Abstract
Either excessive or insufficient cement penetration within the femoral head after hip resurfacing influences the risk of femoral failures. However, the factors controlling cement penetration are not yet fully understood. We determined the effect of femoral component design and cementation technique on cement penetration. Six retrieved femoral heads were resurfaced for each implant (BHR®, ASR®, Conserve Plus®, DuROM®, ReCAP®) using the manufacturers’ recommendations for implantation. In addition, the BHR was implanted using the Conserve Plus® high-viscosity cementation technique, “BHR/hvt,” and vice versa for the Conserve, “Conserve/lvt.” The average cement penetration was highest with BHR (65.62% ± 15.16%) compared with ASR® (12.25% ± 5.12%), Conserve Plus® (19.43% ± 5.28%), DuROM® (17.73% ± 3.96%), and ReCAP® (26.09% ± 5.20%). Cement penetration in BHR/hvt remained higher than all other implants equaling 36.7% ± 6.6%. Greater femoral component design clearance correlated with cement mantle thickness. Femoral component design in hip resurfacing plays a major role in cement penetration.
Introduction
Metal-on-metal hip resurfacing represents an alternative to THA in young, active patients with end-stage arthritis [6]. Although the initial experience of metal-on-polyethylene hip resurfacing was associated with high failure rates [2, 23, 26], the current generation of hip resurfacing with hybrid fixation (cementless acetabulum, cemented femur) combined with metal-on-metal bearings reportedly have promising early outcomes with survivorship rates of 94% to 99% at 4 to 5 years [1, 18, 41]. However, these results stem mainly from centers involved in the development of the implant and higher failure rates (eg, 6% at 2 to 5 years) are being reported from other centers [35, 38]. These discrepancies between centers of expertise and nonspecialized centers are most likely related to surgical technique as well as implant and patient selection.
With the resurgence of hip resurfacing in the treatment of end-stage hip arthritis, it is critical surgeons understand the appropriate indications and the key aspects of the surgical technique to avoid premature failures [7]. Currently, failure rates in the first 4 years are reportedly as high as 6% with the majority of failures occurring on the femoral side [18, 35, 38, 40]. Although the etiology and mechanisms of failure after hip resurfacing can be varied, current reports suggest aseptic loosening of the femoral component and fracture of the femoral neck are the leading causes of revision surgery [1, 3, 31, 38, 40].
In terms of surgical technique, varus positioning of the femoral component [12] and neck notching [8, 40] have been clearly identified as risk factors for short-term failures. Furthermore, with cement used as the primary method of fixation on the femoral side [20], optimal cementing technique will inevitably vary between different centers representing, like in THA, a risk factor for early failure [15, 19, 36]. More importantly, how one achieves sufficient cement penetration in hip resurfacing is influenced by several factors [14, 17, 22, 33], some of which can be controlled by the surgeon such as cement viscosity [33] and pulsatile lavage [22], whereas others such as femoral head bone quality [28] and implant design cannot be controlled.
Recent retrieval analyses of failed resurfacings demonstrate large variability in cement penetration within the femoral head between different implants [36] with excessive cement penetration correlating with implant loosening [16]. However, it remains unclear to which degree each factor leads to this large variability in cement penetration, ie, cement viscosity, femoral head bone quality, and/or component design. This is contrary to stem-type hip replacements in which cementation technique (timing of application, pressurization) as well as femoral component design and their relationship to the cement penetration and mantle have been studied extensively [19, 43]. By understanding the factors that control cement penetration after hip resurfacing, surgeons can better optimize their surgical technique to minimize the risk of early failure as well as provide better insight in terms of long-term implant performance.
We therefore compared the cement penetration and mantle thickness among five commonly used hip resurfacing component designs using the manufacturer’s recommended cementation technique. To determine the effect of design clearance of the femoral component on cement penetration and mantle thickness, we altered the cementation technique (high- and low-viscosity techniques) of two components with varying clearances.
Materials and Methods
We obtained 70 femoral heads with patients’ written informed consent as approved by our institution’s ethical review board. The heads were retrieved from patients younger than 70 years old undergoing elective THA for osteoarthritis and no prior hip surgery. Exclusion criteria included patients undergoing THA as a result of osteonecrosis, hip dysplasia, or fractures. We stored specimens in a −35°C freezer. Each femoral head was randomly assigned into the different groups using a number generator.
Bone mineral density was measured by a dual-energy xray absorptiometry (DEXA) scan as previously described by Trudel and associates [42]. To control for bone mineral density, we retained 42 of the 70 femoral heads that were within ± 1 standard deviation of the sample mean for the study. The mean bone mineral density as measured by the DEXA scans was similar in seven groups (five groups for comparison of designs and two groups for comparison of cement viscosity; analysis of variance, p = 0.98).
