jig for conventional radiographs that defined the anterior pelvic plane to measure the inclination and anteversion of the cup. In 1998, Jaramaz et al. [22] used the anterior pelvic plane in software to determine computer-assisted cup placement in THA.
Anteroposterior Pelvic Tilt
The anterior or posterior pelvic tilt is defined as the angle between the anterior pelvic plane and the coronal plane of the body. Anterior pelvic tilt is defined as the distance between the middle point of the two anterosuperior iliac spines and the coronal plane when this distance is greater than the distance between the anterior surface of the pubic symphysis and the coronal plane (Fig. 1). Posterior pelvic tilt is defined as the distance between the middle point of the two anterosuperior iliac spines and the coronal plane, but now this distance is shorter than the distance between the anterior surface of the pubic symphysis and the coronal plane (Fig. 2). The anterior pelvic plane has also been called pelvic inclination and reclination [3, 6] and the pelvic flexion angle [35].
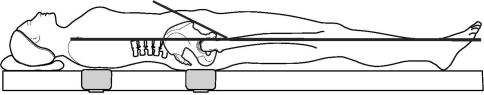
Fig. 1.
A diagram demonstrates anterior pelvic tilt. The distance between the middle point of two anterosuperior iliac spines and the coronal plane is longer than that between the anterior surface of the pubic symphysis and the coronal plane.
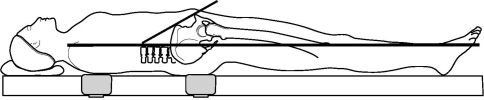
Fig. 2.
A diagram demonstrates posterior pelvic tilt. The distance between the middle point of the two anterosuperior iliac spines and the coronal plane is shorter than that between the anterior surface of the pubic symphysis and the coronal plane.
Murray’s Definitions
Murray [34] assessed the orientation of the acetabular component and described three measurements of inclination and anteversion according to the three different axes of the body. The acetabular axis was defined as the axis perpendicular to the rim of the cup that passes through the center of the cup. One of the most important facts about Murray’s definition is he originally used the coronal plane of the body, not the anteroposterior pelvic plane, although his definitions are often used with the anteroposterior pelvic plane. His definitions are as follows: anatomic inclination is the angle between the acetabular axis and the longitudinal axis of the body; operative inclination is the angle between the acetabular axis and the sagittal plane (the angle of abduction of the acetabular axis); radiographic inclination is the angle between the longitudinal axis of the body and the acetabular axis when projected onto the coronal plane; anatomic anteversion is the angle between the acetabular axis and the transverse axis of the body when the acetabular axis is projected onto the transverse plane; operative anteversion is the angle between the longitudinal axis of the patient and the acetabular axis when projected onto the sagittal plane; and radiographic anteversion is the angle between the acetabular axis and the coronal plane.
Inclination and Anteversion
Various authors have studied the correct positioning of implants by postoperatively measuring their positions [7, 19, 30, 31, 33]. While using conventional anteroposterior pelvic radiographs, radiographic inclination is measured as the angle between the longitudinal axis of the body and the acetabular axis projected onto the coronal plane [21, 30, 34]. Radiographic anteversion is defined as the angle between the acetabular axis and the coronal plane [30, 34]. While measuring these angles on anteroposterior radiographs, inclination is the angle between the face of the cup and the transverse axis; cup anteversion is calculated from the relative size of the major and minor diameters of the ellipse (Fig. 3).
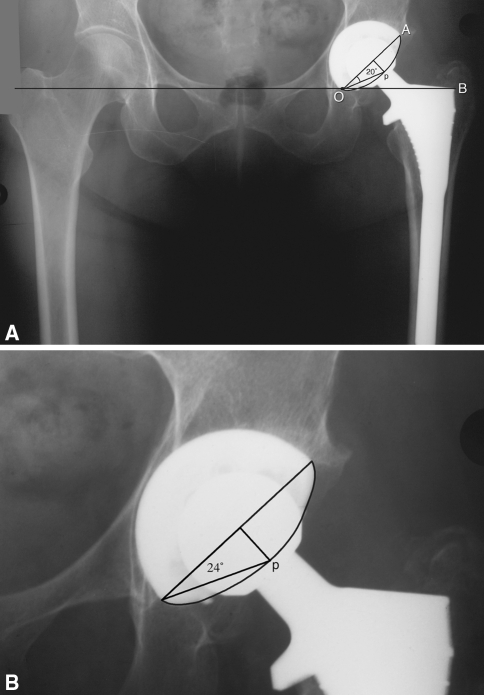
Fig. 3A–B.
(A) In an anteroposterior pelvic radiograph, the angle AOB is the inclination and the angle AOP is the anteversion, which is 20°. (B) In an anteroposterior hip radiograph for the same hip, the anteversion is 24°.
Safe Zone
The safe zone described by Lewinnek et al. [30] is based on angles equivalent to Murray’s radiographic definition on the anterior pelvic plane. Lewinnek et al. [30] used a pelvic coordinate system with an anterior pelvic plane to define the safe zone. A jig device with three legs and a bubble level was used to position the pelvis parallel to the radiographic film. The patient was positioned supine and the three legs of the device pressed directly and firmly over the anterosuperior iliac spines and the symphysis pubis. The patient was then repositioned until the bubble level indicated parallel and horizontal positioning, and the radiograph was then taken. Postoperative cup positions were measured to compare cups with and without dislocation. After this study, the safe zone was defined as 40° ± 10° of inclination and 15° ± 10° of anteversion. Therefore, the safe zone described by Lewinnek et al. [30] does not truly correlate to conventional anteroposterior pelvic radiographs taken in an orthopaedic clinic.
