Abstract
Initial fixation of the femoral component in hip resurfacing is key to the enduring survival of the prosthesis. Cementing the metaphyseal stem increases the interface area between bone and cement. We compared the clinical and survivorship results of two groups in a cohort of 1000 hips (838 patients) implanted with Conserve® Plus hip resurfacing; one group was resurfaced with a cemented metaphyseal stem (400 hips; Group 1) and the other with a press-fit stem (600 hips; Group 2). We carried out a time-dependent analysis to determine the indications for cementing the stem. The 5-year Kaplan-Meier survival estimate was 98.2% for Group 1 and 94.4% for Group 2, using any revision as an endpoint. Femoral aseptic failure was reduced in Group 1 compared to Group 2. Cementing the metaphyseal stem is particularly effective for hips with a small femoral component size (< 48 mm) and hips with large femoral defects (> 1 cm). There was no difference between groups in incidence of femoral neck narrowing or femoral neck fractures. Longer followup is needed to determine if cementing the stem can be detrimental to the long-term durability of the femoral implant.
Level of Evidence: Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The results of metal-on-metal resurfacing already far surpass those of previous resurfacing designs [2, 8–10, 12, 19]. However, early loosening of the femoral component has been an issue and our previous reports identified risk factors such as large femoral defects, small component size, and suboptimal femoral component cementing technique [1, 7]. Improvements to the cementing technique reportedly reduce radiolucencies around the metaphyseal stem and femoral component loosening [6]. In addition to these surgical technique modifications, the cementing of the metaphyseal stem (initially designed for component alignment purposes) increases the area of the bone-cement interface and enhance initial fixation of the component. However, a concern about potential stress shielding in the femoral neck due to stem cementation has been raised in a recent finite-element analysis study [18] and warrants the need for a clinical study to determine the indications and limitations of this technique. Our hypotheses were that cementing the metaphyseal stem is an effective method to reduce femoral component loosening, particularly in hips with known risk factors, without affecting the clinical results of the procedure.
The purpose of the present study was twofold: to compare the clinical and survivorship results of a cohort of hips resurfaced with a cemented metaphyseal stem with those of hips resurfaced with a press-fit stem, and to determine the effects of these two methods of femoral component fixation on implant survival, in groups of patients with and without risk factors known to affect the survivorship results of the procedure.
Materials and Methods
We retrospectively reviewed 838 patients (1000 hips) who underwent hybrid metal-on-metal resurfacing between 26 November 1996 and 5 September 2006, while 375 patients (439 hips) received other devices during the same period. Of these 838 patients, 339 (400 hips) had a metaphyseal stem cemented (Group 1) and 499 patients (600 hips) had the stem left press-fit (Group 2). The resurfacing system used in all hips was the Conserve® Plus device (Wright Medical Technology, Inc, Arlington, TN). The average age of the patients was 50.0 years, with 75% male and 25% female. The two cementing techniques (stem cemented or left press-fit) were previously described [3]. Briefly, when the stem is left press fit, no acrylic is placed on the stem nor is any pressurized into the stem hole prior to component insertion, after the dome suction device is removed. When the stem is cemented, the stem is coated with a thin layer of doughy acrylic, the dome suction device is removed and acrylic is then finger pressurized into the hole for 30 to 45 seconds. For both techniques the intertrochanteric suction device remains active until the femoral component has been pressurized onto the reamed femoral head and the cement has set. The indications for cementing the stem evolved over time, including two series of consecutive hips cemented or left press fit regardless of risk factors. The hips from Groups 1 and 2 were comparable in incidence of femoral defects and surface arthroplasty risk index scores [7], but a higher (p = 0.0000) proportion (48.5%) of the devices from Group 2 were implanted with the early (first-generation) femoral component fixation technique versus only 2.3% in Group 1 (Table 1). The mean followup for the whole cohort was 5.8 years (range, 1.4–11.2 years) with 4.1 years (range 1.4 to 10.3) for group 1 and 6.1 years (range 1.4 to 11.2) for group 2. Three patients were lost to followup, two of them having moved without leaving any contact information, and one of whom was an illegal immigrant who was deported.