Five different hip resurfacing femoral components were implanted: Articular Surface Replacement® (“ASR®”; DePuy, Warsaw, IN), Birmingham Hip Resurfacing® (“BHR”; Smith & Nephew, London, UK), Conserve Plus® (“Conserve Plus”; Wright Medical Technology, Arlington, TN), DuROM® (“DuROM”; Zimmer Inc, Warsaw, IN), and ReCAP® (“ReCAP”; Biomet Inc, Warsaw, IN). We determined the clearance using digital calipers by measuring the inner diameter of the femoral component at its edge and the cutting diameter of the reamer at the corresponding location. Radial clearance was defined as half of the difference between these two diameters (Table 1). Six femoral heads were resurfaced for each of the five different femoral implant designs by an experienced hip resurfacing surgeon (PEB). The resurfacing was carried out according to the specifications of each manufacturer’s technical guidelines (Table 2). We used Simplex® P radio-opaque bone cement (Stryker Canada, Hamilton, Ontario, Canada) in this study. The working time along with the manufacturer’s recommendation were used to achieve the desired lower or higher viscosity cement state. The BHR was cemented using the cement in low-viscosity state, which was poured into the femoral component and then pressurized onto the reamed femoral head at 1 minute. We cemented the remaining four implants using cement in a higher viscosity state with implantation performed between 2 and 4 minutes according to the manufacturer’s recommendation.
Table 1.
Design specifications of the five implants used for resurfacing
| Implant | Implant geometry | Radial clearance (mm)* | |
|---|---|---|---|
| As provided by manufacturer | Measured | ||
| BHR | Conical | Not disclosed | 0.2 |
| ASR® | Conical (3° taper) | Not disclosed | 0.1 |
| Conserve Plus® | Cylindrical | 1.00 | 1.0 |
| DuROM® | Cylindrical | Not disclosed | 0.7 |
| ReCAP® | Cylindrical | 0.50 | 0.6 |
* Radial clearance is defined as half of the difference between the inner diameter of the femoral component at its edge and the cutting diameter of the reamer at the corresponding location.
Table 2.
Manufacturers’ recommended cementation techniques and recommended timing of implantation for each implant design along with the measured cementation time*
| Implant | Cement placed in cup | Cement placed on femoral head | Cementation time (minutes) |
|---|---|---|---|
| BHR | Implant is filled with cement to the top | No | 1 |
| ASR® | No | Prepared femoral head is coated with cement | 2.5 |
| Conserve Plus® | Implant is filled with cement to the chamfer | Prepared femoral head is coated with cement | 4 |
| DuROM® | Implant is filled with cement to the level of the inner recess | No | 2.5 |
| ReCAP® | Implant is filled with cement | Prepared femoral head is coated with cement | 4 |
* Timer was started when adding the liquid monomer to the powder.
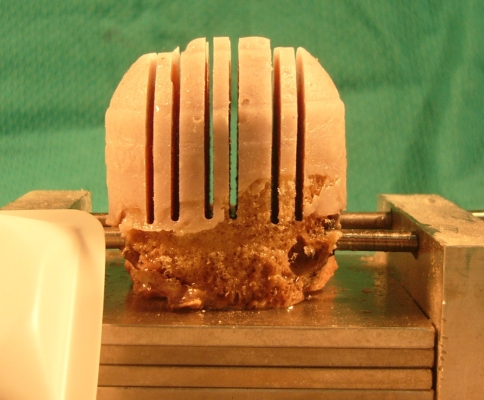
We mounted all femoral heads on custom-made fixtures using Kirschner wires to facilitate and standardize their preparation (Fig. 1). The surgical technique was followed for each of the implants. The margin of the trial was marked on the femoral neck with a surgical marker. We then irrigated the prepared femoral head with a pulse lavage and subsequently dried it. Before cementation, the inner side of the component was coated with a thin layer of petroleum jelly to facilitate its removal after cement curing. We added methylene blue (0.2 cc) to each pack of cement to facilitate subsequent digital measurements. The implant was impacted to the premarked level on the prepared femoral head (Fig. 1A). Constant pressure was then applied until the cement was fully cured.
Fig. 1.
The femoral head was mounted on a custom-designed fixture for head preparation, implantation, and sectioning. The figure illustrates the femoral head after sectioning using a diamond saw blade.
To determine the effects of cement viscosity, the BHR femoral component was implanted using the higher viscosity cementation technique of the Conserve Plus® named BHR/hvt, whereas the Conserve Plus® was implanted using the lower viscosity cementation technique of the BHR named Conserve Plus/lvt. We selected these two implants because they represented the greatest difference in both implant clearance and cementation technique and have the longest clinical track record [4, 41]. Total amount of cement used for each head was weighed before implantation.
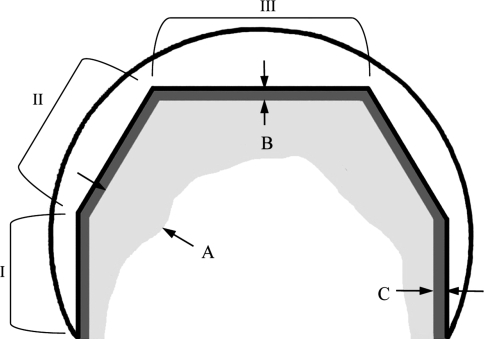
Once cement curing was complete, we subsequently removed all implants from the femoral head except the DuROM, which required sectioning with the implant in place because the implant has a groove interlocking the cement. All femoral heads were cut as described by Campbell and associates [16] into three 2.6-mm longitudinal sections using a diamond saw blade. We obtained three sections at the 25%, midline, and 75% mark (Fig. 1). The sections were then digitally photographed, radiographed, and subsequently analyzed using an image analysis software program by a single observer (KS) blinded to implant type (Image J, version 1.34; National Institutes of Health, Bethesda, MD) (Fig. 2). Cement penetration was calculated as a percentage of bone interdigitated by cement to the total area of bone under the implant. We also calculated the mean depth of cement penetration for each femoral head by taking perpendicular depth measurements at 1-mm intervals along the periphery of the prepared bone. We also recorded the mean depths for the side, chamfer, and dome sections of the prosthesis. The cement mantle thickness was defined as the distance between the prepared bone and the outer edge of the cement mantle (Fig. 2) and measured along the sides of the prosthesis (Zone I) and at the dome (Zone III).
