Abstract
Reorientation acetabular osteotomies can correct dysplastic deformities and provide marked improvement in hip function. Deformities of the proximal femur can produce suboptimal articulation or secondary impingement after acetabular reorientation, yet the incidence and characteristics of such deformities have not been well described. To describe the proximal femoral anatomy in patients with symptomatic acetabular dysplasia, we retrospectively analyzed the radiographs of 108 hips treated with periacetabular osteotomy. The radiographic findings were compared with those in 22 control hips. In the dysplastic group, 80 hips were in women and 28 in men, and the average age was 24.8 years. Of the 108 abnormal radiographs, 44% had coxa valga and 4% coxa vara. Seventy-two percent had an aspheric or deformed femoral head and the head-neck offset was insufficient in 75% of the hips. When compared with the control hips, dysplastic hips had differences in parameters of proximal femoral anatomy that we measured. These data demonstrate a high incidence of proximal femoral abnormalities associated with acetabular dysplasia. Identifying and treating these abnormalities may optimize joint congruency and minimize secondary impingement after acetabular reorientation.
Level of Evidence: Level II, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Periacetabular osteotomy [7] is an effective treatment for symptomatic acetabular dysplasia [2, 3, 7, 9, 10, 18, 22], and ongoing efforts are directed at optimizing the efficacy of this procedure. The clinical results of acetabular reorientation are dependent on various patient-specific factors as well as the precision of the surgical correction. The technical goals of surgery are to correct structural instability, optimize joint biomechanics, normalize articular loading, and avoid secondary femoroacetabular impingement. Secondary impingement can result from overcorrection of the acetabulum and/or from residual deformity of the proximal femur that makes the hip susceptible to femoroacetabular abutment [11]. Although attention has focused on obtaining optimal acetabular reduction, less emphasis has been placed on the structural characteristics of the proximal femur that may contribute to femoroacetabular impingement after acetabular reorientation.
Femoral deformities associated with acetabular dysplasia have been well documented in the literature [12, 14, 16, 19, 20]. The most common deformities include femoral anteversion, an aspheric femoral head, and reduced femoral head-neck offset. Nevertheless, there is limited comprehensive information regarding these deformities relative to acetabular reorientation surgery.
The primary purpose of this study was to determine the incidence and characteristics of proximal femoral abnormalities in symptomatic dysplastic hips. Secondarily, we compared the proximal femoral anatomy of dysplastic hips with that in a cohort of control hips.
Materials and Methods
We retrospectively reviewed the radiographs of 108 hips treated with periacetabular osteotomy for either symptomatic “classic” acetabular dysplasia or acetabular dysplasia associated with a “Perthes-like” deformity of the proximal femur [1, 3]. We compared the findings with a series of radiographs from a group of asymptomatic patients (control group) we previously reported [4, 15]. The study cohort included 108 hips, 80 (74%) in women and 28 in men, with acetabular dysplasia diagnosed by clinical history, physical examination, and radiographic analysis. Ninety-five of the hips were classified as “classic” developmental dysplasia and 13 were classified as acetabular dysplasia with a Perthes-like deformity of the proximal femur [1, 3]. Fourteen patients had staged bilateral periacetabular osteotomies (10 women, four men). The average age of all study patients was 24.8 years (range, 13–50 years). Twelve patients (13 hips) had at least one osteotomy procedure before presentation. The indications for surgery included persistent hip pain (longer than 6 months), failure of nonoperative treatment (which included activity modifications, nonsteroidal antiinflammatory drugs, and physical therapy), and radiographic findings consistent with acetabular dysplasia without advanced arthrosis (Tönnis Grade 3). This study was performed under an Institutional Review Board-approved protocol.
The control group consisted of a series of patients that we had previously reported [4, 15]. These patients had a complete radiographic series of the hip as routine imaging for a chief complaint of “hip pain.” They were seen in the senior author’s (JCC) clinic and determined not to have any evidence of a hip disorder. None of the patients had groin pain, irritability of the hip, or a positive impingement test. All of these patients had signs and symptoms completely consistent with a diagnosis not involving the hip (ie, lumbar osteoarthritis or lumbar radiculopathy). These patients had a mean age of 34 years (range, 17–58 years) with 64% being female. Age and gender were similar in the study and control groups (p = 0.35 and p = 0.51, respectively).