Table 1.
Comparative demographics and risk factors for hips with cemented stems (Group 1, n = 400) and hips with press-fit stems (Group 2, n = 600)
| Demographic/risk factor | Group 1 | Group 2 | p value |
|---|---|---|---|
| Age at surgery* (years) | 50.8 (14–78) | 49.6 (15–72) | 0.0802 |
| Male/female (%) | 65.5/34.5 | 80.3/19.7 | 0.0077 |
| Femoral component size* (mm) | 47.2 (36–54) | 47.7 (36–58) | 0.0454 |
| Cysts greater than 1 cm (%) | 37.0 | 34.3 | 0.4875 |
| Surface arthroplasty risk index* | 2.5 (0–6) | 2.4 (0–6) | 0.2081 |
| Body mass index* | 26.2 (17.5–40.4) | 27.3 (18.3–46.4) | 0.0001 |
| First-generation femoral component fixation technique (%) | 2.3 | 48.5 | 0.0001 |
* Values are expressed as means with ranges in parentheses.
The patients were followed 6 weeks, four months, one year and yearly thereafter. Followup visits included clinical data collection through the use of scannable questionnaires and radiographic studies. We (HCA, MLD) used the UCLA hip scoring system [7] and the Harris hip score [13] as disease-specific evaluations and the SF-12 [20] as an assessment of quality of life.
We (HCA, MLD) performed a radiographic review from anteroposterior radiographs to identify all hips with a narrowing of the femoral neck equal to or greater than 10% of the original diameter of the neck [2, 14]. We also noted the presence of radiolucencies around the metaphyseal stem as described in a previous publication [2]. Aseptic failure was defined as the revision of a component for reasons other than sepsis, specifically the loosening of a component or a femoral neck fracture.
We performed a time-dependent comparison using the log-rank test between the two groups because most of the prostheses with cemented stems were implanted after hip #356. The time to revision for any reason was used as an endpoint to calculate the Kaplan-Meier survival estimates in which all patients with a time to last follow-up greater than 0 were taken into consideration [11]. Then we used the log-rank test in varying conditions of component size (less than 48 mm vs. 48 mm or greater) and femoral bone quality (femoral defect size less than 1 cm vs. 1 cm or greater [1]) to determine usable guidelines for the indication of stem cementation. For this second test, we used the time to revision for aseptic failure of the femoral component (ie, loosening of the femoral component or fracture of the femoral neck) as an endpoint to assess more specifically the effect of cementing the stem on these two dominant modes of failure. All survivorship calculations and comparisons were performed using Stata statistical software package (Stata Corp., College Station, TX).
Results
The postoperative clinical scores were similar between the two groups except for the mental component of the SF-12, which was higher (p = 0.0138) for Group 2 (Table 2). Thirty-four hips underwent a revision of at least one of the components in this series. Thirty-three were converted to THA (including 24 revisions of the femoral component only) and one was maintained as a resurfacing after revision of the acetabular component only. There were five failures in Group 1, but none due to femoral component aseptic loosening. There were three femoral neck fractures, one sepsis, and one protrusion of the acetabular component. The mean time to revision for Group 1 was 11.1 months (range 2.5 to 31.7). There were 29 failures in Group 2, 20 due to aseptic loosening of the femoral component, seven neck fractures, one sepsis, and one recurrent subluxation. The mean time to revision for group 2 was 45.7 months (range 1.4 to 103.4). The details of these failures and other complications that did not warrant reoperation have been published elsewhere [5]. The Kaplan-Meier survivorship at 5 years was similar (p = 0.123) in Group 1 and Group 2 (98.2%, 95% confidence interval, 95.4%–99.3% versus 94.4%, 95% confidence interval, 91.4%–96.4%). However, using the time to aseptic femoral failure only (femoral neck fracture or femoral component loosening) as an endpoint, the survivorship was higher (p = 0.047) in Group 1.