Fig. 2.
The diagram shows the different parameters measured on the digital images and radiographs as well as the three defined zones of the prosthesis: side (I), chamfer (II), and dome (III). Cement penetration depth was measured perpendicular to the implant (A), cement mantle height was measured at the dome (B), and cement mantle thickness was measured at the side (C). Cement penetration was calculated as a percentage of bone interdigitated by cement to the total area of bone under the implant. The mean depths of penetration were also measured for each zone by averaging the depth of penetration at 1-mm intervals.
We used descriptive statistics to examine measures of central tendency (mean, median, mode) and dispersion (standard deviation [SD]). All values are reported as means of 18 values (six femoral heads x three sections per head) ± SD unless otherwise stated. We compared differences across groups for penetration parameter means using one-way analysis of variance (ANOVA). For each measured parameter, we ran an ANOVA model comparing the different groups and evaluated overall group differences using the F statistic. All possible pairwise comparisons between groups were further analyzed using the Tukey correction to identify specific group differences when p < 0.05. The comparisons of implantation with cements of differing viscosities were performed using unpaired t-tests. All analyses were performed using SAS version 9 (SAS Institute, Cary, NC).
Results
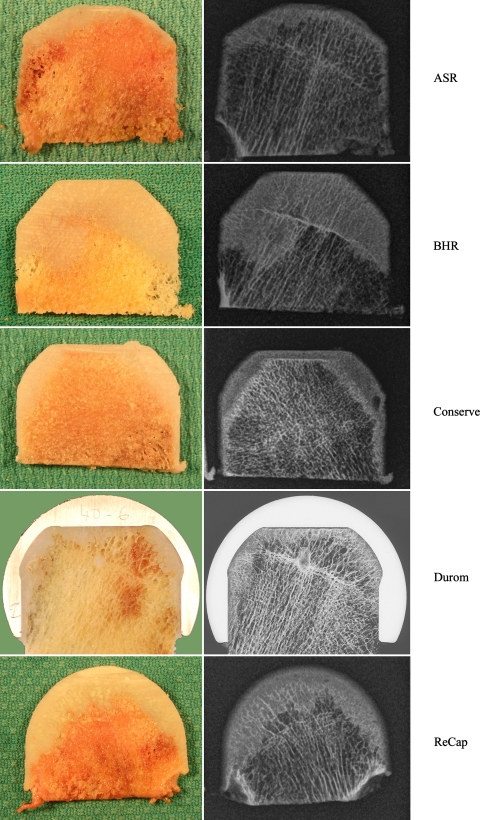
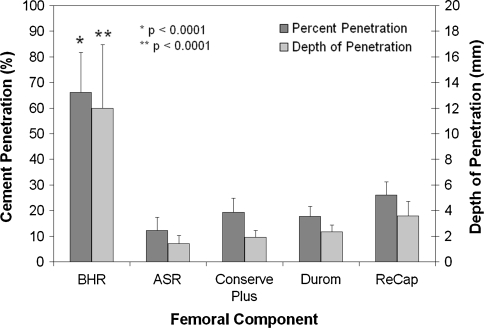
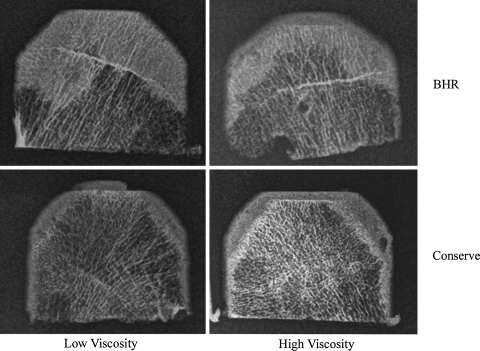
The average cement penetration was greatest in the BHR® (66.2% ± 15.5%) compared with the others (ASR® 12.3% ± 5.1%, Conserve Plus® 19.3% ± 5.5%, DuROM® 17.7% ± 4.0%, ReCAP® 26.1% ± 5.2%) (Figs. 3, 4). The BHR’s cement penetration was greater (p < 0.0001) than all of the other four groups. We observed the same with the mean depth of overall penetration (Fig. 5) (p < 0.0001) and within the three different zones (Table 3) (p < 0.0001).
Fig. 3.
Digital images (left panel) and radiographs (right panel) are shown for the 25% mark of ASR®, BHR, Conserve Plus®, DuROM®, and ReCAP®.
Fig. 4.
Percent and mean depth of cement penetration (mean ± standard deviation) were highest with BHR as compared with all other implants using the manufacturers’ recommended cementation techniques.
