Abstract
Current outcomes data on revision total hip arthroplasty focuses on specific implants and techniques rather than more general outcomes. We therefore examined a large consecutive series of failed THAs undergoing revision to determine if survivorship and modes of failure differ in comparison to the current data. We retrospectively reviewed the medical records of 1100 revision THAs. The minimum followup was 2 years (mean, 6 years; range, 0–20.4 years). Eighty-seven percent of revision total hips required no further surgery; however, 141 hips (13%) underwent a second revision at a mean of 3.7 years (range, 0.025–15.9 years). Seventy percent (98 hips) had a second revision for a diagnosis different from that of their index revision, while 30% (43 hips) had a second revision for the same diagnosis. The most common reasons for failure were instability (49 of 141 hips, 35%), aseptic loosening (42 of 141 hips, 30%), osteolysis and/or wear (17 of 141 hips, 12%), infection (17 of 141 hips, 12%), miscellaneous (13 of 141 hips, 9%), and periprosthetic fracture (three of 141 hips, 2%). Survivorship for revision total hip arthroplasty using second revision as endpoint was 82% at 10 years. Aseptic loosening and instability accounted for 65% of these failures.
Level of Evidence: Level IV, therapeutic (retrospective) study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The success of primary total hip arthroplasty is well-documented in the literature with survival rates over 90% at 15-year followup [7–9, 17, 34, 39]. As our population ages, the number of total hip arthroplasties performed is increasing dramatically. Unfortunately, some are not successful and have eventual revision. Recent projections indicate the burden of revision total hip arthroplasty is expected to increase by 137% over the next 25 years [29]. In addition, the cost and resource utilization of revision procedures are substantially higher than those of primary procedures [4]. While a majority of patients are subjectively satisfied with their revision hip arthroplasty, many have unrealistic expectations regarding the longevity of their revision procedure [3, 11, 31, 44, 45].
The current body of literature on revision total hip arthroplasty focuses mainly on the success of certain types of implants [23, 26, 32, 33, 50, 52], treating specific defects [12, 38, 41], or evaluating specific techniques [6, 47–49]. Survival rates in the literature on revision total hip arthroplasty range from 35% at 10 years for cemented revisions [43] to 100% at 10 years for femoral revision with impaction grafting [46]. Most of the literature on revision THA focuses on specific techniques or implants, rather than outcomes from a variety of approaches and it is unclear whether specific data applies generally.
Therefore, considering patients undergoing revision for a variety of failures and approaches, we raised the following questions: (1) What is the survival probability of index revision hip surgery? (2) What are the most common reasons for the failure of index revision? (3) Have the reasons for failure changed over the time period of the study? Finally, we sought to determine if failures were different in comparison to the current literature on specific techniques and implants in revision total hip arthroplasty and identify areas where improvement is needed.
Materials and Methods
We retrospectively reviewed all 1036 patients (1100 hips) who had revision hip arthroplasties for a variety of indications (Table 1) performed between 1986 and August 2005. There were 594 women and 442 men. The average age was 63.7 years (range, 22–96 years). We identified failed revision hips that had a second revision based on a query of prospectively collected registry data. Periodic audits and comparisons between the institutions practice management data and registry data are performed to ensure completeness of data. The minimum followup was 2 years (mean, 6 years; range, 0–20.4 years).
Table 1.
Indicators for initial revision (N = 1100) from 1985 to 2005
| Initial diagnosis | N (%) |
|---|---|
| Aseptic loosening | 498 (45%) |
| Instability | 172 (16%) |
| Osteolysis/wear | 172 (16%) |
| Deep periprosthetic infection | 118 (11%) |
| Periprosthetic fracture | 63 (6%) |
| Miscellaneous | 77 (7%) |
Revision surgery was defined as any surgery that involved an open procedure to address a mode of failure of the primary hip arthroplasty. It included revision of any major component (acetabular or femoral) as well as exchange of modular parts (femoral head and acetabular liner) and irrigation and débridement to treat deep periprosthetic infection. Closed reductions were not categorized as revision procedures. If patients had not been evaluated within 6 months, we conducted phone surveys to confirm the patient had not undergone revision of the implant for any reason. Lost to followup was defined using a 24-month endpoint. Exhaustive methods were used to locate all patients. One-hundred and eleven patients (114 hips) were categorized as lost-to-followup for the following reasons: five patients were infirmed; 28 patients were contacted but refused followup; and 78 patients had inaccurate contact information.