Table 2.
Postoperative scores for hips with cemented stems (Group 1, n = 400) and hips with press-fit stems (Group 2, n = 600)
| Postoperative score* | Group 1 | Group 2 | p value |
|---|---|---|---|
| UCLA hip scores | |||
| Pain | 9.4 (6–10) | 9.4 (2–10) | 0.1605 |
| Walking | 9.6 (4–10) | 9.6 (3–10) | 0.5102 |
| Function | 9.5 (3–10) | 9.5 (3–10) | 0.9291 |
| Activity | 7.4 (3–10) | 7.6 (2–10) | 0.0532 |
| SF-12 | |||
| Physical | 50.8 (23–63) | 51(17–63) | 0.6862 |
| Mental | 54.6 (14–68) | 53 (10–68) | 0.0138 |
| Harris hip score | 94 (63–100) | 92.8 (38–100) | 0.776 |
* Values are expressed as means with ranges in parentheses.
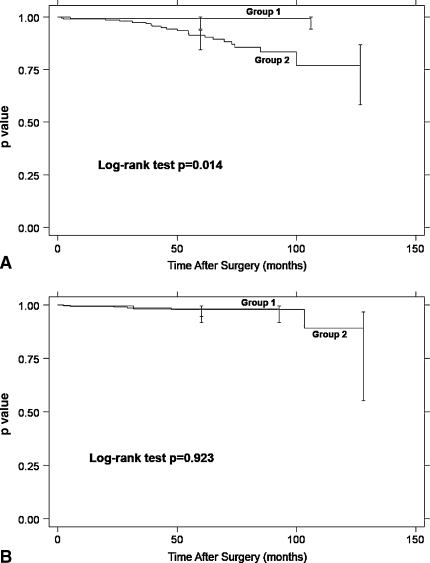
The cemented stems had better (p = 0.014) survivorship (Fig. 1A) using aseptic femoral failure only as an endpoint for small femoral component sizes (< 48 mm, n = 385). For large component sizes (≥ 48, n = 615), cemented and noncemented stems had similar (p = 0.923) survival (Fig. 1B).
Fig. 1A–B.
Comparative survivorship analyses of hips resurfaced with a cemented metaphyseal stem (Group 1) or with a press-fit stem (Group 2) are shown for (A) hips of small component sizes (femoral component < 48 mm in diameter, n = 385) and (B) hips of large component sizes (femoral component ≥ 48 mm in diameter, n = 615). Revision for aseptic femoral failure (femoral neck fracture and femoral component loosening) was used as an endpoint. Note: The difference between the two curves is associated with a difference in the rate of femoral component loosening since the incidence of femoral neck fractures was not different between Groups 1 and 2.
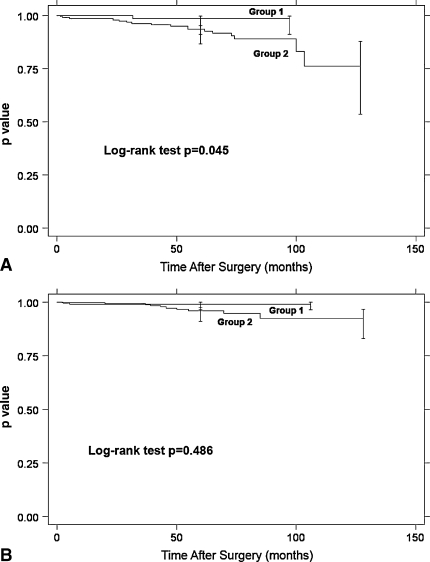
Similarly, for the hips presenting large femoral head defects (> 1 cm, n = 354), the cemented stems had better (p = 0.045) survivorship (Fig. 2A), whereas for the hips with small defects (≤ 1 cm) or no defects (n = 646), survival was similar (p = 0.486) (Fig. 2B).
Fig. 2A–B.