Common Problems of Measurements
Routine Radiographic Measurement
Plain radiographs have been the most important diagnostic measure of inclination and anteversion after THA [30]. Inclination can be directly measured on conventional radiographs, whereas anteversion is still problematic, although different calculations or measurement methods have been published in the literature [1, 12, 15, 20, 37, 46]. Anteversion is more difficult to measure because of the variable rotation of radiographs and the difficulty in distinguishing between anteversion and retroversion [27, 46]. For example, because the metal head overlays the acetabular edges, there will be inexact trigonometric measurements of acetabular anteversion [27]. To make a reliable measurement of anteversion, it is necessary to take two radiographs with different directions of the central beam [39]. Most commonly, this means an anteroposterior pelvic and anteroposterior hip radiograph [12, 15]. It has been shown measurements of cup anteversion on anteroposterior pelvic radiographs provide values 4° to 5° less than that measured from anteroposterior hip radiographs [1, 12, 15]. When anteroposterior pelvic radiographs are used to measure anteversion, 4° to 5° should be added to the measurement to determine the true anteversion of the cup.
The Anterior Pelvic Plane
Currently, in almost all computer-assisted orthopaedic surgery systems that rely on the anterior pelvic plane, the plane is derived by percutaneously identifying three osseous landmarks: the two anterosuperior iliac spines and the pubic symphysis [10, 11, 13, 36, 48]. Using a kinematic model, Wolf et al. [48] showed this registration, and errors in doing the registration, creates inaccuracies on the computer measurement of final orientation of the acetabular cup. Simulation results indicated, for example, if a surgeon aimed for 45° of abduction and 20° of anteversion, a total error of 4 mm in measuring the anterosuperior iliac spine and pubic tubercles would result in a final cup orientation of 47° of abduction and 27° of anteversion (2° of abduction, 7° of anteversion error).
Richolt et al. [41] used ultrasonographic measurements to determine the minimal soft tissue thickness between skin surfaces and bony landmarks in 72 patients. Soft tissue thickness over the anterosuperior iliac spines averaged 7.9 ± 3.4 mm and 13.6 ± 4.1 mm over the pubic tubercles (5.7 ± 3.4 mm thicker than the iliac spines). A thick layer of fat over bone would result in an average underestimation of anteversion by 4.4° (range, 1.3°–5.5°). To reduce this error, Dorr et al. [13] punctured through skin to bone to register the bony landmarks.
Anteroposterior Pelvic Tilt
Modern navigation techniques allow precise positioning of the acetabular cup relative to the anterior pelvic plane according to the plan, which is assumed correct [8, 10, 11, 13, 22, 23, 25, 26, 29, 38]. Pelvic position is not static, but rather dynamic during gait and other activities of daily living, and the means of these different positions have been measured [4, 9, 29, 35]. A safe zone of combined anteversion of the stem and cup (or the anatomic hip) has been repetitively defined as 25° to 45°, lower in men and higher in women [4, 14, 28, 47]. Variations in anteroposterior pelvic tilt will affect the resulting spatial orientation measurement of the cup [29]. Zero pelvic tilt occurs when the anterior pelvic plane is parallel to the coronal plane. It is only in this special case that cup inclination and anteversion have identical measurements on both navigation and postoperative radiographs. Anteroposterior pelvic tilt is the factor that introduces uncertainty in measuring the orientation of the cup when comparing conventional radiographs with CT scans or when using either a free-hand technique or a mechanical alignment guide during performance of THA. With anterior pelvic tilt, less anteversion of the acetabulum will be measured radiographically and with posterior pelvic tilt, increased anteversion of the acetabulum will be measured radiographically [2, 3, 13, 17, 29, 40, 45].
We have studied the effect of anteroposterior pelvic tilt on acetabular component position in THA as measured by imageless computer navigation and the detailed measurement method was asked about in these studies [13, 14]. The same measurement technique was used to measure anteroposterior pelvic tilt in 619 hips. The hips were divided into five groups (Table 1). Of the 619 hips measured, 8.6% had no anteroposterior pelvic tilt, 40.4% had posterior pelvic tilt of 1° to 9°, 12.6% had posterior pelvic tilt of 10° to 25°, 33.6% had anterior pelvic tilt of 1° to 9°, and 4.8% had anterior pelvic tilt of 10° to 20°. An anteroposterior pelvic tilt of 1° led to an approximate 0.8° change of functional cup anteversion, confirming data previously published by Lembeck et al. [29].
Table 1.
The influence of anterior or posterior pelvic tilt on anteversion (n = 619)
| Pelvic tilt | Hips | Adjust* | Adjust coefficient† |
|---|---|---|---|
| Posterior tilt greater than 10° | 78 (12.6%) | 10.4 ± 2.5 (7–20) | 0.8 |
| Posterior tilt 1° to 9° | 250 (40.4%) | 3.6 ± 2 (1–9) | 0.8 |
| No tilt (0°) | 53 (8.6%) | NA | NA |
| Anterior tilt 1° to 9° | 208 (33.6%) | −3.3 ± 1.8 (−7 to −4) | −0.8 |
| Anterior tilt greater than 10° | 31 (4.8%) | −8.3 ± 2.1 (−13 to −4) | −0.7 |
* Adjusted anteversions (expressed as average ± standard deviation with range in parentheses) when converting the anteversion from the anterior pelvic plane to the coronal plane; a positive value is increase and a negative value is decrease; †how many degrees of the anteversion are adjusted by the change of 1° of anteroposterior pelvic tilt; a positive value is increase and a negative value is decrease; NA = not applicable.