All radiographic measurements were performed by one observer (RMN). This observer participated in our previously published radiographic studies [3, 15] that demonstrated “substantial” to “almost perfect” intra- and interobserver reliability with the measurements reported in the present study. All patients had a complete set of preoperative radiographs, which included an anteroposterior (AP) pelvis, AP hip, false profile [8], crosstable lateral, and frog-leg lateral of the affected hip(s). Radiographs were performed using standardized techniques as previously reviewed [4]. Commonly reported radiographic parameters of hip structure were used to objectively define the acetabular and femoral anatomy [4, 15].
On the AP pelvis radiograph, the lateral center-edge angle [23], acetabular inclination [21], femoral head-neck shaft angle, and congruency [24] of the hip were assessed. The femoral neck-shaft angle was measured on the AP radiograph of the hip [15, 17]. We defined coxa vara as a neck-shaft angle less than 126° and coxa valga as greater than 139° [15]. The hip was judged to be congruent if it was classified as “good” or “excellent” according to Yasunaga et al. [24] The anterior center-edge angle was measured on the false profile view [8]. The Tönnis grading classification [21] was used to assess the hip for the presence of arthrosis.
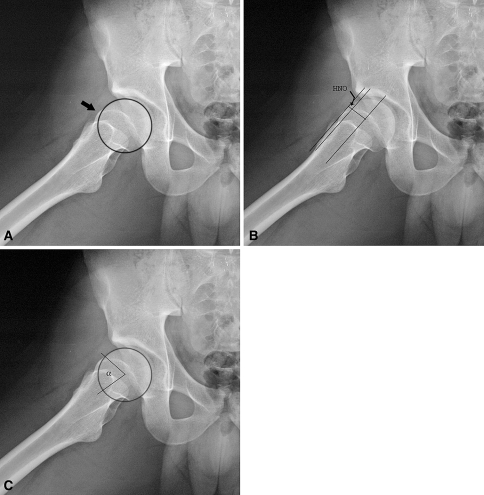
On the crosstable and frog-leg lateral images, measurements were taken of the femoral head-neck offset [5, 6], femoral head diameter, α-angle [13], and femoral head sphericity (Fig. 1A–C). The femoral head-neck offset distance and femoral head diameter were measured on the crosstable lateral and frog-leg lateral images using the method described by Eijer et al. [5, 6]. The femoral head-neck offset ratio, defined as the ratio between the head-neck offset distance and the femoral head diameter, was calculated to standardize the head-neck offset for comparison between patients [6]. The α-angle described by Notzli et al. [13] is the angle between the femoral head-neck axis and the point at which the femoral head deviates from its radius of curvature. The α-angle is increased in patients with hip impingement [13]. Femoral head sphericity was determined using circular templates to determine if the head and head-neck junction were contained within the circle [4].
Fig. 1A–C.
Frog-leg lateral radiographs show (A) assessment of femoral head sphericity using a spheric template (arrow), (B) measurement of head-neck offset (HNO, arrow) as described by Eijer et al. [5], and (C) measurement of the α-angle as described by Notzli et al. [13]. (Reprinted with permission from Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121.)
We have previously shown “substantial” to “almost perfect” intra- and interobserver reliability with the radiographic measurements described and used in this study [4, 15]. Wilcoxon signed-rank test was used to determine differences in averaged data between the two groups for lateral center-edge angle, anterior center-edge angle, acetabular index, femoral neck-shaft angle, head-neck offset, femoral head diameter, α-angle, hip congruency, and the presence of an aspheric head. Data analyses were performed using SAS software for Linux (SAS Institute Inc, Cary, NC).
Results
Proximal femoral deformities were present in 92.6% of the hips treated for symptomatic acetabular dysplasia (Table 1). Assessment of proximal femoral alignment with the neck-shaft angle demonstrated 48% of the hips had coxa valga (44%) or coxa vara (4%) (Fig. 2A–B). All hips with coxa vara had a previous proximal femoral varus-producing osteotomy. Analysis of the femoral head-neck junction (Table 1) revealed 73.1% of the hips had an abnormal head-neck offset ratio (Fig. 3A–B) or α-angle, and 78 (72%) were judged to have an aspheric femoral head (Fig. 4A–B). Average acetabular measurements were consistent with dysplasia as demonstrated by insufficient lateral and anterior femoral head coverage as well as excessive acetabular inclination (Table 1).
Table 1.