Fig. 5.
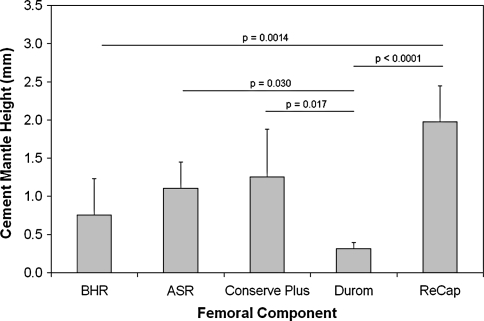
The cement mantle height (mean ± standard deviation) for the DuROM® was lower than that for the Conserve Plus®, ASR®, and ReCAP® and the ReCAP® was higher than that for the ASR®, BHR, and DuROM®.
Table 3.
Mean depth of cement penetration measured at the side, chamfer, and dome of the femoral head for each implant design*
| Implant | Dome depth (mm) | Chamfer depth (mm) | Side depth (mm) |
|---|---|---|---|
| BHR | 13.9 ± 5.5† | 13.1 ± 3.7† | 11.0 ± 4.7† |
| ASR® | 1.7 ± 1.1 | 1.7 ± 0.9 | 1.0 ± 0.3 |
| Conserve Plus® | 2.4 ± 1.2 | 2.6 ± 1.0 | 1.4 ± 0.3 |
| DuROM® | 2.4 ± 0.8 | 2.8 ± 0.9 | 1.7 ± 0.4 |
| ReCAP® | N/A | N/A | N/A |
* Mean depth was measured perpendicularly at 1-mm intervals along the periphery of the femoral head for each section and reported as a mean of the average for each femoral head ± standard deviation; †statistical difference between BHR and all other groups (analysis of variance, p < 0.0001); N/A = not available as a result of semicircular shape of inner geometry of the prosthesis.
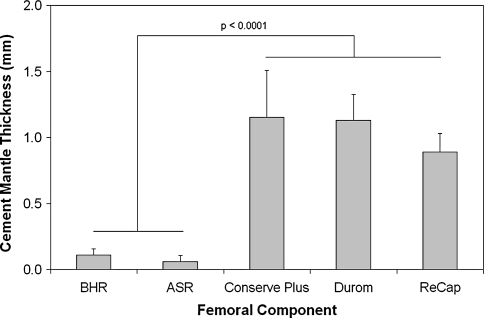
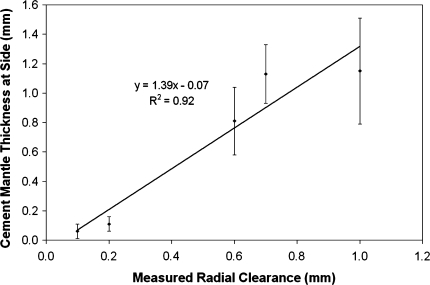
The thickness of the cement mantle at the dome of Zone III (Fig. 3) varied among the different groups (Fig. 5). It was thickest with the ReCAP® (2.0 ± 0.5 mm), which was higher than the BHR (0.8 ± 0.5 mm, p = 0.0014) and the DuROM® (0.3 ± 0.1 mm, p < 0.0001), approached significance when compared with the ASR® (1.2 ± 0.4 mm, p = 0.0548) but was not different from the Conserve Plus® at 1.3 ± 0.6 mm. In addition, the DuROM® cement mantle in Zone III was lower than ASR® (p = 0.0302), Conserve Plus® (p = 0.0167), and ReCAP® (p < 0.0001). The thickness of the cement mantle at the sides (Zone I in Fig. 3) was greater (p < 0.0001) with Conserve Plus® (1.2 ± 0.4 mm), DuROM® (1.1 ± 0.2 mm), and ReCAP® (0.8 ± 0.2 mm) as compared with ASR® (0.1 ± 0.1 mm) and BHR (0.1 ± 0.1 mm) (Fig. 6). We found a positive correlation (r2 = 0.92) between the cement mantle thickness in Zone I and the measured radial clearance of the implant (Fig. 7).
Fig. 6.
Cement mantle thickness (mean ± standard deviation) on the sides of the femoral head was higher with the Conserve Plus®, DuROM®, and ReCAP® as compared with the BHR and ASR®.
Fig. 7.
Correlation is shown between mean cement mantle thickness at sides (mm) and measured radial clearance.
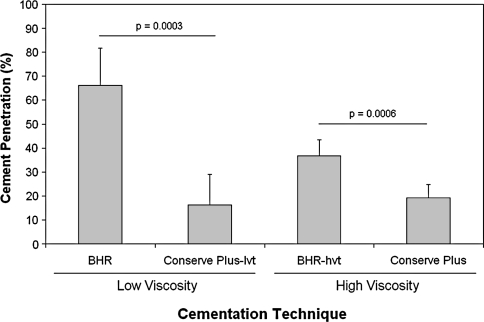
Using the low-viscosity cementation technique of the BHR, the Conserve Plus/lvt cement penetration remained lower (p = 0.0003) than the BHR® (16.3% ± 12.7% versus 66.2% ± 15.5%) (Fig. 8) (Table 4). Alternating to the higher viscosity cementation technique of the Conserve Plus®, the BHR/hvt cement penetration remained higher (p = 0.0006) than the Conserve Plus® (36.7% ± 6.6% versus 19.3% ± 5.5%). Similarly, both mean depth and maximal penetration were higher (Table 4) in the BHR group using the low- and high-viscosity cementation techniques when compared with the Conserve Plus®. The cement mantle thickness at the dome (Zone III) did not change when comparing the BHR® and Conserve Plus/lvt, whereas it was higher in the BHR/hvt when compared with the standard Conserve Plus®. In fact, in the BHR/hvt group, four of the six prostheses could not be seated to the premarked level on the femoral neck (Fig. 9). The side mantle thickness (Zone I) was higher in the Conserve Plus® using both low- and high-viscosity cementation techniques.