Time to failure was defined as the period from index revision surgery to repeat revision surgery. Index revision diagnosis was determined based on information entered into the database by the operating surgeon determined at the time of revision and cross-referenced with ICD-9 codes. The failure rate was determined using the ratio of the number having repeat surgery to the total number. Time to failure and failure rate were calculated for the entire cohort as well as by each diagnosis. The dates of index revision were stratified into three equivalent time periods. Time periods were defined based on three equal periods during which the study took place. Time period 1 was index revision performed from January 1986 through July 15, 1992; time period 2 from July 1, 1992 through February 28, 1999; and time period 3 from February 29, 1999 through August 2005.
We calculated standard descriptive statistics including mean, range, frequency, and proportions for diagnosis and time to failure. Survivorship analysis was conducted using the Kaplan-Meier method using second revision for any reason as the endpoint; survival probability was estimated with 95% confidence intervals [15]. All patients were included regardless of lost-to-followup status. Cases were censored at their last followup evaluation or date of death. Survivorship was calculated for the entire cohort as well as each failure mechanism. Statistical differences in failure rate over time were determined using a 3 × 2 chi square analysis at an a priori significance level of 0.05.
Results
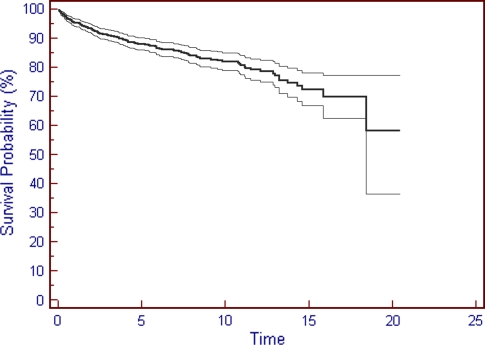
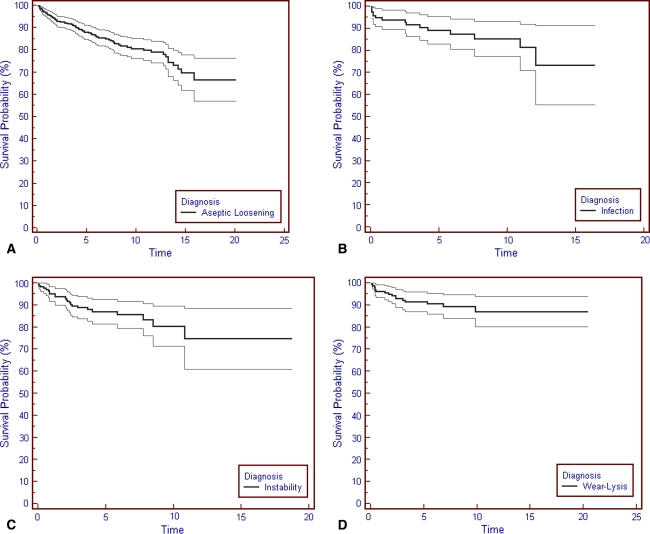
Overall survivorship at 10 years was 82% (95% CI ± 4%) and 72.6% at 15 years (95% CI ± 6%) (Fig. 1). Survivorship was also determined based on diagnosis at time of index revision (Fig. 2A–D). Survivorship for those patients initially revised for aseptic loosening using second revision for any reason was 81% (95% CI ± 4%) at 10 years and 70% at 15 years (95% CI ± 8%). For those patients initially revised for a diagnosis of instability using second revision for any reason, survivorship was 86% (95% CI ± 10%) at 8 years. For those patients initially revised for a diagnosis of osteolysis/wear using second revision for any reason, survivorship was 90% at 5 years (95% CI ± 4%) and 87% at 10 years (95% CI ± 6%). For those patients initially revised for a diagnosis of infection using second revision for any reason, survivorship was 87% at 6 years (95% CI ± 6%) and 81% at 11 years (95% CI ± 10%). One hundred and forty-one (13%) revision total hip arthroplasties in 139 patients failed and underwent a second revision (Table 2). The average time to failure from the index revision was 44 months (range, 0.3–190.3 months). The average age of these 65 men and 74 women was 57.9 years (range, 22–86 years). Of the 911 patients (959 hips) that did not require a second revision, there were 526 women and 385 men at an average age of 64.2 (range, 22.3–96.2 years).
Fig. 1.
The Kaplan-Meier survivorship for 1100 hips undergoing index revision total hip arthroplasty from 1985 to 2005 used second revision for any reason as an endpoint. Survivorship at 10 years was 82% and at 15 years was 72.6%.
Fig. 2A–D.
The Kaplan-Meier survivorship for index revision total hip arthroplasty based on initial index revision diagnosis is shown. Results presented are based on (A) a diagnosis of aseptic loosening; (B) a diagnosis of infection; (C) a diagnosis of instability; and (D) a diagnosis of wear-lysis.
Table 2.
Reasons for failure requiring second revision (N = 141)
| Initial diagnosis | N (%) |
|---|---|
| Instability | 49 (35%) |
| Aseptic loosening | 42 (30%) |
| Osteolysis/wear | 17 (12%) |
| Deep periprosthetic infection | 17 (12%) |
| Miscellaneous | 13 (9%) |
| Periprosthetic fracture | 3 (2%) |
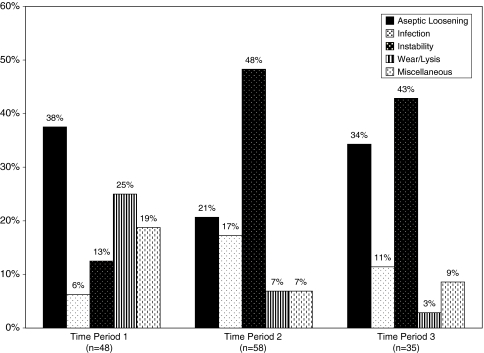
Of the 1100 index revision procedures, 43 hips (30%) had a second revision for the same diagnosis as their index revision, while 98 hips (70%) underwent a second revision for a different diagnosis than their index revision. Over the 236-month time period examined by this study, the major reasons for failure of revision total hip arthroplasty were instability and aseptic loosening (Fig. 3).
Fig. 3.
The most common modes of failure for revision total hip arthroplasty for three equivalent time periods during the study were determined. Instability and infection remained common modes of failure throughout the study, while aseptic loosening and wear/osteolysis were more common modes of failure for those patients revised early in the study.
The percentages of failure changed (p < 0.001) over the time of the study, although aseptic loosening and instability were the primary modes of failure throughout. For revisions performed during time period 1, the most common reasons for failure were aseptic loosening (38%) and wear/osteolysis (25%). For revisions performed during time period 2, the most common reasons for failure were instability (48%), aseptic loosening (21%), and infection (17%). For revisions performed during time period 3, the most common reasons for failure were instability (43%) and aseptic loosening (34%).
Discussion
There is little doubt modern primary total hip arthroplasty has achieved excellent and predictable long-term clinical success [7–9, 17, 34, 39]. Not all primary total hip replacements are successful however. Most outcome studies of revision arthroplasty consider specific mechanisms of failure, techniques, or implants. We therefore raised the following questions considering all revisions in general: (1) What is the survival probability of index revision hip surgery? (2) What are the most common reasons for the failure of index revision? (3) Have the reasons for failure changed over the time period of the study?
There are some limitations with this current study. We chose to use re-revision surgery as our endpoint for failure. Although this is a firm, objective endpoint, patients with radiographic failure, those who have yet to come to second revision, and those with instability treated by closed means were not included as failures. Paprosky et al. [37] reported a 4% radiographic failure rate using extensively porous-coated stems for femoral revision at a mean followup of 13.2 years. Only one patient was awaiting revision surgery. In the study by Haydon [21], survivorship of the cemented femoral component in revision total hip arthroplasty using revision for any reason was 87% at 10 years but decreased to 71% when including radiographic failures. Thus, our ultimate failure rate will likely be higher than reported here with further time since the index revision.
The overall survivorship of revision total hip arthroplasty in our study using re-revision as an endpoint was 82% at 10 years and 72.6% at 15 years (Fig. 1). The results of survivorship in revision total hip arthroplasty for a variety of techniques were evaluated (Table 3). In 1989, Retpen et al. [43] reported overall survival of 35% for revision total hip arthroplasty at an average of 120 months. Englebrecht et al. [16], reviewing the results of mainly cemented revisions, reported an 8.8% failure rate at an average followup of 7.4 years in 138 revisions. An additional 43 stems and 53 cups however had radiographic evidence of loosening. More recently, McCarthy et al. [33] reported on the results of cementless modular revision total hip arthroplasty. The survivorship at 14 years was 60%. Aseptic loosening in patients with compromised femoral bone accounted for the majority of failures.
Table 3.
Failure by diagnosis
| Initial revision diagnosis | N (%) | Second revision diagnosis | N (%) | Time to failure in months (range) |
|---|---|---|---|---|
| Aseptic loosening | 74 (15%) | 54.1 (1.7–190.3) | ||
| Aseptic loosening | 31 (43%) | |||
| Instability | 20 (27%) | |||
| Osteolysis/wear | 12 (16%) | |||
| Miscellaneous | 6 (7%) | |||
| Infection | 4 (5%) | |||
| Periprosthetic fracture | 1 (1%) | |||
| Instability | 21 (12%) | 34.5 (1–129.6) | ||
| Instability | 12 (57%) | |||
| Aseptic loosening | 3 (14%) | |||
| Infection | 2 (10%) | |||
| Osteolysis/wear | 2 (10%) | |||
| Implant fracture | 2 (10%) | |||
| Osteolysis/wear | 16 (9%) | 29.9 (0.7–117.6) | ||
| Instability | 7 (44%) | |||
| Implant fracture | 2 (12.5%) | |||
| Infection | 2 (12.5%) | |||
| Osteolysis/wear | 2 (12.5%) | |||
| Aseptic loosening | 1 (6%) | |||
| Failed bipolar | 1 (6%) | |||
| Periprosthetic fracture | 1 (6%) | |||
| Deep periprosthetic infection | 13 (11%) | 37.7 (0.5–145.1) | ||
| Infection | 6 (38%) | |||
| Instability | 5 (36%) | |||
| Aseptic loosening | 1 (8%) | |||
| Periprosthetic fracture | 1 (8%) | |||
| Periprosthetic fracture | 9 (14%) | 13.2 (0.3–49.4) | ||
| Aseptic loosening | 3 (33.3%) | |||
| Infection | 3 (33.3%) | |||
| Instability | 3 (33.3%) | |||
Our data and that in the literature suggest aseptic loosening and instability continue to be the primary modes of failure for both primary and revision total hip arthroplasty (Table 4) [5, 14, 25, 33, 40, 42]. We found aseptic loosening and instability accounted for 61% of the index revision surgeries. Sixty-five percent of second revisions also were performed for either aseptic loosening (30%) or instability (35%). The majority of failures for aseptic loosening that occurred on the femoral side were associated with proximally coated femoral stems. The majority of femoral stems used at our institution were fully porous-coated stems and failure due to aseptic loosening was rare. This data coincides with the literature on low rates of failure for fully porous-coated stems and high failure rate with proximally porous-coated revision stems [5, 18, 36, 37, 40, 51].
Table 4.
Literature review of revision total hip survivorship
| Author | Year | Number of patients | Followup | Type of revision | Survivorship of revision THA | Most common modes of failure |
|---|---|---|---|---|---|---|
| Repten et al. [43] | 1989 | 306 | 120 months | Cemented revisions (both components) | 35% @ 120 months | Aseptic loosening |
| Kershaw et al. [27] | 1991 | 191 | 75 months | Cemented revisions (both components) | 77% @ 10 years | Aseptic loosening |
| Stromberg & Herberts [49] | 1994 | 59 | 10 years | Cemented revisions pt < 55 years of age (both components) | 48% @ 10 years | Aseptic loosening |
| Berry et al. [5] | 1995 | 375 | 4.7 years | Proximally coated femoral revisions | 58% @ 8 years | Aseptic loosening |
| Iorio et al. [25] | 1995 | 89 | 7.7 years | Cemented revisions (both components) | 76% @ 10 years | Aseptic loosening |
| Peters et al. [40] | 1995 | 49 | 65 months | Proximally coated femoral revisions | 37% @ 72 months | Aseptic loosening |
| Raut et al. [42] | 1995 | 387 | 5.5 years | Cemented acetabular revisions | 85% @ 10 years | Aseptic loosening and instability |
| Paprosky et al. [37] | 1999 | 170 | 13.2 years | Fully porous-coated femoral revisions | 95% @ 13 years | Aseptic loosening |
| Gramkow et al. [20] | 2001 | 84 | 11.4 years | Cemented femoral revisions | 77.9% @ 10 years | Aseptic loosening |
| Whaley et al. [53] | 2001 | 89 | 7.2 years | Acetabular revision with cementless jumbo cups | 93% @ 10 years | Aseptic loosening |
| Head et al. [22] | 2001 | 1179 | 6.2 years | Cementless calcar femoral revisions | 93.6% @ 13 years | Aseptic loosening |
| Engh et al. [18] | 2002 | 34 | 13.3 years | Fully porous stems for severe bone loss | 89% @ 10 years | Aseptic loosening |
| Gerber et al. [19] | 2003 | 61 | min 5 years | Acetabular revision with reinforcement ring | 81% @ 10 years | Aseptic loosening |
| Kwong et al. [30] | 2003 | 143 | 40 months | Modular cementless femoral component revisions | 97.2% @ 5 years | Infection |
| Haydon et al. [21] | 2004 | 129 | min 5 years | Cemented femoral revisions | 71% @ 10 years | Aseptic loosening |
| Hungerford et al. [24] | 2006 | 30 | 8.2 years | Cemented and cementless femoral component revisions | 90% @ 5 years | Aseptic loosening |
| 55% @ 10 years | ||||||
| 27% @ 20 years | ||||||
| Della Valle [14] | 2005 | 138 | 15 years | Cementless acetabular revisions | 81% @ 15 years | Instability |
| Schreurs et al. [46] | 2006 | 33 | 10.4 years | Femoral revision with impaction grafting | 100% @ 10 years | No failures |
| McCarthy & Lee [33] | 2007 | 62 | 14 years | Modular cementless femoral component revisions | 60% @ 14 years | Aseptic loosening |
| Springer et al. | 2008 | 1036 | min 2 years | All revisions | 82% @ 10 years | Instability and aseptic loosening |
Recent reports on cementless hemispherical acetabular fixation in revision surgery have shown promising result with a reported survivorship of 97% at 15-year followup for cementless hemispherical acetabular revisions [13, 14]. Recently, newer 3-D ingrowth materials have been introduced by several manufactures. These implants have highly porous surfaces (eg, trabecular metal) with biological substrates that allow for high bony ingrowth rates. In addition, a high coefficient of friction improves initial stability at the time of implantation. Early to mid-term results even in patients with severe acetabular bone stock deficiency have been promising [50].
Instability is the leading cause of failure in revision total hip arthroplasty and results in the literature range from 2% to 16% [1, 35]. The cause of dislocation after revision total hip arthroplasty is related to multiple etiologies, including patient factors, component design and position, and status of the surrounding soft tissue and muscles. Alberton et al. [1] reported a 7.4% failure rate due to instability after revision total hip arthroplasty. Trochanteric nonunion and small head sizes (22 mm) were associated with higher rates of dislocation. Only 57% of hips were stable at latest followup. We similarly found instability as the leading cause of failure leading to repeat revision. The lack of readily available large-head technology and constrained component options during the span of this 20-year study could have contributed to this finding. All failures having repeat revision for instability in our series were performed prior to 2000. All patients were treated with 28-mm heads with either extended neck length or offset/elevated liners. Larger head sizes and posterior capsular repair may have reduced the incidence of this complication recently. However, little published data exists as to their role in preventing this complication in the revision setting [2, 10, 28, 54].
We evaluated the modes of failure in revision hip arthroplasty and to identify areas where improvement is needed. Overall survivorship of revision total hip arthroplasty at 10 years was 82%. Instability and aseptic loosening accounted for 65% of these failures. Additional focus on these two areas should be made by the revision surgeon to diminish the need for re-revision.
Acknowledgments
We thank Anne Dennos, Amanda Phillips, and Caryn Thompson, CCRC, of the OrthoCarolina Research Institute for all of their hard work in collecting data for this project.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her Institutional Review Board has approved the reporting of this data, and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment option. J Bone Joint Surg Am. 2002;84:1788–1792. [PubMed]
- 2.Amstutz HC, Le Duff MJ, Beaulé PE. Prevention and treatment of dislocation after total hip replacement using large diameter balls. Clin Orthop Relat Res. 2004;429:108–116. [DOI] [PubMed]
- 3.Barrack RL, McClure JT, Burak CF, Clohisy JC, Parvizi J, Hozack W. Revision total hip arthroplasty: the patient’s perspective. Clin Orthop Relat Res. 2006;453:173–177. [DOI] [PubMed]
- 4.Barrack RL, Sawhney J, Hsu J, Cofield RH. Cost analysis of revision total hip arthroplasty A 5-year followup study. Clin Orthop Relat Res. 1999;369:175–178. [DOI] [PubMed]
- 5.Berry DJ, Harmsen WS, Ilstrup D, Lewallen DG, Cabanela ME. Survivorship of proximally porous-coated femoral components. Clin Orthop Relat Res. 1995;319:168–177. [PubMed]
- 6.Boldt JG, Dilawari P, Agarwal S, Drabu KJ. Revision total hip arthroplasty using impaction bone grafting with cemented nonpolished stems and Charnley cups. J Arthroplasty. 2001;16:943–952. [DOI] [PubMed]
- 7.Callaghan JJ, Templeton JE, Liu SS, Pedersen DR, Goetz DD, Sullivan PM, Johnston RC. Results of Charnley total hip arthroplasty at a minimum of thirty years. A concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86:690–695. [DOI] [PubMed]
- 8.Callaghan JJ, Tooma GS, Olejniczak JP, Goetz DD, Johnston RC. Primary hybrid total hip arthroplasty: an interim followup. Clin Orthop Relat Res. 1996;333:118–125. [DOI] [PubMed]
- 9.Capello WN, D’Antonio JA, Feinberg JR, Manley MT. Ten-year results with hydroxyapatite-coated total hip femoral components in patients less than fifty years old. A concise follow-up of a previous report. J Bone Joint Surg Am. 2003;85:885–889. [DOI] [PubMed]
- 10.Chivas DJ, Smith K, Tanzer M. Role of capsular repair on dislocation in revision total hip arthroplasty. Clin Orthop Relat Res. 2006;453:147–152. [DOI] [PubMed]
- 11.Davis AM, Agnidis Z, Badley E, Kiss A, Waddell JP, Gross AE. Predictors of functional outcome two years following revision hip arthroplasty. J Bone Joint Surg Am. 2006;88:685–691. [DOI] [PubMed]
- 12.DeBoer DK, Christie MJ, Brinson MF, Morrison JC. Revision total hip arthroplasty for pelvic discontinuity. J Bone Joint Surg Am. 2007;89:835–840. [DOI] [PubMed]
- 13.Della Valle CJ, Berger RA, Rosenberg AG, Galante JO. Cementless acetabular reconstruction in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;420:96–100. [DOI] [PubMed]
- 14.Della Valle CJ, Shuaipaj T, Berger RA, Rosenberg AG, Shott S, Jacobs JJ, Galante JO. Revision of the acetabular component without cement after total hip arthroplasty A concise follow-up, at fifteen to nineteen years, of a previous report. J Bone Joint SurgAm. 2005;87:1795–1800. [DOI] [PubMed]
- 15.Dorey F, Amstutz H. Survivorship analysis in the evaluation of joint replacement. J Arthroplasty. 1986;1:63–69. [DOI] [PubMed]
- 16.Engelbrecht DJ, Weber FA, Sweet MB, Jakim I. Long-term results of revision total hip arthroplasty. J Bone Joint Surg Br. 1990;72:41–45. [DOI] [PubMed]
- 17.Engh CA, Culpepper WJ, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79:177–184. [DOI] [PubMed]
- 18.Engh CA Jr, Ellis TJ, Koralewicz LM, McAuley JP, Engh CA Sr. Extensively porous-coated femoral revision for severe femoral bone loss: minimum 10-year follow-up. J Arthroplasty. 2002;17:955–960. [DOI] [PubMed]
- 19.Gerber A, Pisan M, Zurakowski D, Isler B. Ganz reinforcement ring for reconstruction of acetabular defects in revision total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2358–2364. [DOI] [PubMed]
- 20.Gramkow J, Jensen TH, Varmarken JE, Retpen JB. Long-term results after cemented revision of the femoral component in total hip arthroplasty. J Arthroplasty. 2001;16:777–783. [DOI] [PubMed]
- 21.Haydon CM, Mehin R, Burnett S, Rorabeck CH, Bourne RB, McCalden RW, MacDonald SJ. Revision total hip arthroplasty with use of a cemented femoral component. Results at a mean of ten years. J Bone Joint Surg Am. 2004;86:1179–1185. [DOI] [PubMed]
- 22.Head WC, Emerson RH Jr, Higgins LL. A titanium cementless calcar replacement prosthesis in revision surgery of the femur: 13-year experience. J Arthroplasty. 2001;16:183–187. [DOI] [PubMed]
- 23.Holt GE, Dennis DA. Use of custom triflanged acetabular components in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;429:209–214. [DOI] [PubMed]
- 24.Hungerford MW, Hungerford DS, Khanuja HS, Pietryak BP, Jones LC. Survivorship of femoral revision hip arthroplasty in patients with osteonecrosis. J Bone Joint SurgAm. 2006;88(Suppl 3):126–130. [DOI] [PubMed]
- 25.Iorio R, Eftekhar NS, Kobayashi S, Grelsamer RP. Cemented revision of failed total hip arthroplasty. Survivorship analysis. Clin Orthop Relat Res. 1995;316:121–130. [PubMed]
- 26.Kelly SJ, Incavo SJ, Beynnon B. The use of a hydroxyapatite-coated primary stem in revision total hip arthroplasty. J Arthroplasty. 2006;21:64–71. [DOI] [PubMed]
- 27.Kershaw CJ, Atkins RM, Dodd CA, Bulstrode CJ. Revision total hip arthroplasty for aseptic failure A review of 276 cases. J Bone Joint Surg Br. 1991;73:564–568. [DOI] [PubMed]
- 28.Kung PL, Ries MD. Effect of femoral head size and abductors on dislocation after revision THA. Clin Orthop Relat Res. 2007;465:170–174. [DOI] [PubMed]
- 29.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. [DOI] [PubMed]
- 30.Kwong LM, Miller AJ, Lubinus P. A modular distal fixation option for proximal bone loss in revision total hip arthroplasty: a 2- to 6-year follow-up study. J Arthroplasty. 2003;18:94–97. [DOI] [PubMed]
- 31.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2003;85:27–32. [DOI] [PubMed]
- 32.McCarthy JC, Lee JA. Constrained acetabular components in complex revision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:210–215. [DOI] [PubMed]
- 33.McCarthy JC, Lee JA. Complex revision total hip arthroplasty with modular stems at a mean of 14 years. Clin Orthop Relat Res. 2007;465:166–169. [DOI] [PubMed]
- 34.Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME. Minimum ten-year follow-up of a straight-stemmed, plasma-sprayed, titanium-alloy, uncemented femoral component in primary total hip arthroplasty. J Bone Joint Surg Am. 2004;86:92–97. [DOI] [PubMed]
- 35.Morrey BF. Instability after total hip arthroplasty. Orthop Clin North Am. 1992;23:237–248. [PubMed]
- 36.Nadaud MC, Griffin WL, Fehring TK, Mason JB, Tabor OB Jr, Odum S, Nussman DS. Cementless revision total hip arthroplasty without allograft in severe proximal femoral defects. J Arthroplasty. 2005;20:738–744. [DOI] [PubMed]
- 37.Paprosky WG, Greidanus NV, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop Relat Res. 1999;369:230–234. [DOI] [PubMed]
- 38.Park YS, Moon YW, Lim SJ. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. JArthroplasty. 2007;22:993–999. [DOI] [PubMed]
- 39.Parvizi J, Sullivan T, Duffy G, Cabanela ME. Fifteen-year clinical survivorship of Harris-Galante total hip arthroplasty. J Arthroplasty. 2004;19:672–677. [DOI] [PubMed]
- 40.Peters CL, Rivero DP, Kull LR, Jacobs JJ, Rosenberg AG, Galante JO. Revision total hip arthroplasty without cement: subsidence of proximally porous-coated femoral components. J Bone Joint Surg Am. 1995;77:1217–1226. [DOI] [PubMed]
- 41.Pieringer H, Auersperg V, Bohler N. Reconstruction of severe acetabular bone-deficiency: the Burch-Schneider antiprotrusio cage in primary and revision total hip arthroplasty. J Arthroplasty. 2006;21:489–496. [DOI] [PubMed]
- 42.Raut VV, Siney PD, Wroblewski BM. Cemented revision for aseptic acetabular loosening A review of 387 hips. J Bone Joint Surg Br. 1995;77:357–361. [PubMed]
- 43.Retpen JB, Varmarken JE, Jensen JS. Survivorship analysis of failure pattern after revision total hip arthroplasty. J Arthroplasty. 1989;4:311–317. [DOI] [PubMed]
- 44.Robinson AH, Palmer CR, Villar RN. Is revision as good as primary hip replacement? A comparison of quality of life. J Bone Joint Surg Br. 1999;81:42–45. [DOI] [PubMed]
- 45.Saleh KJ, Celebrezze M, Kassim R, Dykes DC, Gioe TJ, Callaghan JJ, Salvati EA. Functional outcome after revision hip arthroplasty: a metaanalysis. Clin Orthop Relat Res 2003;416:254–264. [DOI] [PubMed]
- 46.Schreurs BW, Arts JJ, Verdonschot N, Buma P, Slooff TJ, Gardeniers JW. Femoral component revision with use of impaction bone-grafting and a cemented polished stem Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 2):259–274. [DOI] [PubMed]
- 47.Sotereanos N, Sewecke J, Raukar GJ, DeMeo PJ, Bargiotas K, Wohlrab D. Revision total hip arthroplasty with a custom cementless stem with distal cross-locking screws. Early results in femora with large proximal segmental deficiencies. J Bone Joint Surg Am. 2006;88:1079–1084. [DOI] [PubMed]
- 48.Sporer SM, O’Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction. Average ten-year follow-up. J Bone Joint Surg Am. 2005;87:760–765. [DOI] [PubMed]
- 49.Stromberg CN, Herberts P. A multicenter 10-year study of cemented revision total hip arthroplasty in patients younger than 55 years old. A follow-up report. J Arthroplasty. 1994;9:595–601. [DOI] [PubMed]
- 50.Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty. J Arthroplasty. 2005;20:1002–1009. [DOI] [PubMed]
- 51.Weeden SH, Paprosky WG. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17 (Suppl 1):134–137. [DOI] [PubMed]
- 52.Weeden SH, Paprosky WG. Porous-ingrowth revision acetabular implants secured with peripheral screws. A minimum twelve-year follow-up. J Bone Joint Surg Am. 2006;88:1266–1271. [DOI] [PubMed]
- 53.Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001;83:1352–1357. [DOI] [PubMed]
- 54.White RE Jr, Forness TJ, Allman JK, Junick DW. Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop Relat Res. 2001;393:163–167. [DOI] [PubMed]