Abstract
Gender-specific total hip arthroplasty (THA) design has been recently debated with manufacturers launching gender-based designs. The purpose of this study was to investigate the survivorship and clinical outcomes of a large primary THA cohort specifically assessing differences between genders in clinical outcomes, implant survivorship, revisions as well as sizing and offset differences. We reviewed 3461 consecutive patients receiving 4114 primary THAs (1924 women, 1537 men) between 1980 and 2004 with a minimum of 2 years followup (mean, 11.33 ± 6.5 years). A subset of patients with complete implant data was reviewed for sizing and offset differences. Preoperative, latest, and change in clinical outcome scores as well as Kaplan–Meier analysis were performed. Men had higher raw clinical outcome scores preoperatively and postoperatively. Differences in change of clinical outcome scores were found only in the WOMAC pain score in favor of the female cohort (39.4 versus 36.1). Survivorship and revision rate were not significantly different. Men used larger stems with greater stem lengths, neck offset, and neck lengths. Current implant systems were sufficiently versatile to address the different size and offset needs of male and female patients. These data suggest there is no apparent need for a gender-designed THA system.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Total hip arthroplasty is one of the most successful operative interventions for improving quality of life in patients today. The success rate, both short- and long-term, is very high [17], and modern techniques and implants continue to strive for improvement in results, building on the firm foundation of arthroplasty pioneers like Charnley.
A recent arthroplasty development is the concept of gender-specific implants to address potential differences in male and female anatomy of the hip and knee [1, 2]. We focus here on the hip, specifically on the femoral side, as the main gender-based anatomic differences relate to location of the femoral head center (ie, offset or femoral axis) and shape and size of the femoral canal. Females tend to have lower offset or a smaller femoral axis than males [14]. As aging takes place, females develop considerably increased femoral medullary width compared with males as well as losing more bone at the medial calcar and lateral cortex [14]. Current implant designs in general use on the market include a variety of options in stem length and diameter, neck offset, and neck length.
In our study, we addressed the following questions. Using nongender-specific implants, is there a difference in implant survivorship in the long-term? Are the reasons for revision different between males and females? Is there a difference in implant-related intraoperative complications such as major calcar or femoral fractures? Is there a difference between genders for health-related quality of life, pain, and function scores, including preoperative, latest postoperative, and change scores? What are the differences in sizing and offset of femoral stems between males and females?
Materials and Methods
Our study included a consecutive group of 3461 patients having undergone 4114 primary THAs between the years 1980 and 2004. There were 1924 female (56%) and 1537 male (44%) patients. Inclusion criteria for the study were a primary diagnosis of degenerative hip arthritis and hip arthroplasty between 1980 and 2004 with a minimum followup of 2 years. Exclusion criterion was any inflammatory arthritis or primary hip arthroplasty for reasons other than degenerative arthritis. Since 1980, the authors’ institution has prospectively collected patient demographic data and surgical information as well as pre- and postoperative Harris hip, WOMAC, and SF-12 (Version 1) scores for all patients undergoing THAs. The minimum postoperative followup was 2 years (mean, 11.3 years; range, 2–27.4 years). Ethics approval was granted by the Institutional Review Board.
The female patients with a mean age of 65 years (± 13 years) were slightly older (p < 0.0001) than the male patients (mean, 63 ± 12 years) at the date of initial arthroplasty. Women also had a slightly lower (p < 0.002) body mass index at the time of surgery (mean, 29 ± 6 kg/m2) compared with men (mean, 30 ± 5 kg/m2). These are not big differences in age and body mass index; the statistical significance owes more to large numbers rather than wide differences. The mean height for women was 160.2 cm and for men 174.3 cm. The mean weight for female patients was 74.4 kg compared with 90.4 kg for male patients (Table 1).
Table 1.
Patient demographics
| Variable | Group | Significance | Mean | Standard deviation |
|---|---|---|---|---|
| Age | Female | 0.001 | 64.9 | 13.5 |
| Male | 62.8 | 12 | ||
| Height | Female | 0.001 | 160.2 | 7.2 |
| Male | 174.3 | 7.9 | ||
| Weight | Female | 0.001 | 74.4 | 17.2 |
| Male | 90.4 | 17.1 | ||
| Body mass index | Female | 0.002 | 29 | 6.4 |
| Male | 29.7 | 5.1 |
All surgeries were performed at the same institution by one of four surgeons (SJM, RBB, RWM, CHR). A number of different implant designs from various manufacturers were used over the years. These included 1007 Synergy stems (Smith and Nephew Inc, Memphis, TN), 1013 Mallory-Head stems (Biomet, Inc, Warsaw, IN), 278 Spectron stems (Smith and Nephew Inc), 263 PCA stems (Stryker Orthopedics/Howmedica, Mahwah, NJ), 262 Prodigy stems (DePuy Orthopaedics Inc, Warsaw, IN), 191 Endurance stems (DePuy Orthopaedics Inc), 141 Contemporary stems (Stryker Orthopedics/Howmedica), 103 Versys stems (Zimmer Inc, Warsaw, IN), 80 Exeter stems (Stryker Orthopedics/Howmedica), 79 S-ROM stems (DePuy Orthopaedics Inc), 30 AML stems (DePuy Orthopaedics Inc), 27 Echelon stems (Smith and Nephew Inc), 17 Orthinox stems (Stryker Orthopedics/Howmedica), 11 Solution stems (DePuy Orthopaedics Inc), 10 Omnifit (Stryker Orthopedics/Howmedica) stems, eight Summit stems (DePuy Orthopaedics Inc), eight CPCS stems (Smith and Nephew Inc), and six Accolade stems (Stryker Orthopedics/Howmedica). Stem manufacturer information was not collected for a further 580 stems.
Kaplan–Meier survivorship analysis [5] was carried out with an end point of revision for any reason except infection. We excluded infection from our survival analysis because it is not an implant-related problem, but included the revision rate for infection compared between males and females. Reasons for revision were compared between genders and analyzed for significance. Major intraoperative fractures captured in the database were reviewed. We compared the preoperative and most recent outcome scores to determine the differential change after surgery. We also analyzed the differential in outcome scores between preoperatively and the most recent followup. Categorical variables (eg, gender, body mass index group, survival status) were analyzed using crosstables with the chi square test for significance. Student’s t test with Levene’s test for equality of variance was used to analyze continuous variables (eg, height, weight, outcome score totals). We performed all analyses using SPSS, Version 15 (SPSS, Inc, Chicago, IL).
Results
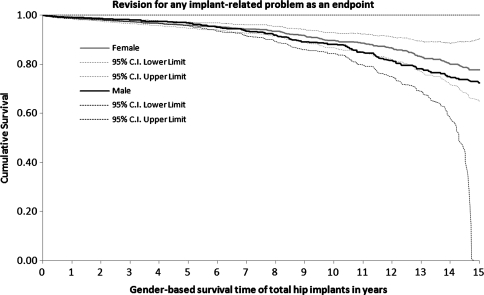
Kaplan–Meier survivorship analysis between the two genders showed no difference (p > 0.14) with a revision rate for women of 8.3% versus 9.3% in men excluding infections (p = 0.16) (Fig. 1). Women had four major intraoperative femur fractures recorded in this group compared with three in the men.
Fig. 1.
Gender-based Kaplan–Meier survivorship graph is shown. CI = confidence interval.
Reasons for revision were similar in males and females. There was no difference in revision rate for aseptic loosening (p = 0.691), implant failure (p = 0.570), periprosthetic fracture (p = 0.246), polyethylene wear (p = 0.065), osteolysis (p = 0.837), or infection (p = 0.930). Females underwent revision more often (p = 0.0375) for instability than males. There were no revisions for leg length problems.
Women had decreased pre- and postoperative health-related quality-of-life scores compared with men, including Harris hip score (Table 2), WOMAC (Table 3), and SF-12 (Table 4). The mean Harris hip scores in men preoperatively were 46 ± 14 with postoperative scores of 87 ± 15, which are greater (p < 0.0001) compared with the female preoperative mean of 42 ± 14 and postoperative mean of 83 ± 16 (Table 2). The male WOMAC scores were 42 ± 16 preoperatively and 78 ± 21 postoperatively with women again scoring lower (p < 0.0001) at 37 ± 16 and 74 ± 22 (Table 3). The SF-12 scores reflected similar findings with men scoring 30 ± 7 preoperatively and 42 ± 11 postoperatively compared with women with scores of 28 ± 7 before surgery and 38 ± 11 after surgery (Table 4).
Table 2.
Harris hip preoperative, postoperative, and change scores
| Variable | Harris Hip score category | Group | Significance | Mean | Standard deviation |
|---|---|---|---|---|---|
| Preoperative | Pain | Female | 0.001 | 16.8 | 8.3 |
| Male | 17.9 | 7.9 | |||
| Function | Female | 0.001 | 20 | 8 | |
| Male | 23.1 | 8.4 | |||
| Total | Female | 0.001 | 41.6 | 14.3 | |
| Male | 45.8 | 14.2 | |||
| Latest | Pain | Female | 0.029 | 39.5 | 8.5 |
| Male | 40.1 | 7.7 | |||
| Function | Female | 0.001 | 34.8 | 10.1 | |
| Male | 38.7 | 8.8 | |||
| Total | Female | 0.001 | 83 | 15.7 | |
| Male | 87.3 | 14.6 | |||
| Change | Pain | Female | 0.450 | 22.5 | 11.9 |
| Male | 22.2 | 10.6 | |||
| Function | Female | 0.094 | 15.1 | 10.6 | |
| Male | 15.8 | 10.1 | |||
| Total | Female | 0.608 | 41.5 | 19.2 | |
| Male | 41.9 | 18.3 |
Table 3.
WOMAC preoperative, postoperative, and change scores
| Variable | WOMAC scoring category | Group | Significance | Mean | Standard deviation |
|---|---|---|---|---|---|
| Preoperative | Pain | Female | 0.001 | 39 | 18 |
| Male | 44.9 | 17.5 | |||
| Joint stiffness | Female | 0.007 | 35.9 | 19.8 | |
| Male | 38.6 | 20.4 | |||
| Function | Female | 0.001 | 35.1 | 17.1 | |
| Male | 39.9 | 16.8 | |||
| Total | Female | 0.001 | 36.9 | 16 | |
| Male | 41.7 | 15.9 | |||
| Latest | Pain | Female | 0.001 | 76.9 | 23.3 |
| Male | 80.5 | 22.1 | |||
| Joint stiffness | Female | 0.001 | 70.1 | 25 | |
| Male | 73.9 | 24.4 | |||
| Function | Female | 0.001 | 71.6 | 23.8 | |
| Male | 76.4 | 22.7 | |||
| Total | Female | 0.001 | 73.5 | 22.1 | |
| Male | 77.6 | 21.5 | |||
| Change | Pain | Female | 0.011 | 39.4 | 26.7 |
| Male | 36.1 | 24.5 | |||
| Joint stiffness | Female | 0.828 | 35.3 | 29.2 | |
| Male | 35.8 | 28.8 | |||
| Function | Female | 0.174 | 39.3 | 26 | |
| Male | 37.5 | 24.5 | |||
| Total | Female | 0.107 | 38.6 | 24.8 | |
| Male | 36.6 | 23.6 |
Table 4.
SF-12 preoperative, postoperative, and change scores
| Variable | SF-12 score category | Group | Significance | Mean | Standard deviation |
|---|---|---|---|---|---|
| Preoperative | Mental | Female | 0.001 | 50.3 | 11.3 |
| Male | 53.6 | 11.2 | |||
| Physical | Female | 0.001 | 27.8 | 6.7 | |
| Male | 29.8 | 7.4 | |||
| Latest | Mental | Female | 0.021 | 52.7 | 10.4 |
| Male | 53.6 | 9.7 | |||
| Physical | Female | 0.001 | 37.8 | 11.3 | |
| Male | 41.6 | 11.2 | |||
| Change | Mental | Female | 0.001 | 2.6 | 11.9 |
| Male | 0.4 | 11.3 | |||
| Physical | Female | 0.072 | 11.4 | 12.3 | |
| Male | 12.6 | 12.4 |
We observed no difference in the overall differential scores from pre- to postoperatively between male and female patients, although women had greater improvement than men in two subsets of health-related quality-of-life scores. Harris hip change score was 42 ± 18 for men and 42 ± 19 for women. The WOMAC scores for men and women were 39 ± 24 and 39 ± 25, respectively, and the SF-12 score was identical for the genders at 11 ± 12. Women had greater (p < 0.0001) improvement in SF-12 mental scores with a change score of 2.6 compared with 0.4 for men. The pain component of the WOMAC score also improved (p < 0.01) more in women with a change score of 39.4 compared with 36.1 for men (Tables 2–4).
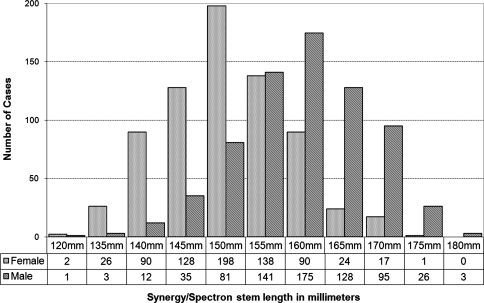
Using a subset of 1414 patients who had the same implant types (Synergy or Spectron stems; Smith and Nephew, Inc), we observed differences in implant-related factors between the genders. We more frequently used a high-offset stem in men than in women (61.8% in men versus 42.4% in women, p < 0.0001). We also more frequently used higher mean stem lengths, neck offset, and neck lengths in men (Fig. 2) (p < 0.0001 in all cases).
Fig. 2.
Stem length (reflecting stem size) distribution is shown in males and females.
Discussion
Our study rationale was to investigate gender-based differences in THA outcomes, including survivorship, revision reasons, outcomes including quality-of-life and function scores, and differences in implant size and offset. We strive to demonstrate that despite the use of nongender-specific implants, there is no major difference between male and female outcomes. Limitations of this study include the concern that leg length difference pre- and postoperatively and offset restoration are not measured. Our database does not capture this information. However, there were no revisions in either males or females for leg length problems. As well, at our institution, a leg length and offset guide is routinely used intraoperatively to optimize restoration of leg length and offset based on our preoperatively templated plan. Other limitations include the retrospective nature of the study, although all data were collected in a prospective fashion.
Our data using a large cohort with prospectively gathered data indicate no difference in survivorship of implants comparing men with women. This finding that implants in women do as well or better than implants in men with similar complication rates has been corroborated in previous studies [7]. Large registries such as the Swedish Total Hip Replacement Register confirm that revision rates have been equal for men and women over the years [10]. Reasons for revision were also the same between genders [10].
There was no difference between genders in improvement of health-related quality-of-life outcomes. However, there are certain differences between male and female patients that are apparent based on this and previous research. Women are older when they have joint arthroplasty, which may reflect a greater fear of surgery and delaying surgery to avoid disrupting caregivers’ roles [6]. Our data showing lower health-related quality-of-life scores preoperatively confirm previous studies indicating women are more disabled than men at the time of THA [4, 6, 8]. Gender differences in terms of accessing care are also a factor [3] with women underusing joint arthroplasty compared with men.
Regarding anatomic differences (reflecting sizing and offset of implant issues), both the forensic and hip fracture/osteoporosis literature have a number of interesting findings in terms of gender-based differences in the proximal femur. Forensic literature cites differences between genders of the same race in the anatomic dimensions of the proximal femur (maximal vertical and horizontal dimensions of the femoral head, cortical thickness, medullary diameter) in addition to dual-energy xray absorptiometry and radiographic differences [14, 18, 19]. The gender in 90% of femora can be determined by gross anatomic examination of the femur en bloc and the femoral head in isolation [11, 15]. The gross dimensions of the proximal femur can also be used with great accuracy [16].
Bone aging in the proximal femur has different effects on men compared with women [20]. Women tend to increase trochanteric bone area, whereas men tend to increase femoral neck area with these differing trends being independent of height and weight in this Chinese study [18].
However, a substantial proportion of the proximal femoral morphology and density observed between the genders is based on size differences [9], and differences between races are also important. Wheatley [19] reported a difference in proximal femoral bone density between black and white women taking weight into consideration as well. Nelson et al. [13] found differences between black and white women in terms of bone density in the proximal femur as well as cross-sectional geometric measures of the neck with a smaller endocortical diameter in black female patients. Forensic data on gender-based differences must of necessity take race into account. These differences are also seen in the hip fracture literature with not only gender differences in proximal femoral morphology and strength, but race as well [12].
Clearly, gender differences do exist in terms of the timing of patients’ access to surgical treatment, use of arthroplasty, and level of disability before treatment. Variations in proximal femoral bone density and morphology do exist; multiple factors, including race, individual size and weight, presence or absence of osteoporosis, and gender, all play a role. However, there is no evidence that current or historical implants have been associated with any gender-based difference in outcomes that necessitates newer and more expensive implants. Improvement in outcomes with multiple different stems over 25 years of multisurgeon clinical experience remains excellent for both female and male patients.
Acknowledgments
We thank Kory Charron for his assistance with the statistical analysis.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Booth RE Jr. The gender-specific (female) knee. Orthopedics. 2006;29:768–769. [DOI] [PubMed]
- 2.Booth RE Jr. Sex and the total knee: gender-sensitive designs. Orthopedics. 2006;29:836–838. [DOI] [PubMed]
- 3.Hawker G, Wright J, Coyte P, Williams J, Harvey B, Glazier R, Badley E. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342:1044–1045. [DOI] [PubMed]
- 4.Holtzman J, Saleh K, Kane R. Gender differences in functional status and pain in a Medicare population undergoing elective total hip arthroplasty. Med Care. 2002;40:461–470. [DOI] [PubMed]
- 5.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [DOI]
- 6.Karlson EW, Daltroy LH, Liang MH, Eaton HE, Katz JN. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med. 1997;102:524–530. [DOI] [PubMed]
- 7.Katz JN, Wright EA, Guadagnoli E, Liang MH, Karlson EW, Cleary PD. Differences between men and women undergoing major orthopedic surgery for degenerative arthritis. Arthritis Rheum. 1994;37:687–694. [DOI] [PubMed]
- 8.Kennedy D, Hanna S, Stratford P, Wessel J, Gollish J. Preoperative function and gender predict pattern of functional recovery after hip and knee arthroplasty. J Arthroplasty. 2006;21:559–566. [DOI] [PMC free article] [PubMed]
- 9.Looker A, Beck T, Orwoll E. Does body size account for gender differences in femur bone density and geometry? J Bone Miner Res. 2001;16:1291–1299. [DOI] [PubMed]
- 10.Malchau H, Herberts P, Eisler T, Garellick G, Söderman P. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84:2–20. [DOI] [PubMed]
- 11.Mall G, Graw M, Gehring K, Hubig M. Determination of sex from femora. Forensic Sci Int. 2000;113:315–321. [DOI] [PubMed]
- 12.Marshall LM, Zmuda JM, Chan BK, Barrett-Connor E, Cauley JA, Ensrud KE, Lang TF, Orwoll ES; Osteoporotic Fractures in Men (MrOS) Research Group. Race and ethnic variation in proximal femur structure and BMD among older men. J Bone Miner Res. 2008;23:121–130. [DOI] [PMC free article] [PubMed]
- 13.Nelson D, Barondess D, Hendrix S, Beck T. Cross-sectional geometry, bone strength, and bone mass in the proximal femur in black and white postmenopausal women. J Bone Miner Res. 2000;15:1992–1997. [DOI] [PubMed]
- 14.Peacock M, Liu G, Carey M, Ambrosius W, Turner C, Hui S, Johnston CJ. Bone mass and structure at the hip in men and women over the age of 60 years. Osteoporosis Int. 1998;8:231–239. [DOI] [PubMed]
- 15.Purkait R. Sex determination from femoral head measurements: a new approach. Leg Med (Tokyo). 2003;5 (Suppl 1):S347–S350. [DOI] [PubMed]
- 16.Purkait R. Triangle identified at the proximal end of femur: a new sex determinant. Forensic Sci Int. 2005;147:135–139. [DOI] [PubMed]
- 17.Röder C, Parvizi J, Eggli S, Berry D, Müller M, Busato A. Demographic factors affecting long-term outcome of total hip arthroplasty. Clin Orthop Relat Res. 2003;417:62–73. [DOI] [PubMed]
- 18.Tsai K, Cheng W, Sanchez T, Chen C, Chieng P, Yang R. Bone densitometry of proximal femur in Chinese subjects: gender differences in bone mass and bone areas. Bone. 1997;20:365–369. [DOI] [PubMed]
- 19.Wheatley B. An evaluation of sex and body weight determination from the proximal femur using DXA technology and its potential for forensic anthropology. Forensic Sci Int. 2005;147:141–145. [DOI] [PubMed]
- 20.Yates LB, Karasik D, Beck TJ, Cupples LA, Kiel DP. Hip structural geometry in old and old-old age: similarities and differences between men and women. Bone. 2007;41:722–732. [DOI] [PMC free article] [PubMed]