Comparative survivorship analyses of hips resurfaced with a cemented metaphyseal stem (Group 1) or with a press-fit stem (Group 2) are shown for (A) hips with large femoral defects (> 1 cm, n = 354) and (B) hips with small femoral defects (≤ 1 cm) or no defect (n = 646). Revision for aseptic femoral failure (femoral neck fracture and femoral component loosening) was used as an endpoint.
The two groups had similar (p = 0.864) survival using femoral neck fractures alone as an end point. However, the failure rate was higher (p = 0.017) in Group 2 using aseptic loosening of the femoral component alone as an end point; there were no femoral loosening or hips with metaphyseal stem radiolucencies in Group 1.
Twenty four hips (2.4%) exhibited narrowing of the femoral neck of 10% or more. Group1 and Group 2 had a similar (p = 0.134) incidence (six or 1.5% versus 18 or 3%, respectively).
Discussion
Cementing the metaphyseal stem increases the area of the bone-cement interface and enhances the initial fixation of the component. We hypothesized that cementing the stem would reduce femoral component loosening, particularly in hips with known risk factors.
The main limitation of our study is that the bone preparation and cementing techniques have evolved over time during the series and the efficacy of the second-generation fixation technique was demonstrated for components resurfaced with a press-fit metaphyseal stem [6]. Group 1 may have benefited from these technique improvements more than Group 2 because most the components with a cemented stem were implanted after hip #356 in our series. However, there were no failures or evidence of early signs of femoral loosening in any of the components implanted with a cemented stem and the first-generation fixation technique. Also, our data show the effect of stem cementation for the Conserve® Plus System with an average followup of 4.1 years and may not be applicable to other systems.
At short- to medium-term followup, our data suggest a beneficial effect of cementing the stem on one mode of failure (the aseptic loosening of the femoral component) but did not alter the incidence of femoral neck fractures (which is low with 1% overall). This result is of importance as no other attempt to clinically evaluate the effects of this technique has been reported in the literature. At the beginning of the series (up to hip #356), our indications for cementing the stem were restricted to hips with extremely severe femoral head defects (20 hips). Then a series of 92 hips had the stem cemented regardless of femoral head defect size, followed by a series of 83 hips all implanted with a press-fit metaphyseal stem, to study more particularly the effects of cementing the stem on the results of resurfacing. The remaining hips of the series followed the indications provided by our early results and the stem was cemented essentially in cases with large head defect, small component size, or both. Group 2 had a lower survivorship than group 1 despite a higher BMI value, which has previously been associated with a good performance of the device possibly explained by a lower activity level and larger component size [4, 16]. This supports the effectiveness of cementing the stem to prevent early failures of the femoral component. Based on our current data, it seems that cementing the stem could be a satisfactory technique for all cases. However, it is not currently possible to predict the effect of cementation of the stem on the long-term results, and this should lead the resurfacing surgeon to use this technique only when deemed necessary. Stress shielding around a fixed metaphyseal stem was reported by Kim et al. [15] in a canine study that featured cementless resurfacing femoral components with a porous-coated stem. This concern originally led the senior author (HCA) to design the Conserve® Plus femoral component with a smooth, press-fit metaphyseal stem and to cement the stem only in cases where the initial fixation might be insufficient.
Narrowing of the femoral neck after hip resurfacing has been observed with most current resurfacing designs [14, 17] and stress shielding has been cited as a possible cause for this phenomenon. In our study, we did not find any difference in the incidence of femoral neck narrowing between the hips with a cemented stem and the hips with a press-fit stem. This result indicates that the concerns of potential stress shielding raised by Little et al. [18] about the technique of cementing the metaphyseal stem do not appear to materialize from a clinical perspective with the current followup of our series.
Our results define our current indications for this surgical technique to increase surface area for fixation by cementing the stem: (1) patients undergoing resurfacing with a femoral component size smaller than 48 mm; (2) patients with a femoral head presenting defects single or multiple greater than 1 cm; and (3) patients with both of these risk factors.
Footnotes
One or more of the authors (HCA - MLD) have received funding from St Vincent Medical Center, Los Angeles, CA, and Wright Medical Technologies, Inc, Arlington, TN. Each author certifies that he has or may receive payments or benefits from a commercial entity related to this work.