Fig. 8.
Percent cement penetration (mean ± standard deviation) for the BHR and Conserve Plus® implants with low- and high-viscosity cementation techniques is shown.
Table 4.
The BHR resulted in significantly higher overall percent cement penetration, mean depth, and maximal penetration as compared with the Conserve Plus® using both the lower- and higher-viscosity cementation techniques*
| Cement parameter measured | Lower-viscosity cementation technique | Higher-viscosity cementation technique | ||||
|---|---|---|---|---|---|---|
| BHR | Conserve Plus®-lvt | p value | Conserve Plus® | BHR-hvt | p value | |
| Cement penetration (%) | 66.2 ± 15.5 | 16.3 ± 12.7† | 0.0003 | 19.3 ± 5.5 | 36.7 ± 6.6† | 0.0006 |
| Mean depth (mm) | 12.0 ± 5.0 | 1.9 ± 1.5† | 0.003 | 1.9 ± 0.5 | 4.6 ± 1.1† | 0.0003 |
| Maximal penetration (mm) | 21.7 ± 7.3 | 4.7 ± 2.2† | 0.002 | 4.6 ± 1.9 | 9.7 ± 2.1† | 0.001 |
| Dome mantle height (mm) | 0.8 ± 0.5 | 0.5 ± 0.2 | NS | 1.3 ± 0.6 | 2.9 ± 0.7† | 0.002 |
| Side mantle thickness (mm) | 0.1 ± 0.1 | 1.1 ± 0.2† | 0.0001 | 1.3 ± 0.6 | 0.2 ± 0.1† | 0.001 |
* The BHR could not always be seated properly when using the higher-viscosity technique as reflected by the thicker cement mantle at dome in this group; the side mantle was thinner for the BHR in both cases; NS = nonsignificant.
Fig. 9.
Digital radiographs taken at the 25% mark demonstrate higher cement penetration for the BHR as compared with the Conserve Plus® implant for both the low-viscosity cementation technique (left panel) and the high-viscosity cementation technique (right panel). With the high-viscosity technique, four of six BHR implants could not be seated properly (in the current figure, Conserve is not seated also).
Discussion
Excessive cement penetration after hip resurfacing has been correlated with femoral component loosening [16]. Factors such as cement viscosity, pulse lavage, and femoral bone quality are known to influence cement penetration [13, 27, 28, 32, 33]. The effect of femoral component design or, more specifically, the clearance between the reamed bone and femoral component on cement penetration, is not yet understood. The aim of this study was first to compare cement penetration and mantle thickness after implantation in vitro with five commercially available hip resurfacing components using the manufacturer’s cementation technique. After this, the sole effect of the femoral component design clearance on cement penetration was investigated by alternating cementation techniques between two implants.
Our study has certain limitations. It is well known that other variables such as pressurization techniques, temperature, and humidity as well as the presence of blood can considerably impact cement penetration, the latter depending on femoral head vascularity [9]. We prepared femoral heads and cemented in vitro at room temperature. Although no blood was present and test conditions were not physiological, each parameter was kept constant to study the sole contribution of implant design and cementation technique on cement penetration; the experiments were performed in a controlled setting using fresh-frozen rather than fixed cadaveric femoral heads. More importantly, the effect of varying bone porosity on cement penetration was minimized by having all femoral heads within one SD for their bone mineral density measurements.
Our data demonstrate hip resurfacing femoral implants have a major effect on cement penetration within the femoral head. This difference was most striking when comparing the BHR with the four other implants. In terms of percent difference in mean cement penetration, the BHR on average had 39% to 53% more cement penetration with the ASR® design having the lowest overall. Interestingly, Campbell and associates [16] also found the BHR had the greatest amount of cement penetration averaging 58%, whereas the Conserve Plus had on average 35%, which is higher than we found. These results represent critical information for clinicians as well as manufacturers because all components were implanted according to the recommended manufacturers’ cementation technique and performed within a controlled environment in terms of bone mineral density and femoral head preparation. In addition, our results point out the importance of current and future recommendations on techniques of cementation, which cannot necessarily be used interchangeably between different implants and provide a baseline for clinical performance of these various implants in terms of cement fixation. However, despite the contrast in overall cement penetration between the BHR® and Conserve Plus®, both have comparable survivorship rates at 4 to 5 years [1, 18, 38]. In addition, because all of the femoral heads were prepared in an optimal fashion, we cannot account for effects of eccentric femoral head preparation as well as implant positioning, which can affect penetration and mantle thickness [17].