Comparison of mean radiographic measurements
| Measurement | Periacetabular osteotomy (n = 108) | Control (n = 22) | p value |
|---|---|---|---|
| Lateral center-edge angle (degrees) | 6.2 (–29–26) | 32 (25–42) | < 0.0001 |
| Acetabular index (degrees) | 25.4 (11–42) | 6.2 (0–15) | < 0.0001 |
| Anterior center-edge angle (degrees) | 4.4 (−34–34) | ND | |
| Head-neck offset (mm) | 7.25 (13.5–6.5) | 10.6 (6.5–14.5) | < 0.0001 |
| Femoral head diameter (mm) | 53.8 (44–63) | 54.8 (49–65) | 0.43 |
| Head-neck offset ratio | 0.145 (−0.14–0.27) | 0.194 (0.097–0.275) | 0.003 |
| Alpha angle | 75.1 (42–140) | 43.9 (33–78) | < 0.0001 |
Values are mean (range); ND = not determined.
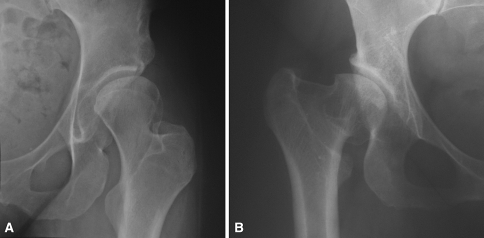
Fig. 2A–B.
Proximal femoral deformities associated with acetabular dysplasia. (A) An anteroposterior radiograph of the left hip in a 31-year-old woman with a history of insidious-onset hip pain demonstrates acetabular dysplasia and associated coxa valga. (B) Anteroposterior right hip radiograph of a 36-year-old female patient with a history of developmental hip dysplasia and previous proximal femoral varus-producing osteotomy shows residual coxa vara.
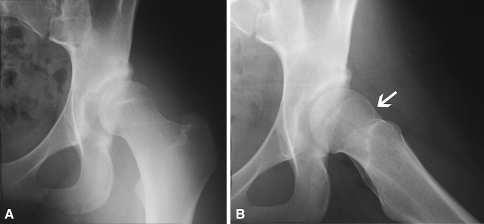
Fig. 3A–B.
Reduced femoral head-neck offset associated with acetabular dysplasia. Anteroposterior and frog-leg lateral radiographs of a 19-year-old woman with hip pain. (A) The anteroposterior view demonstrates acetabular dysplasia with a spheric femoral head. (B) The frog-leg lateral view depicts an area of insufficient head-neck offset anteriorly (arrow).
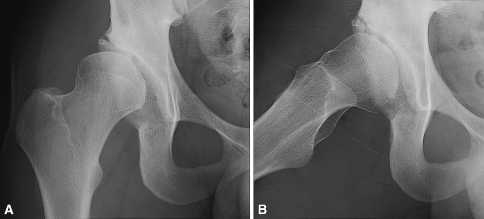
Fig. 4A–B.
Asphericity of the femoral head associated with acetabular dysplasia. Anteroposterior and frog-leg lateral radiographs of the right hip in a 23-year-old man with hip pain. (A) The anteroposterior view demonstrates acetabular dysplasia and mild asphericity of the femoral head. (B) The frog-leg lateral radiograph better visualizes the aspheric head shape and insufficient offset of the head-neck junction.
The dysplastic hip cohort had different average radiographic parameters for proximal femoral anatomy (Table 1) and a higher percentage of femoral radiographic abnormalities as compared with the control hip cohort (Table 2). The percentage of hips with insufficient femoral head-neck offset, femoral head asphericity, coxa vara, and coxa valga was higher in the dysplastic group (all p < 0.0001) (Table 2). As expected, the percentage of abnormal radiographic parameters for acetabular dysplasia (lateral center-edge angle and acetabular inclination) was far more common in the dysplastic hips (Table 2). The osteoarthritis (Tönnis) grade and hip congruency were similar in the two study groups.
Table 2.
Numbers and percentages of abnormal measurements
| Measurement | Periacetabular osteotomy (n = 108) | Control (n = 22) | p value |
|---|---|---|---|
| Lateral center edge angle less than 25° | 106 (93%) | 0 (0%) | < 0.0001 |
| Acetabular index greater than 10° | 108 (100%) | 1 (5%) | < 0.0001 |
| Head-neck offset less than 9 mm | 81 (75%) | 1 (5%) | < 0.0001 |
| Head-neck offset ratio less than 0.17 | 69 (64%) | 2 (9%) | < 0.0001 |
| Aspheric femoral head | 78 (72%) | 0 (0%) | < 0.0001 |
| Coxa vara (NSA less than 126°) | 4 (3.7%) | 0 (0%) | < 0.0001 |
| Coxa valga (NSA less than 139°) | 48 (44.4%) | 5 (23%) | < 0.0001 |
| Tönnis Grade 1 or 2 | 22 (20.3%) | 2 (9%) | 0.32 |
| Congruency | 102 (94%) | ND |
ND = not determined.