Studies of variations in natural pelvic orientation have indicated a need for greater knowledge of anteroposterior pelvic tilt for intraoperative alignment and postoperative measurements [16]. McCollum et al. [31] suggested adjusting cup placement based on the patient’s anteroposterior pelvic tilt as a means of reducing dislocation after THA. A large range (–37° to 44°) in preoperative supine pelvic anteroposterior tilt supports this recommendation [9, 13, 35]. Pelvic orientation is unique to each patient and changes according to patient position. Placing the acetabular component without considering the tilt of the patient’s pelvis could lead to impingement, dislocation, and increased wear, although cup placement was relative to the bony anatomy of the acetabulum [31, 44]. It is also important to know the pelvic orientation for measuring an accurate cup alignment from postoperative radiographs [5], although this is not available in orthopaedic offices.
Safe Zone
The instrumented radiographic technique of Lewinnek et al. [30] has rarely been used in clinical practice. Despite this, the safe zone concept, originally defined for free-hand cup positioning on the coronal plane, has been commonly referenced. However, the safe zone has been incorrectly applied to both radiographic and operative definitions on the coronal plane as well as to anatomic, operative, and radiographic definitions on the anterior pelvic plane [9–11, 18, 23, 25, 27, 36, 38]. Therefore, it is incorrect, and impossible, to compare literature results based solely on the safe zone. For example, Pierchon et al. [38] evaluated dislocation in 38 THAs and concluded 11 of 38 cups in hips that had dislocated were placed inside Lewinnek’s safe zone. They concluded cup orientation did not play a major role in dislocation. These authors had no control for anteroposterior pelvic tilt so they did not use the true Lewinnek safe zone.
Use of Murray’s Definitions of Acetabular Orientation
When Murray [34] published his definitions of acetabular orientation in 1993, his definitions only referred to the coronal plane. However, Murray’s definitions have been applied to measurements related to the anterior pelvic plane. Because of anteroposterior pelvic tilt, measurements on the coronal plane cannot be directly compared with those on the anterior pelvic plane. Many reports in the literature have ignored such differences [9–11, 18, 23, 25, 27, 36, 38]. To resolve this problem, Murray’s definition should be expanded from the anatomic, operative, and radiographic coronal plane to the same three orientations on the anterior pelvic plane, which would create six definitions of cup inclination and anteversion. This is important because most measurements by computer navigation and CT are now referenced from the anterior pelvic plane.
The apparent inclincation and anteversion resulting from the three means of observations (anatomic, operative, and radiographic) have a greater spread in difference as the anteversion of the cup increases or the inclination of the cup decreases even when measured on the same plane (Table 2). These data were developed from Lewinnek’s safe zone (40° ± 10° of inclination and 25° ± 10° of anteversion; see Appendix 1 for methods of calculation) [30]. When inclination and anteversion are in the safe zone for one of the planes of Murray’s definitions, they may be out of the safe zone by another definition (Table 2). If the anteversion of the cup is in the safe zone by the operative definition, it may be 11° outside by the anatomic definition; if the cup anteversion is in the safe zone by the radiographic definition, it would be 18° more anteverted in the anatomic plane. The definitions assume a zero tilt. Pelvic tilt compounds this problem, because the differences among the three definitions would be larger if anteroposterior pelvic tilt were present.
Table 2.
Differences in anatomic, operative, and radiographic inclination and anteversion on the same plane
| Anatomic | Operative | Radiographic | |||
|---|---|---|---|---|---|
| Inclination | Anteversion | Inclination | Anteversion | Inclination | Anteversion |
| 30 | 5 | 29.9 | 2.9 | 29.9 | 2.5 |
| 30 | 25 | 26.9 | 13.7 | 27.6 | 12.2 |
| 40 | 15 | 38.4 | 12.3 | 39.0 | 9.6 |
| 50 | 5 | 49.7 | 5.9 | 49.9 | 3.8 |
| 50 | 25 | 44.0 | 26.7 | 47.2 | 18.9 |
| 30.4 | 8.6 | 30 | 5 | 30.1 | 4.3 |
| 38.3 | 36.2 | 30 | 25 | 32.5 | 21.5 |
| 42.3 | 17.1 | 40 | 15 | 41.0 | 11.4 |
| 50.2 | 4.2 | 50 | 5 | 50.1 | 3.2 |
| 54.4 | 19.5 | 50 | 25 | 52.7 | 15.8 |
| 30.4 | 9.9 | 29.9 | 5.8 | 30 | 5 |
| 38.3 | 43.0 | 26.9 | 28.3 | 30 | 25 |
| 42.3 | 22.6 | 38.4 | 19.3 | 40 | 15 |
| 50.2 | 6.5 | 49.7 | 7.8 | 50 | 5 |
| 54.4 | 31.3 | 44.0 | 36.0 | 50 | 25 |
In general, on either the coronal or anterior pelvic plane, anatomic inclination and anteversion are always greater than radiographic inclination and anteversion; anatomic inclination is always greater than operative inclination; and operative anteversion is always greater than radiographic anteversion. If a difference exists (depending on the combination of inclination and anteversion), the difference in inclination is small, whereas the difference in anteversion may be large.
Mixed Use of Murray’s Definitions in the Literature
Different definitions of inclination and anteversion have been used in the same study. For example, Haaker et al. [18] compared two groups of patients with and without the use of computer navigation and used two definitions to compare results. They used target numbers of 45° of inclination and 20° of anteversion with respect to the anterior pelvic plane in both groups of patients and validated the position with CT scans. The authors ignored two facts: two different definitions were used for inclination and anteversion and anteroposterior pelvic tilt was ignored. For the cup target in the free-hand group, the operative definition on the coronal plane was used, whereas in the computer-navigated group, the anatomic definition on the anterior pelvic plane was used. The postoperative CT scans used the anatomic definition on the anterior pelvic plane as the reference plane for both groups and did not include the anteroposterior pelvic tilt for navigated hips but did for free-hand hips. With these differences in measurements, a greater variation of cup inclination and anteversion will occur between the two groups and they cannot be accurately compared.