When looking at the overall depth of cement penetration within the femoral head, the findings were comparable to the percentage of cement penetration; however, depth of penetration provides insight for the potential of excessive heat generation during curing as well as fixation of the implant [16, 17]. Campbell and associates [16] reported 6 mm or more of cement penetration leads to temperatures sufficiently high (ie, greater than 50°C) to cause thermal necrosis of the surrounding bone. This initial insult to the fixation between bone and cement was extensively studied by Mjoberg and associates [34], who demonstrated the resorptive and reparative phase that follows could lead to instability of the implant followed by migration and eventually loosening of the prosthesis, which has been reported in the current generation of hip resurfacing [11]. In their retrieval analyses, both Little and associates [31] and Campbell and associates [16] also observed femoral neck fractures associated with necrotic bone as well as zones of complete avascularity. Similar to our results, when comparing the BHR and Conserve Plus, Campbell and associates [16] reported the BHR had the highest average depth of cement penetration and the Conserve Plus had the larger average cement mantle.
Although excessive penetration can put the bone at risk of thermal necrosis, a minimum amount of penetration is required for fixation. Noble and Swarts [37] suggested 3 to 5 mm of cement penetration is needed to achieve proper three-dimensional interlocking into cancellous bone, which was confirmed by other researchers [5, 30]. This would appear reasonable because 6 mm or more can cause excessive heat generation [16]. Although heat generation can be negated by cooling methods of irrigation and suction, Jansson and associates [25] reported increased cement penetration within the bone stiffens the cancellous bone increasing interface stresses and putting the underlying bone at risk of fatigue failure as postulated by Huiskes et al. [24]. This can be further compounded by the fact that a considerable percentage of patients with hip resurfacing participate in impact sports [18, 29].
Our data also demonstrate component design, specifically the clearance between the component and reamed femoral head, is a critical determinant of cement penetration. Both the BHR® and ASR® components have a conical design, whereas all other femoral components have cylindrical designs. Not surprisingly, the thinnest cement mantle in Zone 1 was noted with the two designs with the lowest clearance (BHR®, ASR®) despite the use of two different cementation techniques. Furthermore, by altering cementation technique, the BHR/hvt had close to a 30% reduction in penetration. However, despite the lower values for the BHR/hvt’s cement penetration percentage and depth, they remained higher than the cement penetration obtained with the Conserve Plus® using both high- and low-viscosity cementation techniques (Fig. 4). This suggests the higher cement penetration noted with the BHR cannot be solely dependent on its low-viscosity cementation technique. Alternating cementation techniques in the Conserve Plus group did not result in comparable changes like in the BHR group, suggesting the impact of cementation technique may be greater in low-clearance implants [17]. Another important finding was the variance in the cement mantle thickness at the dome (Zone III), which is a reflection of both implant design as well as seating of the implant. We observed a greater risk of incomplete seating of the implant (four of six implants) when the BHR was implanted using the higher viscosity cementation technique (BHR/hvt). This was confirmed with the cement mantle in Zone III being almost 3 mm on average compared with less than 1 mm with the standard BHR (Fig. 9) (Table 4). This is in accordance with the findings of Bitsch and associates [14], which noted a thicker cement mantle at the dome using the ASR® component, which has a conical design like the BHR, especially when cement was poured in the femoral shell as part of the cementation technique. We also recorded a major difference in cement mantle thickness with the ReCAP® having the thicker mantle and the DuROM® the thinnest mantle with all of the implants being fully seated, again emphasizing the influence of implant design because the ReCAP® is the only implant without a chamfer design being purely spherical. These results are important because incomplete seating of the femoral component is a recognized risk factor for early neck fracture [3, 35], which can be further compounded by eccentric reaming of the femoral head.
Although a few studies have attempted to look at the cement mantle, these were limited to one implant design in which different cementation techniques were studied [14, 17, 22]. How implant design may influence cement mantle and penetration becomes important because mantle thickness and penetration plays a role in stress transfer to the underlying bone [39] with stress shielding still remaining a concern in terms of the long-term performance of hip resurfacing [10, 21, 44]. Radcliffe and Taylor [39] examined the effect of varying cement mantle and penetration thickness on transfers within the resurfaced femoral head and reported the greater mantle and penetration thickness leads to major decreases in strain within the proximal femur, ie, increased risk of proximal stress shielding with a mean percentage change of −6% with a 1-mm thin cement mantle, −18% with a 3-mm mantle, and −27% for a 5-mm mantle. This could in part explain the phenomenon of femoral neck narrowing after hip resurfacing, which is reportedly as high as 27% [10, 21]. Although this had not demonstrably led to short-term failure, it certainly puts the femoral neck at risk of fracture in the long term.
Current failure mechanisms of hip resurfacing suggest failure of the femoral component as an important determinant of the short-term clinical performance. Because cement fixation is the current preferred method used, how one achieves and what factors influence adequate penetration within the femoral head are important to understand. Our study demonstrates clinicians using hip resurfacing can expect to find major differences in cement penetration and mantle thickness depending on which implant design and cementation technique they use. Researchers and clinicians involved in the development and implantation of hip resurfacing in the treatment of osteoarthritis need to understand these effects because excessive or insufficient cement penetration can lead to early failure.