Each author certifies that his or her institution has approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amstutz H, Ball S, Le Duff M, Dorey F. Hip resurfacing for patients under 50 years of age. Results of 350 Conserve Plus with a 2–9 year follow-up. Clin. Orthop Relat Res. 2007;460:159–164. [DOI] [PubMed]
- 2.Amstutz H, Beaulé P, Dorey F, Le Duff M, Campbell P, Gruen T. Metal-on-metal hybrid surface arthroplasty: two to six year follow-up.J. Bone Joint Surg Am. 2004;86:28–39. [PubMed]
- 3.Amstutz H, Beaulé P, Dorey F, Le Duff M, Campbell P, Gruen T. Metal-on-metal hybrid surface arthroplasty – Surgical technique. J. Bone Joint Surg Am. 2006;88(suppl 1 Part 2):234–249. [DOI] [PubMed]
- 4.Amstutz H, Le Duff M. Eleven years of experience with metal-on-metal hybrid hip resurfacing: a review of 1,000 ConservePlus. J Arthroplasty. 2008;23:36–43. [DOI] [PubMed]
- 5.Amstutz H, Le Duff M. Results of Conserve®Plus hip resurfacing. In: Amstutz HC, ed. Hip Resurfacing: Principles, Indications, Technique and Results. Philadelphia, PA: Elsevier; 2008:103–117.
- 6.Amstutz H, Le Duff M, Campbell P, Dorey F. The effects of technique changes on aseptic loosening of the femoral component in hip resurfacing Results of 600 Conserve Plus with a 3–9 year follow-up. J Arthroplasty. 2007;22:481–489. [DOI] [PubMed]
- 7.Amstutz H, Thomas B, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed]
- 8.Back D, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings. An independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329. [DOI] [PubMed]
- 9.Daniel J, Pynsent PB, McMinn D. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–188. [DOI] [PubMed]
- 10.De Smet K. Belgium experience with metal-on-metal surface arthroplasty. Orthop Clin North Am. 2005;36:203–213. [DOI] [PubMed]
- 11.Dorey F, Amstutz HC. The validity of survivorship analysis in total joint arthroplasty [see comments]. J Bone Joint Surg Am. 1989;71:544–548. [PubMed]
- 12.Grigoris P, Roberts P, Panousis K. The development of the Durom metal-on-metal hip resurfacing. Hip International. 2006;16(suppl 4):65–72. [DOI] [PubMed]
- 13.Harris W. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 14.Hing C, Young D, Dalziel R, Bailey M, Back D, Shimmin A. Narrowing of the neck in resurfacing arthroplasty of the hip: A radiological study. J Bone Joint Surg Br. 2007;89:1019–1024. [DOI] [PubMed]
- 15.Kim WC, Amstutz HC, O’Carroll PF, Hedley AK, Coster I, Schmidt I. Porous ingrowth in canine resurfacing hip arthroplasty: analysis of results with up to a 2-year follow-up. Hip. 1984:211–243. [PubMed]
- 16.Le Duff M, Amstutz H, Dorey F. Metal-on-metal hip resurfacing for obese patients. J Bone and Joint Surg Am. 2007;89:2705–2711. [DOI] [PubMed]
- 17.Lilikakis A, Vowler S, Villar R. Hydroxyapatite-coated femoral implant in metal-on-metal resurfacing hip arthroplasty: minimum of two years follow-up. Orthop Clin North Am. 2005;36:215–222. [DOI] [PubMed]
- 18.Little JP, Taddei F, Viceconti M, Murray DW, Gill HS. Changes in femur stress after hip resurfacing arthroplasty: response to physiological loads. Clin Biomech (Bristol, Avon). 2007;22:440–448. [DOI] [PubMed]
- 19.Treacy R, McBryde C, Pynsent P. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. [DOI] [PubMed]
- 20.Ware J, Kosinski M, Keller S. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed]