Abstract
Background:
Because dietary fat has been postulated to affect obesity and estrogen levels, two important risk factors for endometrial cancer, its association with this disease has received some attention. We summarize here the current evidence for several dietary lipids.
Methods:
Searches were conducted to identify peer-reviewed manuscripts up to December 2006. Two cohort studies and nine case-control studies were included in meta-analyses.
Results:
Random-effects summary estimates for case-control studies were 1.24 (95% CI: 1.10, 1.41) per 10 percent kcal from total fat and 1.28 (95% CI: 1.12, 1.47) per 10 g/1000 kcal of saturated fat. The only cohort study evaluating total fat and saturated fat did not find an association. We estimated a 35% increased risk (95% CI: 0.96, 1.90) per 150 mg/1000 kcal of cholesterol intake, based on six case-control studies. For animal fat (per 10 g/1000 kcal) the summary estimates were 0.78 (95% CI: 0.63, 0.96) and 1.34 (95% CI: 1.06, 1.69) for two cohort and four case-control studies, respectively.
Conclusions:
Case-control data suggest an increased risk for total, saturated, and animal fat. However, the limited available cohort data do not support these associations. Additional data, particularly from prospective studies, are needed before conclusions can be drawn.
Keywords: endometrial carcinoma, diet, fat, saturated fat, cholesterol, meta-analysis, systematic literature review
INTRODUCTION
Endometrial cancer is the most common female gynecological cancer in the United States [1]. Because obesity and unopposed estrogens are strong risk factors for endometrial cancer [2] and fat intake has been postulated to affect both risk factors [3-5], its role on the etiology of this disease has received some attention. The role of dietary fat and cholesterol on endometrial cancer risk was reviewed in the 1997 WCRF/AICR Report on Food, Nutrition, and the Prevention of Cancer [6]. The evidence for an increased endometrial cancer risk was deemed “possible” for saturated/animal fat and “insufficient” for total fat and cholesterol.
In support of the Second WCRF/AICR Report on Food, Nutrition, and the Prevention of Cancer, we conducted a systematic and comprehensive literature review of diet, nutrition, physical activity and endometrial cancer [7]. This second report, to be published November 2007, enhances and updates the previous 1997 review [6]. The objective of this manuscript is to summarize the scientific literature examining the role of dietary lipids on endometrial cancer risk and present the current evidence of an association. To our knowledge, this is the first systematic literature review and meta-analysis on this topic. This comprehensive review includes dose-response meta-analyses and evaluation of the role of total fat, fat subtypes, and cholesterol (as nutrients) on endometrial cancer risk. We do not include here analyses of foods or food groups high in fat.
METHODS
Our general methods followed the WCRF Specification Manual for systematic literature reviews, available online at www.wcrf.org. The methods used in this manuscript diverge from the WCRF protocol in that we followed our own criteria for inclusion of studies, as well as our own methods for data tabulation and analysis and for interpretation of the evidence. While WCRF required the inclusion of all studies regardless of quality, this systematic review and meta-analysis was limited to case-control and cohort studies. Randomized trials would have been included, but none were found. Ecological and cross-sectional studies were excluded. For the purpose of this manuscript we conducted additional analyses, such as sensitivity analyses repeating analyses after excluding studies that did not meet certain a priori criteria (i.e., population-based studies with more than 200 cases, known hysterectomy status among controls, and adjustment for total energy intake and body mass). Furthermore, interpretation of the evidence may not represent the views of WCRF and may differ from those in the upcoming WCRF report summarizing evidence related to food, nutrition, physical activity, and cancer risk.
Search strategy
Searches were conducted in July 2003, October 2004, and December 2005. Databases included Medline, ISI Web, Embase, Biosis, Ingenta, CINAHL, Science Direct, LILACS, Pascal, ExtraMed, and Allied CompMEd. Results from the 2003 searches indicated that most citations were found in Medline and, therefore, some of the databases that did not produce any new results were not used in subsequent searches. These searches were complemented with manual searches of bibliographies in published papers. Translations were provided by WCRF when necessary. For this manuscript we also monitored the literature using PubMed Alerts for all new papers on endometrial cancer from January through December 2006.
Exposure terms for PubMed were provided by WCRF and can be found in the Specification Manual and in the Appendix of another manuscript (Bandera et al. Consumption of animal foods and endometrial cancer risk: A systematic literature review and meta-analysis, submitted). General terms included diet[tiab] OR diets[tiab] OR dietetic[tiab] OR dietary[tiab] OR eating[tiab] OR intake[tiab] OR nutrient*[tiab] OR nutrition[tiab] OR vegetarian*[tiab] OR vegan*[tiab] OR “Seventh Day Adventist”[tiab] OR macrobiotic[tiab] OR food and beverages[MeSH Terms]. Specifically for dietary fats, terms included fat[tiab] OR fats[tiab] OR fatty[tiab] OR lipid*[tiab] OR linoleic acid*[tiab] OR sterols[tiab] OR stanols[tiab] OR cholesterol[tiab].
Following WCRF instructions, our searches included endometrial hyperplasia as this includes precancerous lesions. However, we only found a few papers evaluating the role of diet and nutrition on endometrial hyperplasia and none of them evaluated dietary fats. Outcomes terms included: (1): endometrial neoplasm [MeSH]; (2): malign* [tiab] OR cancer*[tiab] OR carcinoma*[tiab] OR tumor*[tiab] OR tumour*[tiab]; (3): endometr* [tiab] OR corpus uteri [tiab] OR uterine [tiab]; (4): #2 AND #3; (5): #3 AND hyperplasia [tiab].
Manuscript selection and data extraction
Overall search results and manuscript selection have been described elsewhere [8]. In brief, citations identified from these searches were reviewed independently by two of us (LHK, EVB) for relevance. Of the 285 papers identified evaluating some aspect of nutrition, diet, physical activity and endometrial cancer, 28 mentioned dietary fats; all but one of them [9] were written in English. Through monitoring the endometrial cancer literature in 2006 using PubMed Alerts nine additional papers were identified that evaluated nutrition, diet, or physical activity and endometrial cancer risk; but none of them evaluated fat intake.
In addition to one animal study [10] and four ecologic studies [11-14], three manuscripts were excluded for presenting data for foods or food groups only [15-17]. Three additional manuscripts were excluded for not presenting risk estimates [9, 18, 19]. We also excluded three publications from the same case-control study [20-22], as these included a subset of the study population in the manuscript by Potischman et al. [23]. One additional study [24] was excluded for having the same dietary data as in Littman et al., 2001 [25].
Excluding these 15 manuscripts left a total of 13 manuscripts [23, 25-36], two of them representing the same study by Goodman et al. [29, 30]. However, the two papers contributed data to analyses as one presents odds ratios and confidence intervals with more precision [30], while the other presents more variables and analyses [29]. Therefore, either of these papers (but not both) may contribute data to a given meta-analysis.
Data were extracted by trained research personnel on study characteristics and results using an Access® program developed by Leeds University under WCRF sponsorship. Each entry was reviewed by at least one of us.
Assessment of study quality and sensitivity analyses
In our review, we decided not to grade individual papers according to a quality score for two reasons: 1) there is not a widely-accepted tool for quality assessment of epidemiologic studies, and 2) we had few papers evaluating separately each exposure, thus limiting ability to conduct sensitivity analyses. Instead, we decided to present all the evidence from the several case-control studies, and then repeated certain analyses excluding studies that did not meet certain a priori quality criteria. The a priori quality criteria were: a) population-based studies as the appropriateness of hospital controls in diet and cancer studies is controversial; b) sample size of at least 200 cases for more optimal statistical power; c) exclusion of hysterectomies from the control group; and d) adjustment for important confounders such as total energy and body mass. In the forest plots, studies excluded are marked and the specific reasons for exclusion are indicated in the footnotes.
Statistical analysis
We followed WCRF criteria to decide when to conduct meta-analyses. For a given exposure, meta-analyses were conducted if there were at least two randomized clinical trials, at least two cohort studies, and/or at least five case-control studies evaluating that exposure. Meta-analyses were conducted separately by study design. Because only a few studies evaluated each dietary fat variable, we had limited power to assess publication bias through funnel plots, or to conduct sensitivity analyses and meta-regression.