Acknowledgments
We thank Patricia Campbell, PhD, and Christina Esposito from Los Angeles Orthopaedic Hospital for their assistance in cutting the DuROM® resurfaced femoral heads; Diane Robertson for her assistance in collecting the femoral heads; Philippe St-Laurent for his assistance with the DEXA scans; Maryam Shahrokni for her assistance in cutting the femoral heads; and Steve Doucette, PhD, for statistical support. Finally, this study would not have been possible without the manufacturers of implants and bone cement providing the materials free of charge.
Footnotes
One or more of the authors (PEB) have received funding from Wright Medical Technologies.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Amstutz HC, Beaule PE, Dorey FJ, Campbell PA, Le Duff MJ, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six year follow-up. J Bone Joint Surg Am. 2004;86:28–39. [PubMed]
- 2.Amstutz HC, Dorey F, O’Carroll PF. THARIES resurfacing arthroplasty. Evolution and long-term results. Clin Orthop Relat Res. 1986;213:92–114. [PubMed]
- 3.Amstutz HC, Le Duff MJ, Campbell PA. Fracture of the neck of the femur after surface arthroplasty of the hip. J Bone Joint Surg Am. 2004;86:1874–1877. [DOI] [PubMed]
- 4.Amstutz HC, LeDuff MJ, Campbell PA, Dorey FJ. The effects of technique changes on aseptic loosening of the femoral component in hip resurfacing. Results of 600 Conserve Plus with a 3 to 9 year follow-up. J Arthroplasty. 2007;22:481–489. [DOI] [PubMed]
- 5.Askew MJ, Streege JW, Lewis JL, Ranieri JR, Wixson RL. Effect of cement pressure and bone strength on polymethylmethacrylate fixation. J Orthop Res. 1984;1:412–420. [DOI] [PubMed]
- 6.Beaule PE. Surface arthroplasty of the hip: a review and current indications. Semin Arthroplasty. 2005;16:70–76. [DOI]
- 7.Beaule PE, Antoniades J. Patient selection and surgical technique for surface arthroplasty of the hip. Orthop Clin North Am. 2005;36:177–185. [DOI] [PubMed]
- 8.Beaule PE, Campbell PA, Hoke R, Dorey FJ. Notching of the femoral neck during resurfacing arthroplasty of the hip. A vascular study. J Bone Joint Surg Br. 2006;88:35–39. [DOI] [PubMed]
- 9.Beaule PE, Campbell PA, Lu Z, Leunig-Ganz K, Beck M, Leunig M, Ganz R. Vascularity of the arthritic femoral head and hip resurfacing. J Bone Joint Surg Am. 2006;88:85–96. [DOI] [PubMed]
- 10.Beaule PE, Dorey FJ, LeDuff MJ, Gruen T, Amstutz HC. Risk factors affecting outcome of metal on metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. [DOI] [PubMed]
- 11.Beaule PE, Krismer M, Mayrhofer P, Manner M, Le Duff MJ, Mattesich M, Stoeckl B, Amstutz HC, Biedermann R. EBRA-FCA for measurement of migration of the femoral component in surface arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:741–744. [DOI] [PubMed]
- 12.Beaule PE, Lee J, LeDuff M, Dorey FJ, Amstutz HC, Ebramzadeh E. Orientation of femoral component in surface arthroplasty of the hip: a biomechanical and clinical analysis. J Bone Joint Surg Am. 2004;86:2015–2021. [DOI] [PubMed]
- 13.Benjamin JB, Gie GA, Lee AJC, Ling RSM, Volz RG. Cementing technique and the effects of bleeding. J Bone Joint Surg Br. 1987;69:620–624. [DOI] [PubMed]
- 14.Bitsch R, Heisel C, Silva M, Schmalzried TP. Femoral cementing technique for hip resurfacing arthroplasty. J Orthop Res. 2007;25:423–431. [DOI] [PubMed]
- 15.Callaghan JJ. Total hip arthroplasty. Clinical perspective. Clin Orthop Relat Res. 1992;276:33–40. [PubMed]
- 16.Campbell PA, Beaule PE, Ebramzadeh E, LeDuff MJ, DeSmet KA, Lu Z, Amstutz HC. The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res. 2006;453:35–46. [DOI] [PubMed]
- 17.Chandler M, Kowalski RSZ, Watkins ND, Briscoe A, New AMR. Cementing techniques in hip resurfacing. Proc Inst Mech Eng [H]. 2006;220:321–331. [DOI] [PubMed]
- 18.Daniel J, Pynsent PB, McMinn DJW. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. [DOI] [PubMed]
- 19.Ebramzadeh E, Sarmiento A, McKellop HA, Llinas A, Gogan W. The cement mantle in total hip arthroplasty. Analysis of long-term radiographic results. J Bone Joint Surg Am. 1994;76:77-87. [DOI] [PubMed]
- 20.Grigoris P, Roberts P, Panousis K, Bosch H. The evolution of hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:125–134. [DOI] [PubMed]
- 21.Hing CB, Young DA, Dalziel RE, Bailey M, Back DL, Shimmin AJ. Narrowing of the neck in resurfacing arthroplasty of the hip: a radiological study. J Bone Joint Surg Br. 2007;89:1019–1024. [DOI] [PubMed]