Discussion
Anterior femoroacetabular impingement is a known cause of recurrent symptoms after acetabular reorientation for the treatment of symptomatic hip dysplasia [11]. Overcorrection and/or proximal femoral abnormalities can contribute to secondary impingement. Therefore, the purpose of this study was to define the incidence and characteristics of proximal femoral abnormalities in the setting of symptomatic dysplasia and to compare these findings with a cohort of control hips.
The limitations of this study primarily include its descriptive design and lack of clinical outcome data regarding combined femoral and acetabular reorientation procedures. Nevertheless, our stated purpose was to characterize these femoral deformities as a first step in determining the potential need for femoral-sided augmentation procedures. The second major weakness is the control cohort was established retrospectively. These patients were determined (by the senior author) to not have symptoms relative to the hip. Nevertheless, the possibility of an atypical clinical presentation of hip disease cannot be entirely excluded for these patients. If present, this would be uncommon and unlikely to affect the conclusion regarding comparison of the dysplasia and control cohorts. The final major weakness is our analysis and conclusions are based on plain radiographs only, and three-dimensional imaging was not used. This radiographic evaluation has limitations in detecting certain deformities like proximal femoral anteversion.
Our analysis of proximal femoral anatomy in the dysplastic hip and comparison with control hips produced several major findings. Proximal femoral malalignment was common with 47% of the hips having coxa valga or coxa vara. Coxa valga was associated with “classic” acetabular dysplasia in all cases. Coxa vara was present as a result of previous proximal femoral varus osteotomy in all cases. Insufficient femoral head-neck offset (less than 9 mm) was present in 75% of the hips and 78% of the hips were judged to be aspheric. Our results are consistent with other data in the literature. Specifically, Okano et al. [14] and Steppacher et al. [19] have emphasized the common findings of femoral head asphericity and reduced head-neck offset in dysplastic hips. Additional studies [12, 20] with three-dimensional analyses have also highlighted the common deformity of increased proximal femoral anteversion. Collectively, these data indicate proximal femoral abnormalities are quite common in hips that are symptomatic from structural instability. Many of these deformities predispose the hip to continued structural instability (coxa valga) or secondary femoroacetabular impingement (head-neck offset abnormalities) after acetabular reorientation. These findings should prompt surgeons to analyze the proximal femoral anatomy preoperatively and to contemplate whether the deformity should be corrected at the time of the acetabular procedure.
The major technical goals of acetabular reorientation are to create stable articulation, improve articular loading patterns, and to prevent secondary femoroacetabular impingement. The periacetabular osteotomy is advantageous because it allows major multiplanar corrections [2]. Nevertheless, this advantage is tempered by the potential problem of overcorrection or improper reduction. Even with an appropriate correction, the periacetabular osteotomy reduces hip flexion motion [18, 22]. Therefore, enhancing impingement-free flexion motion is a major goal of the procedure. In hips with an aspheric femoral head or reduced anterolateral femoral head-neck offset, secondary femoroacetabular impingement can be problematic after acetabular repositioning [11] because the more normal position of the acetabular rim creates abnormal contact with the deformity of the proximal femur (insufficient head-neck offset). In this setting, the surgeon may consider a head-neck osteochondroplasty to prevent femoroacetabular impingement. In our practice, it is now routine to perform anterior arthrotomy to assess the labrum and, more importantly, inspect the relationship of the acetabular rim and the femoral head-neck junction. The contour of the head-neck junction is directly visualized and is tested in hip flexion and internal rotation. If there is lack of femoral head-neck junction offset or if impingement is observed in flexion and/or internal rotation, recontouring of the femoral head-neck junction is performed.
In cases of acetabular dysplasia with associated coxa valga, we recommend performing the acetabular reorientation followed by careful assessment of joint stability directly through the anterior arthrotomy and by intraoperative radiographic evaluation. If residual instability is present (subluxation, incongruency, or insufficient head coverage), proximal femoral varus osteotomy can be considered. This is performed to augment approximately 5% of our periacetabular osteotomy cases. Perthes-like deformities pose the most difficult problems because the acetabular dysplasia can be associated with major deformities of the proximal femur. In this setting, the surgeon may consider reshaping the femoral head, relative lengthening of the neck, trochanteric advancement, and proximal femoral valgus osteotomy (5% of our cases) when appropriate [1, 3]. Isolated acetabular reorientation in this setting can be problematic as a result of secondary femoroacetabular impingement.