For total fat, saturated fat, animal fat, vegetable fat, and cholesterol there were a sufficient number of studies to conduct meta-analyses. Most of the studies categorized relevant exposures into four or five groups, and reported odds ratios for each category relative to the lowest exposure category. A few studies reported parameter estimates from a continuous logistic regression analysis. To compare these studies, it was necessary to convert the grouped results into an estimate of what would have resulted from continuous logistic regression analysis, had those been reported.
Results were first transformed into a common scale. For example, analyses related to dietary fat intake were reported in units measured as g/day, kcal/day, g/1,000 kcal, or percent of energy. Similarly, for dietary cholesterol, analyses may be based on mg/day or mg/1,000 kcal. Average daily kcal intake from study to study varied considerably, and much of this variance is probably attributable to dietary assessment methods rather than to true differences in food intake. For example, median daily energy intake in the study by Potischman et al. [23] was 1,248 kcal, whereas in the study by McCann et al. [32], it was 2,102 kcal. Both of these studies were conducted in the US, making it unlikely that cultural or lifestyle differences were a major contributor to these differences in reported intake. Thus, for dose-response meta-analyses, we elected to convert reported intake levels to nutrient density measures expressed as either percent of energy from fat (for total fat intake) or g/1,000 kcal (for saturated fat and animal fat intake). For dietary cholesterol, we converted study-specific cutpoints that were provided as mg/day into mg/1,000 kcal before pooling. In order to convert reported category intake levels or medians into nutrient density measures, it was necessary to have a reported value for median (or mean) kcal/day intake for the study population; this was available in most studies.
For studies not reporting confidence intervals, these were estimated based on the number of cases and controls in each category of exposure [37]. While this results in an estimate of the variance of the crude odds ratio, in general, this variance is similar to that after taking covariates into account.
For studies reporting only categorical analyses, an estimate of mean intake for each category was computed following the methodology developed by Chêne and Thompson [38]. The iterative method described in Greenland and Longnecker [39] was used to estimate a single logistic regression parameter per study. This method imputes expected numbers of cases and controls (or cases for a prospective study) and computes the logistic regression slope parameter (which may be interpreted as the log odds ratio) and standard error. Finally, we estimated fixed effects and random effects pooled logistic regression coefficients across studies. We used the random effects models in forest plots and for interpretation of the evidence, since it combines “within study” variance and “between study” variance for computing weights. The Chêne and Thompson [38] and Greenland and Longnecker [39] algorithms described above were implemented in the statistical language R (R Development Core Team, 2003).
RESULTS
This systematic literature review included 13 manuscripts from three cohort studies [26, 27, 36] and 9 case-control studies [23, 25, 28, 29, 31-35] evaluating dietary fats. Selected characteristics of these studies and exposures of interest evaluated are listed in Table 1. As shown in the table, these studies were conducted in several countries and varied considerably in the quality of dietary assessment, as well as in the evaluation of dietary fats and methods of dealing with the strong confounding effect of total energy intake. The case-control study by Salazar-Martinez et al. [33] was not included in dose-response meta-analyses because it did not present an estimate of total energy intake and, therefore, transformation of exposure estimates into nutrient density measures was not possible.
Table 1.
Characteristics of observational studies evaluating dietary fats and endometrial cancer risk
| Reference | Country | Cases/ controls or cohort size |
Age | Dietary assessment |
Method of adjustment for total energy intake [56] |
Time frame* | Dietary fats evaluated |
|---|---|---|---|---|---|---|---|
| Cohort studies | |||||||
| Furberg et al., 2003 [27]† |
Norway | 130/24,460 | 20 - 49 | FFQ (64 items) | Not adjusted for total energy |
Total fat intake | |
| Zheng et al., 1995 [36] |
United States | 216/ 23,070 |
55-69 | FFQ (127 items) | Standard multivariate method |
Current intake | Total fat from animal sources, total fat from plant sources |
| Jain et al., 2000 [26] |
Norway | 221/3697 | 40 - 59 | FFQ (86 items) | Residuals method | One month prior |
Total fat, saturated fat, oleic acid, linoleic acid, animal fat, vegetable fat |
| Population-based case-control studies | |||||||
| Shu et al., 1993 [28] |
China | 268/268 | 18-74 | FFQ (63 items) | Not adjusted for total energy intake |
10 years | Calories from fat, animal fat, plant fat |
| Potischman et al., 1993 [23] |
United States | 399/296 | 20-74 | FFQ (Block, 60 items) |
Multivariate nutrient density method and modified energy partition method (fat calories adjusted for carbohydrate calories) |
“past few years” |
Saturated fat, oleic acid, linoleic acid, cholesterol, fat calories, % calories from fat |
| Goodman et al., 1997 [29, 30] |
United States | 332/511 | 18-84 | Dietary history (250 items) |
Standard multivariate method (similar results using the residual method) |
1 year | Fat calories, % calories from fat, total fat, animal fat, plant fat, cholesterol, saturated fat, unsaturated fat, monounsaturated fat, polyunsaturated fat |
| Jain et al., 2000 [31] |
Canada | 552/562 | 30-79 | Dietary history (n Items ?) |
Residuals method | 1 year | Total fat, saturated fat, monounsaturated fat, linoleic acid, linolenic acid, animal fat |
| McCann et al., 2000 [32] |
United States | 232/639 | 40-85 | FFQ (172 items) | Unspecified | 2 years | Total fat, saturated fat, monounsaturated fat, polyunsaturated fat, cholesterol |
| Littman et al., 2001 [25] |
United States | 679/944 | 45-74 | FFQ (modified Block, 98 items) |
Multivariate nutrient density method |
5 years | Percent energy from fat, saturated fat, linoleic acid, oleic acid, cholesterol |
| Hospital-based case-control studies | |||||||
| Tzonou et al, 1996 [34]† |
Greece | 145/298 | FFQ (115 items) | “in marginal quartiles, continuously” |
1 year | Total fat, saturated fat, monounsaturated fat, polyunsaturated fat, cholesterol | |
| Barbone et al., 1993 [35] |
United States | 103/236 | FFQ (Willett, 116 items) |
Residuals method | 1 year | Animal fat, vegetable fat, cholesterol | |
| Salazar-Martinez et al., 2005 [33] |
Mexico | 85/629 | 18-81 | FFQ (116 items) | Residuals method and standard multivariate method |
1 year | Total fat, saturated fat, monounsaturated fat, polyunsaturated fat, animal fat, vegetable fat, cholesterol |
Abbreviations: FFQ, food frequency questionnaire; ?, unspecified
Time frame for dietary assessment.
Whether hysterectomies were excluded unspecified
Total fat
As shown in Table 2, case-control studies in general supported an increased risk with increased fat intake, with odds ratios ranging from 1.2 to 3.9, although most confidence intervals included one. In contrast, cohort data showed little evidence of an association.
Table 2.