- 22.Howald R, Kesteris U, Klabunde R. Factors affecting the cement penetration of a hip resurfacing implant: an in-vitro study [Abstract]. Osteologie. 2005;14:10. [DOI] [PubMed]
- 23.Howie DW, Campbell D, McGee M, Cornish BL. Wagner resurfacing hip arthroplasty. The results of one hundred consecutive arthroplasties after eight to ten years. J Bone Joint Surg Am. 1990;72:708–714. [PubMed]
- 24.Huiskes R, Heck J, Slooff TJJH. Interface stresses in the resurfaced hip. Finite element analysis of load transmission in the femoral head. Acta Orthop Scand. 1985;56:474–478. [DOI] [PubMed]
- 25.Jansson V, Kheimkes B, Zimmer M. Stress transfer at the femoral bone/bone cement interface as a function of the cement thickness. Arch Orthop Trauma Surg. 1993;112:65–68. [DOI] [PubMed]
- 26.Jolley MN, Salvati EA, Brown GC. Early results and complications of surface replacement of the hip. J Bone Joint Surg Am. 1982;64:366–377. [PubMed]
- 27.Juliusson R, Flivik G, Nilsson J, Ryd L, Onnerfalt R. Circulating blood diminishes cement penetration into cancellous bone. In vitro studies of 21 arthrotic femoral heads. Acta Orthop Scand. 1995;66:234–238. [DOI] [PubMed]
- 28.Juliusson R, Ryd L, Arve J. Cementation pressure in arthroplasty. In vitro study of cement penetration into femoral heads. Acta Orthop Scand. 1994;65:131–134. [DOI] [PubMed]
- 29.Kilgus DJ, Dorey FJ, Finerman GA, Amstutz HC. Patient activity, sports participation, and impact loading on the durability of cemented total hip replacements. Clin Orthop Relat Res. 1991;269:25–31. [PubMed]
- 30.Krause WR, Krug W, Miller J. Strength of the cement-bone interface. Clin Orthop Relat Res. 1982;163:290–299. [PubMed]
- 31.Little CP, Ruiz AL, Harding IJ, McLardy-Smith P, Gundle R, Murray DW, Athanasou NA. Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:320–323. [DOI] [PubMed]
- 32.Markolf KL, Amstutz HC. In vitro measurement of bone-acrylic interface pressure during femoral component insertion. Clin Orthop Relat Res. 1976;121:60–66. [PubMed]
- 33.Markolf KL, Kabo JM, Stoller DW, Zager SA, Amstutz HC. Flow characteristics of acrylic bone cements. Clin Orthop Relat Res. 1984;183:246–254. [PubMed]
- 34.Mjoberg B, Pettersson H, Rosenqvist R, Rydholm A. Bone cement, thermal injury and the radiolucent zone. Acta Orthop Scand. 1984;55:597–600. [DOI] [PubMed]
- 35.Mont MA, Seyler TM, Ulrich SD, Beaule PE, Boyrd HS, Grecula MJ, Goldberg VM, Kennedy WR, Marker DR, Schmalzried TP, Sparling EA, Vail TP, Amstutz HC. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70. [DOI] [PubMed]
- 36.Morlock MM, Bishop N, Ruther W, Delling G, Hahn M. Biomechanical, morphological, and histological analysis of early failures in hip resurfacing. Proc Inst Mech Eng [H]. 2006;220:333–344. [DOI] [PubMed]
- 37.Noble PC, Swarts E. Penetration of acrylic bone cements into cancellous bone. Acta Orthop Scand. 1983;54:566–573. [DOI] [PubMed]
- 38.Pollard TCB, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip. Two to seven year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600. [DOI] [PubMed]
- 39.Radcliffe IA, Taylor M. Investigation into the affect of cementing techniques on load transfer in the resurfaced femoral head: a multi-femur finite element analysis. Clin Biomech (Bristol, Avon). 2007;22:422–430. [DOI] [PubMed]
- 40.Shimmin A, Back D. Femoral neck fractures following Birmingham hip resurfacing. A national review of 50 cases. J Bone Joint Surg Br. 2005;87:463–464. [DOI] [PubMed]
- 41.Treacy R, Pynsent P. Birmingham Hip Resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. [DOI] [PubMed]
- 42.Trudel G, Koike Y, Dinh L, Uhthoff HK. Thawing of frozen calcaneus bone specimens has no effect on the bone mineral density using dual energy x-ray absorptiometry: a study in rabbits and humans. Physiol Meas. 2005;26:769–777. [DOI] [PubMed]
- 43.Valdivia GG, Dunbar MJ, Parker DA, Woolfrey MR, MacDonald SJ, McCalden RW, Rorabeck CH, Bourne RB. The John Charnley Award: three-dimensional analysis of the cement mantle in total hip arthroplasty. Clin Orthop Relat Res. 2001;393:38–51. [DOI] [PubMed]
- 44.Watanabe Y, Shiba N, Matsuo S, Higuchi F, Tagawa Y, Inoue A. Biomechanical study of the resurfacing hip arthroplasty. Finite element analysis of the femoral component. J Arthroplasty. 2000;15:505–511. [DOI] [PubMed]