These data demonstrate proximal femoral abnormalities are commonly associated with symptomatic acetabular dysplasia. These abnormalities can result from the primary hip deformity or may be secondary to previous surgical treatment. To optimize surgical reconstruction of the hip, it is important to emphasize the proximal femoral anatomy should be evaluated preoperatively. This facilitates preoperative planning and provides information regarding comprehensive surgical reconstruction of the joint. The surgeon must also balance the potential benefit of a femoral procedure with the associated risks and complications. Specifically, a proximal femoral osteotomy considerably increases the magnitude of the procedure and prolongs the postoperative rehabilitation. Alternatively, osteochondroplasty of the femoral head-neck junction at the time of arthrotomy seems to be well tolerated and not associated with major risks. In our practice, we commonly combine a proximal femoral procedure with acetabular reorientation to enhance hip stability, congruency, and impingement-free flexion motion of the hip. Most commonly (80% of cases), osteochondroplasty of the femoral head-neck junction is performed to minimize secondary impingement. Proximal femoral osteotomies are used less commonly (10% of cases) and only in the setting of major coxa valga or coxa vara. Mid- and long-term data analyzing the clinical results of these techniques is important in defining the role of proximal femoral procedures in combination with periacetabular osteotomy.
Footnotes
One or more of the authors has received funding from a grant from Zimmer, Inc (JCC). This work was supported in part by Award Number UL1RR024992 from the National Center For Research Resources (JCC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health. This work was also supported in part by the Curing Hip Disease Fund (JCC).
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Beck M, Mast JW. The periacetabular osteotomy in Legg-Perthes-like deformities. Semin Arthroplasty. 1997;8:102–107.
- 2.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87:254–259. [DOI] [PubMed]
- 3.Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89:1417–1423. [DOI] [PubMed]
- 4.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. [DOI] [PubMed]
- 5.Eijer H, Leunig M, Mahomed M, Ganz R. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip International. 2001;11:37–41.
- 6.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15:475–481. [DOI] [PubMed]
- 7.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed]
- 8.Lequesne M, de Seze. False profile of the pelvis. A new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies [in French]. Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed]
- 9.Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. J Bone Joint Surg Am. 2001;83:438–448.
- 10.Millis MB, Kim YJ. Rationale of osteotomy and related procedures for hip preservation: a review. Clin Orthop Relat Res. 2002;405:108–121. [DOI] [PubMed]
- 11.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. [DOI] [PubMed]
- 12.Noble PC, Kamaric E, Sugano N, Matsubara M, Harade Y, Ohzono K, Paravic V. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003;417:27–40. [PubMed]
- 13.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. [DOI] [PubMed]
- 14.Okano K, Enomoto H, Osaki M, Shindo H. Outcome of rotational acetabular osteotomy for early hip osteoarthritis secondary to dysplasia related to femoral head shape: 49 hips followed for 10–17 years. Acta Orthop. 2008;79:12–17. [DOI] [PubMed]
- 15.Peelle MW, Della Rocca GJ, Maloney WJ, Curry MC, Clohisy JC. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333. [DOI] [PubMed]
- 16.Robertson DD, Essinger JR, Imura S, Kuroki Y, Sakamaki T, Shimizu T, Tanaka S. Femoral deformity in adults with developmental hip dysplasia. Clin Orthop Relat Res. 1996;327:196–206. [DOI] [PubMed]
- 17.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. [DOI] [PubMed]
- 18.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. [DOI] [PubMed]
- 19.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. [DOI] [PMC free article] [PubMed]
- 20.Sugano N, Noble PC, Kamaric E, Salama JK, Ochi T, Tullos HS. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br. 1998;80:711–719. [DOI] [PubMed]
- 21.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. [DOI] [PubMed]
- 22.Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85. [DOI] [PubMed]
- 23.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83:7–38.
- 24.Yasunaga Y, Takahashi K, Ochi M, Ikuta Y, Hisatome T, Nakashiro J, Yamamoto S. Rotational acetabular osteotomy in patients forty-six years of age or older: comparison with younger patients. J Bone Joint Surg Am. 2003;85:266–272. [DOI] [PubMed]