Studies evaluating total fat intake and endometrial cancer risk
| Reference | Country | Age | Cases/ Controls or total cohort |
Exposure evaluated |
Contrast | RR/O R |
95% confidence interval |
P for trend |
Covariates Considered* |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | E | S | H | R | |||||||||
| Cohort studies | ||||||||||||||
| Jain et al., 2000 [26]† |
Canada | 40-59 | 221/3,697 | Total fat, g/day | >102.8 vs. <85.9 g | 0.84 | 0.58, 1.23 | 1 | 1 | 1 | 1 | 1 | 2 | |
| Furberg et al., 2003 [27] |
Norway | 130/24,460 | Total fat, g/day | Per 19.4 g | 0.99 | 0.82, 1.2 | 1 | |||||||
| Population-based case-control studies | ||||||||||||||
| Potischman et al., 1993 [23] |
United States | 20-74 | 399/296 | Fat calories, kcal/day |
>634 vs. <344 kcal | 1.5 | 0.8, 2.7 | 1 | 1 | ‡ | 1 | 1 | 1 | |
| % Calories from fat | >43.4% vs. <32.2% | 1.5 | 0.9, 2.4 | 1 | 1 | 1 | 1 | 1 | 1 | |||||
| Shu et al., 1993 [28] |
China | 18-74 | 268/268 | Calories from fat | ≥659.32 vs. ≤475.20 kcal | 3.9 | 2.2, 6.8 | <0.01 | 1 | 1 | 1 | |||
| Goodman et al., 1997 [30]§ |
United States | 18-84 | 332/511 | Fat calories | ≥847 vs. <420 kcal | 1.60 | 0.97, 2.61 | 0.04 | (1) | 1 | 1 | 1 | ||
| Fat, g/day | >94.1 vs. <46.7 g | 1.68 | 0.77, 3.69 | 0.17 | (1) | 1 | 1 | 1 | 1 | |||||
| Goodman et al., 1997 [29]§ |
United States | 18-84 | 332/511 | % Calories from fat |
>38.1 vs. <27.9% | 1.6 | 0.11 | (1) | 1 | 1 | 1 | 1 | ||
| Jain et al., 2000 [31] |
Canada | 30-79 | 552/562 | Total fat, g/day | >66.3 vs. <46 g | 1.21 | 0.84, 1.83 | 0.65 | 1 | 1 | 1 | 1 | 1 | 2 |
| Per 20 g | 1.12 | 0.95, 1.33 | 1 | 1 | 1 | 1 | 1 | 2 | ||||||
| McCann et al., 2000 [32] |
United States | 40-85 | 232/639 | Total fat, g/day | >102 vs. ≤60 g | 1.6 | 0.7, 3.4 | 0.75 | 1 | 1 | 1 | 1 | 1 | 3 |
| Littman et al., 2001 [25] |
United States | 45-74 | 679/944 | % Calories from fat |
>45.1% vs. <30.8% | 1.7 | 1.2, 2.4 | 0.006 | 1 | 1 | 1 | 1 | 1 | |
| Hospital-based case-control studies | ||||||||||||||
| Salazar-Martinez et al., 2005 [33] |
Mexico | 18-81 | 85/629 | Total fat, g/day | >59 vs. <37 g | 1.45 | 0.61, 3.44 | 0.54 | 1 | 1 | 1 | 1 | ||
Adjustment columns: A = Age; B = BMI/weight; E = Total Energy; S = Smoking; H = HRT/ERT use; R = Reproductive factors; (1): matched on age. Numbers in columns refer to the number of covariates adjusted for under that grouping.
Case-cohort design.
Adjusted for carbohydrate calories.
Same case-control study.
Abbreviations: OR: odds ratio, RR: relative risk.
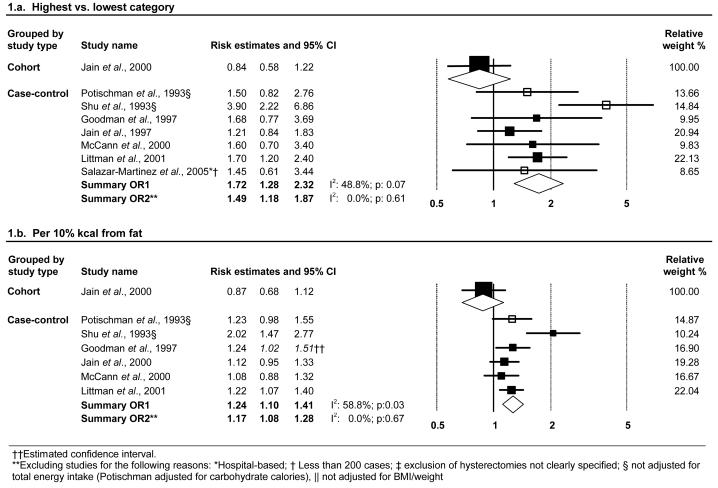
Meta-analysis
The two cohort studies [26, 27] and seven independent case-control studies [23, 25, 28-33] evaluating total fat, listed in Table 2, were considered for inclusion in meta-analyses. The analysis by Furberg et al. [27] was excluded because analyses were only adjusted for age. Therefore, we were unable to conduct meta-analysis with cohort data. The random-effects summary estimate, shown in Figure 1.a, for the seven case-control studies was 1.72 (95% CI: 1.28, 2.32), with moderate heterogeneity (I2: 48.8%, p: 0.07). After excluding studies that did not meet our quality criteria the estimate was attenuated but there was still a 49 percent increased risk for the highest category of consumption compared to the lowest and no heterogeneity among studies. In Figure 1.b, estimated ORs for each study for an increment of 10 percent kcal from fat and the summary estimate are shown. Based on the random-effects model, we estimated a 24 percent increased risk per 10 percent kcal from fat increment. Although this estimate was attenuated after excluding two studies [23, 28] that did not adjust for total energy intake, there was still suggestion of an association and no evidence of heterogeneity (Figure 1.b.). However, the only cohort study examining total fat was inconsistent with this association, with a derived RR of 0.87 (95% CI: 0.68-1.12) per 10 percent kcal from fat.
Figure 1.
Random-effects meta-analysis of total fat intake and endometrial cancer risk.
Saturated fat
Studies reporting on saturated fat intake and endometrial cancer risk are listed in Table 3. Four [23, 25, 29, 31] of the five population-based case-control studies [23, 25, 29, 31, 32] suggested elevated risk associated with higher saturated fat intake, while two small hospital-based case-control studies [33, 34] did not support such association. We found only one cohort study reporting on saturated fat intake, the Canadian National Breast Screening (CNBS) Study [26], which suggested an inverse association (RR=0.7), although the confidence interval included one (Table 3).
Table 3.
Studies evaluating saturated fat intake and endometrial cancer risk
| Reference | Country | Age | Cases/ Controls or total cohort |
Exposure evaluated |
Contrast | RR/OR | 95% confidence interval |
P for trend |
Covariates Considered* |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | E | S | H | R | |||||||||
| Cohort studies | ||||||||||||||
| Jain et al., 2000 [26]† |
Canada | 40-59 | 221/3,697 | Saturated fat, g/day | Q4 vs. Q1 | 0.7 | 0.47, 1.04 | 1 | 1 | 1 | 1 | 1 | 2 | |
| Population-based case-control studies | ||||||||||||||
| Potischman et al., 1993 [23] |
United States | 20-74 | 399/296 | Saturated fat, g/day | >25 vs. <12 g | 2.1 | 1.2, 3.7 | 1 | 1 | ‡ | 1 | 1 | 1 | |
| Goodman et al., 1997 [29] |
United States | 18-84 | 332/511 | Saturated fat, g/day | >27.2 vs. <12.5 g | 2.2 | 0.13 | (1) | 1 | 1 | 1 | 1 | ||
| Jain et al., 2000 [31] |
Canada | 30-79 | 552/562 | Saturated fat, g/day | Q4 vs. Q1 | 1.22 | 0.85, 1.75 | 0.57 | 1 | 1 | 1 | 1 | 1 | 2 |
| Per 12 g. | 1.19 | 0.96, 1.46 | 1 | 1 | 1 | 1 | 1 | 2 | ||||||
| McCann et al., 2000 [32] |
United States | 40-85 | 232/639 | Saturated fat, g/day | >37 vs. ≤21 g | 1.1 | 0.5, 2.4 | 0.75 | 1 | 1 | 1 | 1 | 1 | 3 |
| Littman et al., 2001 [25] |
United States | 45-74 | 679/944 | Saturated fat, g/day | >33.4 vs. <13.3 g | 1.6 | 1.1, 2.3 | 0.001 | 1 | 1 | 1 | 1 | 1 | |
| Hospital-based case-control studies | ||||||||||||||
| Tzonou et al., 1996 [34] |
Greece | 145/298 | Saturated fat, g/day | Per 8 g | 0.94 | 0.64, 1.38 | 1 | 1 | 1 | 1 | 1 | 5 | ||
| Salazar-Martinez et al., 2005 [33] |
Mexico | 18-81 | 85/629 | Saturated fat, g/day | >25 vs. <17 g | 0.67 | 0.29, 1.53 | 0.08 | 1 | 1 | 1 | 1 | ||
Adjustment columns: A = Age; B = BMI/weight; E = Total Energy; S = Smoking; H = HRT/ERT use; R = Reproductive factors; (1): matched on age. Numbers in columns refer to the number of covariates adjusted for under that grouping.
Case-cohort design.
Adjusted for carbohydrate calories.
Abbreviations: OR: odds ratio, RR: relative risk; Q: quantile.