A second example is that of DiGioia et al. [11], who compared acetabular component orientation using mechanical guides versus CT-aided computer navigation. The cup was targeted at 45° of inclination and 20° of anteversion. With mechanical guides, 78% of the acetabular components would have been outside the safe zone of Lewinnek et al. [30] based on the operative definition on the coronal plane. CT scans used the anatomic definition on the anterior pelvic plane. Neither compensated for anteroposterior pelvic tilt. Therefore, the safe zones being compared are not the same and this can influence the differences observed in the comparison.
A third example is that of Kalteis et al. [26], who compared targeted cup positions between free-hand and image-free navigation techniques using postoperative CT scans as the true value. The target for free-hand cups was on the coronal plane using the operative definition, whereas for image-free navigation, it was on the anterior pelvic plane by the anatomic definition. The postoperative CT scans converted all measurements to the operative definition but left the free-hand measurements on the coronal plane and the navigation on the anterior pelvic plane. In addition, the anteroposterior pelvic tilt was ignored in all hips.
Validation Methods
Our interest in this subject originated with our attempts to validate our computer navigation system with two different CT scan reconstruction methods. We operated on 100 patients with primary THA and used computer navigation for acetabular inclination and anteversion. We obtained postoperative CT scans of the hip to validate the computer navigation measurements in all 100 patients. The anteversion and inclination were measured by a three-dimensional model using both the HipNav™ System (Institute for Computer Assisted Orthopaedic Surgery, Pittsburgh, PA) and the Navitrack® System (ORTHOsoft, Inc, Montreal, Canada). The results were an inclination of 46.8° ± 4.1° and an anteversion of 37.5° ± 7.5° by HipNav™ and an inclination of 39.8° ± 3.3° and an anteversion of 25.8° ± 5.5° by Navitrack®. Initially, we did not understand the reasons for such differences because both methods were based on the anterior pelvic plane. We subsequently determined HipNav™ used Murray’s anatomic definition of the anterior pelvic plane, whereas Navitrack® used the radiographic definition of the anterior pelvic plane. If the HipNav™ values on the anatomic plane were converted by Murray’s algorithm onto the radiographic definition, the comparison for inclination was 39.8° ± 3.3° for Navitrack® and 39.5° ± 3.2° for HipNav™, whereas the comparison for anteversion was 25.8° ± 5.5° for Navitrack® and 25.6° ± 6.2° for HipNav™. Using a single definition, the measurements could be compared.
Because of the variation in measurement methods, we constructed a bench test to validate the validation methods. We wanted to confirm the computer navigation measurements were accurately measured by the software and the CT scans were reconstructed and measured with minimal error. In addition, this would validate the formula (found in Appendices 1 and 2) for connecting anatomic, operative, and radiographic inclination and anteversion on the same plane and converting inclination and anteversion between the anterior pelvic plane and the coronal plane.
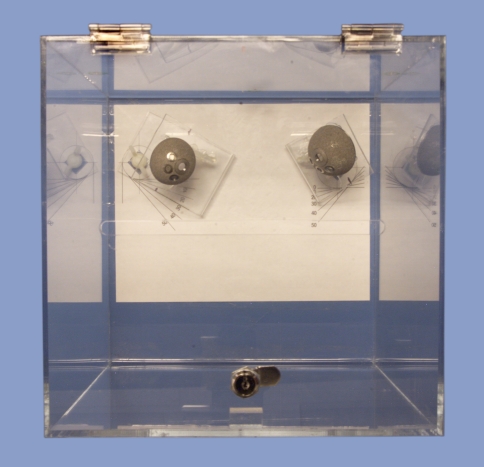
We constructed a jig consisting of a silicone cube with two acetabular cups mounted on a mobile base so cup anteversion could be varied (Fig. 4). This mobility allowed six different positions for anteversion (0°, 10°, 20°, 30°, 40°, 50°). The cups were fixed at an inclination of 47° for the right and 35° for the left. Metal markers were embedded within the jig to simulate the two anterosuperior iliac spines and the pubic tubercles. With the cup fixed in each of its possible positions (for example, right cup at 47° inclination and 10° anteversion and left cup at 35° inclination and 40° anteversion), measurements were performed with computer navigation and CT scans of each of the positions. Because the acetabular position was known, the values obtained by computer navigation and CT scans could be judged for accuracy. There were 36 combinations of cup positions studied (Tables 3–5). The computer navigation system used was the ORTHOsoft Imageless software. This system measures the cup position on the radiographic anterior pelvic plane and the software adjusts it according to the tilt of the pelvis to the radiographic coronal plane. Tilt has no bearing on inclination and anteversion when the results are measured just on the anterior pelvic plane. The effect of adding pelvic tilt creates a difference of 0.8° anteversion for each 1° of tilt between the anterior pelvic plane and the coronal plane (Table 3). Pelvic tilt of 6°, either posterior or anterior, can change the cup anteversion by approximately 5°. There is a large difference between the different planes (Table 3).
Fig. 4.
The jig consisted of a silicone cube with two acetabular cups mounted on a mobile base so the cup anteversion could be varied from 0° to 50°.
Table 3.
Computer navigation values with adjustment for tilt
| Tilt | Real anteversion (°) | Real inclination 47° | Real inclination 35° | ||
|---|---|---|---|---|---|
| Inclination (°) | Anteversion (°) | Inclination (°) | Anteversion (°) | ||
| No tilt | 0 | 46.7 | 1.3 | 35.3 | −0.3 |
| 10 | 46.7 | 6.7 | 34.7 | 6.3 | |
| 20 | 45.0 | 15.3 | 33.0 | 12.0 | |
| 30 | 43.0 | 22.0 | 31.3 | 17.0 | |
| 40 | 40.0 | 27.7 | 28.3 | 21.7 | |
| 50 | 34.7 | 33.3 | 24.0 | 26.3 | |
| Posterior pelvic tilt 6° | 0 | 47.3 | 3.0 | 34.7 | 5.0 |
| 10 | 45.3 | 10.7 | 34.3 | 10.7 | |
| 20 | 47.0 | 18.0 | 33.7 | 16.3 | |
| 30 | 44.3 | 24.7 | 32.0 | 21.0 | |
| 40 | 42.3 | 31.3 | 28.7 | 26.7 | |
| 50 | 38.3 | 37.3 | 25.0 | 31.3 | |
| Anterior pelvic tilt 6° | 0 | 47.3 | −3.3 | 34.3 | −4.7 |
| 10 | 46.0 | 3.7 | 34.7 | 1.7 | |
| 20 | 44.7 | 10.0 | 33.0 | 7.0 | |
| 30 | 42.0 | 17.0 | 30.7 | 12.0 | |
| 40 | 38.3 | 23.3 | 29.0 | 18.0 | |
| 50 | 33.3 | 30.0 | 23.7 | 21.7 | |
Table 5.
Computer navigation and computed tomography values with cup at 47° of inclination
| Tilt | Real anteversion (°) | Measurement of inclination (°) | Measurement of anteversion (°) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Anatomic | Radiographic | Anatomic | Radiographic | ||||||
| PT | PT* | MONT | CN | PT | PT* | MONT | CN | ||
| No tilt | 0 | 48 | 48.0 | 47.9 | 46.7 | −1 | −0.7 | 0 | 1.3 |
| 10 | 48 | 47.6 | 47.3 | 46.7 | 10 | 7.4 | 7.8 | 6.3 | |
| 20 | 48 | 46.4 | 46.3 | 45.0 | 19 | 14.0 | 15 | 15.0 | |
| 30 | 48 | 43.9 | 43.9 | 43.0 | 30 | 21.8 | 21.5 | 21.3 | |
| 40 | 48 | 40.8 | 40.9 | 40.0 | 39 | 27.9 | 28.3 | 27.7 | |
| 50 | 48 | 35.5 | 35.4 | 34.7 | 50 | 34.7 | 34.4 | 33.3 | |
| Posterior pelvic tilt 6° | 0 | 48 | 48.0 | 48.2 | 47.0 | 0 | 0.0 | 0 | 1.0 |
| 10 | 48 | 47.7 | 47.6 | 45.3 | 8 | 5.9 | 7.7 | 7.0 | |
| 20 | 48 | 46.4 | 46 | 45.7 | 19 | 14.0 | 14.8 | 14.0 | |
| 30 | 48 | 43.9 | 44 | 43.0 | 30 | 21.8 | 22 | 20.7 | |
| 40 | 48 | 40.4 | 40.1 | 40.3 | 40 | 28.5 | 28 | 27.0 | |
| 50 | 48 | 36.6 | 36 | 35.7 | 48 | 33.5 | 35.1 | 33.0 | |
| Anterior pelvic tilt 6° | 0 | 48 | 48.0 | 48.3 | 47.3 | 0 | 0.0 | 0 | 0.3 |
| 10 | 48 | 47.6 | 47.3 | 46.7 | 10 | 7.4 | 7.5 | 7.0 | |
| 20 | 48 | 46.2 | 46 | 45.0 | 20 | 14.7 | 15.3 | 14.0 | |
| 30 | 48 | 44.2 | 44.1 | 43.0 | 29 | 21.1 | 21.8 | 20.3 | |
| 40 | 48 | 40.4 | 40.6 | 40.0 | 40 | 28.5 | 28 | 27.3 | |
| 50 | 48 | 35.5 | 35.4 | 35.0 | 50 | 34.7 | 34.7 | 33.7 | |
* These values were calculated from the anatomic values from HipNav™; PT = HipNav™; MONT = Navitrack®; CN = computer navigation.
The CT scans were reconstructed using two systems, one using the Navitrack®-based software and the second using the HipNav™ software. The Navitrack® software uses the radiographic definition of Murray and the HipNav™ system uses the anatomic definition of Murray both on the anterior pelvic plane. Even without the influence of tilt, we observed a large difference between anatomic and radiographic definitions on the anterior pelvic plane (Tables 4, 5). However, after converting the anatomic inclination and anteversion of the HipNav™ system to the radiographic definition on the anterior pelvic plane, the difference in the true value measurements between the two systems is very small (Tables 4, 5). This demonstrates different computer navigation systems and different CT systems used to validate computer navigation systems can be comparable if the data are always expressed by the same defined plane.
Table 4.
Computer navigation and computed tomography values with cup at 35° of inclination
| Tilt | Real anteversion (°) | Measurement of inclination (°) | Measurement of anteversion (°) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Anatomic | Radiographic | Anatomic | Radiographic | ||||||
| PT | PT* | MONT | CN | PT | PT* | MONT | CN | ||
| No tilt | 0 | 35 | 35.0 | 35.2 | 35.3 | 0 | 0.0 | 0.1 | −0.3 |
| 10 | 36 | 35.5 | 34.6 | 34.7 | 11 | 6.4 | 6 | 6.3 | |
| 20 | 35 | 33.3 | 33.6 | 33.0 | 20 | 11.3 | 11.2 | 12.0 | |
| 30 | 35 | 31.2 | 31 | 31.3 | 30 | 16.7 | 16.5 | 17.0 | |
| 40 | 35 | 27.9 | 28.2 | 28.3 | 41 | 22.1 | 21.3 | 21.7 | |
| 50 | 35 | 24.2 | 23.8 | 24.0 | 50 | 26.1 | 26 | 26.3 | |
| Posterior pelvic tilt 6° | 0 | 35 | 35.0 | 35 | 34.3 | 0 | 0.0 | 0 | 0.3 |
| 10 | 35 | 34.5 | 34.5 | 34.0 | 11 | 6.3 | 5.9 | 6.0 | |
| 20 | 35 | 33.3 | 33.8 | 33.3 | 20 | 11.3 | 11.5 | 11.3 | |
| 30 | 35 | 31.0 | 31.5 | 31.0 | 31 | 17.2 | 16.4 | 16.3 | |
| 40 | 35 | 27.9 | 28.5 | 27.3 | 41 | 22.1 | 22 | 22.0 | |
| 50 | 36 | 25.0 | 24.5 | 24.0 | 50 | 26.8 | 26.4 | 26.3 | |
| Anterior pelvic tilt 6° | 0 | 35 | 35.0 | 34.5 | 34.3 | 0 | 0.0 | 0.1 | 0.7 |
| 10 | 35 | 34.6 | 34.2 | 34.7 | 10 | 5.7 | 5.7 | 5.7 | |
| 20 | 35 | 33.3 | 33.4 | 33.7 | 20 | 11.3 | 11.2 | 11.0 | |
| 30 | 35 | 31.0 | 31 | 31.3 | 31 | 17.2 | 16.5 | 16.3 | |
| 40 | 35 | 28.2 | 28.5 | 29.7 | 40 | 21.6 | 21.5 | 22.0 | |
| 50 | 35 | 24.2 | 24.3 | 24.3 | 50 | 26.1 | 26 | 26.3 | |
* These values were calculated from the anatomic values from HipNav™; PT = HipNav™; MONT = Navitrack®; CN = computer navigation.
Discussion
Six different definitions have been used to measure and report the inclination and anteversion of the cup. Murray [34] originally defined anatomic, operative, and radiographic inclination and anteversion on the coronal plane. Authors who used CT scans and computer navigation changed the definition to the anterior pelvic plane [10, 11, 21–23, 25–27, 32]. The anterior pelvic plane deviates from the coronal plane in almost all patients. The placement of the cup may be in the safe zone by one definition but outside the safe zone by other definitions. It is nearly impossible to directly compare reports in the literature because of the mixed definitions of cup inclination and anteversion. Second, anteroposterior pelvic tilt plays an important role in accurate measurements, especially with CT scans and computer navigation, and is uncommonly included. Ignoring tilt is of clinical importance because there may still be a risk of dislocation, increased wear, and/or impingement, even if computer navigation is used to determine ideal cup position with reference to the anterior pelvic plane [13].
Four authors have recently studied the pelvic flexion-extension arc in different body positions [4, 9, 29, 35]. We determined this arc in our patients to confirm our measuring methods, and our patient population had results similar to those previously reported. Three of these authors studied the supine to standing positions and measured a change of –2°, −4°, and −5.4° pelvic extension as patients stood compared with our patients who also tilted posterior a mean −4.1° between supine and standing [4, 9, 35]. The preoperative to postoperative change in supine tilt in our patients was a mean of −4.8° posterior and this was similar to the −3.0° posterior found by Nishihara et al. [35]. In Babisch et al.’s study [4], the preoperative to postoperative change in supine tilt was a mean of 0.04° posterior in 10 patients with coxarthrosis, 2.5° anterior in 30 patients with dysplasia, and 1.9° anterior in all patients (dysplasia in 75% of patients). The authors who studied pelvic motion concluded it should be considered when implanting an acetabular component and a constant anteversion angle should not be selected [4, 9, 29, 35].
The solution to stability with variable pelvis angles is to consider the combined anteversion of the acetabulum and femur and not the acetabulum alone. Combined anteversion is nature’s method of hip stability and has been studied with THA with finite element reconstruction [47] and by computer navigation [14]. The acetabular anteversion is adjusted according to stem anteversion.
Currently, in most computer-assisted navigation systems that rely on the definition of the anterior pelvic plane, the plane is derived by identifying three osseous landmarks: the anterosuperior iliac spines and the pubic symphysis [9–11, 13, 23, 29]. Computer navigation techniques then use sophisticated algorithms and tracking systems to allow surgeons to assess the three-dimensional placement of instruments and prosthetic components during surgery. In measuring the outcome of the use of computer navigation systems, CT scans must be evaluated by the same definition on the same plane. If the radiographic anterior pelvic plane was used by the computer navigation, this same plane must be used for the CT scan. If the computer navigation plane was adjusted for tilt to the radiographic coronal plane, the CT scan must be converted. Plain radiographic measurements of acetabular alignment are not directly comparable to those made on the anterior pelvic plane [29].
All orthopaedic surgeons are familiar with the definition of inclination and anteversion from anteroposterior pelvic radiographs [1, 7, 12, 15, 19–21, 30, 31, 33, 34, 46]. Therefore, we recommend all measurements of inclination and anteversion on CT scans and by computer navigation be converted to the radiographic inclination and anteversion on the coronal plane. Measurement of CT scans and computer navigation is now based on the anterior pelvic plane. Converting to the radiographic coronal plane allows comparison to the measurements made for inclination and anteversion on the anteroposterior pelvic radiograph. It is important that a common technique of measurement is used and this provides the most useful common technique.
There is support for the coronal plane from other investigators. The anterior pelvic plane can vary by 10° or more from the coronal plane in some patients [9, 16, 29, 35, 41]. Therefore, there is support for the concept of functional orientation of the acetabular component, which is based on the longitudinal axis of the body (coronal plane) [9, 29, 35]. This was first suggested in 1990 by McCollum et al. [31] who recommended adjusting cup placement based on the longitudinal axis of the body as a means of reducing dislocation after THA. Pelvic orientation is unique to each patient and changes with patient position. Placing the acetabular component without considering the relationship of the pelvis to the longitudinal axis of the body can lead to dislocations, although the cup may have been placed ideally relative to the bony anatomy of the anterior pelvic plane [31, 44].
By using the radiographic coronal plane, the numeric values reported for inclination and anteversion will be the same as surgeons are accustomed to using. The confusion that can occur without a common measurement is illustrated by the recommendations of combined anteversion of the cup and stem in THA in three different publications. Widmer and Zurfluh [47] recommended a combined anteversion of 37.3°, which was based on Murray’s radiographic plane. Jolles et al. [24] recommended 40° to 60°, which was measured from a special lateral radiograph, and the anteversion of the cup is not compatible with Murray’s definition or routine radiographic measurement method. Komeno et al. [28] studied dislocation using two-dimensional CT scans and reported combined anteversion of 72.2° for patients with anterior dislocation, 27.4° in patients with posterior dislocation, and 47.8° as optimal. These numbers were obtained by using only a single cut through a two-dimensional CT scan and were not correlated to any of Murray’s plane. That is the reason the numbers are so high compared with numbers measured on the radiographic coronal plane with three-dimensional reconstructed CT scans.
We have summarized the different definitions of acetabular positions of inclination and anteversion used in the literature. Because there is no common measurement used, there has been confusion in reporting and comparing results. The anterior pelvic plane defines the acetabular position only in reference to the pelvis and therefore is a static measurement. The coronal plane defines the acetabular position in the functional coronal plane of the body. Second, surgeons are familiar with the measurement numbers of the radiographic coronal plane of plain radiographs. For these reasons, we recommend the common measurement used for reporting computer navigation and CT scan values be the radiographic coronal plane.
Appendix 1. Equations Connecting Anatomic, Operative, and Radiographic
Inclination and Anteversion on the Same Plane
| OI = asin (sin (AI) * cos (AV)) | (1) |
| OV = atan (tan (AI) * sin (AV)) | (2) |
| RI = atan (tan (AI) * cos (AV)) | (3) |
| RV = asin (sin (AI) * sin (AV)) | (4) |
| AI = acos (cos (OI) * cos (OV)) | (5) |
| AV = atan (cot (OI) * sin (OV)) | (6) |
| RI = atan (tan (OI) / cos (OV)) | (7) |
| RV = asin (cos (OI)* sin (OV)) | (8) |
| AI = acos (cos (RI) * cos (RV)) | (9) |
| AV = atan (tan (RV) / sin (RI)) | (10) |
| OI = asin (sin(RI) * cos (RV)) | (11) |
| OV = atan (tan (RV) / cos (RI)) | (12) |
AI = anatomic inclination; AV = anatomic version; OI = operative inclination; OV = operative version; RI = radiographic inclination; RV = radiographic version; formulas (2), (4), (6), (8), (10), and (12) are cited from Murray’s formulas [34].
Appendix 2. Converting Inclination and Anteversion Between the Anterior Pelvic Plane and the Coronal Plane [29]
| A0 = arcsin (- cos (A1) * cos (I1) * sin (α) + sin (A1) * cos (α)) | (13) |
| I0 = arcot (cot (I1) * cos (α) + sin (α) * tan (A1) / sin (I1)) | (14) |
AP = pelvic tilt; when converting the anteversion from the anterior pelvic plane to the coronal plane, I0 and A0 are the inclination and anteversion on the coronal plane; I1 and A1 are the inclination and anteversion on the anterior pelvic plane; the α is positive for the anterior pelvic tilt and negative for the posterior pelvic tilt; when converting anteversion from the coronal plane to the anterior pelvic plane, I0 and A0 are the inclination and anteversion on the anterior pelvic plane; I1 and A1 are the inclination and anteversion on the coronal plane; the α is negative for the anterior pelvic tilt and positive for the posterior pelvic tilt.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK. Anteversion of the acetabular cup. Measurement of angle after total hip replacement. J Bone Joint Surg Br. 1986;68:409–413. [DOI] [PubMed]
- 2.Anda S, Svenningsen S, Dale LG, Benum P. The acetabular sector angle of the adult hip determined by computed tomography. Acta Radiol Diagn (Stockh). 1986;27:443–447. [DOI] [PubMed]
- 3.Anda S, Svenningsen S, Grontvedt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum. A radiographic, computed tomographic and clinical investigation. Acta Radiol. 1990;31:389–394. [PubMed]
- 4.Babisch JW, Layher F, Amiot LP. The rationale for tilt-adjusted acetabular cup navigation. J Bone Joint Surg Am. 2008;90:357–365. [DOI] [PubMed]
- 5.Blendea S, Eckman K, Jaramaz B, Levison TJ, Digioia AM 3rd. Measurements of acetabular cup position and pelvic spatial orientation after total hip arthroplasty using computed tomography/radiography matching. Comput Aided Surg. 2005;10:37–43. [DOI] [PubMed]
- 6.Chen E, Goertz W, Lill CA. Implant position calculation for acetabular cup placement considering pelvic lateral tilt and inclination. Comput Aided Surg. 2006;11:309–316. [DOI] [PubMed]
- 7.Coventry MB, Beckenbaugh RD, Nolan DR, Ilstrup DM. 2,012 total hip arthroplasties. A study of postoperative course and early complications. J Bone Joint Surg Am. 1974;56:273–284. [PubMed]
- 8.D’Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW Jr. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–321. [DOI] [PubMed]
- 9.DiGioia AM, Hafez MA, Jaramaz B, Levison TJ, Moody JE. Functional pelvic orientation measured from lateral standing and sitting radiographs. Clin Orthop Relat Res. 2006;453:272–276. [DOI] [PubMed]
- 10.DiGioia AM, Jaramaz B, Blackwell M, Simon DA, Morgan F, Moody JE, Nikou C, Colgan BD, Aston CA, Labarca RS, Kischell E, Kanade T. The Otto Aufranc Award. Image guided navigation system to measure intraoperatively acetabular implant alignment. Clin Orthop Relat Res. 1998;355:8–22. [DOI] [PubMed]
- 11.Digioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364. [DOI] [PubMed]
- 12.Dorr LD, Bechtol CO, Watkins RG, Wan Z. Radiographic anatomic structure of the arthritic acetabulum and its influence on total hip arthroplasty. J Arthroplasty. 2000;15:890–900. [DOI] [PubMed]
- 13.Dorr LD, Hishiki Y, Wan Z, Newton D, Yun A. Development of imageless computer navigation for acetabular component position in total hip replacement. Iowa Orthop J. 2005;25:1–9. [PMC free article] [PubMed]
- 14.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res. 2007;465:92–99. [DOI] [PubMed]
- 15.Dorr LD, Wan Z. Causes of and treatment protocol for instability of total hip replacement. Clin Orthop Relat Res. 1998;355:144–151. [DOI] [PubMed]
- 16.Eckman K, Hafez MA, Ed F, Jaramaz B, Levison TJ, Digioia AM 3rd. Accuracy of pelvic flexion measurements from lateral radiographs. Clin Orthop Relat Res. 2006;451:154–160. [DOI] [PubMed]
- 17.Eddine TA, Migaud H, Chantelot C, Cotten A, Fontaine C, Duquennoy A. Variations of pelvic anteversion in the lying and standing positions: analysis of 24 control subjects and implications for CT measurement of position of a prosthetic cup. Surg Radiol Anat. 2001;23:105–110. [DOI] [PubMed]
- 18.Haaker RG, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007;22:151–159. [DOI] [PubMed]
- 19.Harris WH. Advances in surgical technique for total hip replacement: without and with osteotomy of the greater trochanter. Clin Orthop Relat Res. 1980;146:188–204. [PubMed]
- 20.Hassan DM, Johnston GH, Dust WN, Watson LG, Cassidy D. Radiographic calculation of anteversion in acetabular prostheses. J Arthroplasty. 1995;10:369–372. [DOI] [PubMed]
- 21.Herrlin K, Pettersson H, Selvik G. Comparison of two- and three-dimensional methods for assessment of orientation of the total hip prosthesis. Acta Radiol. 1988;29:357–361. [PubMed]
- 22.Jaramaz B, DiGioia AM 3rd, Blackwell M, Nikou C. Computer assisted measurement of cup placement in total hip replacement. Clin Orthop Relat Res. 1998;354:70–81. [DOI] [PubMed]
- 23.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179. [DOI] [PubMed]
- 24.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty. 2002;17:282–288. [DOI] [PubMed]
- 25.Kalteis T, Handel M, Bathis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88:163–167. [DOI] [PubMed]
- 26.Kalteis T, Handel M, Herold T, Perlick L, Baethis H, Grifka J. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. Int Orthop. 2005;29:272–276. [DOI] [PMC free article] [PubMed]
- 27.Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup—accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58:294–300. [DOI] [PubMed]
- 28.Komeno M, Hasegawa M, Sudo A, Uchida A. Computed tomographic evaluation of component position on dislocation after total hip arthroplasty. Orthopedics. 2006;29:1104–1108. [DOI] [PubMed]
- 29.Lembeck B, Mueller O, Reize P, Wuelker N. Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop. 2005;76:517–523. [DOI] [PubMed]
- 30.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed]
- 31.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res. 1990;261:159–170. [PubMed]
- 32.Mian SW, Truchly G, Pflum FA. Computed tomography measurement of acetabular cup anteversion and retroversion in total hip arthroplasty. Clin Orthop Relat Res. 1992;276:206–209. [PubMed]
- 33.Muller ME. Proceedings: the present state of total hip joint prosthesis [in German]. Z Orthop Ihre Grenzgeb. 1974;112:933–938. [PubMed]
- 34.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. [DOI] [PubMed]
- 35.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140–151. [DOI] [PubMed]
- 36.Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163. [DOI] [PubMed]
- 37.Pettersson H, Gentz CF, Lindberg HO, Carlsson AS. Radiologic evaluation of the position of the acetabular component of the total hip prosthesis. Acta Radiol Diagn (Stockh). 1982;23:259–263. [DOI] [PubMed]
- 38.Pierchon F, Pasquier G, Cotten A, Fontaine C, Clarisse J, Duquennoy A. Causes of dislocation of total hip arthroplasty. CT study of component alignment. J Bone Joint Surg Br. 1994;76:45–48. [PubMed]
- 39.Pradhan R. Planar anteversion of the acetabular cup as determined from plain anteroposterior radiographs. J Bone Joint Surg Br. 1999;81:431–435. [DOI] [PubMed]
- 40.Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum in patients with idiopathic increased anteversion of the femoral neck. Acta Orthop Scand. 1982;53:847–852. [DOI] [PubMed]
- 41.Richolt JA, Effenberger H, Rittmeister ME. How does soft tissue distribution affect anteversion accuracy of the palpation procedure in image-free acetabular cup navigation? An ultrasonographic assessment. Comput Aided Surg. 2005;10:87–92. [DOI] [PubMed]
- 42.Robinson A. Pelvis. In: Robinson A, ed. Cunningham’s Text-book of Anatomy. 5th Ed. New York: William Wood and Company; 1918:255–260.
- 43.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. [DOI] [PubMed]
- 44.Tang WM, Chiu KY. Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthroplasty. 2000;15:52–58. [DOI] [PubMed]
- 45.Visser JD, Konings JG. A new method for measuring angles after total hip arthroplasty. A study of the acetabular cup and femoral component. J Bone Joint Surg Br. 1981;63:556–559. [DOI] [PubMed]
- 46.Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19:387–390. [DOI] [PubMed]
- 47.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. [DOI] [PubMed]
- 48.Wolf A, Digioia AM 3rd, Mor AB, Jaramaz B. Cup alignment error model for total hip arthroplasty. Clin Orthop Relat Res. 2005;437:132–137. [DOI] [PubMed]