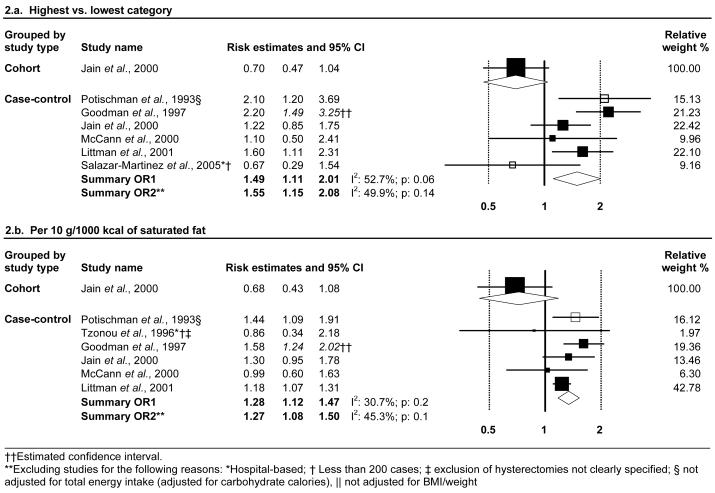
Meta-analysis
A meta-analysis comparing high v. low intake categories, shown in Figure 2.a, suggested a 50 percent increased risk associated with higher saturated fat intake, based on case-control data. The two studies (cohort and case-control) by Jain et al. [26, 31] to report on saturated fat-endometrial cancer associations did not present cutpoints for the quartile-based analyses. To allow inclusion of these studies in dose-response meta-analyses, we contacted Dr. Meera Jain and she provided these values for her two studies (Personal communication, March 17, 2004). In dose-response meta-analyses of the case-control data, we estimated a 28 percent increased risk per 10 g/1000 kcal of saturated fat intake, with little heterogeneity among studies (Figure 2.b). Once again, the only cohort study evaluating this association [26] was inconsistent with these findings, suggesting instead a decreased risk associated with higher saturated fat intake.
Figure 2.
Random-effects meta-analysis of saturated fat intake and endometrial cancer risk.
Monounsaturated fat
As shown in Table 4, several studies have evaluated monounsaturated fat intake and endometrial cancer, but results are inconsistent. The cohort study by Jain et al. [26] examined oleic acid intake, the predominant monounsaturated fatty acid in most diets, and reported a non-significant weak inverse association. Five case-control studies [29, 31-34] reported on the association of monounsaturated fat intake and risk of endometrial cancer and an additional two reported on oleic acid intake [23, 25]. ORs ranged from 0.76 to 2.5 across these studies. Given the inconsistent data, meta-analyses were not conducted.
Table 4.
Studies evaluating monounsaturated fat intake and endometrial cancer risk
| Reference | Country | Age | Cases/ Controls or total cohort |
Exposure evaluated |
Contrast | RR/OR | 95% confidence interval |
P for trend |
Covariates Considered* |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | E | S | H | R | |||||||||
| Cohort studies | ||||||||||||||
| Jain et al., 2000 [26]† |
Canada | 40-59 | 221/3,697 | Oleic acid, g/day | >39.2 vs. <32.5 g | 0.79 | 0.54, 1.17 | 1 | 1 | 1 | 1 | 1 | 2 | |
| Population-based case-control studies | ||||||||||||||
| Goodman et al., 1997 [29] |
United States | 18-84 | 332/511 | Monounsaturated fat, g/day |
>32.5 vs. <15.7 g | 2.5 | 0.03 | (1) | 1 | 1 | 1 | 1 | ||
| Jain et al., 2000 [31] |
Canada | 30-79 | 552/562 | Monounsaturated fat, g/day |
>26.4 vs. <17.4 g | 1.08 | 0.76, 1.53 | 0.63 | 1 | 1 | 1 | 1 | 1 | 2 |
| McCann et al., 2000 [32] |
United States | 40-85 | 232/639 | Monounsaturated fat, g/day |
>28 vs. <16 g | 0.9 | 0.4, 1.8 | 0.08 | 1 | 1 | 1 | 1 | 1 | 3 |
| Potischman et al., 1993 [23] |
United States | 20-74 | 399/296 | Oleic acid, g/day | >25 vs. <13 g | 2.2 | 1.2, 4 | 1 | 1 | ‡ | 1 | 1 | 1 | |
| Littman et al., 2001 [25] |
United States | 45-74 | 679/944 | Oleic acid, g//1000 kcal/day |
>35.9 vs. <14.4 g | 1.4 | 1, 2 | 0.01 | 1 | 1 | 1 | 1 | 1 | |
| Hospital-based case-control studies | ||||||||||||||
| Tzonou et al., 1996 [34] |
Greece | 145/298 | Monounsaturated fat, g/day |
Per 15 g | 0.76 | 0.56, 1.03 | 1 | 1 | 1 | 1 | 1 | 5 | ||
| Salazar-Martinez et al., 2005 [33] |
Mexico | 18-81 | 85/629 | Monounsaturated fat, g/day |
>19 vs. <12 g | 0.98 | 0.41, 2.43 | 0.79 | 1 | 1 | 1 | 1 | ||
Adjustment columns: A = Age; B = BMI/weight; E = Total Energy; S = Smoking; H = HRT/ERT use; R = Reproductive factors; (1): matched on age. Numbers in columns refer to the number of covariates adjusted for under that grouping.
Case-cohort design.
Adjusted for carbohydrate calories.
Abbreviations: OR: odds ratio, RR: relative risk.
Polyunsaturated fatty acid
The few studies evaluating polyunsaturated fat intake and endometrial cancer risk are listed in Table 5. Four case-control studies [29, 32-34] reported on polyunsaturated fat intake, with mixed findings, and three additional population-based case-control studies [23, 25, 31] reported on linoleic acid intake with similarly inconsistent results. One of these three studies also reported on linolenic acid intake, and found no association [31]. Given the limited and inconsistent data, meta-analyses were not conducted.
Table 5.
Studies evaluating polyunsaturated fatty acids intake and endometrial cancer risk
| Reference | Country | Age | Cases/ Controls or total cohort |
Exposure evaluated |
Contrast | RR/OR | 95% confidence interval |
P for trend |
Covariates Considered* |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | E | S | H | R | |||||||||
| Cohort studies | ||||||||||||||
| Jain et al., 2000 [26]† |
Canada | 40-59 | 221/3,697 | Linoleic acid, g/day | >14 vs. <9.2 g | 1.11 | 0.77, 1.61 | 1 | 1 | 1 | 1 | 1 | 2 | |
| Population-based case-control studies | ||||||||||||||
| Goodman et al., 1997 [29] |
United States | 18-84 | 332/511 | Polyunsaturated fat, g/day |
>27 vs. <13.3 g | 1.5 | 0.17 | (1) | 1 | 1 | 1 | 1 | ||
| McCann et al., 2000 [32] |
United States | 40-85 | 232/639 | Polyunsaturated fat, g/day |
>15 vs. ≤8 g | 1 | 0.5, 1.8 | 0.58 | 1 | 1 | 1 | 1 | 1 | 3 |
| Jain et al., 2000 [31] |
Canada | 30-79 | 552/562 | Linolenic acid, g/day | >1.6 vs. ≤0.8 g | 1.02 | 0.72, 1.46 | 0.99 | 1 | 1 | 1 | 1 | 1 | 2 |
| Linoleic acid, g/day | >9 vs. <5.9 g | 1.14 | 0.81, 1.61 | 0.48 | 1 | 1 | 1 | 1 | 1 | 2 | ||||
| Potischman et al., 1993 [23] |
United States | 20-74 | 399/296 | Linoleic acid, g/day | >14 vs. <7 g | 1.6 | 0.9, 2.8 | 1 | 1 | ‡ | 1 | 1 | 1 | |
| Littman et al., 2001 [25] |
United States | 45-74 | 679/944 | Linoleic acid, g//1000 kcal/day |
>18.9 vs. <6.9 g | 1 | 0.74, 1.5 | 0.94 | 1 | 1 | 1 | 1 | 1 | |
| Hospital-based case-control studies | ||||||||||||||
| Tzonou et al., 1996 [34] |
Greece | 145/298 | Polyunsaturated fat, g/day |
Per 8 g | 1.02 | 0.8, 1.3 | 1 | 1 | 1 | 1 | 1 | 5 | ||
| Salazar-Martinez et al., 2005 [33] |
Mexico | 18-81 | 85/629 | Polyunsaturated fat, g/day |
>5.8 vs. <4.2 g | 2.23 | 0.98, 5.05 | 0.34 | 1 | 1 | 1 | 1 | ||
Adjustment columns: A = Age; B = BMI/weight; E = Total Energy; S = Smoking; H = HRT/ERT use; R = Reproductive factors; (1): matched on age. Numbers in columns refer to the number of covariates adjusted for under that grouping.
Case-cohort design.
Adjusted for carbohydrate calories.
Abbreviations: OR: odds ratio, RR: relative risk.
Cholesterol
Studies evaluating dietary cholesterol are listed in Table 6. Of the seven case-control studies, two suggested an inverse association comparing high with low intake [32, 33], one was essentially null [34], while the others [23, 25, 29, 35] reported ORs ranging from 1.30 to 2.2.
Table 6.
Studies evaluating cholesterol intake and endometrial cancer risk
| Reference | Country | Age | Cases/ Controls or total cohort |
Exposure evaluated |
Contrast | RR/ OR |
95% confidence interval |
P for trend |
Covariates Considered* |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | E | S | H | R | |||||||||
| Population-based case-control studies | ||||||||||||||
| Potischman et al., 1993 [23] |
United States | 20-74 | 399/296 | Cholesterol, mg/day | >245 vs. <123 mg | 2 | 1.2, 3.3 | 1 | 1 | † | 1 | 1 | 1 | |
| Goodman et al., 1997 [29] |
United States | 18-84 | 332/511 | Cholesterol, mg/day | >302 vs. <132 mg | 2.2 | 0.02 | (1) | 1 | 1 | 1 | 1 | ||
| McCann et al., 2000 [32] |
United States | 40-85 | 232/639 | Cholesterol, mg/day | >427 vs. ≤239 mg | 0.7 | 0.4, 1.4 | 0.03 | 1 | 1 | 1 | 1 | 1 | 3 |
| Littman et al., 2001 [25] |
United States | 45-74 | 679/944 | Cholesterol, mg/day | >341.5 vs. <122.3 mg | 1.3 | 0.85, 2.1 | 0.15 | 1 | 1 | 1 | 1 | 1 | |
| Hospital-based case-control studies | ||||||||||||||
| Barbone et al., 1993 [35] |
United States | 102/203 | Cholesterol, mg/day | >293.6 vs. <218.9 mg | 1.6 | 0.8, 2.9 | 0.23 | 1 | 1 | 1 | 1 | 1 | 3 | |
| Tzonou et al., 1996 [34] |
Greece | 145/298 | Cholesterol, mg/day | Per 70 mg | 1.09 | 0.76, 1.57 | 1 | 1 | 1 | 1 | 1 | 5 | ||
| Salazar-Martinez et al., 2005 [33] |
Mexico | 18-81 | 85/629 | Cholesterol, mg/day | >186 vs. <126 mg | 0.81 | 0.37, 1.76 | 0.65 | 1 | 1 | 1 | 1 | ||
Adjustment columns: A = Age; B = BMI/weight; E = Total Energy; S = Smoking; H = HRT/ERT use; R = Reproductive factors; (1): matched on age. Numbers in columns refer to the number of covariates adjusted for under that grouping.
Adjusted for carbohydrate calories.
Abbreviations: OR: odds ratio, RR: relative risk.
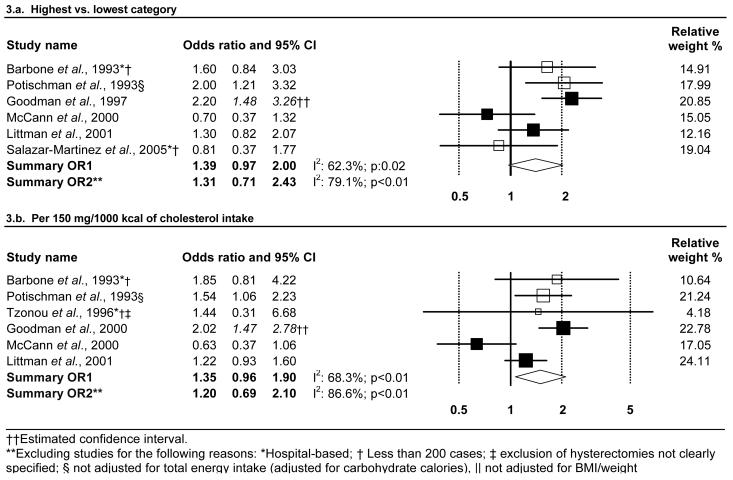
Meta-analysis
Both high vs. low and dose-response meta-analyses, shown in Figures 3.a and 3.b and based solely on case-control data, suggested elevated endometrial cancer risk associated with higher cholesterol intake. However, confidence intervals for the summary estimate include the null value and there was high and significant heterogeneity among studies.
Figure 3.
Random-effects meta-analysis of cholesterol intake and endometrial cancer risk.
Animal fat
Several studies, shown in Table 7, have evaluated the risk associated with animal and vegetable fat. Two cohort studies reported on animal fat intake with inconsistent results. One of these two studies, the CNBS Study [26], reported an inverse association of animal fat intake and risk of endometrial cancer, whereas the other study, the Iowa Women's Health Study [36], found no association.
Table 7.
Studies evaluating animal and vegetable fat intake and endometrial cancer risk
| Reference | Country | Age | Cases/ Controls or total cohort |
Exposure evaluated |
Contrast | RR/ OR |
95% confidence interval |
P for trend |
Covariates Considered* |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | E | S | H | R | |||||||||
| Cohort studies | ||||||||||||||
| Zheng et al., 1995 [36] | United States | 55-69 | 216/23,070 | Animal fat, g/day | >23.8 vs. <13.3 g | 1 | 0.5, 1.8 | 0.97 | 1 | 1 | 1 | 2 | ||
| Plant fat, g/day | >20.7 vs. <11.2 g | 0.9 | 0.5, 1.6 | 0.59 | 1 | 1 | 1 | 2 | ||||||
| Jain et al., 2000 [26]† | Canada | 40-59 | 221/3,697 | Animal fat, g/day | >75.6 vs. <56.4 g | 0.6 | 0.4, 0.9 | 1 | 1 | 1 | 1 | 1 | 2 | |
| Plant fat, g/day | >33.6 vs. <20.2 g | 1.32 | 0.9, 1.93 | 1 | 1 | 1 | 1 | 1 | 2 | |||||
| Population-based case-control studies | ||||||||||||||
| Shu et al., 1993 [28] | China | 18-74 | 268/268 | Animal fat, g/day | >29.18 vs. <11.96 g | 3.5 | 2, 6 | <0.01 | 1 | 1 | 1 | |||
| Plant fat, g/day | >45.44 vs. <34.37 g | 1.2 | 0.7, 1.9 | 0.80 | 1 | 1 | 1 | |||||||
| Goodman et al., 1997 [29] | United States | 18-84 | 332/511 | Animal fat, g/day | >40.9 vs. <16.9 g | 1.7 | 0.37 | (1) | 1 | 1 | 1 | 1 | ||
| Plant fat, g/day | >53.8 vs. <26.1 g | 1.7 | 0.09 | (1) | 1 | 1 | 1 | 1 | ||||||
| Jain et al., 2000 [31] | Canada | 30-79 | 552/562 | Animal fat, g/day | >44 vs. <22.1 g | 1.66 | 1.15, 2.4 | 0.03 | 1 | 1 | 1 | 1 | 1 | 2 |
| Per 22 g | 1.18 | 0.98, 1.41 | 1 | 1 | 1 | 1 | 1 | 2 | ||||||
| Hospital-based case-control studies | ||||||||||||||
| Barbone et al., 1993 [35] | United States | 102/203 | Animal fat, g/day | >35.3 vs. <26.7 g | 1.3 | 0.7, 2.6 | 0.76 | 1 | 1 | 1 | 1 | 1 | 3 | |
| Plant fat, g/day | >32.3 vs. <25.8 g | 0.6 | 0.3, 1.1 | 0.84 | 1 | 1 | 1 | 1 | 1 | 3 | ||||
| Salazar-Martinez et al., 2005 [33] |
Mexico | 18-81 | 85/629 | Animal fat, g/day | >47 vs. <28 g | 1.19 | 0.55, 2.58 | 0.69 | 1 | 1 | 1 | 1 | ||
| Plant fat, g/day | >14 vs. <7 g | 1.5 | 0.68, 3.32 | 0.39 | 1 | 1 | 1 | 1 | ||||||
Adjustment columns: A = Age; B = BMI/weight; E = Total Energy; S = Smoking; H = HRT/ERT use; R = Reproductive factors; (1): matched on age. Numbers in columns refer to the number of covariates adjusted for under that grouping.
Case-cohort design.
Abbreviations: OR: odds ratio, RR: relative risk.
Case-control studies have offered more consistent results. The five studies evaluating animal fat suggested an increased risk with higher animal fat intake. ORs ranged from 1.19 [33] to 3.5 [28]. The study reporting the highest OR did not adjust this association for energy intake [28].
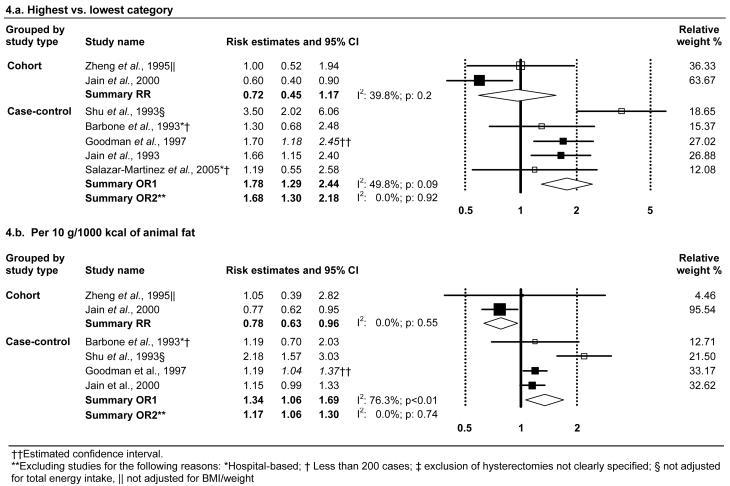
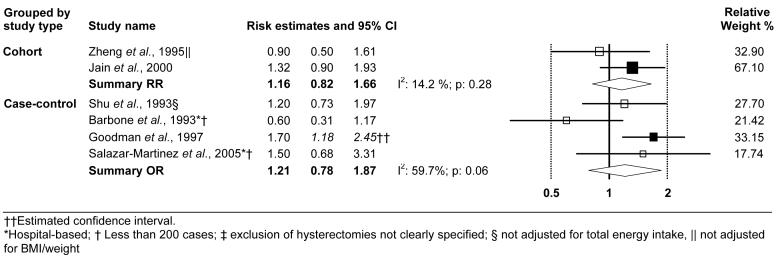
Meta-analysis
High vs. low meta-analysis indicated a strong relationship with animal fat based on case-control studies (Figure 4.a). After excluding two small hospital-based studies and another study that did not adjust for total energy intake, there was still a 68 percent increased risk associated with high animal intake and no evidence of heterogeneity. We also estimated a 17-34 percent increase in endometrial cancer risk per 10 g/1000 kcal of animal fat intake, based on case-control data (Figure 4.b). However, cohort data pointed to an inverse association with animal fat, but the confidence interval for the high vs. low summary estimates included the null value (Figures 4.a and 4.b). Dose-response analyses of the cohort data should be viewed with caution, as the paper by Zheng et al. [36], from the Iowa Women's Health Study, provides considerably lower intake estimates than the other cohort study [26]. We believe that there may have been an error, as the median intake in Q3 (of 5 quintiles) for animal fat and vegetable fat intakes are given as 18.1 g/day and 15.5 g/day, respectively. However, the mean total fat intake in this cohort, obtained from a different report from the same study [40], is about 68.7 g.
Figure 4.
Random-effects meta-analysis of animal fat and endometrial cancer risk.
Vegetable fat
Two cohort studies [26, 36] and four case-control studies [28, 29, 33, 35] reported on the relationship with vegetable fat, with conflicting results (Table 7). All confidence intervals included the null value.
Meta-analysis
Because of concerns regarding the cutpoints presented in the report by Zheng et al. (1995), mentioned earlier, and the inconsistent results across studies, dose-response meta-analyses were not conducted. High vs. low meta-analysis, shown in Figure 5, suggested an elevated risk but the confidence intervals around the summary estimates for both cohort and case-control studies included one. Although the current available data is very limited, it should be noted that the two studies that were not marked for having some quality issue, represented in the figure with a solid square, suggested an elevated risk.
Figure 5.
Random-effects meta-analysis of vegetable fat (highest vs. lowest category) and endometrial cancer risk.
DISCUSSION
This meta-analysis suggested an increased endometrial cancer risk associated with total fat, saturated fat, and animal fat intakes. However, these findings were based on a limited numbers of case-control studies and were not observed in the one or two cohort studies evaluating these associations. Case-control data suggested a 24 percent increased risk per 10 percent kcal from total fat, and a 29 percent increased risk per 10 g/1,000 kcal of intake for saturated fat. Similarly, results from case-control studies suggested a strong association for animal fat, whereas two cohort studies suggested an inverse association. Our meta-analysis of six case-control studies reporting on cholesterol also suggested a positive association, but the confidence interval included the null value.
In general, it is assumed in nutritional epidemiology that cohort studies provide better estimates of the association of dietary factors with risk of cancer and other chronic diseases. This is mainly because temporality of the association and potential differential recall bias are not in dispute. On the other hand, in the case of endometrial cancer, there is an important caveat that must be considered when weighing results from cohort vs. case-control studies. Specifically, women who have had a hysterectomy are at virtually no risk of developing endometrial cancer. Properly, two of the three cohort studies [26, 36] evaluating dietary lipids and endometrial cancer excluded women with a hysterectomy at baseline. Notably, the third [27] did not, an additional reason for exclusion of that study from consideration in meta-analysis. However, none of the three studies [26, 27, 36] updated hysterectomy status of their population during follow-up; ideally, women would be censored at the time of hysterectomy. If indications for hysterectomy are associated with fat intake, and fat intake is also associated with endometrial cancer risk (as suggested by the case-control studies), then failure to account for updated hysterectomy status would bias results toward the null, or may even result in an inverse association.
For breast cancer, a cancer site with a risk factor profile similar to that for endometrial cancer, it has also been noted that generally case-control studies have observed elevated risks with increasing dietary fat intake [41], whereas results from cohort studies have been null [42]. However, a meta-analysis published in 2003 [43] and including 31 case-control studies and 14 cohort studies found similar weak positive associations for dietary fat intake and breast cancer for case-control (summary estimate: 1.14; 95% CI: 0.99-1.32) and cohort studies (summary estimate: 1.11; 95% CI: 0.99-1.25).
Because of the limited number of studies evaluating these associations, we estimated confidence intervals when they were not reported so that we could include as many studies in the analyses as possible. In addition to the assumptions related to distribution of cases and controls, these calculations also assume that confounding factors have minimal impact on the variance. That is, the variance estimate derived from the distribution of cases and controls is based on “crude” distributions, and do not take intake account the influence of confounding variables. In the case of dietary fat intake (measured as g/day or kcal/day) as the exposure of interest and total energy intake (kcal/day) as a confounding variable, this may not be a reasonable assumption (e.g., see Willett et al.[44] for descriptions of differences in confidence limits according to energy adjustment method). For nutrient density measures, however, this is probably a reasonable assumption.
To our knowledge this is the first systematic literature review and meta-analysis of the role of fat intake on endometrial cancer risk. In the 1997 WCRF/AICR Report [6], based on a narrative (and not comprehensive) review of this association, saturated and animal fat intakes were deemed to “possibly” increase risk, while there was “insufficient” evidence for total fat and cholesterol. These conclusions were based on four case-control studies [23, 28, 29, 35], all included in our review, plus two hospital-based case-control studies [16, 45] which evaluated “added fats”. We excluded these two papers as our review was based on dietary lipids as nutrients. Furthermore, odds ratios in these latter two papers did not adjust for total energy intake.
The association of total fat intake and cancer risk is controversial and the role of different types of fat is not well understood [46-48]. Although the association with endometrial cancer has received relatively little attention, several lines of evidence support a possible association. A meta-analysis of dietary intervention studies to lower fat intake found effects on decreased serum estradiol levels [5]. Although this may not be due specifically to the fat content of the diet, these studies suggest that dietary patterns low in fat may favorably influence long-term exposure to high levels of endogenous estrogens. These results are congruent with earlier observations of lower plasma estradiol levels and increased fecal excretion of estrogens in vegetarians than non-vegetarians [49]. Diets high in fat may enhance reabsorption of estrogens in the gut [50]. Although controversial, several lines of evidence suggest that increased dietary fat is also associated with increased risk of obesity [3, 4]. Higher dietary fat intake tends to be associated with lower dietary fiber and fruit and vegetable intake, with resultant lower exposure to nutritive antioxidants and a large variety of other potentially anticarcinogenic phytochemicals [51, 52].
There is also growing evidence that the metabolic consequences are different for different fatty acids [3]. Saturated fat intake tends to be highly correlated with total and animal fat intake and the potential mechanisms by which total fat intake may influence endometrial carcinogenesis generally apply to the effects of saturated and animal fat intake as well. Epidemiologic and intervention studies have shown that saturated fat intake has a negative impact in insulin resistance, while monounsaturated and polyunsaturated fat improves it [53]. Insulin resistance is believed to play a major role in the development of endometrial cancer [54]. There is growing interest in the effects of dietary fats on immune function and inflammatory responses [55]. Saturated and animal fat intake also travel with animal foods in the diet, particularly with red meat, which has been suggested to increase endometrial cancer risk (Bandera et al., Consumption of animal foods and endometrial cancer risk: a systematic literature review and meta-analysis, submitted).
In summary, the current epidemiologic evidence suggests a possible role for total fat, saturated fat, and animal fat on endometrial cancer risk. However, because the limited available cohort data did not confirm these findings, conclusions cannot be drawn until more data are published, particularly from cohort studies.
ACKNOWLEDGEMENTS
We would like to thank James Thomas for his valuable help with the data extraction Access® program.
Funding: This work was funded in part by the WCRF and NIH-K07 CA095666. Although this work was funded in part by WCRF, interpretation of the evidence may not represent the views of WCRF and our conclusions may differ from those in the 2007 WCRF report summarizing evidence related to food, nutrition, physical activity, and cancer risk.
Abbreviations:
- WCRF
World Cancer Research Fund International
- AICR
American Institute for Cancer Research
- SLR
Systematic Literature Review
- OR
Odds Ratio
- RR
Relative Risk
- CI
Confidence Interval
- FFQ
food frequency questionnaire
- BMI
body mass index
- HRT
hormone replacement therapy
REFERENCES
- 1.Cancer Facts and Figures: American Cancer Society 2006 [Google Scholar]
- 2.Persson I, Adami H-O. Endometrial cancer. In: Adami H-O, Hunter D, Trichopoulos D, editors. Textbook of Cancer Epidemiology. Oxford University Press; New York, NY: 2002. pp. 359–77. [Google Scholar]
- 3.Bray GA, Lovejoy JC, Smith SR, et al. The influence of different fats and fatty acids on obesity, insulin resistance and inflammation. J Nutr. 2002;132:2488–91. doi: 10.1093/jn/132.9.2488. [DOI] [PubMed] [Google Scholar]
- 4.Astrup A, Ryan L, Grunwald GK, et al. The role of dietary fat in body fatness: evidence from a preliminary meta-analysis of ad libitum low-fat dietary intervention studies. Br J Nutr. 2000;83(Suppl 1):S25–32. doi: 10.1017/s0007114500000921. [DOI] [PubMed] [Google Scholar]
- 5.Wu AH, Pike MC, Stram DO. Meta-analysis: dietary fat intake, serum estrogen levels, and the risk of breast cancer. J Natl Cancer Inst. 1999;91:529–34. doi: 10.1093/jnci/91.6.529. [DOI] [PubMed] [Google Scholar]
- 6.World Cancer Research Fund, American Institute for Cancer Research . Food, Nutrition and the Prevention of Cancer: A Global Perspective. American Cancer Institute for Cancer Research; Washington, DC: 1997. [Google Scholar]
- 7.Bandera EV, Kushi LH, Moore DF, Gifkins DM, McCullough ML. Second Report on Food, Nutrition, Physical Activity and the Prevention of Cancer. World Cancer Research Fund International/American Institute for Cancer Research; 2007. The association between food, nutrition, and physical activity and the risk of endometrial cancer and underlying mechanisms. In Press. [Google Scholar]
- 8.Bandera EV, Kushi LH, Moore DF, Gifkins DM, McCullough ML. Fruits and vegetables and endometrial cancer risk: a systematic literature review and meta-analysis. Nutr Cancer. 58 doi: 10.1080/01635580701307929. In Press. [DOI] [PubMed] [Google Scholar]
- 9.Zhang CY, Wang TG. [A case-control study of endometrial cancer in Beijing] Zhonghua Liu Xing Bing Xue Za Zhi. 1989;10:235–7. [PubMed] [Google Scholar]
- 10.Nagaoka T, Onodera H, Hayashi Y, Maekawa A. Influence of high-fat diets on the occurrence of spontaneous uterine endometrial adenocarcinomas in rats. Teratog Carcinog Mutagen. 1995;15:167–77. doi: 10.1002/tcm.1770150403. [DOI] [PubMed] [Google Scholar]
- 11.Armstrong B, Doll R. Environmental factors and cancer incidence and mortality in different countries, with special reference to dietary practices. Int J Cancer. 1975;15:617–31. doi: 10.1002/ijc.2910150411. [DOI] [PubMed] [Google Scholar]
- 12.Kolonel LN, Hankin JH, Lee J, Chu SY, Nomura AM, Hinds MW. Nutrient intakes in relation to cancer incidence in Hawaii. Br J Cancer. 1981;44:332–9. doi: 10.1038/bjc.1981.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolonel LN, Nomura AM, Hinds MW, Hirohata T, Hankin JH, Lee J. Role of diet in cancer incidence in Hawaii. Cancer Res. 1983;43:2397s–402s. [PubMed] [Google Scholar]
- 14.Prentice RL, Sheppard L. Dietary fat and cancer: consistency of the epidemiologic data, and disease prevention that may follow from a practical reduction in fat consumption. Cancer Causes Control. 1990;1:81–97. doi: 10.1007/BF00053187. discussion 9-109. [DOI] [PubMed] [Google Scholar]
- 15.Petridou E, Kedikoglou S, Koukoulomatis P, Dessypris N, Trichopoulos D. Diet in relation to endometrial cancer risk: a case-control study in Greece. Nutr Cancer. 2002;44:16–22. doi: 10.1207/S15327914NC441_3. [DOI] [PubMed] [Google Scholar]
- 16.La Vecchia C, Decarli A, Fasoli M, Gentile A. Nutrition and diet in the etiology of endometrial cancer. Cancer. 1986;57:1248–53. doi: 10.1002/1097-0142(19860315)57:6<1248::aid-cncr2820570631>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 17.La Vecchia C, Decarli A, Negri E, Parazzini F. Epidemiological aspects of diet and cancer: a summary review of case-control studies from northern Italy. Oncology. 1988;45:364–70. doi: 10.1159/000226642. [DOI] [PubMed] [Google Scholar]
- 18.Villani C, Pucci G, Pietrangeli D, Pace S, Tomao S. Role of diet in endometrial cancer patients. Eur J Gynaecol Oncol. 1986;7:139–43. [PubMed] [Google Scholar]
- 19.Lissner L, Kroon UB, Bjorntorp P, Blosk S, Wilhelmsen L, Silverstolpe G. Adipose tissue fatty acids and dietary fat sources in relation to endometrial cancer: a retrospective study of cases in remission, and population-based controls. Acta Obstet Gynecol Scand. 1993;72:481–7. doi: 10.3109/00016349309021139. [DOI] [PubMed] [Google Scholar]
- 20.Swanson CA, Potischman N, Barrett RJ, et al. Endometrial cancer risk in relation to serum lipids and lipoprotein levels. Cancer Epidemiol Biomarkers Prev. 1994;3:575–81. [PubMed] [Google Scholar]
- 21.Potischman N, Hoover RN, Brinton LA, et al. Case-control study of endogenous steroid hormones and endometrial cancer. J Natl Cancer Inst. 1996;88:1127–35. doi: 10.1093/jnci/88.16.1127. [DOI] [PubMed] [Google Scholar]
- 22.Sturgeon SR, Brock JW, Potischman N, et al. Serum concentrations of organochlorine compounds and endometrial cancer risk (United States) Cancer Causes Control. 1998;9:417–24. doi: 10.1023/a:1008823802393. [DOI] [PubMed] [Google Scholar]
- 23.Potischman N, Swanson CA, Brinton LA, et al. Dietary associations in a case-control study of endometrial cancer. Cancer Causes Control. 1993;4:239–50. doi: 10.1007/BF00051319. [DOI] [PubMed] [Google Scholar]
- 24.Littman AJ, Voigt LF, Beresford SA, Weiss NS. Recreational physical activity and endometrial cancer risk. Am J Epidemiol. 2001;154:924–33. doi: 10.1093/aje/154.10.924. [DOI] [PubMed] [Google Scholar]
- 25.Littman AJ, Beresford SA, White E. The association of dietary fat and plant foods with endometrial cancer (United States) Cancer Causes Control. 2001;12:691–702. doi: 10.1023/a:1011292003586. [DOI] [PubMed] [Google Scholar]
- 26.Jain MG, Rohan TE, Howe GR, Miller AB. A cohort study of nutritional factors and endometrial cancer. Eur J Epidemiol. 2000;16:899–905. doi: 10.1023/a:1011012621990. [DOI] [PubMed] [Google Scholar]
- 27.Furberg AS, Thune I. Metabolic abnormalities (hypertension, hyperglycemia and overweight), lifestyle (high energy intake and physical inactivity) and endometrial cancer risk in a Norwegian cohort. Int J Cancer. 2003;104:669–76. doi: 10.1002/ijc.10974. [DOI] [PubMed] [Google Scholar]
- 28.Shu XO, Zheng W, Potischman N, et al. A population-based case-control study of dietary factors and endometrial cancer in Shanghai, People's Republic of China. Am J Epidemiol. 1993;137:155–65. doi: 10.1093/oxfordjournals.aje.a116655. [DOI] [PubMed] [Google Scholar]
- 29.Goodman MT, Hankin JH, Wilkens LR, et al. Diet, body size, physical activity, and the risk of endometrial cancer. Cancer Res. 1997;57:5077–85. [PubMed] [Google Scholar]
- 30.Goodman MT, Wilkens LR, Hankin JH, Lyu LC, Wu AH, Kolonel LN. Association of soy and fiber consumption with the risk of endometrial cancer. Am J Epidemiol. 1997:294–306. doi: 10.1093/oxfordjournals.aje.a009270. [DOI] [PubMed] [Google Scholar]
- 31.Jain MG, Howe GR, Rohan TE. Nutritional factors and endometrial cancer in Ontario, Canada. Cancer Control. 2000;7:288–96. doi: 10.1177/107327480000700312. [DOI] [PubMed] [Google Scholar]
- 32.McCann SE, Freudenheim JL, Marshall JR, Brasure JR, Swanson MK, Graham S. Diet in the epidemiology of endometrial cancer in western New York (United States) Cancer Causes Control. 2000;11:965–74. doi: 10.1023/a:1026551309873. [DOI] [PubMed] [Google Scholar]
- 33.Salazar-Martinez E, Lazcano-Ponce E, Sanchez-Zamorano LM, Gonzalez-Lira G, Escudero de los Rios P, Hernandez-Avila M. Dietary factors and endometrial cancer risk. Results of a case-control study in Mexico. Int J Gynecol Cancer. 2005;15:938–45. doi: 10.1111/j.1525-1438.2005.00253.x. [DOI] [PubMed] [Google Scholar]
- 34.Tzonou A, Lipworth L, Kalandidi A, et al. Dietary factors and the risk of endometrial cancer: a case--control study in Greece. Br J Cancer. 1996;73:1284–90. doi: 10.1038/bjc.1996.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barbone F, Austin H, Partridge EE. Diet and endometrial cancer: a case-control study. Am J Epidemiol. 1993;137:393–403. doi: 10.1093/oxfordjournals.aje.a116687. [DOI] [PubMed] [Google Scholar]
- 36.Zheng W, Kushi LH, Potter JD, et al. Dietary intake of energy and animal foods and endometrial cancer incidence. The Iowa women's health study. Am J Epidemiol. 1995;142:388–94. doi: 10.1093/oxfordjournals.aje.a117646. [DOI] [PubMed] [Google Scholar]
- 37.Rothman KJ. Modern epidemiology. 1st ed Little, Brown; Boston: 1986. pp. 174–5. [Google Scholar]
- 38.Chêne G, Thompson SG. Methods for summarizing the risk associations of quantitative variables in epidemiologic studies in a consistent form. Am J Epidemiol. 1996;144:610–21. doi: 10.1093/oxfordjournals.aje.a008971. [DOI] [PubMed] [Google Scholar]
- 39.Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135:1301–9. doi: 10.1093/oxfordjournals.aje.a116237. [DOI] [PubMed] [Google Scholar]
- 40.Kushi LH, Sellers TA, Potter JD, et al. Dietary fat and postmenopausal breast cancer. J Natl Cancer Inst. 1992;84:1092–9. doi: 10.1093/jnci/84.14.1092. [DOI] [PubMed] [Google Scholar]
- 41.Howe GR, Hirohata T, Hislop TG, et al. Dietary factors and risk of breast cancer: combined analysis of 12 case-control studies. J Natl Cancer Inst. 1990;82:561–9. doi: 10.1093/jnci/82.7.561. [DOI] [PubMed] [Google Scholar]
- 42.Hunter DJ, Spiegelman D, Adami HO, et al. Cohort studies of fat intake and the risk of breast cancer--a pooled analysis. N Engl J Med. 1996;334:356–61. doi: 10.1056/NEJM199602083340603. [DOI] [PubMed] [Google Scholar]
- 43.Boyd NF, Stone J, Vogt KN, Connelly BS, Martin LJ, Minkin S. Dietary fat and breast cancer risk revisited: a meta-analysis of the published literature. Br J Cancer. 2003;89:1672–85. doi: 10.1038/sj.bjc.6601314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Willett WC, Howe GR, Kushi LH. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65:1220S–8S. doi: 10.1093/ajcn/65.4.1220S. discussion 9S-31S. [DOI] [PubMed] [Google Scholar]
- 45.Levi F, Franceschi S, Negri E, La Vecchia C. Dietary factors and the risk of endometrial cancer. Cancer. 1993;71:3575–81. doi: 10.1002/1097-0142(19930601)71:11<3575::aid-cncr2820711119>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 46.Kushi LH, Byers T, Doyle C, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2006;56:254–81. doi: 10.3322/canjclin.56.5.254. quiz 313-4. [DOI] [PubMed] [Google Scholar]
- 47.Kushi L, Giovannucci E. Dietary fat and cancer. Am J Med. 2002;113(Suppl 9B):63S–70S. doi: 10.1016/s0002-9343(01)00994-9. [DOI] [PubMed] [Google Scholar]
- 48.McCullough ML, Giovannucci EL. Diet and cancer prevention. Oncogene. 2004;23:6349–64. doi: 10.1038/sj.onc.1207716. [DOI] [PubMed] [Google Scholar]
- 49.Goldin BR, Adlercreutz H, Gorbach SL, et al. Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women. N Engl J Med. 1982;307:1542–7. doi: 10.1056/NEJM198212163072502. [DOI] [PubMed] [Google Scholar]
- 50.Gorbach SL, Goldin BR. Diet and the excretion and enterohepatic cycling of estrogens. Prev Med. 1987;16:525–31. doi: 10.1016/0091-7435(87)90067-3. [DOI] [PubMed] [Google Scholar]
- 51.Kris-Etherton PM, Hecker KD, Bonanome A, et al. Bioactive compounds in foods: their role in the prevention of cardiovascular disease and cancer. Am J Med. 2002;113(Suppl 9B):71S–88S. doi: 10.1016/s0002-9343(01)00995-0. [DOI] [PubMed] [Google Scholar]
- 52.Steinmetz KA, Potter JD. Vegetables, fruit, and cancer. II. Mechanisms. Cancer Causes Control. 1991;2:427–42. doi: 10.1007/BF00054304. [DOI] [PubMed] [Google Scholar]
- 53.Riccardi G, Giacco R, Rivellese AA. Dietary fat, insulin sensitivity and the metabolic syndrome. Clin Nutr. 2004;23:447–56. doi: 10.1016/j.clnu.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 54.Kaaks R, Lukanova A, Kurzer MS. Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol Biomarkers Prev. 2002;11:1531–43. [PubMed] [Google Scholar]
- 55.Wu D. Modulation of immune and inflammatory responses by dietary lipids. Curr Opin Lipidol. 2004;15:43–7. doi: 10.1097/00041433-200402000-00009. [DOI] [PubMed] [Google Scholar]
- 56.Willett W, Stampfer M. Implications of total energy intake for epidemiologic studies. In: Willett W, editor. Nutritional Epidemiology. 2nd ed Oxford University Press; New York: 1998. pp. 273–301. [Google Scholar]